Abstract
Background
Cuffed and uncuffed endotracheal tubes are commonly used for pediatric patients in surgery and emergency situations. It is still controversial which approach should be adopted. The purpose of the study was to compare the application of cuffed and uncuffed endotracheal tubes in pediatric patients.
Methods
We searched PubMed, Web of Science and Cochrane Library for clinical trials, which compared the two applications in children. The study characteristics and clinical data were summarized by two independent reviewers. Meta-analysis of the data was done using Revman 5.3 software.
Results
6 studies with 4141 cases were included in this meta-analysis. The pooling analysis showed that more patients need tube changes in uncuffed than cuffed tubes (OR: 0.07, 95% CI: 0.05-0.10, P < 0.00001). However, there were no differences on intubation duration, reintubation occurrence, accidental extubation rate, croup occurrence and racemic epinephrine use during the intubation process. Also we didn’t find any differences on laryngospasm and stridor occurrence after extubation.
Conclusions
Our study demonstrated that uncuffed endotracheal tubes increased the need for tube changes. Other incidences or complications between the two groups had no differences. Cuffed tubes may be an optimal option for pediatric patients. But more trials are needed in the future.
Keywords: Cuffed, Uncuffed, Endotracheal tube, Children, Meta-Analysis
1. Introduction
Endotracheal tubes are widely used in pediatric patients in emergency department and surgical operations [1]. In clinical practice, uncuffed tracheal tubes are preferred in children for the fear that the cuff would make airway mucosal injury, tissue edema and fibrosis, leading a life-threatening result [2]. Cuffed tracheal tubes emerge for its unique role in avoiding air leakage and safety use during treatment [3]. However, there are still no clear preference for the selection of them in these sufferers. Although a meta-analysis with 4 included studies was undertaken in 2015 [4], those items analyzed in the previous pooling analysis was relatively limited. Also, new studies are being done in recent years. This encourages a new pooling of the current evidences. Thus, a new meta-analysis is done in the study to demonstrate this issue.
2. Materials and Methods
2.1. Search strategy
This meta-analysis was conducted according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) standards [5,6]. Institutional review board approval then was not needed for this study. A thorough search was done in PubMed, Cochrane Library and Web of Science for the potential studies which compared cuffed and uncuffed endotracheal tubes in children, from the inception to November, 2017, without restriction of languages and article types.
2.2. Inclusion and exclusion criteria
The study selection was done by two independent reviewers. Studies meeting the following criteria were included: (1) randomized controlled trials, prospective or retrospective studies; (2) endotracheal tubes were applied in children or pediatric patients without any restriction of disease types; (3) outcomes were compared between cuffed and uncuffed groups. The exclusion criteria were: (1) case reports, editorials, letters, basic studies and reviews; (2) articles that lack the original data.
2.3. Data extraction
Data in the included studies were extracted and summarized independently by two authors. Any disagreement was resolved by consensus-based discussion among all the authors and determined by the corresponding author. The study outcomes extracted were classified into peri- and post-procedural outcomes. Peri-intubation outcomes were tube change, duration of intubation, accidental extubation and reintubation. Post-procedural results included racemic epinephrine, croup, laryngospasm and stridor.
2.4. Quality assessment
The quality of observational studies was assessed using the Newcastle-Ottawa Quality Assessment Scale [7], which consists of three factors: patient selection, comparability of the study groups, and assessment of outcome. A score of 0–9 was allocated to each study. Studies that achieved six or more stars were considered to be of high quality. The quality assessment of randomized controlled trial was done according to the Cochrane risk of bias tool [8].
2.5. Statistical analysis
Meta-analyses were conducted using Review Manager 5.3. The weighted mean difference (WMD) and odds ratio (OR) were used to compare continuous and dichotomous variables, respectively. All results were reported with 95% confidence intervals (CIs). Statistical heterogeneity between trials in this analysis was assessed using the I2 values and χ2 statistics with p value < 0.1, which is significant being set at I2 > 50% according to the Cochrane Reviewer’s Handbook. Random effects and fix effects models were used for the meta-analysis. The risk of publication bias was planned to be assessed using funnel plot. All statistical tests were two-sided.
