Abstract
Introduction:
In National Programme for Prevention and Control of Deafness (NPPCD), the management of ear diseases of rural India is now guided by Revised Indian Public Health Standards (IPHS) for Rural Health Facilities for providing quality ear care. However, despite the IPHS existence, coverage and quality ear care is questionable. Moreover, this issue has not yet been studied till now in the Indian context. The objective of the study was to assess the role of Private Medical College Training Center (Rural Health Training Centre [RHTC]) in augmenting quality of ear care services in NPPCD at district level by adopting IPHS Standards.
Materials and Methods:
A combined retrospective and prospective cohort study was done at RHTC of a Medical College in West Uttar Pradesh from January 1, 2013, to December 31, 2017, by retrospective approach of selecting all ear patients (n = 3840) and prospective way of assessing the impact of IPHS for ear care. The semi-structured Pro forma was used in exploring the coverage and quality of ear care. The data were analyzed by Epi Info version 7.2.
Results:
Out of total 4817 ear, nose, and throat (ENT) patients, the majority of ear patients (n = 3840) were initially dissatisfied with coverage and quality of ear services provided by ENT specialists at RHTC. However, when IPHS exposure was given from July 1, 2015 to December 31, 2017, not only majority of patients were satisfied (n = 3110, 81%) but also ear curative treatment was significantly higher (n = 2120, 68.1% vs. n = 130, 17.8%, odds ratio = 9.8, RR = 1.5, P < 0.00001).
Conclusions:
Adherence to IPHS in NPPCD is essential for delivering better ear care by RHTC through primary health-care approach.
Keywords: Cohort study, Indian Public Health Standards, National Programme for Prevention and Control of Deafness, otology, Rural Health Training Centre
Introduction
Ear, nose, and throat (ENT) disorders are one of the prime reasons for a visit to a primary care doctor in both rural and urban communities across the world.[1] Even though ENT symptoms are common reasons for consulting GPs,[2,3] most individuals manage their problem in the community without seeking help.[4,5,6,7] Moreover, in many developing countries, there is a lack of ENT specialists and overburdened ENT hospital units.[8]
The Indian Rural Community is also currently bearing the rising burden of ENT diseases, where the prevalence of ENT disorders ranging from 4.3% in a district to 11% has been reported from various studies in literature.[9,10,11,12,13,14,15,16,17,18,19,20] This situation further complexes, as there are only a few population-based epidemiological studies on ENT assessments among adults in the Indian context.[13] Moreover, in developing world such as India, there also exists a scarcity of services and training in otolaryngology, audiology, and speech therapy, which is reflected by the gap between health-care delivery in high-income countries and low-income countries with a shortfall in services and training in all areas of otorhinolaryngology.[14]
Among ENT diseases, hearing loss is the most common sensory deficit in humans today. Worldwide, it is the second leading cause for “Years lived with Disability” the first being depression. Nearly 450 million people in the world had been disabled by hearing loss.[21] In India also, there are a large number of hearing impaired young people which is causing severe loss of productivity, both physical as well as economic. A large percentage of children between the ages of 0 and 14 years are also suffering from significant auditory impairment.[22] Further few studies[10,11,12] in Indian Rural Context have also reported the high prevalence of otological morbidities in pediatric population also.
The larger percentage of Indian population also suffers from milder degrees of hearing loss and unilateral (one sided) hearing loss. According to WHO (2018) data,[23] the prevalence of hearing impairment (HI) in India is around 6.3% (63 million people suffering from significant auditory loss). The estimated prevalence of adult-onset deafness in India is 7.6% and childhood-onset deafness is 2%.
Although secondary and tertiary ENT care services are useful in creating awareness of the common ENT conditions, with their recognized important role in decreasing the burden of the otorhinolaryngological disorders in the community.[1] However, the models of primary health-care approach in ENT care can provide a new opportunity for tackling ENT diseases from primary care level.[2] This new strategy has many benefits as seen from studies[1,18,19] which are in favor that common ENT disorders in outpatient department can be tackled at the level of primary health care efficiently as well as effectively. Even WHO says that nearly 50% of deafness can be prevented if primary health-care approach is adopted for otological care across the world. Hence, adoption of primary health-care approach in National Programme for Control of Deafness has been done, as a new strategy since its prevention and inception in 2006.[1,24,25] The strategy to motivate and integrate health professionals working in the field of ear and hearing to bring services to the community level by involving both government and private sectors in systematic training and ENT care services by primary health-care professionals is also recommended by the WHO Guidelines and other studies in literature.[23,24,25]
Moreover, the management of ear diseases of rural India nowadays is now further guided and strengthened by new revised updated Indian Public Health Standards (IPHS) since 2012 for National Programme for Prevention and Control of Deafness (NPPCD) from rural health facilities such as subcenter (SC), primary health center (PHC), and community health center (CHC).[9,10,11] However, even despite the existence of IPHS, the coverage and quality impact of IPHS on ear care from primary care level are still questionable and not yet been studied till now. Therefore, this study explores an impact of applying IPHS for rural health-care facilities in private setup in augmenting services of National Programme for Control of Deafness in India. Moreover, no such kind of study has been done so far in area of a Rural Health Training Centre (RHTC) of a Medical College in India, making this study unique in its own kind.
