Abstract
Background:
Occupational exposure to bloodborne pathogen is a significant risk to health-care workers. In any teaching hospital apart from regular health-care workers and employees, there are significant population of students and trainee. It is important to assess the health-care worker in hospital which has maximum chances of exposure to these pathogens. The aim of this study is to determine the most susceptible job group for needlestick injury (NSI) reported in a newly established teaching medical institute in the Western part of Rajasthan, India.
Methods:
This is a retrospective analysis of data of NSI occurred during September 2014 to January 2017.
Results:
Sixty three NSIs were reported during the study. Nursing students were the most vulnerable group who reported maximum number of NSI. Among the nursing students, 72% were completely vaccinated against hepatitis B virus.
Conclusions:
Nursing students are at utmost risk for NSIs, the prevention of which requires regular training and education.
Keywords: Health-care worker, hepatitis B virus, needlestick injury, nursing students
Introduction
Percutaneous injuries among health-care workers (HCWs) caused by needles and sharps pose a significant risk of occupational transmission of bloodborne pathogens such as human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV). According to the Centers for Disease Control and Prevention, approximately 384,000 percutaneous injuries occur annually in the US hospitals, with about 236,000 of these resulting from needle sticks involving hollow-bore needles.[1] In an estimate, it was observed that every year proportions of HCWs exposed to bloodborne pathogens is 2.6% for HCV, 5.9% for HBV, and 0.5% for HIV, corresponding to about 16,000 HCV infections and 66,000 HBV infections in HCWs worldwide.[2] In developing regions, 40%–65% of HBV and HCV infections in HCWs were attributable to percutaneous occupational exposure.[2] Nurses are an important t bridge between doctors and patients. They sustain most sharp-related injuries in any hospital as observed in a multicentric study carried out in India.[3] Apart from HCWs, there are many trainees who receive their training in teaching Institutes and medical colleges. In India, the number of nursing schools and colleges has increased by more than 300% in the last 15 years, resulting in the annual capacity to train more than 216,000 nurses.[4] Nursing institutes offering the Bachelor of Science in Nursing have increased to more than 1500 in our country. More than 76,000 nursing student are passing from these institutes every year. Apart from this, more than 100,000 students pass out from Auxiliary Nursing and Midwifery and General Nursing and Midwifery courses in India annually.[4,5] The students are trained to provide care to people of all ages. The broad fundamental principles of nursing care are based on sound knowledge and satisfactory levels of skill; which includes standard precautions, hospital infection control (HIC) practices, safe injection practices, and others.[6] In a questionnaire-based study carried out in Brazil, it was seen that 18.1% nursing students had suffered sharp-related injury.[7] Needlestick injury (NSI) among this group is not only associated with physical issues but also psychological issues.[8] The other important group that is susceptible to sharp injuries is housekeeping staff. Although they are not involved in handling sharp directly, they directly come in contact with patients. However, mostly they suffer injuries due to failure to dispose sharp properly. They also bear the significant burden of sharp-related blood and body fluid exposures as was observed in an prospective study carried out in India.[9]
This study was undertaken with an aim to determine the most susceptible job group for NSIs reported in a newly established Teaching Medical Institute in the Western part of Rajasthan, India.
Materials and Methods
This is a retrospective study with the study period of September 2014 to January 2017. Our institute is a 250-bedded newly established tertiary care hospital and medical institute in Western Rajasthan, where 75 students are admitted to the nursing college, and 100 students take admission into the MBBS course, annually. As a routine protocol of the Health Informatics Center unit of our institute, all relevant information for NSI are collected in a pro forma, which has details of the (i) source, including his/her diagnosis, hepatitis B surface antigen (HBsAg), HIV, and HCV antibody status, (ii) health worker's designation and work experience, previous history of NSIs or blood transfusions and vaccination status for hepatitis-B including anti-HBsAg titer if done, HIV, HBsAg, and anti-HCV antibody status, and (iii) time of reporting, duration since injury, time and place of incident, mode of injury, description of the injury (mucosal exposure, spill on preexisting cut, superficial percutaneous, or deep percutaneous), type of first aid given and whether universal precautions were followed by the HCW. All HCWs are managed as per current National AIDS Control Organization (NACO) guidelines.[10]
All the NSI cases which were reported to the department within study period and had complete NSI records were included in the study. Follow-up cases and cases with incomplete records were excluded from the study. The group receiving most number of NSIs was studied further regarding the type of injury and their hepatitis-B vaccination status.
