Abstract
Objectives
To identify aspects of medication management that are associated with a greater risk of hospital readmission.
Patients and Methods
We conducted a prospective cohort study, with a thorough medication history and reconciliation performed at admission and discharge. Patients 18 years or older (N=258) were prospectively enrolled on admission to a cardiology service at a tertiary care hospital from September 1, 2011, through July 31, 2012. All patients received their hospital and outpatient care within our institution, which minimized loss to follow-up. Readmission rates within 30 days and 6 months after discharge were recorded and used to investigate associations with specific characteristics related to medication regimen and management. Nominal logistic fit tests were used to establish associations with risk factors.
Results
A higher risk of readmission within 30 days after discharge was seen with heart failure diagnosis (P=.003) and with increased severity of comorbid conditions based on Charlson score (P=.02). Patients whose family managed their medications entirely had a higher risk of readmission at 30 days (odds ratio, 2.92; 95% CI, 1.25-5.6; P=.01) and at 6 months (odds ratio, 3.54; 95% CI, 1.70-7.65; P<.001). These findings were independent of the presence of heart failure.
Conclusion
Patients requiring family member support with medication management should be considered at increased risk for readmission. Increased focus on these patients at discharge may help decrease readmissions.
Abbreviations and Acronyms: CAD, coronary artery disease; HF, heart failure; OR, odds ratio; PADE, potential adverse drug event
Hospital readmissions are costly. It has been estimated that Medicare alone spends $26 billion annually on readmitted patients and that $17 billion might be avoided with appropriate care.1 The Affordable Care Act of 2010 authorized the Hospital Readmission Reduction Program, which created penalties for hospitals with excess readmissions of patients with a principal diagnosis of heart failure (HF), myocardial infarction, or pneumonia beginning October 1, 2012. The program expanded to include chronic obstructive lung disease and total artificial hip and knee arthroplasty in fiscal year 2015 and coronary artery bypass grafting in fiscal year 2017.2
The immediate post–hospital discharge period can be overwhelming for patients as they physically recover and assume responsibility for managing new long-term health problems, with potentially new or complex medication regimens. Several initiatives—Better Outcomes by Optimizing Safe Transitions,3 Re-Engineered Discharge,4 Hospital to Home,5 State Action on Avoidable Rehospitalizations,6 and Patient-Centered Medical Home,7—emphasize the importance of both a coordinated transition of care from the hospital to the home environment and identification of adequate community resources to meet patients' needs after discharge.
Other strategies for strengthening the quality of care in the home environment focus on early clinical follow-up and health education for patients and their families or caregivers. Pivotal topics to address with these interactions include improving understanding of the role and importance of medications, overcoming other barriers to medication adherence such as access and cost, and arranging additional help managing medications at home if needed.8, 9, 10, 11, 12
Medication reconciliation, the process of establishing an accurate list of the patient's home medications at care transitions, has been emphasized as an important tool available to pharmacists and other health care professionals in their effort to optimize treatment.13 We believe that the process of medication reconciliation also provides an excellent opportunity for health care professionals to gather important information about patients' health literacy, medication adherence, and ability to understand and manage the prescribed medical regimen. The goal of this study was to determine whether factors related to home medication management before hospital admission to a medical cardiology service are associated with early readmission.
Patients and Methods
Patient Screening and Enrollment
Patients admitted to a medical cardiology service at Mayo Clinic Hospital, Saint Marys Campus, in Rochester, Minnesota, from September 1, 2011, through July 31, 2012, were prospectively considered for enrollment. Included patients were at least 18 years old, fluent in English, and received most of their medical care from Mayo Clinic providers because their primary care physicians were members of the Mayo Clinic staff. Patients were excluded if they were unable to understand or answer questions because of medical conditions, were residents of long-term care facilities, had professional home health care, or were not available for interview within 48 hours of admission. For each patient, only the index admission (first admission within the time frame of our study) prompted an interview and was counted as a case. Subsequent admissions within the 6 months following the index admission were counted as readmissions. Informed consent was obtained from all participants. The study was approved by the Mayo Clinic Institutional Review Board (IRB#11-005326).