Materials and Methods
Research question
Can a Private Medical College Training Centre (RHTC) augment the quality of ear care services in NPPCD at District level (In public–private partnership (PPP) Model) by adopting IPHS?
Key objective of study
The objective of the study was to assess the impact of applying IPHS on coverage, quality, and satisfaction fulfillment of ear care of patients.
Ethical approval
An approval of Ethical Committee of the institution as well as permission from CMO of District Muzaffarnagar for coordination of ear patients’ management under IPHS guidelines in NPPCD was sought. This was followed by health center's patients’ consent for their participation in the study followed by their enlisting.
Methodology
Study design: A combined retrospective and prospective cohort study [Figure 1]
Duration of study: January 1, 2013–December 31, 2017 (5 years) (from June 30, 2015 to January 1, 2013 – for ear patients’ selection retrospectively from RHTC and SC records of cohort of ENT patients and prospective follow-up of ear patients from July 1, 2015 to December 31, 2017, for IPHS exposure in NPPCD)
Place of Study: At RHTC of a Private Medical College (Muzaffarnagar) Uttar Pradesh. Here both EAR patients of Private RHTC and government health facility – SC in catchment area of six villages were treated at RHTC for study after sensitization of ENT specialists to IPHS in NPPCD of this medical college after joining hands with District Provincial Medical Health Services in PPP mode. RHTC was chosen for this study because it had a sufficient catering population of 44,100 (up to July 1, 2015) covering six villages (i.e., Dhandhera, Bhagwanpur, Shernagar, Bilaspur, Makhiyali, and Sikheda) and the medical college to which the RHTC was attached – ensured the regular availability of the ENT specialists visit at RHTC
Ear care services provided in study: Level of SC (house-to-house survey – ear patients identification) and PHC (otoscopic examination of ear and tuning fork test [512 Hz] –test only).
Figure 1.

Methodology of cohort study
Sampling technique
All ENT patients who were seen at RHTC and SC as identified by Health Worker (M and F), their residences in these six villages, were first enlisted from this area at RHTC in first 2½ years. Then, from all these ENT patients (collected retrospectively), only all ear patients under NPPCD were selected and followed in cohort study for IPHS exposure at RHTC. Hence, the sufficient representativeness of population in the study was maintained, without any bias.
Inclusion criteria
Revised IPHS services criteria followed since 2012 in NPPCD (primary to secondary health level [SC, PHC, andCHC]/RHTC [services by ENT specialist posted at RHTC):
Early detection and referral of HI and deafness (D) cases (SC level – house-to-house survey)
Basic diagnostic and treatment services of common ear diseases (Wax, OE, ASOM, CSOM, etc,) awareness generation for ear diseases – IEC approach
Improving participation of community in primary prevention and early detection of HI/D
PPP Models – for ear care in NPPCD – private ENT clinics/private medical College training centers.
Working definitions for study
Deafness (WHO definition)
Complete loss of hearing ability in one or two ears (hearing loss >90 dB in better ear [profound impairment] or total loss of hearing in both the ears)
The WHO definition of “hearing impairment” refers to both complete and partial loss of ability to hear.
Hearing handicapped
It is defined by the Rehabilitation Council of India Act. (1992). In India, it is defined as HI of 70 dB and above in better ear or total loss of hearing in both ears.
Hearing impairment
Section 2 (i and iv) Persons with Disability (PWD) Act, 1995 – A disability and a “PWD” means a person suffering from not <40% of any disability as certified by a medical authority.
Hearing disability
Section 2 (i) – “a hearing disable person is one who has the hearing loss of 60 dB or more in the better ear for conversational range of frequencies.”