Collected data were entered and analyzed using Microsoft Excel, and the results were expressed as percentages in tabular form.
Results
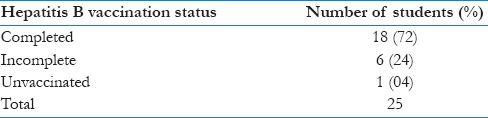
A total of 63 cases of needlestick injuries (NSIs) were reported to HIC unit during the study. Nursing students accounted for almost one-third of the total reported cases followed by nursing staff, housekeeping staff, senior residents, junior residents, and others [Table 1]. Most common type of injury among nursing students was deep percutaneous, followed by superficial percutaneous [Table 2], and most of the injuries were sustained in the hospital during their duty hours. In time duration between exposure and seeking postexposure prophylaxis, more than 50% of nursing students reported within the first 2 hrs of injury [Table 3]. Of the total exposed nursing students, 18 (72%) students had the history of complete hepatitis B vaccination at the time of exposure, and one student was completely unvaccinated at the time of exposure [Table 4]. Of the total 25 events of NSI, the source was known in 23 cases whereas in 2 cases, the source of injury was not traceable as injury occurred from abandoned sharps. In case of known source, none were found to be suffering from HIV, hepatitis-B, or hepatitis-C on testing.
Table 1.
Distribution of needle stick injury among health-care workers according to their professional status (n=63)
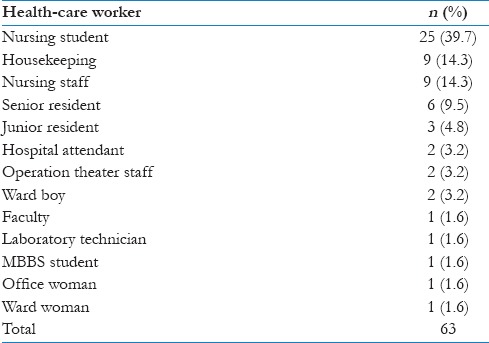
Table 2.
Type of injury sustained by nursing students (n=25)
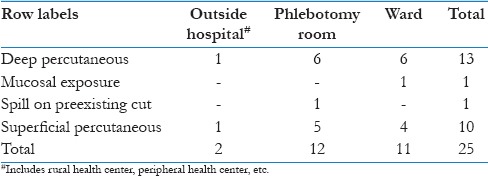
Table 3.
Distribution of time since exposure and reporting of needle sticks injuries among nursing students
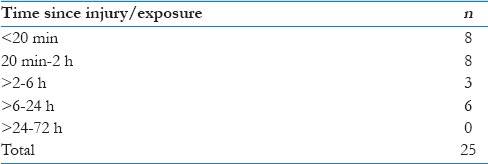
Table 4.
Hepatitis B vaccination status of the nursing students with needle sticks injuries
Discussion
Every year, many NSI are reported in hospitals worldwide and are associated with exposure to bloodborne pathogens such as HIV, HCV, and HBV.