Demographic Characteristics and Diagnoses
Demographic and clinical data were obtained for all patients, including age, sex, duration of hospital stay, number of admissions in the previous 12 months, living arrangements before admission, admission diagnoses, and living arrangements after dismissal. Patients who were admitted for acute coronary syndrome or HF were specifically noted because these are cardiac-related, Medicare-targeted populations. Patients admitted with other diagnoses (mostly arrhythmias) were placed in a third category. The Charlson comorbidity index14 was calculated using an online tool (available at: http://www.soapnote.org/elder-care/charlson-comorbidity-index).15 We recorded any previous diagnoses of coronary artery disease (CAD) or HF in the patient's medical history, regardless of the admission diagnosis.
Medication Management Strategies and Health Literacy
A structured interview was conducted during the first 48 hours of hospitalization to assess patients' home medication management strategies (eg, use of pillbox or other aid), medication adherence, and health literacy. Family involvement in medication management was specifically assessed and categorized as (1) no assistance (self-managed), (2) family members participated in medication management (family helped), or (3) family members handled all the medications for patients (family handled all). Of note, some patients had help from nonprofessional, non–family members, but all were categorized and referred to as family help. Health literacy was assessed using a short assessment tool: 3 questions, 3-part Likert scale, score ranging from 3 (highest health literacy) to 9 (lowest health literacy), based on work by Chew et al.16
Medication History and Reconciliation
Admission Medication Reconciliation
The home medications of all patients were reviewed by 1 of 2 hospital pharmacists (M.P.D.M., J.M.L.). We noted the source of the patient's medication information as: pill bottles, pillbox, written list, patient's recollection, family's recollection, or patient's outpatient pharmacy records. All discrepancies between sources were noted. The number of prescribed scheduled (including aspirin) and as-needed medications was recorded. Patients were questioned about discrepancies between reported medication use, pharmacy prescription refills, and prescribed medications. If there had been no documented prescriber-initiated change in medication or dose, the discrepancy was attributed to patient “possible nonadherence” (if adherence was uncertain from the interview) or “nonadherence.”
The updated home medication list was compared with the hospital admission medications. All discrepancies were defined as potential adverse drug events (PADEs) and characterized by the reviewing pharmacist as intentional, unintentional, or unknown based on a review of the admitting physician records. Clarification of admitting physician intent was obtained for discrepancies through personal communication. All unintentional discrepancies were classified independently by 2 pharmacists (M.P.D.M., J.M.L.) using the National Coordinating Council for Medication Error Reporting and Prevention algorithm17 and were assigned a severity from A to I. When classifications differed, consensus was achieved after joint review.
Discharge Medication Reconciliation
Dismissal instructions were examined to determine if accurate instructions regarding changes to the original home medications list were included (eg, new/modified/stopped medications). Any unexplained discrepancies between the dismissal medications and earlier lists were scored using the National Coordinating Council for Medication Error Reporting and Prevention algorithm.17
Postdischarge Outcomes: Death and Hospital Readmission
Patients' integrated inpatient and outpatient electronic medical records were reviewed to determine subsequent readmissions or death within 30 days after discharge from the index admission and within 6 months after discharge. The primary reason for all readmissions was recorded and classified as “same as” or “unrelated to” the reason for the primary admission.
Statistical Analyses
Study data were collected and managed using REDCap (Research Electronic Data Capture) electronic data capture tools hosted at Mayo Clinic (National Center for Advancing Translational Sciences grant UL1 TR000135).18 Data were analyzed using JMP 9 statistical software (SAS Institute).
Nominal logistic fit tests were performed to establish associations between risk factors and adverse outcomes (readmission or death) within 30 days and 6 months postdischarge from the index admission. A value of P<.05 was considered statistically significant.