Exclusion criteria
However, responses of newborns were excluded to obtain a better quality response of respondents as well as nose and throat patients were excluded from this study.
Data collection and analysis
Both quantitative and qualitative data in our study was collected through semi-structured interview and observations. The data on ENT care needs of patients studied by various Pro formas were analyzed by appropriate statistical software such as Epi Info (version 7.2).
Results
The majority of patients availing ENT care at RHTC were initially dissatisfied with coverage and quality of ear services provided by ENT specialists (39.1%, n = 4817) before July 1, 2015. From ENT patients, 3840 ear patients were selected who attended ear specialist services at RHTC for 2.6 years from July 1, 2015 to December 31, 2017). Hence, total ear patients given services in NPPCD (IPHS – after removal of 977 Nose and throat patients was therefore 3840.
Overall 39.1% patients availed ENT specialist services in 2.6-year duration from January 1, 2013 to June 30, 2015, which was although higher in next 2.6 years on December 31, 2017 (45.8%) and this ENT services’ usage was more from Bilaspur village (35.1%) [Table 1].
Table 1.
Profile of patients availing general and ear, nose, or throat specialist services

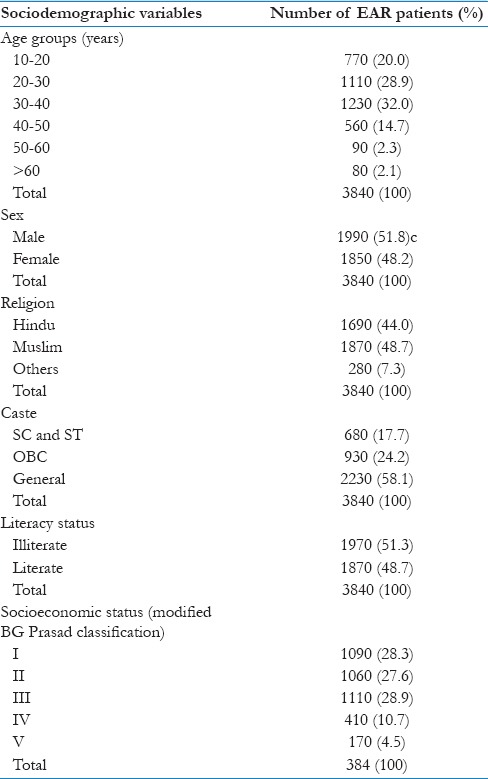
The majority of patients availing ear specialist services at RHTC were male (51.8%), in 30–40-year age group (32.0%), belonged to Muslim religion (48.7%), and general caste (58.1%), illiterate category (51.3%), and majority of them were in Class III (Senior Executive Service, 28.9%) [Table 2].
Table 2.
Sociodemographic profile of patients availing EAR specialist services at Role of Private Medical College Training Centre (n=3840)
Even after applying IPHS, out of total 3840 patients, 19% (n = 730) who attended ear specialist services and were even dissatisfied from ear services in IPHS at RHTC – the most common dissatisfaction reason was the need for minor ENT procedures on first visit (10.4%, n = 400) and least was for the ear drops’ requirement for ear disorders (4.2%, n = 160). However, majority of ear patients who were satisfied from ear services at RHTC (81%, n = 3110); the prime reasons were early diagnosis and proper ear care services’ education from ear, specialists [Tables 3 and 4].
Table 3.
Profile of patients for presence of satisfaction from EAR specialist services at Rural Health Training Centre in National Programme for Prevention and Control of Deafness (Indian Public Health Standards criteria) (n=3840)

Table 4.
Profile of EAR patients types of satisfaction for services received from EAR specialist services with Indian Public Health Standards criteria in National Programme for Prevention and Control of Deafness (n=3840)

It was also further seen that, after strict adherence to IPHS (July 1, 2015–December 31, 2017), out of the satisfied ear Patients (n = 3110, 81%), the majority of them completed the full ear curative treatment (n = 2120, 68.1% vs. n = 130, 17.8%, odds ratio = 9.8, RR = 1.5) and this difference was also statistically significant (P < 0.00001) [Table 5].
Table 5.