In present study, nursing students were the most common HCW who sustained NSI, followed by housekeeping staff, and nursing staff. In an Australian questionnaire-based study carried out in 2005, it was observed that 38 nursing students (13·9%) reported a needle stick or sharps injury during the study of 12 months, and 39.5% of NSIs were not reported.[11] In another questionnaire-based study done among the nursing students in India, Prasuna et al. reported that the occurrence of NSI during their training program was reported by 39.76% of nursing students. Moreover, maximum NSIs (57.6%) occurred during the first year of course.[12] High rate of injury in nursing students may be due to a large number of exposure during the procedures conducted by them as their learning protocol, combined with their inexperience. In a retrospective study done at a tertiary care medical institute in India, it was seen that HCWs with work experience of less than 1 year accounted for about 50% of reported.[13] Clarke et al. in their study found that the probability of ever having a NSI was inversely related to the years of experience.[14] Less number of injuries among senior doctors in the present study is surprising; however, it could be due to underreporting of the NSIs as in most of the surgical cases, the patient's HIV, HBsAg, and HCV test is done before the surgical procedure. Elder and Paterson in their review concluded that the degree of underreporting of sharps injuries may be as much as 10 fold when recorded through standard reporting systems.[15] In a questionnaire-based study done in Egypt, it was seen that 74.7% HCWs did not report the injury to employee health services, and physicians were less likely to report an NSI as compared to other health-care professionals.[16]
In the present study, most common type of NSI in the nursing population was deep percutaneous, followed by superficial percutaneous. The deep percutaneous injury was mostly due to wide hollow bore needle mostly at the time of collecting blood from venipuncture and was categorized as severe exposure. In case of HIV-positive source, this incident will necessitate starting of three drug regimes as per the NACO guidelines.[10] Deep injury is one of the important factors that increase the likelihood of transmission of HIV after percutaneous injury because of high-viral load in blood and direct access of vein or artery.[13,17] It has been seen in animal studies that the effectiveness of postexposure prophylaxis following NSI is time dependent.[18,19] Most of the guidelines recommend that postexposure prophylaxis should be started within first 72 h duration as it is effective only if given during this period.[20] In our study, it was seen that all the nursing students reported within first 24 h of exposure and more than half of them reported within first 2 h. This shows the considerable awareness among this group of HCW. In addition, there is a need to further reinforce this awareness among all HCWs.
As far as, the vaccination status of nursing students is concerned, 72% students were found to be completely vaccinated for hepatitis B. In a study carried out during 2015 in Agartala, it was seen that 80% of nursing students were vaccinated against HBV.[21] Similarly, in a multicentric study carried out in Turkey, it was seen that 85% students were completely vaccinated against hepatitis-B although the results varied among students of various nursing schools.[22] Vaccination plays an indispensable role in preventing hepatitis-B infection by formation of anti-HBsAg antibodies. However, even after complete vaccination, there are chances that seroconversion will not occur in almost 5% of vaccinated individuals (nonresponders) rendering them susceptible to HBV transmission following any NSI.[23] Titer of anti-HBsAg antibody >10 mIU/ml is considered as protective in vaccinated individuals if they get an injury. All HCWs are at a risk for occupational blood or body fluid exposure should undergo compulsory vaccination against hepatitis-B and get their anti-HBsAg antibody level tested after 1–2 months of receipt of the last dose of the vaccine series. In case of injury among nonresponders (anti-HBs <10 mIU/ml), additional booster doses are required and measures taken as per recent guidelines.[24] The previous studies on HCWs published from various parts of the world have reported 12%–21% nonresponders among total HBV vaccine recipients.[25] India is considered to have intermediate level of endemicity with regard to HBV. The point prevalence of HBV is 3.7%, which include over 40 million HBV carriers. HBV is the second most common cause of acute viral hepatitis after HEV in India.[26] Unvaccinated and incompletely immunized student are at higher risk of getting hepatitis-B infection in case of NSI.[26] In addition, causes of underreporting of NSI require further evaluation, which is the need of the hour.
