Key Clinical Message
Apples, if indiscriminately consumed without appropriate preventive measures to check erosion, can cause accelerated wear of the teeth.Dentists must be fully aware of the intrinsic and extrinsic factors that cause erosive tooth wear. Management strategy for tooth erosion depends on the severity of erosion, esthetics, function, and patient's preference.
Keywords: Granny Smith Apples, Tooth Erosion, Preventive Management
1. INTRODUCTION
Every individual is unique, so dental treatment requires a certain degree of clinical artistry, but there are certain basic principles that are common to every case. In recent years, dentistry is increasingly being considered as a field of healthcare incorporating science as well as art. It is an established science as its fundamentals are derived from the scientific principles of research, while it is also an art because science cannot always address all the given variables in a particular clinical scenario; hence, it draws from the expertise and personal experiences of the practitioner. The basis of meaningful dental care is therefore provided by a sound understanding of common scientific principles based on research and good clinical observations and deliverance. Consequently, evidence‐based dentistry steps can be utilized to address both these building blocks of dental care. David Sackett laid the foundation of evidence‐based practice by defining it as “integrating individual clinical expertise with the best available external clinical evidence from systemic research.”1
Dental erosion is clinically defined as the progressive and irreversible loss of dental hard tissue caused by a chemical process of acid dissolution that does not involve bacteria.2 It is believed to be caused by extrinsic and intrinsic acids as well as an interplay of physiologic factors such as salivary composition and flow rate, buffering capacity, tooth composition, dental and soft tissue anatomy.3 The Granny Smith apple is an acidic, crisp, green apple with a unique flavor and aroma. It has a pH of 3.2, far more acidic than the pH of 5.5 that is universally acknowledged to be the threshold at which demineralization of the calcific portions of the tooth begins.4, 5
This case report describes a patient who presented with severe dental erosion on the facial and cervical aspects of the teeth. Evidence‐based methods were used to establish the causative agent as well as to formulate a treatment strategy. Although the patient rejected the management strategy presented to him, this case is academically interesting as it establishes the causative agent to be the Granny Smith apple, which is widely consumed but not reported in the literature as yet. This report increases clinicians’ awareness of the harmful acidic effects of Granny Smith apples as well as adding to the existing literature regarding extrinsic causes of dental erosion.
2. CASE DESCRIPTION
A 48‐year‐old male patient attended the clinic complaining of pain in the gum behind the lower second molar. The consent form was obtained from the patient to use clinical information and photographic material of the treatment. The patient did not report any significant medical history, except for a dental history of amalgam fillings 15 years ago. The patient brushed his teeth once daily using a medium bristled brush and a horizontal tooth brushing technique. Upon examination of the oral cavity, the upper third molar opposing the site of the pain appeared to be supra‐erupted, forming abnormal contact with the soft tissue. Radiographic examination (bitewing radiographs in Figure 1 and panoramic radiographs in Figure 2) confirmed the clinical findings. The supra‐erupted upper third molar that formed abnormal contact with the lower gum was determined as the cause of pain in the area. The oral examination also revealed generalized erosion on the facial, cervical (Figure 3), incisal and occlusal (Figure 4) surfaces of the teeth. Heat and cold sensitivity tests revealed normal results indicating that the patient experienced no dentin hypersensitivity. The medical history did not reveal usual suspected causes of erosion.
Figure 1.
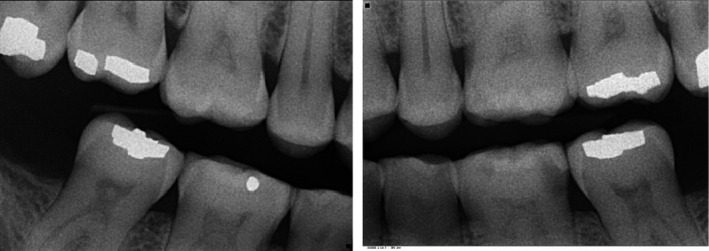
Preoperative bite‐wing radiographs
Figure 2.

Preoperative panoramic radiograph
Figure 3.

Intraoral photographs showing erosion on the cervical and facial aspects of the teeth
Figure 4.
