Abstract
Background:
This study tried to find out the prevalence of menstrual abnormalities in adolescent girls and their association with dietary and exercise pattern in Garhwal region of India.
Materials and Methods:
In this study, cross-sectional questionnaires survey was conducted in different schools of Garhwal. These questionnaires were based on socioeconomic data, dietary and physical activities, and menstrual abnormalities.
Results:
The age of menarche was 13.5 ± 0.64 years. Dysmenorrhea (62.75%), premenstrual syndrome (PMS) (40.42%), and irregular cycle (28.72%) were observed common problems among adolescent girls. The result showed that dysmenorrhea, PMS, and menstrual irregularities were directly associated with dietary habits and physical activities. Dysmenorrhea was associated with eating junk food (66.10%), and PMS was associated with lacking of physical activities (78.94%).
Conclusion:
The result suggests that feeding habit and physical activities directly affecting the menstrual health of adolescent girls.
Keywords: Adolescent, dysmenorrhea, menarche, menstrual abnormalities, premenstrual syndrome
Introduction
Adolescence is a high-risk group because during this stage major physical and mental change occurs. Menarche is a hallmark biological process of puberty[1] in adolescence girls and it leads to reproductive capacity. Menstrual abnormalities are common in adolescent and can lead to stressful conditions.[2] All over the world around 75% of girls are experiencing problems associated with menstruation.[3] The major abnormalities are dysmenorrhea, premenstrual syndrome (PMS), and menstrual irregularities.[4] These disorders may lead to problems in daily activities such as academic excellence, achievements in sports, and loss of self-confidence.[5,6,7] The lifestyle pattern of any individual leads to their prone of disease. Female reproductive cycle directly or indirectly influence with diet, physical work, and mental stress.
Dietary habits are directly related with individual quality of life,[6] and adolescence is a potential group to view the rapid growth and maturation which requests extranutrients and energy-rich food.[8] Food habits of adolescents in the recent past have changed[9] in their nutrient intake and needs such as widespread consumption of fast food, skipping of food intake.[5,6]
The present study focused on a Garhwali population of Uttarakhand. Influence of globalization changes the lifestyle of local people in positive as well as negative aspect. In Uttarakhand, one-third of the females between 15 and 49 years are undernourished[10] due to poor energy intake and junk food. The dietary pattern in hilly region also shifts from local pahari food to Western foods among the adolescent age group. Hence, it is important to evaluate the influence of eating habits on menstrual disorders in young women. The relationship between food habit and menstrual dysfunction has been becoming an important issue in the world.[6] Apart from feeding habits, physical activities, daily routine lifestyle, and work stress also influence directly or indirectly the female reproductive cycle.
Although menstrual disorders are common among females, no study on regarding their prevalence and associate factors were found in hilly populations, especially in Garhwali communities. Hence, this study aims to find out the pattern of menstrual abnormalities in school going girls in Garhwali population and their association with dietary habits and physical work.
Materials and Methods
A school-based cross-sectional study was conducted in adolescent girls. In this study, 13–19-year age girls were selected from different location of Garhwal region. The purpose of the study was clearly explained to each student and after that who were willing to participate, selected for further study. The girls were asked to signed a consent form before participating in the study.
The questionnaires were explained properly to them, which dealt with different parameters such as socioeconomic data, feeding habits, physical activity, menstrual history, and irregularities. Students, who were suffering from any chronic health issues, were excluded from the study.
The healthy diet concluded based on nutritional value. The nutritional value calculated, based on the food present on particular area Garhwal region (green vegetables, pulses, wheat, finger millet, rice, and milk). The consumption of junk food was also including in the dietary habit. It is also categorized into two parts: (1) Junk food intake <3 days/week, (2) junk food intake 4–7 days/week. Physical activity calculated in terms of the number of days of regular exercise, household work, and sports per week. Physical exercise categorized into two: (1) <2 days of physical work per week and (2) 3–7 days of physical work per week.
Regarding menstrual abnormalities, girls were asking to date their Menarche. The questions regarding the menstrual pattern concerned duration of the most recent menstrual intervals, average days of bleeding, and regarding menstrual problem and their frequency with menstrual abnormalities.
Chi-square test was applied to compare the dietary and exercise patterns among students having menstrual disorders and those who do not have menstrual disorders. For statistical analysis, SPSS Ver. 14 (Inc, Chicago IL, USA) Software and MS Excel were used.