3. Results
3.1. Description of the study selection
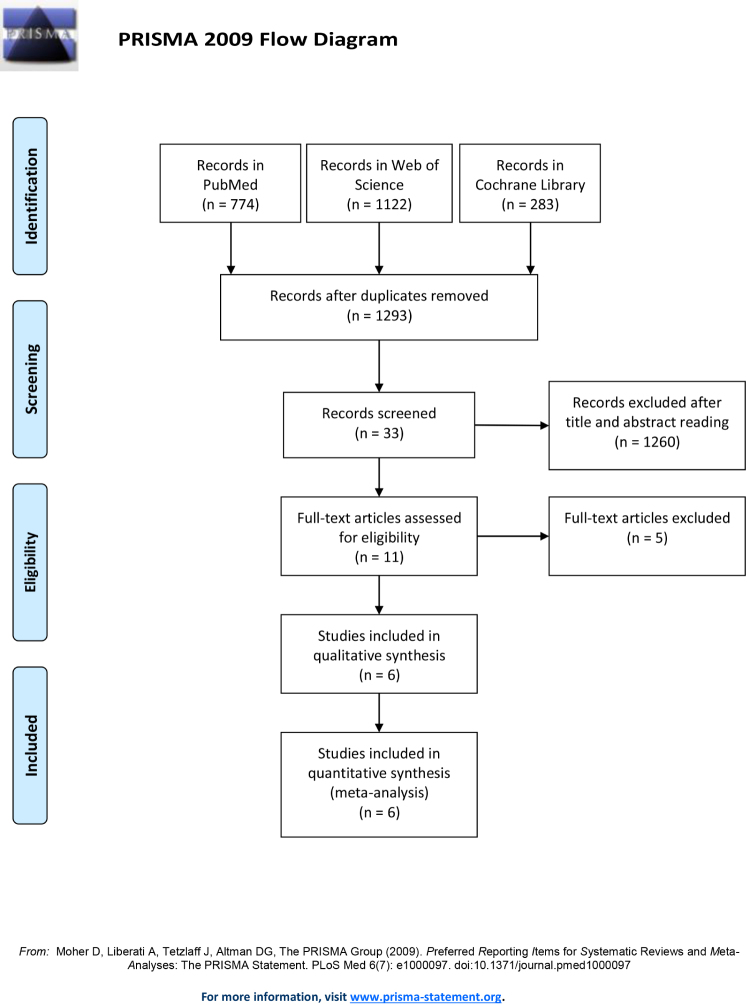
The study flow of this meta-analysis was displayed in Figure 1. The initial electronic search in PubMed, Cochrane Library and Web of Science from inception to November, 2017 yielded 2179 articles. After removal of the duplicates, 1293 articles were further analyzed. A following thorough review of the titles and abstracts excluded 1260 studies. We then evaluated the full-texts of the remaining studies, with a final inclusion of 6 records. The study characteristics were shown in Table 1. There were 4141 cases in total, with 2078 in cuffed and 2063 in uncuffed group. There were 2 randomized controlled trials [9,10] and 4 cohort studies [11,12,13,14] in the pooling analysis. 3 studies came from USA, 2 were undertaken in Switzerland, and 1 was from Turkey. 3 of them gave the precise study period, 1 only give the investigation duration, and this information was not applicable in 2 studies. Other information, including gender, age, weight, endotracheal pathway, peri-intubation, post-extubation variables and quality assessment were shown in detail in Table 1.
Figure 1.
The study flow of the meta-analysis.
Table 1.