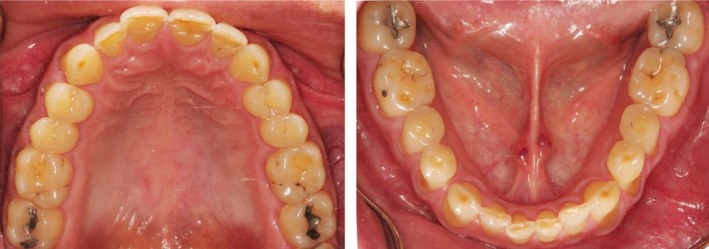
Intraoral photograph showing erosion on the incisal and occlusal aspects of the teeth
The patient was asked to make a diet log for 1 week until the next appointment to determine the extrinsic source of erosion as intrinsic factors were ruled out due to negative medical history (Table 1). Salivary tests were carried out to measure salivary flow, pH, and buffering capacity (Figure 5), revealing normal salivary flow with a decrease in salivary pH and buffering capacity. On examining the diet log at the next appointment, the only dietary agent that was consistently consumed by the patient that had the potential to cause such erosion was Granny Smith apples, which the patient consumed 3‐4 for lunch for the last 10 years.
Table 1.
Diet log (1 wk)
| Breakfast | Lunch | Dinner | Snacks between meals | |
|---|---|---|---|---|
| Sunday | Cappuccino, Cheese sandwich | Four green apples | Grilled chicken sandwich | Corn in a cup |
| Monday | Coffee, egg sandwich | Caesar salad, three green apples | Rice and roasted lamb, Laban | Chocolate |
| Tuesday | Coffee, croissant | Four green apples | Rice and grilled chicken, Laban | ‐ |
| Wednesday | Coffee, Cheese sandwich | Four green apples | Rice and lamb, lamb soup | ‐ |
| Thursday | Coffee, Cheese sandwich | Four green apples | Pizza, garlic bread | Popcorn, Ice‐cream |
| Friday | Scrambled egg, bread, tea | Rice, three green apples | Beef Steak, mashed potato | ‐ |
| Saturday | Bean,bread, tea | Rice, Grilled chicken, Laban (buttermilk), three green apples | Grilled chicken and rice, Salad | French fries |
Figure 5.
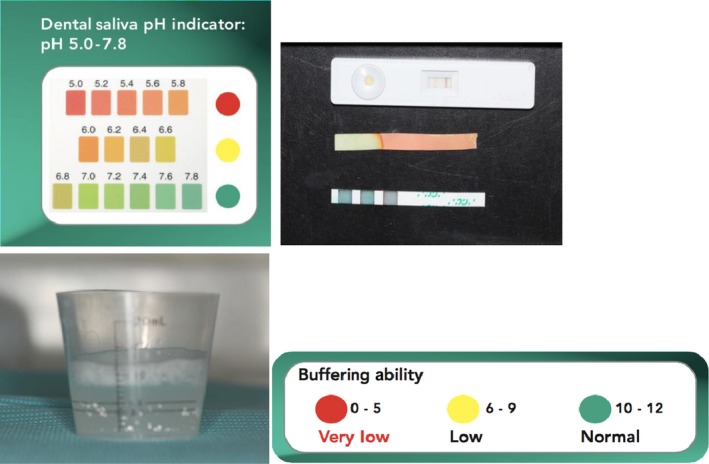
Salivary tests for quantity and pH
3. LITERATURE SEARCH
While following the evidence‐based strategy to deliver the patient care, this present case followed the standard five‐step approach6 to draft an evidence‐based treatment strategy suitable for the needs of the patient. This clinical scenario was converted to the PICO format wherein P refers to the Problem, I refers to the Intervention, C refers to Comparison, and O is the Outcome of the treatment.7, 8 Keeping this in mind, the PICO question that resulted from this clinical scenario was “Whether the teeth with dental erosion (P) should be managed with preventive care (I) or restorative treatment (C) and what will the expected prognosis be (O)?”