Results
Lifestyle characteristics
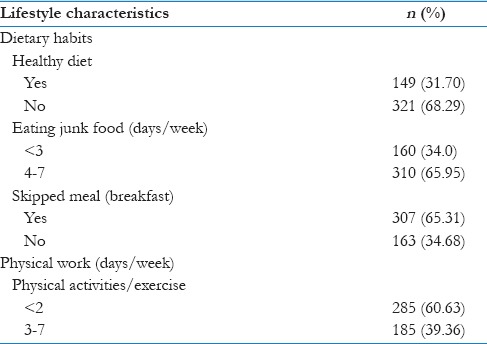
In total, 470 girls were taken participation in this study. All the participants of this study belong to moderate middle-class families. The lifestyle pattern showed that 31.70% girls were taking healthy diet while maximum girls (68.29%) showed poor nutritional diet. Eating junk food habit was found in 65.95% girls. The study also revealed that 65.31% girls skipped their breakfast. The study showed 60.63% girls were worked <2 days/week and 39.36% girls were worked 4–7 days\week [Table 1].
Table 1.
Lifestyle characteristics of adolescent girls in Garhwal region
Menstrual irregularities and their association with lifestyle characteristics
The age of menarche was 13.5 ± 0.64 years and the average days of period from 4 to 6 days were recorded. The menstrual abnormalities, such as dysmenorrhea, were present in 62.75% girls, PMS in 40.42%, and menorrhagia in 9.5% of the whole sampling population. The irregular cycle was observed in 28.72% girls [Table 2].
Table 2.
Prevalence of menstrual abnormalities in adolescent girls of Garhwal region
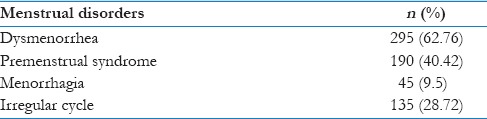
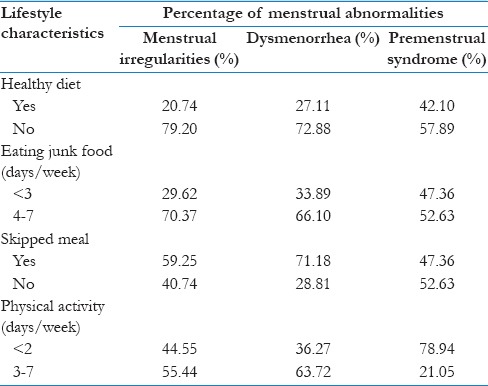
Table 3 showed the association between the menstrual problems and lifestyle factors. Dysmenorrhea was more frequently observed among those adolescents who were associated eating junk food (66.10%) and unhealthy diet (72.88%). Menstrual irregularities were also significantly more common among girls who were eating junk food regularly (70.37%) and who were not having a healthy diet (79.20%). Dysmenorrhea was also more common in the girls who were skipping breakfast (71.18%). The PMS showed a direct relationship with physical activity of girls. Participants who were doing less physical activities/work had a higher percent (78.94%) of PMS. Chi-square test was showed significant (χ2 = 213, P < 0.05) difference among students having menstrual abnormalities and those who do not have menstrual abnormalities on the basis of dietary and exercise.
Table 3.
Association of menstrual abnormalities with feeding habit and physical work
Menstrual interference with life activities
The result also showed that menstrual abnormalities affecting the quality of life in girls. Nearly 45% percent of the girls indicated that they missed school because of their periods. Of the girls who missed school, dysmenorrhea (pain) was the most common reason reported for school absence (35%). The result also showed that in the severe pain 42% girls were using painkiller (Analgesic). Apart from dysmenorrhea, PMS (15%) and menstrual irregularities (4%) affecting daily routine work and social activities.
Discussion
The study on the prevalence of menstrual disorder and its association with food habits was the first kind of study in Garhwali population. Most of the participants in this region were belongs to middle-class families. With the support of the schools, a very positive response observed for most of the questions. This study attempted to find a relation between various lifestyle factors such as eating junk food, healthy food, and lack of physical activities with the menstrual problems experienced by the adolescent girls.