The study characteristics of the included studies. RCT, randomized controlled trial; NA, not applicable;
| No. | Gender | Age | Weight | Oral/Nasal | Peri-intubation | Post-extubation | Quality | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Year | Region | Design | period | Cuffed | Uncuffed | Cuffed | Uncuffed | Cuffed | Uncuffed | Cuffed | Uncuffed | Cuffed | Uncuffed | |||
| Ozden [9] | 2016 | Turkey | RCT | 2010.06-2011.06 | 40 | 40 | 7 | 12 | 14.2 ±8.6 | 10.2 ±8.9 | 10 ±3.3 | 8± 3.2 | NA | NA | duration of intubation, surgery time, anesthesia time, reintubation, 02 desaturation, difficulties with intubation | stridor, laryngospasm, croup, coughing, retching, vomiting, blood on tubes, blood at aspiration | RCT |
| Sathyamoorthy [11] | 2015 | USA | cohort | 2011.05-2012.06 | 29 | 195 | NA | NA | NA | NA | NA | NA | NA | NA | NA | stridor | 7 |
| Weiss [10] | 2009 | Switzerland | RCT | NA | 1197 | 1049 | 66.9% | 65.00% | 1.84 | 1.85 | 11.4 ±4.7 | 11.2 ±4.6 | 1142/55 | 961/88 | patients need tube changes, duration of intubation, accidental extubation, reintubation | stridor, laryngospasm | RCT |
| Newth [12] | 2004 | Switzerland | cohort | 1 year | 438 | 422 | NA | NA | NA | NA | NA | NA | NA | NA | duration of intubation, racemic epinephrine use | NA | 5 |
| Khine [13] | 1997 | USA | cohort | NA | 251 | 237 | NA | NA | 3.3 ±2.4 | 2.9 ±2.2 | 15.1 ±7.4 | 14.3 ±7.7 | NA | NA | patients need tube changes, patients need >2 FGF, duration of intubation, reintubation, racemic epinephrine use | croup | 7 |
| Deakers [14] | 1994 | USA | cohort | 1988.07-1989.02 | 123 | 120 | 77 | 64 | 8.08 ±0.59 | 2.53 ± 0.35 | NA | NA | 114/9 | 112/8 | duration of intubation, accidental extubation, air leak present at extubation, PRISM score, reintubation | stridor | 7 |
3.2. Outcome of interest
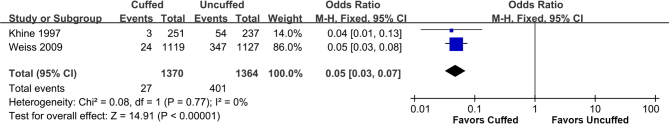
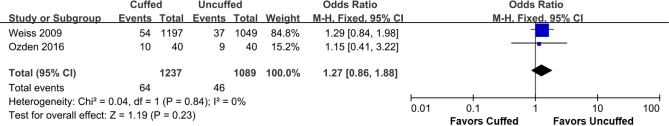
We collected and summarized the data into two sections: peri- and post-procedural. For parameters during procedure, we found that more patients in uncuffed group need tube changes than cuffed group (OR: 0.05, 95% CI: 0.03-0.07; P < 0.00001) (Figure 2). But the duration of intubation (Supplemental Figure 1), the incidence of accidental extubation (Supplemental Figure 2), tube reintubation (Supplemental Figure 3) and racemic epinephrine use (Supplemental Figure 4) were not significantly different between the two groups (Table 2). For post-extubation events, we collected data of the incidence of croup (Supplemental Figure 5), stridor (Supplemental Figure 6) and laryngospasm (Supplemental Figure 7). And we didn’t find any differences of them between uncuffed and cuffed groups in pooling results (Table 3).
Figure 2.
The meta-analysis of tube changes between cuffed and uncuffed groups.
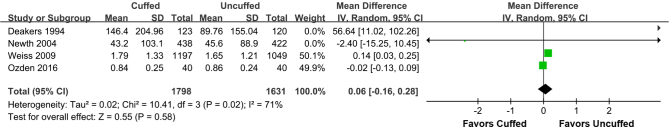
Supplemental Figure 1.
The meta-analysis of duration of intubation between cuffed and uncuffed groups.
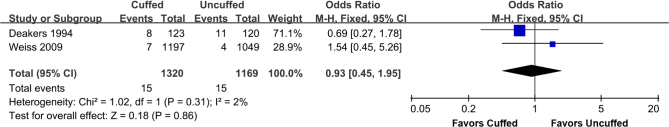
Supplemental Figure 2.
The meta-analysis of accidental extubation between cuffed and uncuffed groups.
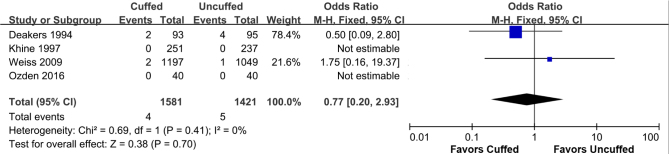
Supplemental Figure 3.
The meta-analysis of tube reintubation between cuffed and uncuffed groups.
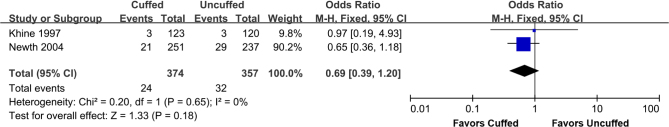
Supplemental Figure 4.
The meta-analysis of racemic epinephrine use between cuffed and uncuffed groups.
Table 2.