The effects of risk factors (Charlson score >3, diagnosis of HF, family handling all medications or helping with medications, 3 or more admissions in the previous 12 months) were modeled using logistic regression to predict readmission within 30 days and 6 months after the date of discharge from index admission. Goodness of fit of the logistic models was calculated using the C statistic for both equations. Kaplan-Meier curves were plotted for number of days to readmission for selected subpopulations.
Results
Population Description
Of 428 patients screened, 170 were excluded: 33 were residents of a long-term care facility, 5 required a translator, 18 were unable to answer questions because of altered mental status or intubation, 39 declined participation, and 75 were unavailable for interview because of short stay or procedure. Among the 258 patients enrolled in the study, acute coronary syndrome, CAD, and HF were the admitting diagnoses in more than half. The patient group was generally elderly (median age, 70.5 years) (Table 1).
Table 1.
| Characteristic | Value |
|---|---|
| Men | 135 (52) |
| Age (y) | 70.5 (58-81) |
| Duration of hospitalization (d) | 2 (1-4) |
| Admission diagnosis | |
| Acute coronary syndrome | 89 (35) |
| HF | 41 (16) |
| Other cardiac diagnosis | 128 (50) |
| Charlson comorbidity index | 4 (2-5) |
| Comorbid conditionsc | |
| CAD alone | 90 (35) |
| HF alone | 43 (17) |
| CAD and HF | 59 (23) |
| Neither CAD nor HF | 66 (25) |
| Handling medications at home | |
| Self-managed | 175 (68) |
| Family or friend helped | 48 (19) |
| Family handled all medications | 35 (14) |
| Pillbox use | 170 (66) |
| Scheduled home prescriptions | 7.5 (5-10) |
| Health literacy score | 4 (3-5) |
| Self-reported adherence | 213 (83) |
CAD = coronary artery disease; HF = heart failure.
Data are presented as No. (percentage) of patients or median (interquartile range).
CAD and HF were identified by established diagnoses in medical records; other comorbid conditions were not emphasized because they were not targeted by Medicare.
Handling Medications at Home
The median number of scheduled, prescribed medications was 7.5 (interquartile range, 5-10). Self-reported medication adherence was high (83% [213 of the 258 patients]). Medication nonadherence did not significantly affect readmission rates (P=.39 at 30 days, P=.50 at 6 months). Most patients (175 [68%]) handled their medications with no help (self-managed), 48 (19%) participated in their medication management while receiving some help (family helped), and 35 (14%) received family assistance for all aspects of their medication management (family handled all medications). Health literacy assessed using the Chew protocol16 varied among patients (median score, 4 [on a scale of 3-9]). A pillbox was used by 170 patients (66%) to facilitate medication adherence (Table 1).
Potential Adverse Drug Events
On admission, discrepancies were found in 156 of our 258 patients' records (60%). These discrepancies translated into errors in written orders on admission for 45% (116 patients) of our patients (some patients had more than 1 type of error): 11% (29 patients) type B errors (error did not reach the patient); 37% (96 patients) type C errors (reached the patient but did not cause harm); and 7% (17 patients) type D errors (required additional monitoring). We did not observe any errors more serious than type D.
Nominal logistic fit tests revealed associations between PADEs and higher number of prescriptions (odds ratio [OR], 1.13 per additional prescription; 95% CI, 1.06-1.21; P<.001), higher Charlson index score (OR, 1.19 per 1-unit score increase; 95% CI, 1.05-1.35; P<.005). In the logistic regression models, both the number of prescriptions and the Charlson index score were parameterized per units as continuous variables.
In all, 51 of our 256 patients (20%; 2 patients died during index admission) had errors in the medication lists they were given as part of their dismissal instructions. Among those, type C errors (reached patients) occurred in 37 patients (14%), and type D errors (reached patients, likely to cause adverse effects) were found in 17 patients (7%). We were unable to capture type B errors on dismissal because the medical record reviews took place retrospectively (ie, after dismissal). On nominal logistic fit tests, a PADE on the discharge medication list was associated with the number of prescriptions (OR, 1.08 per additional prescription; 95% CI, 1.01-1.16; P=.03) and higher Charlson index score (OR, 1.2 per 1-unit score increase; 95% CI, 1.08-1.45; P=.002).