In previous, it would be thought that menstrual abnormalities are found higher in metropolitan cities as compared to small hilly towns due to lifestyle pattern. Now, this study highlights that due to globalization, lifestyle pattern change in everywhere, which was affecting adolescent in every way. Yet, the age of menarche in Garhwal population show lower (13.5) compared to European and Western countries.[11] Most of the studies showed the menarcheal age stabilized at the age of 12 to13 year.[12,13] The lower age of menarche could explain that the variation in age of menarche change according to the hereditary pattern, nutritional status, and climate difference.[7]
The result suggested that the dysmenorrhea is the highest among all menstrual abnormalities in a mountainous region, which support the fact that dysmenorrhea is common among 70%–90% adolescent girls[14,15] globally. Overall, the prevalence of menstrual problems in girls of Garhwal is similar to other reported communities.[3,16,17] PMS was also more commonly present in this region, although its percentage is less in Garhwal region as compare to Lakkawar (69%), Sarkar (61.5%) and Rupa (51.2%) studies, which were conducted in other parts of India.[7,18,19]
The unhealthy and inadequate dietary habits affecting every female's quality of life not only in the present but also in the upcoming future. In this study, the majority of the girls, skipping their breakfast and associated with higher consumption of junk food. Dysmenorrhea was considerably higher in girls who were consistently eating fast food. Because junk foods are rich in saturated fatty acids, and these acids affect the metabolism of progesterone in the menstrual cycle.[6] Junk foods also lack micronutrients, which might be responsible for triggering dysmenorrhea, premenstrual symptoms, and menstrual irregularities. Nowadays, skipping breakfast is common habits among in adolescent, this pattern shows in Garhwali population also, which leads obesity[16] and menstrual abnormalities.[5,20] The diet limitation and skipping breakfast lead gynecological problems[6] specifically the hormonal changes which cause menstrual disorders in most of the females.[21] This study clearly indicates that dysmenorrhea not only affected by the dietary habit but also with the physical activity. This study supporting the fact that there was a positive correlation between the lower risk of dysmenorrhea and followed regular exercise and healthy physical activity for adolescent girls.[22] A bunch of studies in nursing students also revealed that menstrual disorders are very common in adolescent girls and regular exercise and improved dietary habits are essential to prevent menstrual abnormalities.[23,24]
In this study, premenstrual symptoms were present high in those girls who were not doing regular physical work. The PMS and physical work association also showed in school going girls of Pondicherry, India.[7] Other parts of worlds also showed similar kind of associations between positive diagnosis of PMS and lower level of physical work.[25,26] The physical activities release more endorphins hormones, which can decrease the PMS symptoms such as pain, depression, and anxiety.[7,27] In the present scenario, menstrual abnormalities are causing significant debility in adolescent girls. Self-medication was practiced by 42% of the adolescent girls, which indicate dysmenorrhea affecting the maximum population of adolescent girls. The study showed that routine activities, school absentees, and emotional distress were due to dysmenorrhea and PMS. Sickness absenteeism is notably more among dysmenorrheic girls, this conclusion also finds by other studies.[28,29] Even Bergsjo's study in the USA disclosed that sickness absenteeism because of dysmenorrhea causes wastage of millions of dollars due to suffering work satisfaction, personal relationships, confidence, and concentration at workplaces.[30] Some other studies also show that dysmenorrhea and PMS were perceived as the most stressful symptoms leading to school absenteeism and household activities in girls.[31,32,33,34] Overall, there is a significant association present between consumption of junk food, dieting,[35] and physical exercise with an abnormal flow.[18]