The meta-analysis results of peri-procedure parameters.
| Study heterogeneity | ||||||
|---|---|---|---|---|---|---|
| Peri-intubation | OR/WMD (95% CI) | P | df | χ2 | P-Q test | I2 |
| tube change | 0.05 (0.03, 0.07) | <0.00001 | 1 | 0.08 | 0.77 | 0 |
| duration of intubation | 0.02 (-0.13, 0.09) | 0.58 | 3 | 10.41 | 0.02 | 71 |
| accidental extubation | 0.93 (0.45, 1.95) | 0.86 | 1 | 1.02 | 0.31 | 2 |
| reintubation | 0.77 (0.20, 2.93) | 0.7 | 3 | 0.69 | 0.41 | 0 |
Supplemental Figure 5.
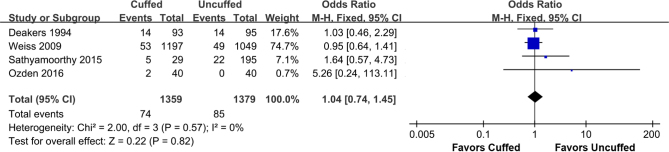
The meta-analysis of croup between cuffed and uncuffed groups.
Supplemental Figure 6.
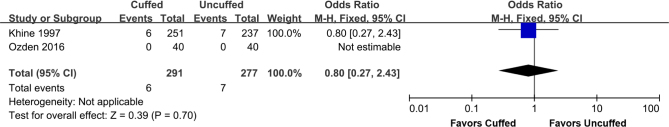
The meta-analysis of stridor between cuffed and uncuffed groups.
Supplemental Figure 7.
The meta-analysis of laryngospasm between cuffed and uncuffed groups.
Table 3.
The meta-analysis results of post-extubation parameters.
| Study heterogeneity | ||||||
|---|---|---|---|---|---|---|
| After extubation | OR/WMD (95% CI) | P | df | χ2 | P-Qtest | I2 |
| racemic epinephrine | 0.69 (0.39, 1.20) | 0.18 | 1 | 0.2 | 0.65 | 0 |
| croup | 0.80 (0.27, 2.43) | 0.7 | NA | NA | NA | NA |
| laryngospasm | 1.27 (0.86, 1.88) | 0.23 | 1 | 0.04 | 0.84 | 0 |
| stridor | 1.04 (0.74, 1.45) | 0.82 | 3 | 2 | 0.57 | 0 |
3.3. Quality Assessment, sensitivity and publication bias analysis
A description of the quality of the included trials was provided in Table 1. All the study quality were relatively high, indicating the reliability of the pooling analysis. As there were less than 5 studies in each comparison, the sensitivity analysis cannot be performed accurately. Publication bias was not assessed using funnel plot as the number of studies in each category was too small to make an appropriate inference.
4. Discussion
This meta-analysis compared the application of cuffed with uncuffed endotracheal tubes among pediatric patients. We found that more patients need tube changes in the uncuffed group than those with cuffed tubes. However, no significant differences were found between the two groups on intubation duration, reintubation occurrence, accidental extubation rate, croup occurrence and racemic epinephrine use during the intubation process. Also we didn’t find any differences on laryngospasm and stridor occurrence after tube extubation.
We are fully aware of a previous meta-analysis which was done on the same topic [4]. The conclusions in the two studies were quite similar, but the parameters analyzed in that article were limited. The outcomes in the current meta-analysis were displayed as peri- and post-procedural. For parameters during procedure, tube change, duration of intubation accidental extubation, tube reintubation and racemic epinephrine use were compared. For post-extubation events, we collected data of the incidence of croup, stridor and laryngospasm. This increased the evidence level of our study. Also, a few studies have been published in recent years. Two more studies were included in this analysis, compared with the previous one.
Endotracheal intubation is a frequent procedure in pediatric emergency and surgery department. The intubation in children may be performed by staff in emergency department, intensive care unit, anesthesia and general pediatric staff [15]. Once the decision for intubation has been made, the choice should be between the cuffed or uncuffed endotracheal tubes [16]. Cuffed tubes provide a leak-proof connection between the patient’s lung and the bag or ventilator without causing undue pressure to laryngeal or tracheal structures [17]. However, an uncuffed endotracheal tube usually causes air leakage or laryngeal injury. The unappropriate size of the tube might be the main cause, leading to an increased number of tube exchanges in these patients [18]. From the pooling analysis we found that patients with uncuffed endotracheal tubes had a higher incidence of tube changes. This is consistent with the previous meta-analysis by Shi et al. [4]. They demonstrated that cuffed tubes may be safely used in children. There was also no significance of post-procedural stridor. Although the conclusion was quite similar between the two studies, our study provided more subjects, indicating a reliable basis.