Diagnoses and Outcomes Within 30 Days and 6 Months
Among our 258 patients, 2 died during the index admission. The number of deaths overall was 6 (2%) at 30 days and 15 (6%) at 6 months; the numbers were too small for statistical analysis.
Rates of readmission overall were 17% (44 of 258) within 30 days of dismissal and 38% (98 of 258) within 6 months of dismissal. We compared readmission rates within 30 days after discharge across patient groups with previous diagnoses of HF, CAD, both, or neither. We observed a significantly higher readmission rate for patients with both CAD and HF compared with the other groups within 30 days of discharge (29% readmission rate [17 of 59 patients]; P=.01) and within 6 months of discharge (56% readmission rate [33 of 59]; P=.001) (Table 2). However, the reason for the index admission (as indicated by the primary admission diagnosis in the medical record) did not affect readmission rate (data not shown). Health literacy, use of a pillbox (P=.17 at 30 days, P=.06 at 6 months) or other aid (P=.51 at 30 days, and P=.38 at 6 months), and presence of a PADE on admission (P=.44 at 30 days, and P=.45 at 6 months) or at discharge (P=.73 at 30 days, and P=.14 at 6 months) were not related to 30-day or 6-month readmission rates (P=.51 at 30 days, and P=.38 at 6 months).
Table 2.
| Readmission | Total (N=258) | Comorbid condition |
P valuec | |||
|---|---|---|---|---|---|---|
| HF (n=43) | CAD (n=90) | Both (n=59) | Neither (n=66) | |||
| 30 Days | 44 (17) | 9 (21) | 13 (14) | 17 (29) | 5 (8) | .01 |
| 6 Months | 98 (38) | 18 (42) | 33 (37) | 33 (56) | 14 (21) | .001 |
CAD = coronary artery disease; HF = heart failure.
Data are presented as No. (percentage) of patients readmitted.
P values were calculated for differences in readmission rates between comorbid condition groups either within 30 days after discharge date or within 6 months after discharge date.
Family Helping With Medication Management
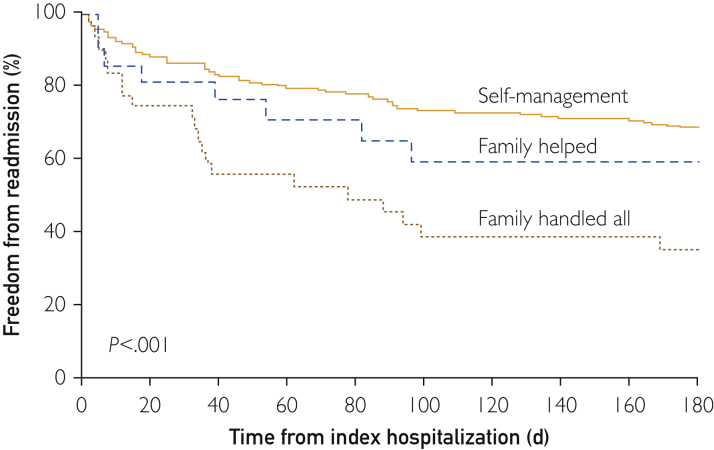
Patients who received help managing their medications at home had a higher readmission rate than patients managing their medications on their own. As early as 30 days after discharge, patients whose family handled all medication needs had a higher readmission rate (11 out of 35 patients [31%]) than patients requiring some help from family for their medication management (11 out of 48 patients [23%]) and patients managing their medications on their own (25 out of 175 patients [14%]) (P=.04). Within 6 months of discharge, the rate of readmission for patients not able to participate in their medication management was 63% (22 out of 35 patients), significantly higher than for patients requiring some help (24 out of 48 patients [50%]) and patients able to manage their medications on their own (56 out of 175 patients [32%]; P<.002). The Figure depicts the readmission pattern for the 3 medication management strategies over the 6-month follow-up.