Profile of satisfaction of patients from EAR specialists services in National Programme for Prevention and Control of Deafness on Indian Public Health Standards criteria and its consequent impact on achievement of EAR curative treatment (n=3840)

Discussion
WHO says that nearly 50% of deafness can be prevented across the world if primary health-care approach is adopted for ear care.[23] No doubt that even the most common ENT disorders in the form of ear disorders presenting to the emergency department can be managed at the level of primary health-care level as revealed by similar kind of studies in literature.[1,8,9,18,26,27,28,29] For decreasing such burden of the ENT diseases in the community, studies have, therefore, suggested the adoption of primary health-care delivery model of ENT disease services.[1,8,9,10,11,12,13,14,15,16,17,18,19,27,28,29] The role of RHTCs in delivery of community-oriented primary care is also an important strategy for primary level ENT care as revealed in many similar kinds of studies in literature.[1,26,27,28,29] However, the actual focus on quality, coverage, and needs of ear care at primary level is revealed further from our present study.
In the present study, increasing prevalence of ENT disorders from 39.1% in June 2015 to 45.8% in December 2017 in RHTC and SC area indicates possibly increasing popularity of ENT specialist services in the study area, probably due to the positive effect of IPHS adopted in NPPCD. This could also be due to the fact that the majority of patients who were availing ear specialist services at RHTC were adult males of Muslim religion with illiterate background and belonging to medium class of socioeconomic status; who initially might not have been able to appreciate the ENT specialist services without NPPCD till June 2015 but later on with proper ICE messages on ear care might have appreciated the ENT specialist advices. Hence, from the present study, the higher burden of otorhinolaryngological disorders in the form of ear disorders till June 2015 reveals the fact that possibly the health education messages related to ear care/hearing loss might have been well received by patients from ENT specialists in the study area with standard programmatic of IPHS in NPPCD. Our finding was in unison with many studies indicating higher burden of ENT diseases in community for which some structured programs are required for them.[9,10,11,12,13,14,15,16,17,18,19]
Although the actual burden of primary health-care services’ delivery for ear disorders is government health facilities such as SC, PHC, and CHC, the good role of private health training centers (RHTC) as a supportive and substantial role in primary ENT care services has been seen in many studies[27,28,29] in the past, so it should be taken into consideration in view of the rising private medical colleges in health system of India.[9,10,11,12,13,14]
In our study, we further found that maximum felt need was for minor ENT procedures even with IPHS in NPPCD; this indicates that this ENT care also needs attention in terms of service delivery in NPPCD. This finding was also in unison with many other studies.[1,8,9,10,19,29] The key finding of our study that majority of ear patients being satisfied from ear services at RHTC (81%, n = 3110) is possibly due to early diagnosis and proper ear care services’ education from ear specialists adopting IPHs criteria in NPPCD. It has also been evident from studies[1,8,9,10,19,27,28,29,30,31] in literature that, for increasing awareness of the people in developing countries on ENT diseases, adoption of modes such as social campaigns and health education aimed at providing quality ENT primary health care services may also be a one answer similar to the issue raised in our study. Our study also reveals that after strict adherence to IPHS increased not only the satisfaction level of ear patients (81%) but was also associated statistically significantly (P < 0.00001) with full ear curative treatment completion (68.1%). This also indicates that there is a dire need of coverage and quality of ear services by patients for ENT care in NPPCD. Many studies in the past have also emphasized the similar role of psychological factors as an important determinants of treatment outcomes in other diseases including ENT diseases.[32,33,34,35] It has also been seen from literature that discussing one's feelings about the diagnosis, and attention to other psychosocial issues, can also predict patient satisfaction[35] as also studied in our study.
It has been seen from literature that ENT disorders such as hearing loss also have a direct impact on mental health,[36] so link with psychosocial component cannot be ruled out, as found in our study also. Hence, finally, from our cohort study, therefore, it is evident that, by taking into account the multiple factors such as focus on coverage, quality, and satisfaction of ear patients, IPHS for NPPCD can augment ear care at primary level if implemented properly.
Limitations of study
Generalization of study finding should be done with caution as only ear patients were taken from sampled villages in a specified programme. Lack of other psychosocial issues and other infrastructure issues can be a constraint in our study.