We then didn’t reveal any significance of duration of intubation. The intubation time should be determined by the disease severity and surgery method. From this point, the option of tube types didn’t affect it. Accidental extubation is a potentially life-threatening event, which leads to emergent, less-controlled endotracheal reintubation [19]. Sometimes, the unwillingness or unconsciousness of the children usually make the intubation failed. The repeated intubations increase the risk of laryngeal or tracheal injury or scarring, pulmonary injury and ventilator-related pneumonia. In this study, both accidental extubation and reintubation between cuffed and uncuffed groups shared no differences. Croup, laryngospasm and stridor are common adverse events occurring after extubation [20,21,22]. Reintubation is needed in serious condition of them. The pooling analysis identified no differences of them between the two groups. Racemic epinephrine is used to produce vasoconstriction which markedly decreases blood flow to capillary beds, especially in the mucosal surfaces [23]. It alleviates the airway resistance, decreasing the risk of respiratory insufficiency and extubation failure.
Also, there were some limitations in this study. First, although it is an updated meta-analysis for the previous one, the number of the included studies was relatively small. This hindered the operation of the sensitivity and publication bias analysis. Second, because of the limited information, not all the peri-intubation and postextubation incidences were recorded. More studies were needed in the future to assist a thorough comparison of cuffed and uncuffed endotracheal tubes application.
Our study demonstrated that uncuffed endotracheal tubes increased the need for tube changes. Other incidences or complications between the two groups had no differences. Cuffed tubes may be an optimal option for pediatric patients. But more trials are needed in the future.
Footnotes
Conflict of interest
Conflict of interest statement: Authors state no conflict of interest
References
- [1].von Rettberg M, Thil E, Genzwurker H, Gernoth C, Hinkelbein J.. Endotracheal tubes in pediatric patients. Published formulas to estimate the optimal size. Anaesthesist. 2011;60(4):334–342. doi: 10.1007/s00101-010-1756-0. [DOI] [PubMed] [Google Scholar]
- [2].Orliaguet GA, Renaud E, Lejay M, Meyer PG, Schmautz E. Telion C and Carli PA. Postal survey of cuffed or uncuffed tracheal tubes used for paediatric tracheal intubation. Paediatr Anaesth. 2001;11(3):277–281. doi: 10.1046/j.1460-9592.2001.00689.x. [DOI] [PubMed] [Google Scholar]
- [3].Tobias JD.. Pediatric airway anatomy may not be what we thought: implications for clinical practice and the use of cuffed endotracheal tubes. Paediatr Anaesth. 2015;25(1):9–19. doi: 10.1111/pan.12528. [DOI] [PubMed] [Google Scholar]
- [4].Shi F, Xiao Y, Xiong W. Zhou Q and Huang X. Cuffed versus uncuffed endotracheal tubes in children: a meta-analysis. J Anesth. 2016;30(1):3–11. doi: 10.1007/s00540-015-2062-4. [DOI] [PubMed] [Google Scholar]
- [5].Knobloch K. Yoon U and Vogt PM. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg. 2011;39(2):91–92. doi: 10.1016/j.jcms.2010.11.001. [DOI] [PubMed] [Google Scholar]
- [6].Moher D, Cook DJ, Eastwood S, Olkin I. Rennie D and Stroup DF. Improving the Quality of Reports of Meta-Analyses of Randomised Controlled Trials: The QUOROM Statement. Onkologie. 2000;23(6):597–602. doi: 10.1159/000055014. [DOI] [PubMed] [Google Scholar]
- [7].Stang A.. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- [8].Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons; 2011. [Google Scholar]