With this question in mind, a standard literature search was conducted in PubMed and Google Scholar using keywords for each component of the PICO format as illustrated in Table 2. The search terms were converted into Medical Subject Headings (MeSH) terms where possible. MeSH refers to the controlled vocabulary thesaurus that is developed by the National Library of Medicine that gives uniformity and consistency to the indexing and cataloging of biomedical literature.9 The search revealed one meta‐analysis, two systematic reviews, eight review articles, two in vitro case‐control studies, and two in vitro case studies pertaining to the search terms entered (Table 3).
Table 2.
Search terms or keywords used during literature search
| Pico question | Search terms |
|---|---|
| P | Dental Erosion or Tooth Erosion (MeSH), granny smith apple |
| I | Preventive therapy of tooth erosion, prophylaxis |
| C | Restorative treatment, dental erosion management |
| O | The above search terms revealed what was required to ascertain the outcome of the interventions |
Table 3.
Literature search
| Source of literature | Relevant studies |
|---|---|
| PubMed (http://www.pubmed.gov) and Google Scholar (https://scholar.google.com) |
1 Meta‐analysis
|
2 Systematic Reviews
|
|
7 Review Articles
| |
2 in‐vitro Case‐Control Studies
|
|
2 in‐vitro Case Studies
|
Dental erosion is a widely researched subject and is extensively reported in the literature. According to the Bulletin of the World Health Organization,10 it affects 8%‐13% of the adult population in developing countries and is caused by consumption of acidic beverages. An evidence‐based approach was used through the diagnosis and treatment planning stage as depicted in Figure 6. The causative agent was established at this stage to be the Granny Smith apples after examining the diet log submitted by the patient. The next step was the formulation of a management strategy to contain the erosive process. Bartlett et al11 developed a scoring system for erosive wear of the teeth, where the tooth surface most severely affected by dental erosion is in each sextant recorded based on a four‐point score system. The score is then added to obtain a total which is matched with risk levels to guide the management strategy. This is called the Basic Erosive Wear Examination (BEWE) and it is a simple, reproducible, and transferable scoring system for recording clinical findings and for assisting in the decision making process for the management of erosive tooth wear.11 The BEWE assigns the following scores based on the severity of erosion11: 0—no erosive tooth wear; 1—initial loss of surface texture; 2—distinct defect, hard tissue loss which involves <50% of the surface area (dentin involved); 3—hard tissue loss greater than 50% of the tooth surface.
Figure 6.
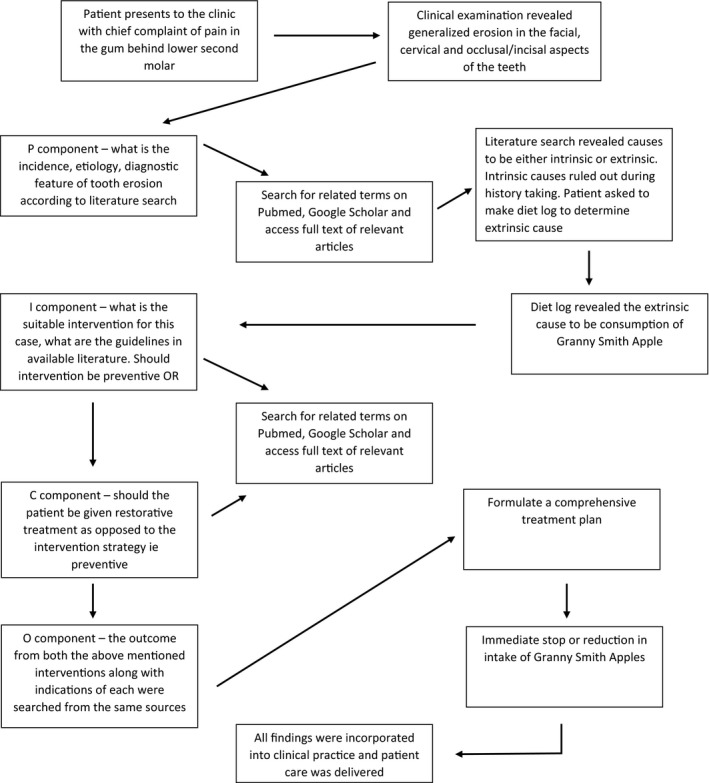
Evidence‐based process used for treatment planning of the present case
Table 4 depicts the management strategies recommended by Bartlett et al based on the cumulative score. According to Wang and Lussi,12 restorative treatment is warranted in case the affected surfaces are compromised to the degree that: the structural integrity of the tooth is threatened; the exposed dentin is hypersensitive; erosive defect is esthetically unacceptable to the patient; or the defect is so deep that it may result in pulpal exposure. Davies et al11 further recommend that active treatment with restorations is only necessary in cases of noncarious tooth surface loss, when there is concern regarding one or more of the following factors: esthetics, sensitivity, function, or space loss in vertical dimension. Based on these recommendations and information obtained from the patient, a treatment plan was formulated.