Conclusions
Greater coverage and quality of otological care in rural areas is possible, provided IPHS for NPPCD are implemented properly at rural health facilities level such as SC and RHTC. The RHTC of a private medical college can be a useful resource for NCD programme (NPPCD) at a district level provided the adherence to IPHS for EAR care – is followed for delivering better EAR care by primary health care approach.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Emerson LP, Job A, Abraham V. A model for provision of ENT health care service at primary and secondary hospital level in a developing country. Biomed Res Int. 2013;2013:562643. doi: 10.1155/2013/562643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dong W, Erens B, Shaw A, McMunn A, Field J, Haskell WL, et al. Scottish Health Statistics. Edinburgh, Scotland, SD: Information and Statistics Division, National Health Service in Scotland; 1998. [Google Scholar]
- 3.McCormick A, Fleming D, Charlton J. London: Office of National Statistics, HMSO; 1995. Morbidity Statistics from General Practice 4th National Study 1992–1993. [Google Scholar]
- 4.White KL, Williams TF, Greenberg BG. The ecology of medical care. N Engl J Med. 1961;265:885–92. doi: 10.1056/NEJM196111022651805. [DOI] [PubMed] [Google Scholar]
- 5.Hannay DR. London: Routledge & Kegan Paul; 1979. The Symptom Iceberg. A Study of Community Health. [Google Scholar]
- 6.Dunnell K, Cartwright A. Medicine Takers, Prescribers and Hoarders. London: Routlege & Kegan Paul; 1972. [Google Scholar]
- 7.Green LA, Fryer GE, Jr, Yawn BP, Lanier D, Dovey SM. The ecology of medical care revisited. N Engl J Med. 2001;344:2021–5. doi: 10.1056/NEJM200106283442611. [DOI] [PubMed] [Google Scholar]
- 8.Hannaford PC, Simpson JA, Bisset AF, Davis A, McKerrow W, Mills R, et al. The prevalence of ear, nose and throat problems in the community: Results from a national cross-sectional postal survey in Scotland. Fam Pract. 2005;22:227–33. doi: 10.1093/fampra/cmi004. [DOI] [PubMed] [Google Scholar]
- 9.Singh A, Kumar S. A survey of ear, nose and throat disorders in rural India. Indian J Otolaryngol Head Neck Surg. 2010;62:121–4. doi: 10.1007/s12070-010-0027-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Indian Public Health Standards for Sub-centres, Primary Health Centres, Community Health Centres, Government of India, Ministry of Health and Family Welfare. [Last accessed on2018 Apr 15; Last updated on 2018 Apr 15]. Available from: http://www.nhm.gov.in/nhm/nrhm/guidelines/indian-public-health-standards.html .
- 11.Government of India, Ministry of Health and Family Welfare. National Programme for Prevention and Control of Deafness. 2016. [Last accessed on 2018 Apr 18; Last updated on 2016 Jun 29]. Available from: http://www.dghs.gov.in/content/1362_3_NationalProgrammePreventionControl.aspx .
- 12.Kishve SP, Kumar N, Kishve PS, Syed MM, Kalakoti P. Ear nose and throat disorders in paediatric patients at a rural hospital in India. Acad Manag J. 2010;3:786–90. [Google Scholar]
- 13.Rao RS, Subramanyam MA, Nair NS, Rajashekhar B. Hearing impairment and ear diseases among children of school entry age in rural South India. Int J Pediatr Otorhinolaryngol. 2002;64:105–10. doi: 10.1016/s0165-5876(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 14.Srinivasan K, Prabhu GR. A study of the morbidity status of children in social welfare hostels in Tirupati town. Indian J Community Med. 2006;31:170–2. [Google Scholar]
- 15.Hannula S, Bloigu R, Majamaa K, Sorri M, Mäki-Torkko E. Audiogram configurations among older adults: Prevalence and relation to self-reported hearing problems. Int J Audiol. 2011;50:793–801. doi: 10.3109/14992027.2011.593562. [DOI] [PubMed] [Google Scholar]
- 16.Wagner R, Fagan J. Survey of otolaryngology services in central America: Need for a comprehensive intervention. Otolaryngol Head Neck Surg. 2013;149:674–8. doi: 10.1177/0194599813505972. [DOI] [PubMed] [Google Scholar]
- 17.Yeli SS. Prevalence of ENT disorders in children: A tertiary medical care study. J Otorhino Laryngol. 2015;3:1–6. [Google Scholar]
- 18.Sharma K, Bhattacharjya D, Barman H, Goswami SC. Common ear, nose, and throat problems in pediatric age group presenting to the emergency clinic – Prevalence and management: A hospital-based study. Indian J Clin Pract. 2014;24:756–60. [Google Scholar]
- 19.Nepali R, Sigdel B. Prevalence of ENT diseases in children: Hospital based study. Internet J Otorhinolaryngol. 2012;14:1–5. [Google Scholar]
- 20.Chadha SK, Sayal A, Malhotra V, Agarwal AK. Prevalence of preventable ear disorders in over 15,000 schoolchildren in Northern India. J Laryngol Otol. 2013;127:28–32. doi: 10.1017/S0022215112002691. [DOI] [PubMed] [Google Scholar]
- 21.Vasileiou I, Giannopoulos A, Klonaris C, Vlasis K, Marinos S, Koutsonasios I, et al. The potential role of primary care in the management of common ear, nose or throat disorders presenting to the emergency department in Greece. Qual Prim Care. 2009;17:145–8. [PubMed] [Google Scholar]
- 22.Nanda MS, Bhalke ST. Epidemiology of Otorhinolaryngology Diseases Seen in Health Camps in Rural Backward Areas of Himachal Pradesh. 2016. Mar 23, [Last accessed on 2018 Apr 23; Last updated on 2016 Mar 23]. Available from: http://www.jorl.net/otolaryngology/otolaryngology/epidemiology-of-otorhinolaryngology-diseases-seen-inhealth-camps-inrural-backward-areas-of-himachal-pradesh.html .