- [9].Ozden ES, Meco BC. Alanoglu Z and Alkis N. Comparison of ProSeal (TM) laryngeal mask airway (PLMA) with cuffed and uncuffed endotracheal tubes in infants. Bosnian Journal of Basic Medical Sciences. 2016;16(4):286–291. doi: 10.17305/bjbms.2016.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Weiss M, Dullenkopf A, Fischer JE, Keller C, Gerber AC.. Prospective randomized controlled multi-centre trial of cuffed or uncuffed endotracheal tubes in small children#. Brit J Anaesth. 2009;103(6):867–873. doi: 10.1093/bja/aep290. [DOI] [PubMed] [Google Scholar]
- [11].Sathyamoorthy M, Lerman J, Asariparampil R, Penman AD, Lakshminrusimha S.. Stridor in Neonates After Using the Microcuff (R) and Uncuffed Tracheal Tubes: A Retrospective Review. Anesth Analg. 2015;121(5):1321–1324. doi: 10.1213/ANE.0000000000000918. [DOI] [PubMed] [Google Scholar]
- [12].Newth C, Rachman B, Patel N, Hammer J.. The use of cuffed versus uncuffed endotracheal tubes in pediatric intensive care. J Pediatr. 2004;144(3):333–337. doi: 10.1016/j.jpeds.2003.12.018. [DOI] [PubMed] [Google Scholar]
- [13].Khine HH, Corddry DH, Kettrick RG, Martin TM, McCloskey JJ, Rose JB, Theroux MC, Zagnoev M.. Comparison of cuffed and uncuffed endotracheal tubes in young children during general anesthesia. Anesthesiology (Hagerstown). 1997;86(3):627–631. doi: 10.1097/00000542-199703000-00015. [DOI] [PubMed] [Google Scholar]
- [14].Deakers TW, Reynolds G, Stretton M, Newth CJL.. Cuffed endotracheal tubes in pediatric intensive care. J Pediatr. 1994;125(1):57–62. doi: 10.1016/s0022-3476(94)70121-0. [DOI] [PubMed] [Google Scholar]
- [15].Bai W, Golmirzaie K, Burke C, Van Veen T, Christensen R, Voepel Lewis T, Malviya S.. Evaluation of emergency pediatric tracheal intubation by pediatric anesthesiologists on inpatient units and the emergency department. Pediatric Anesthesia. 2016;26(4):384–391. doi: 10.1111/pan.12839. [DOI] [PubMed] [Google Scholar]
- [16].De Orange FA, Lemos A, Hall AM, Borges PS. Figueiroa J and Kovatsis PG. Cuffed versus uncuffed endotracheal tubes for general anaesthesia in children aged eight years and under. The Cochrane Library. 2015 doi: 10.1002/14651858.CD011954.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Kriner EJ. Shafazand S and Colice GL. The endotracheal tube cuff-leak test as a predictor for postextubation stridor. Respiratory care. 2005;50(12):1632–1638. [PubMed] [Google Scholar]
- [18].Krishna SG, Hakim M, Sebastian R, Dellinger HL. Tumin D and Tobias JD. Cuffed endotracheal tubes in children: the effect of the size of the cuffed endotracheal tube on intracuff pressure. Pediatric Anesthesia. 2017;27(5):494–500. doi: 10.1111/pan.13099. [DOI] [PubMed] [Google Scholar]
- [19].Da Silva PSL, Reis ME. Aguiar VE and Fonseca MCM. Unplanned extubation in the neonatal ICU: a systematic review, critical appraisal, and evidence-based recommendations. Respiratory care. 2013;58(7):1237–1245. doi: 10.4187/respcare.02164. [DOI] [PubMed] [Google Scholar]
- [20].Koka BV, Jeon IS, Andre JM. MacKAY I and Smith RM. Postintubation croup in children. Anesthesia & Analgesia. 1977;56(4):501–505. doi: 10.1213/00000539-197707000-00008. [DOI] [PubMed] [Google Scholar]
- [21].Flick RP, Wilder RT, Pieper SF, Vankoeverden K, Ellison KM, Marienau ME, Hanson AC, Schroeder DR, Sprung J.. Risk factors for laryngospasm in children during general anesthesia. Pediatric Anesthesia. 2008;18(4):289–296. doi: 10.1111/j.1460-9592.2008.02447.x. [DOI] [PubMed] [Google Scholar]
- [22].Mhanna MJ, Zamel YB. Tichy CM and Super DM. The “air leak” test around the endotracheal tube, as a predictor of postextubation stridor, is age dependent in children. Crit Care Med. 2002;30(12):2639–2643. doi: 10.1097/00003246-200212000-00005. [DOI] [PubMed] [Google Scholar]
- [23].Sathyamoorthy M, Lerman J, Lakshminrusimha S, Feldman D.. Inspiratory stridor after tracheal intubation with a MicroCuff® tracheal tube in three young infants. Anesthesiology: The Journal of the American Society of Anesthesiologists. 2013;118(3):748–750. doi: 10.1097/ALN.0b013e318282cc7a. [DOI] [PubMed] [Google Scholar]