Figure.
Kaplan-Meier curves showing freedom from readmission stratified by medication management (percentage of patients): no help, some family help with medication management, and family helping with all medication management.
Logistic Fit Analysis
The nominal logistic fit test revealed an association between readmission within 30 days and high Charlson index score (calculated per unit increase, P=.02), diagnosis of HF (P=.003), and family handling all medications (P=.01) (Table 3). The family handling all medications group was compared with the patient handling medications alone group. Using this methodology, readmission within 6 months was associated with high Charlson index score (calculated per unit increase, P=.002), HF diagnosis (P=.001), family handling all medications (P<.001), high number of scheduled prescriptions (calculated per unit increase, P<.001), and a high number of admissions in the previous 12 months (calculated per unit increase, P<.001).
Table 3.
| Risk factor | 30 Days (n=44) |
6 Months (n=98) |
||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Age (per year) | 1 (0.99-1.03) | .47 | 1.00 (0.99-1.02) | .56 |
| Admission diagnosisc | .86 | .29 | ||
| HF vs other | 1.2 (0.47-2.88) | .69 | 1.71 (0.83-3.50) | .14 |
| ACS vs other | 0.92 (0.44-1.91) | .83 | 1.34 (0.77-2.35) | .30 |
| Charlson index score | 1.19 (1.03-1.39) | .02 | 1.22 (1.08-1.38) | .002 |
| HF diagnosisd | 2.67 (1.38-5.26) | .003 | 2.32 (1.39-3.90) | .001 |
| Medications handlinge | .04 | .002 | ||
| Family handles all | 2.92 (1.25-5.6) | .01 | 3.54 (1.70-7.65) | <.001 |
| Family helps | 1.79 (0.56-4.97) | .3 | 2.09 (0.85-5.13) | .10 |
| Health literacy score | 1.15 (0.94-1.38) | .17 | 1.16 (0.99-1.37) | .06 |
| No. of scheduled prescriptions (per drug) | 1.05 (0.97-1.14) | .19 | 1.14 (1.07-1.23) | <.001 |
| Presence of discharge PADE | 1.15 (0.50-2.44) | .73 | 1.59 (0.86-2.93) | .14 |
| No. of admissions in previous 12 mo (per admission) | 1.14 (0.94-1.37) | .18 | 1.50 (1.24-1.85) | <.001 |
| Adherencef | 1.72 (0.46-5.22) | .39 | 0.69 (0.21-1.94) | .50 |
ACS = acute coronary syndrome; HF = heart failure; OR = odds ratio; PADE = potential adverse drug event.
Analyses were calculated per unit increase for the parameters: age, Charlson index score, health literacy score, No. of prescribed medications, No. of admissions in previous 12 months.
Admission diagnoses divided in 3 groups: heart failure, acute coronary syndrome, and other. Heart failure and acute coronary syndrome groups were each compared to other.
Heart failure pertains to the presence of the comorbidity, regardless of the admission diagnosis.
Medication handling was divided in 3 groups: patients handling their medications on their own (no help; reference group), family helping patients (patient still participates), and family handling all medications (patient unable to handle any of the medications). Family helping and family handling all medications groups were compared to the reference group.
The numbers for nonadherent and doubtful adherent were very small and did not reach statistical significance. Results of readmission (30 days or 6 months) of nonadherent vs adherent.
Based on the nominal logistic fit tests for readmission within 30 days and 6 months after discharge from index admission, we modeled the effect of these factors to predict readmission risk at 30 days or 6 months (Supplemental Appendix S1, available online at http://mcpiqojournal.org/). Multifactorial modeling showed that an HF diagnosis (OR, 2.67; 95% CI, 1.38-5.26; P=.003) and family handling all medications (OR, 2.92; 95% CI, 1.25-5.6; P=.01) carried the highest risk of readmission within 30 days of discharge. Highest readmission rates within 6 months of discharge were associated with an HF diagnosis (OR, 2.32; 95% CI, 1.39-3.90; P=.001), higher Charlson index score (OR, 1.22; 95% CI, 1.08-1.38; P=.002), and family handling all medications (OR, 3.54; 95% CI, 1.70-7.65; P<.001).