Table 4.
Risk levels as a guide to clinical management (adapted from Bartlett et al)11
| Risk Level | Cumulative Score of all Sextants | Management |
|---|---|---|
| None | Less than or equal to 2 |
|
| Low | Between 3 and 8 |
|
| Medium | Between 9 and 13 |
|
| High | 14 and above |
|
4. EVIDENCE‐BASED TREATMENT PLAN AND MANAGEMENT
At the next appointment, the patient's BEWE score was recorded (Table 5) and risk levels were assessed. Based on the examination, the patient fell under low risk which did not require active/restorative treatment. Furthermore, the absence of sensitivity and patient's satisfaction with the appearance and function of his teeth did not require any restorative treatment because the teeth were not visible upon smiling (Figure 6). The supra‐erupted third molars were extracted (Figure 7A), and the proximal surface of the lower left first molar was restored using composite resin (Figure 7B). Topical application of fluoride was performed on all the teeth (Figure 7C). The patient was counseled with regard to his diet and oral hygiene to reduce his intake of the acidic agent, that is, the Granny Smith apple, to follow up any exposure to an acidic agent with milk or cheese, use a straw to drink any acidic beverage, use a medium to soft bristled toothbrush, and avoid brushing too hard.
Table 5.
Pre‐treatment Basic Erosive Wear Examination (BEWE) score of the patient
| Sextant | Score |
|---|---|
| Sextant 1 (17‐14) | 1 |
| Sextant 2 (13‐23) | 2 |
| Sextant 3 (24‐27) | 1 |
| Sextant 4 (37‐35) | 1 |
| Sextant 5 (34‐44) | 2 |
| Sextant 6 (45‐47) | 1 |
| Total | 8 |
Figure 7.
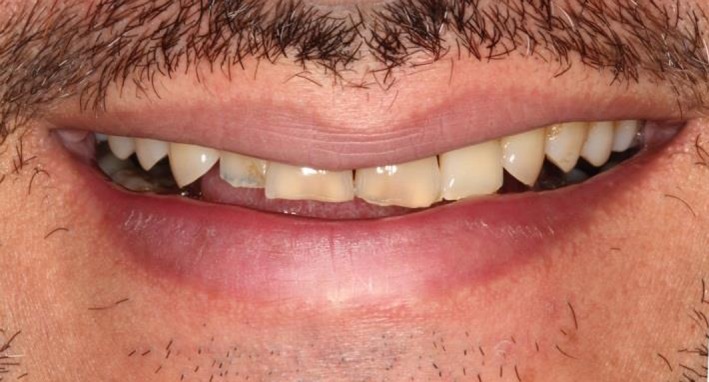
Patient's teeth hardly visible upon smiling
Figure 8.

A, Postoperative bite‐wing radiograph showing proximal restoration. B, Fluoride application on the teeth
5. FOLLOW‐UP AND PROGNOSIS
The patient was recalled for a follow‐up visit after 12 months, the examination revealed extrinsic staining on the teeth (Figure 9), indicating a reduced intake of the erosive agent, that is, Granny Smith apple. Discussion with the patient confirmed that he had reduced his consumption of apples and was following the diet and oral hygiene advice. Dental prophylaxis was performed on the extrinsically stained teeth, and the patient was prescribed a night guard (Figure 10). The teeth were scored again using the BEWE index and assessed for risk levels (Table 6). The examination revealed a consistent total score and risk level highlighting the positive maintenance of the erosive condition.
Figure 9.

Post‐treatment photograph at follow‐up after 1 year showing extrinsic staining of teeth
Figure 10.