- 23.Wilson J. Deafness in developing countries. Approaches to a global program of prevention. Arch Otolaryngol. 1985;111:2–9. doi: 10.1001/archotol.1985.00800030036002. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization. Report of the International Workshop on Primary Ear & Hearing Care. 2018. Mar 14, [Last accessed on 2018 Apr 15; Last updated on 2018 Apr 15]. pp. 1–19. Available from: http://www.who.int/pbd/deafness/activities/en/capetown_final_report.pdf .
- 25.Mulwafu W, Kuper H, Viste A, Goplen FK. Feasibility and acceptability of training community health workers in ear and hearing care in Malawi: A cluster randomised controlled trial. BMJ Open. 2017;7:e016457. doi: 10.1136/bmjopen-2017-016457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization. [Last accessed on 2018 Apr 15; Last updated on 2018 Apr 15];Increasing community awareness on ear and hearing health. 2013 10:1–12. Available from: http://www.disabilitycentre.lshtm.ac.uk/files/2012/10/CEHH13_final-2014_low-res-f.pdf . [Google Scholar]
- 27.Nutter S. The Health Triangle Anchor Points, Inc; 2003. ISBN 0974876003. [Google Scholar]
- 28.Ancker JS, Kern LM, Abramson E, Kaushal R. The triangle model for evaluating the effect of health information technology on healthcare quality and safety. J Am Med Inform Assoc. 2012;19:61–5. doi: 10.1136/amiajnl-2011-000385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singer S, Danker H, Dietz A, Hornemann B, Koscielny S, Oeken J, et al. Screening for mental disorders in laryngeal cancer patients: A comparison of 6 methods. Psychooncology. 2008;17:280–6. doi: 10.1002/pon.1229. [DOI] [PubMed] [Google Scholar]
- 30.Davey S, Raghav SK, Singh JV, Davey A, Singh N. A comparative evaluation of public health centers with private health training centers on primary healthcare parameters in India: A study by data envelopment analysis technique. Indian J Community Med. 2015;40:252–7. doi: 10.4103/0970-0218.164394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davey S, Raghav SK, Muzammil K, Singh JV, Davey A, Singh SK, et al. Study on role of rural health training centre (RHTC) as a supporting component to a primary health care system for NRHM programme in district Muzaffarnagar (UP) Int J Res Med Sci. 2014;2:653–61. [Google Scholar]
- 32.Davey S, Raghav SK, Singh JV, Davey A, Singh N, Maheshwari C. Psycho-social needs fulfilment- can it be a predictor of otorhinolaryngological services outcome of a rural heath training centre. A study by wellness triangle analysis? Int J Community Med Public Health. 2017;4:1032–8. [Google Scholar]
- 33.Fasunla AJ, Samdi M, Nwaorgu OG. An audit of ear, nose and throat diseases in a tertiary health institution in South-Western Nigeria. Pan Afr Med J. 2013;14:1. doi: 10.11604/pamj.2013.14.1.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brown EL. Meeting patients’ psychosocial needs in the general hospital. Ann Am Acad Polit Soc Sci. 1963;346:117–25. [Google Scholar]
- 35.Beran D. Needs and needs assessments: A gap in the literature for chronic diseases. SAGE Open. 2015;5:1–10. [Google Scholar]
- 36.Semple C, Parahoo K, Norman A, McCaughan E, Humphris G, Mills M, et al. Psychosocial interventions for patients with head and neck cancer. Cochrane Database Syst Rev. 2013;16:CD009441. doi: 10.1002/14651858.CD009441.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]