Discussion
Our study found a higher rate of hospital readmission among patients receiving help at home for their medication management. Our patient cohort, admitted to a medical cardiology service, was elderly (mean age, 70.5 years) and had substantial comorbid conditions (median Charlson comorbidity index score of 4). One-third of the study cohort required some or complete assistance with medication management before admission. Although a diagnosis of HF was common in this group and associated with a higher risk of early readmission, the increased risk of readmission associated with receiving assistance at home with medications management was independent of the HF diagnosis. Other factors associated with higher risk of early readmission were number of prescribed, scheduled medications and frequent past admissions.
Medication nonadherence was present in 17% of patients (45 of 258) but did not appear to affect readmissions in our study. Patients in this nonadherent group were typically younger than our average patients and had fewer comorbid conditions. The complexity of medication programs also was associated with a high percentage of discrepancies in medical records. A possible explanation for these discrepancies is that changes to the medical regimen, either by a health care professional or by patients on their own, are not documented in real time. These discrepancies led to errors by the medical teams in medication management at both admission and dismissal. These errors, although disturbing, were not related to the readmission rate.
The reason for higher readmission rates among patients receiving help with medications was not evaluated in this study. Patients' families are often in the best position to judge the mental and physical ability of the patient to carry out the complex tasks of home health care. One possible explanation for the higher rate of admissions in these patients is that the family's involvement may be a marker for frailty or subtle cognitive decline. The usual measures of frailty, cognitive capability, and health status are more complex, and a standardized definition of frailty has been elusive.19, 20 Each of these factors has been associated with increased risk of hospitalization.19, 21, 22 A recent study23 used the Mini-Cog test as a simplified tool for assessment of cognitive decline in patients with HF and found an association between poor performance on that test and an increased risk of early readmission. Patients with limited ability to manage medications may have similar limitations regarding other common home tasks such as daily weight measurement, dietary restrictions, and reporting of adverse changes in symptoms to their health care professionals. Regardless of the underlying reasons for the decision of families to assist with medication management, our assessment tool was simple, easy to use at hospital admission, and nonthreatening to the patient.
This study had several limitations. It encompassed a small population of patients who primarily received their care within our health care system to ensure complete follow-up. Participation in the study was voluntary. We also excluded patients who could not understand our questions, either because of confusion or a language barrier. Thus, through various methods, we may have narrowed the scope of our results and may have limited their application to other populations. In addition, we categorized patients as receiving help from family or caregivers or not receiving this form of help. Thus, potentially important subsets of patients may not have been captured, such as patients who need help with medications but for whom help is unavailable or unused.
Conclusion
With our simple assessment, help with medication management appears to be strongly associated with higher risk of readmission. The help received from family might only be a marker for subtle cognitive decline or increased frailty, but documenting its presence would allow for better identification of patients requiring additional follow-up in the community. Further evaluation of this measure in broader populations and to include more precise categories of patients is indicated.
Acknowledgments
We thank Dana Gerberi for help with literature searches and Drs Julie Cunningham and Michael Gharacholou for their comments on the submitted manuscript.
The sponsor had no role in the design, methods, recruitment, data collections, analysis, and preparation of the submitted manuscript. The contents of the article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Footnotes
Grant Support: This work was supported by an intramural grant from Pharmacy Services, Mayo Clinic, and by grant UL1 TR000135 from the National Center for Advancing Translational Sciences for statistical analyses.
Potential Competing Interests: The authors report no competing interests.