Conclusion
HCWs are always at high risk of attaining NSIs, and nursing students are the most vulnerable group among all, requiring extra attention. There should be a regular training and education of nursing students regarding the prevention and treatment of NSIs, and it should be ensured that proper standard precautions are followed at all levels. In a tertiary teaching hospital, mandatory provisions for complete vaccination against hepatitis-B should be made for all the medical/nursing students and all HCWs including senior faculty and residents, followed by detection of anti-HBsAg antibody titers. Since many NSI cases go underreported, regular counseling and teaching should be carried out, so that early and prompt postexposure prophylaxis measures can be undertaken in NSI cases, wherever required.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.The National Institute for Occupational Safety and Health (NIOSH). Stop Sticks Campaign. NIOSH. [Last accessed on 2017 Aug 08]. Available from: http://www.cdc.gov/niosh/stopsticks/sharpsinjuries.html .
- 2.Prüss-Üstün A, Rapiti E, Hutin Y, Campbell-Lendrum D, Corvalán C, Woodward A. Geneva: World Health Organisation; 2003. Sharps Injuries Global Burden of Disease from Sharps Injuries to Health-Care Workers. [Google Scholar]
- 3.Chakravarthy M, Singh S, Arora A, Sengupta S, Munshi N. The epinet data of four Indian hospitals on incidence of exposure of healthcare workers to blood and body fluid: A multicentric prospective analysis. Indian J Med Sci. 2010;64:540–8. [PubMed] [Google Scholar]
- 4.Hazarika I. Health workforce in India: Assessment of availability, production and distribution. WHO South East Asia J Public Health. 2013;2:106–12. doi: 10.4103/2224-3151.122944. [DOI] [PubMed] [Google Scholar]
- 5.Indian Nursing Council. [Last accessed on 2017 Aug 01]. Available from: http://www.indiannursingcouncil.org/pdf/Govt_Pvt_data_31-10-2016_final.pdf .
- 6.Neerja K. Textbook of Nursing Education. 1st ed. Noida: Jaypee Medical Publisher Pvt Ltd; 2005. [Google Scholar]
- 7.Souza-Borges FR, Ribeiro LA, Oliveira LC. Occupational exposures to body fluids and behaviors regarding their prevention and post-exposure among medical and nursing students at a Brazilian public university. Rev Inst Med Trop Sao Paulo. 2014;56:157–63. doi: 10.1590/S0036-46652014000200012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hambridge K, Nichols A, Endacott R. The impact of sharps injuries on student nurses: A systematic review. Br J Nurs. 2016;25:1064–71. doi: 10.12968/bjon.2016.25.19.1064. [DOI] [PubMed] [Google Scholar]
- 9.Chakravarthy M, Singh S, Arora A, Sengupta S, Nita M, Rangaswamy S, et al. Epidemiology of sharp injuries e prospective EPINet data from five tertiary care hospitals in India e data for 144 cumulated months, 1.5 million inpatient days. Clin Epidemiol Glob Health. 2014;2:121–6. [Google Scholar]
- 10.New Delhi: NACO, Ministry of Health and Family Welfare, Government of India, National AIDS Control Organization; 2007. Antiretroviral Therapy Guidelines for HIV – Infected Adults and Adolescents including Post-exposure Prophylaxisnone. [Google Scholar]
- 11.Smith DR, Leggat PA. Needlestick and sharps injuries among nursing students. J Adv Nurs. 2005;51:449–55. doi: 10.1111/j.1365-2648.2005.03526.x. [DOI] [PubMed] [Google Scholar]
- 12.Prasuna J, Sharma R, Bhatt A, Arazoo, Painuly D, Butola H, et al. Occurrence and knowledge about needle stick injury in nursing students. J Ayub Med Coll Abbottabad. 2015;27:430–3. [PubMed] [Google Scholar]