Hence, the changing lifestyle patterns such as eating junk food and reducing physical activities are directly affecting the menstrual cycle of females. Hence, it is important to promote the health education programs which should include promoting adequate dietary habit, regular exercise, and awareness on menstrual hygiene in school level for improving the menstrual health. The improvement of menstrual health is important for preventing the many present and future gynecological problems (infertility, obesity, and polycystic ovaries).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rigon F, De Sanctis V, Bernasconi S, Bianchin L, Bona G, Bozzola M, et al. Menstrual pattern and menstrual disorders among adolescents: An update of the Italian data. Ital J Pediatr. 2012;38:38. doi: 10.1186/1824-7288-38-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deligeoroglou E, Creatsas G. Menstrual disorders. Endocr Dev. 2012;22:160–70. doi: 10.1159/000331697. [DOI] [PubMed] [Google Scholar]
- 3.Lee LK, Chen PC, Lee KK, Kaur J. Menstruation among adolescent girls in Malaysia: A cross-sectional school survey. Singapore Med J. 2006;47:869–74. [PubMed] [Google Scholar]
- 4.Deligeoroglou E, Tsimaris P, Deliveliotou A, Christopoulos P, Creatsas G. Menstrual disorders during adolescence. Pediatr Endocrinol Rev. 2006;3(Suppl 1):150–9. [PubMed] [Google Scholar]
- 5.Fujiwara T. Skipping breakfast is associated with dysmenorrhea in young women in Japan. Int J Food Sci Nutr. 2003;54:505–9. doi: 10.1080/09637480310001622369. [DOI] [PubMed] [Google Scholar]
- 6.Fujiwara T, Sato N, Awaji H, Sakamoto H, Nakata R. Skipping breakfast adversely affects menstrual disorders in young college students. Int J Food Sci Nutr. 2009;60(Suppl 6):23–31. doi: 10.1080/09637480802260998. [DOI] [PubMed] [Google Scholar]
- 7.Rupa Vani K, Veena KS, Subitha L, Hemanth Kumar VR, Bupathy A. Menstrual abnormalities in school going girls – Are they related to dietary and exercise pattern? J Clin Diagn Res. 2013;7:2537–40. doi: 10.7860/JCDR/2013/6464.3603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anand K, Kant S, Kapoor SK. Nutritional status of adolescent school children in rural North India. Indian Pediatr. 1999;36:810–5. [PubMed] [Google Scholar]
- 9.Balbi C, Musone R, Menditto A, Di Prisco L, Cassese E, D’Ajello M, et al. Influence of menstrual factors and dietary habits on menstrual pain in adolescence age. Eur J Obstet Gynecol Reprod Biol. 2000;91:143–8. doi: 10.1016/s0301-2115(99)00277-8. [DOI] [PubMed] [Google Scholar]
- 10.Fact Sheet, Uttranchal. 2005-2006 National Family Health Survey NHFS-3. International Institute for Population Sciences. 2006 [Google Scholar]
- 11.Wyshak G, Frisch RE. Evidence for a secular trend in age of menarche. N Engl J Med. 1982;306:1033–5. doi: 10.1056/NEJM198204293061707. [DOI] [PubMed] [Google Scholar]
- 12.Gaudineau A, Ehlinger V, Vayssiere C, Jouret B, Arnaud C, Godeau E, et al. Factors associated with early menarche: Results from the French health behaviour in school-aged children (HBSC) study. BMC Public Health. 2010;10:175. doi: 10.1186/1471-2458-10-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Papadimitriou A, Fytanidis G, Douros K, Bakoula C, Nicolaidou P, Fretzayas A, et al. Age at menarche in contemporary Greek girls: Evidence for levelling-off of the secular trend. Acta Paediatr. 2008;97:812–5. doi: 10.1111/j.1651-2227.2008.00806.x. [DOI] [PubMed] [Google Scholar]
- 14.Hillen TI, Grbavac SL, Johnston PJ, Straton JA, Keogh JM. Primary dysmenorrhea in young Western Australian women: Prevalence, impact, and knowledge of treatment. J Adolesc Health. 1999;25:40–5. doi: 10.1016/s1054-139x(98)00147-5. [DOI] [PubMed] [Google Scholar]
- 15.Banikarim C, Chacko MR, Kelder SH. Prevalence and impact of dysmenorrhea on Hispanic female adolescents. Arch Pediatr Adolesc Med. 2000;154:1226–9. doi: 10.1001/archpedi.154.12.1226. [DOI] [PubMed] [Google Scholar]
- 16.Vicdan K, Kukner S, Dabakoglu T, Ergin T, Keles G, Gokmen O, et al. Demographic and epidemiologic features of female adolescents in Turkey. J Adolesc Health. 1996;18:54–8. doi: 10.1016/1054-139x(95)00127-e. [DOI] [PubMed] [Google Scholar]