After dental prophylaxis and insertion of night guard at the 1‐year follow‐up appointment
Table 6.
BEWE score of the patient at 1 year follow‐up appointment
| Sextant | Score |
|---|---|
| Sextant 1 (17‐14) | 1 |
| Sextant 2 (13‐23) | 2 |
| Sextant 3 (24‐27) | 1 |
| Sextant 4 (37‐35) | 1 |
| Sextant 5 (34‐44) | 2 |
| Sextant 6 (45‐47) | 1 |
| Total | 8 |
6. CONCLUSION
The relationship between certain dietary factors and dental erosion is well established. Apples, if indiscriminately consumed without appropriate preventive measures to check erosion, can cause accelerated wear of the teeth. As in the present case, dental erosion is usually a chance encounter in the clinic and seldom presented by the patient unless there is some debilitation involved. Severe erosion can lead to dentin hypersensitivity, pulpal involvement, unpleasant appearance, as well as loss of function in advanced cases. The dentist must be familiar with the identification, causes, and management strategies pertaining to noncarious tooth wear in general and dental erosion in particular. Evidence‐based decision making is crucial for delivering quality dental care, equipping the practitioner with the necessary theoretical knowledge and allowing them to make decisions based on the established guidelines and treatment protocols as well as on the latest advancements in techniques and practice methodologies.
CONFLICT OF INTEREST
The author declares that there is no conflict of interest regarding the publication of this manuscript.
AUTHORSHIP
Al Anazi EZ: diagnosed the case, patient management, took photos and wrote the manuscript.
Al Anazi EZ. Dental erosion caused by Granny Smith apples: An evidence‐based case report and 1‐year follow‐up. Clin Case Rep. 2018;6:1689–1696. 10.1002/ccr3.1702
REFERENCES
- 1. Somaraj V, Shenoy RP, Panchmal GS, Jodalli P, Sonde S. Evidence based dental practice: a review. J Appl Med Dent Sci. 2016;1:112‐121. [Google Scholar]
- 2. Ganss C. Definition of erosion and links to tooth wear. Monogr Oral Sci. 2006;20:9‐16. [DOI] [PubMed] [Google Scholar]
- 3. Lussi A, Jaeggi T, Zero D. The role of diet in the aetiology of dental erosion. Caries Res. 2006;38:134‐144. [DOI] [PubMed] [Google Scholar]
- 4. Fejerskov O, Kidd E. Dental Caries: the disease and its clinical management, 2nd edn Oxford: Blackwell Munksgaard; 2008. [Google Scholar]
- 5. Touyz LZG. Demystifying apples in health and dentistry. Dent Health Curr Res. 2016;2:1. [Google Scholar]
- 6. Al Hazzani SA. Use of evidence‐based decision‐making in comprehensive dental treatment of a patient with meth mouth‐a case report. J Evid Based Dent Pract. 2017;17:92‐98. [DOI] [PubMed] [Google Scholar]
- 7. Forest JL, Miller SA, Overman PR, Newman MG. Evidence‐based decision making: a translational guide for dental professionals. Philadelphia, PA: Lippincott Williams & Wilkins; 2009:1‐5, 15‐22. [Google Scholar]
- 8. Sackett DL, Strauss SE, Richardson WS, Rosenberg W, Haynes RB. Evidence‐based medicine: how to practice and teach EBM. Edinburgh: Churchill Livingstone; 2000:3‐4, 15‐27. [Google Scholar]
- 9. https://www.nlm.nih.gov/bsd/disted/meshtutorial/introduction/02.html. Accessed Last reviewed: 09 May 2018.
- 10. Erik PP, Denis B, Hiroshi O, Saskia E‐D, Charlotte N. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83:661‐669. [PMC free article] [PubMed] [Google Scholar]
- 11. Bartlett D, Ganss C, Lussi A. Basic Erosive Wear Examination (BEWE): a new scoring system for scientific and clinical needs. Clin Oral Investig. 2008;12:S65‐S68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wang X, Lussi A. Assessment and management of dental erosion. Dent Clin North Am. 2010;54:565‐578. [DOI] [PubMed] [Google Scholar]