- 13.Jayanth ST, Kirupakaran H, Brahmadathan KN, Gnanaraj L, Kang G. Needle stick injuries in a tertiary care hospital. Indian J Med Microbiol. 2009;27:44–7. [PubMed] [Google Scholar]
- 14.Clarke SP, Rockett JL, Sloane DM, Aiken LH. Organizational climate, staffing, and safety equipment as predictors of needlestick injuries and near-misses in hospital nurses. Am J Infect Control. 2002;30:207–16. doi: 10.1067/mic.2002.123392. [DOI] [PubMed] [Google Scholar]
- 15.Elder A, Paterson C. Sharps injuries in UK health care: A review of injury rates, viral transmission and potential efficacy of safety devices. Occup Med (Lond) 2006;56:566–74. doi: 10.1093/occmed/kql122. [DOI] [PubMed] [Google Scholar]
- 16.Hanafi MI, Mohamed AM, Kassem MS, Shawki M. Needlestick injuries among health care workers of University of Alexandria hospitals. East Mediterr Health J. 2011;17:26–35. [PubMed] [Google Scholar]
- 17.Cardo DM, Culver DH, Ciesielski CA, Srivastava PU, Marcus R, Abiteboul D, et al. A case-control study of HIV seroconversion in health care workers after percutaneous exposure. Centers for Disease Control and Prevention Needlestick Surveillance Group. N Engl J Med. 1997;337:1485–90. doi: 10.1056/NEJM199711203372101. [DOI] [PubMed] [Google Scholar]
- 18.Spira AI, Marx PA, Patterson BK, Mahoney J, Koup RA, Wolinsky SM, et al. Cellular targets of infection and route of viral dissemination after an intravaginal inoculation of simian immunodeficiency virus into rhesus macaques. J Exp Med. 1996;183:215–25. doi: 10.1084/jem.183.1.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsai CC, Emau P, Follis KE, Beck TW, Benveniste RE, Bischofberger N, et al. Effectiveness of postinoculation (R)-9-(2-phosphonylmethoxypropyl) adenine treatment for prevention of persistent simian immunodeficiency virus SIVmne infection depends critically on timing of initiation and duration of treatment. J Virol. 1998;72:4265–73. doi: 10.1128/jvi.72.5.4265-4273.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sultan B, Benn P, Waters L. Current perspectives in HIV post-exposure prophylaxis. HIV AIDS (Auckl) 2014;6:147–58. doi: 10.2147/HIV.S46585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reang T, Chakraborty T, Sarker M, Tripura A. A study of knowledge and practice regarding Hepatitis B among nursing students attending tertiary care hospitals in Agartala city. Int J Res Med Sci. 2015;3:1641–9. [Google Scholar]
- 22.Yamazhan T, Durusoy R, Tasbakan MI, Tokem Y, Pullukcu H, Sipahi OR, et al. Nursing students’ immunisation status and knowledge about viral hepatitis in Turkey: A multi-centre cross-sectional study. Int Nurs Rev. 2011;58:181–5. doi: 10.1111/j.1466-7657.2010.00869.x. [DOI] [PubMed] [Google Scholar]
- 23.Walayat S, Ahmed Z, Martin D, Puli S, Cashman M, Dhillon S, et al. Recent advances in vaccination of non-responders to standard dose hepatitis B virus vaccine. World J Hepatol. 2015;7:2503–9. doi: 10.4254/wjh.v7.i24.2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schillie S, Murphy TV, Sawyer M, Ly K, Hughes E, Jiles R, et al. CDC guidance for evaluating health-care personnel for hepatitis B virus protection and for administering postexposure management. MMWR Recomm Rep. 2013;62:1–9. [PubMed] [Google Scholar]
- 25.Zeeshan M, Jabeen K, Ali AN, Ali AW, Farooqui SZ, Mehraj V, et al. Evaluation of immune response to hepatitis B vaccine in health care workers at a tertiary care hospital in Pakistan: An observational prospective study. BMC Infect Dis. 2007;7:120. doi: 10.1186/1471-2334-7-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shrivastava A, Kumar S. Hepatitis in India: Burden, strategies and plans. NCDC Q Newsl. 2014;3:1–3. [Google Scholar]