- 17.Wiksten-Almströmer M, Hirschberg AL, Hagenfeldt K. Menstrual disorders and associated factors among adolescent girls visiting a youth clinic. Acta Obstet Gynecol Scand. 2007;86:65–72. doi: 10.1080/00016340601034970. [DOI] [PubMed] [Google Scholar]
- 18.Lakkawar NJ, Jayavani RL, Arthi N, Alaganandam P, Vanajakshi N. A study of menstrual disorders in medical students and its correlation with biological variables. Scholars J Appl Med Sci. 2014;2:3165–75. [Google Scholar]
- 19.Sarkar AP, Mandal R, Ghorai S. Premenstrual syndrome among adolescent girl student in a rural school of West Bengal, India. Int J Med Sci Public Health. 2016;5:408–11. [Google Scholar]
- 20.Fujiwara T, Nakata R. Current problems of food intake in young women in Japan: Their influence on female reproductive function. Reprod Med Biol. 2004;3:107–14. doi: 10.1111/j.1447-0578.2004.00063.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Randhawa JK, Mahajan K, Kaur M, Gupta A. Effect of dietary habits and socio-economic status on menstrual disorders among young females. Am J Biosci. 2016;4:19–22. [Google Scholar]
- 22.Latthe P, Mignini L, Gray R, Hills R, Khan K. Factors predisposing women to chronic pelvic pain: Systematic review. BMJ. 2006;332:749–55. doi: 10.1136/bmj.38748.697465.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kafaei M, Ajorpaz N, Abbaszadeh F, Mohebbi Z, Asghari M. Association between menstrual cycle regularity and obesity-related anthropometric indices in dormitory students of Kashan University of Medical Sciences. Nurs Pract Today. 2014;1:101–6. [Google Scholar]
- 24.Said AR, Mettwaly MG. Improving life style among nursing students regarding menstrual disorders through an educational training program. Int J Nurs Sci. 2017;7:35–43. [Google Scholar]
- 25.Seedhom AE, Mohammed ES, Mahfouz EM. Life style factors associated with premenstrual syndrome among El-Minia University Students, Egypt. ISRN Public Health. 2013;2013:1–6. [Google Scholar]
- 26.Teixeira AL, Oliveira ÉC, Dias MR. Relationship between the level of physical activity and premenstrual syndrome incidence. Rev Bras Ginecol Obstet. 2013;35:210–4. doi: 10.1590/s0100-72032013000500004. [DOI] [PubMed] [Google Scholar]
- 27.Cerin A, Collins A, Landgren BM, Eneroth P. Hormonal and biochemical profiles of premenstrual syndrome. Treatment with essential fatty acids. Acta Obstet Gynecol Scand. 1993;72:337–43. doi: 10.3109/00016349309021108. [DOI] [PubMed] [Google Scholar]
- 28.Kumbhar SK, Reddy M, Sujana B, Reddy R, Divya BK, Balkrishna C. Prevalence of dysmenorrhea among adolescent girls (14-19 yrs) of Kadapa district and its impact on quality of life: A cross sectional study. Natl J Community Med. 2011;2:265–8. [Google Scholar]
- 29.Avasarala AK, Panchangam S. Dysmenorrhoea in different settings: Are the rural and urban adolescent girls perceiving and managing the dysmenorrhoea problem differently? Indian J Community Med. 2008;33:246–9. doi: 10.4103/0970-0218.43231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bergsjø P. Socioeconomic implications of dysmenorrhea. Acta Obstet Gynecol Scand Suppl. 1979;87:67–8. doi: 10.3109/00016347909157793. [DOI] [PubMed] [Google Scholar]
- 31.Busch CM, Costa PT, Jr, Whitehead WE, Heller BR. Severe perimenstrual symptoms: Prevalence and effects on absenteeism and health care seeking in a non-clinical sample. Women Health. 1988;14:59–74. doi: 10.1300/J013v14n01_05. [DOI] [PubMed] [Google Scholar]
- 32.Dean BB, Borenstein JE. A prospective assessment investigating the relationship between work productivity and impairment with premenstrual syndrome. J Occup Environ Med. 2004;46:649–56. doi: 10.1097/01.jom.0000131796.62115.84. [DOI] [PubMed] [Google Scholar]
- 33.Drive JO, Magian BA. Saunders Publication; 2004. Normal Menstrual Cycle Clinical Obstetrics and Gynecology; p. 121. [Google Scholar]
- 34.Robinson RL, Swindle RW. Premenstrual symptom severity: Impact on social functioning and treatment-seeking behaviors. J Womens Health Gend Based Med. 2000;9:757–68. doi: 10.1089/15246090050147736. [DOI] [PubMed] [Google Scholar]
- 35.Fujiwara T. Dietary habits affecting reproductive functions in young women. Rep Syst Sex Dis Int J. 2017;1:00010. [Google Scholar]