Supplemental Online Material
Supplemental material can be found online at http://mcpiqojournal.org/. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
References
- 1.Goodman D.C., Fisher E.S., Chang C.-H. The revolving door: a report on U.S. hospital readmissions; an analysis of Medicare data by the Dartmouth Atlas Project; stories from patients and health care providers by PerryUndem Research & Communication. http://www.rwjf.org/content/dam/farm/reports/reports/2013/rwjf404178 Robert Wood Johnson Foundation website. Published February 2013. Accessed April 20, 2015.
- 2.Centers for Medicare and Medicaid Services Readmissions Reduction Program (HRRP) https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html Centers for Medicare and Medicaid Services website. Updated April 18, 2016. Accessed September 4, 2017.
- 3.Project BOOST Team. The Society of Hospital Medicine Care Transitions Implementation Guide: Project BOOST: Better Outcomes by Optimizing Safe Transitions. http://www.hospitalmedicine.org Society of Hospital Medicine website. Published December 2013. Accessed April 20, 2015.
- 4.Agency for Healthcare Research and Quality Re-Engineered Discharge (RED) Toolkit. http://www.ahrq.gov/professionals/systems/hospital/red/toolkit/index.html Agency for Healthcare Research and Quality website. Published March 2013. Updated May 2017. Accessed April 20, 2015.
- 5.American College of Cardiology Hospital to home. http://cvquality.acc.org/Initiatives/H2H.aspx American College of Cardiology website. Accessed July 15, 2015.
- 6.Rutherford P., Nielsen G.A., Taylor J., Bradke P., Coleman E. How-to guide: improving transitions from the hospital to community settings to reduce avoidable rehospitalizations. http://www.ihi.org/resources/Pages/Tools/HowtoGuideImprovingTransitionstoReduceAvoidableRehospitalizations.aspx Institute for Healthcare Improvement website. Published June 2013. Accessed April 20, 2015.
- 7.Peikes D., Zutshi A., Genevro J.L., Parchman M.L., Meyers D.S. Early evaluations of the medical home: building on a promising start. Am J Manag Care. 2012;18(2):105–116. [PubMed] [Google Scholar]
- 8.Viswanathan M., Golin C.E., Jones C.D., et al. Medication adherence interventions: comparative effectiveness: closing the quality gap: revisiting the state of the science. Evidence Report No. 208. AHRQ Publication No. 12-E010-EF. http://www.effectivehealthcare.ahrq.gov/ehc/products/296/1248/EvidenceReport208_CQGMedAdherence_FinalReport_20120905.pdf Agency for Healthcare Research and Quality website. Published September 11, 2012. Accessed April 20, 2015. [PMC free article] [PubMed]
- 9.Hope C.J., Wu J., Tu W., Young J., Murray M.D. Association of medication adherence, knowledge, and skills with emergency department visits by adults 50 years or older with congestive heart failure. Am J Health Syst Pharm. 2004;61(19):2043–2049. doi: 10.1093/ajhp/61.19.2043. [DOI] [PubMed] [Google Scholar]
- 10.Murray M.D., Tu W., Wu J., Morrow D., Smith F., Brater D.C. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther. 2009;85(6):651–658. doi: 10.1038/clpt.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Retrum J.H., Boggs J., Hersh A., et al. Patient-identified factors related to heart failure readmissions. Circ Cardiovasc Qual Outcomes. 2013;6(2):171–177. doi: 10.1161/CIRCOUTCOMES.112.967356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marvanova M., Roumie C.L., Eden S.K., Cawthon C., Schnipper J.L., Kripalani S. Health literacy and medication understanding among hospitalized adults. J Hosp Med. 2011;6(9):488–493. doi: 10.1002/jhm.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boockvar K.S., Blum S., Kugler A., et al. Effect of admission medication reconciliation on adverse drug events from admission medication changes. Arch Intern Med. 2011;171(9):860–861. doi: 10.1001/archinternmed.2011.163. [DOI] [PubMed] [Google Scholar]
- 14.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 15.Morgan M. Charlson comorbidity index. http://www.soapnote.org/elder-care/charlson-comorbidity-index SOAPnote Project website. Accessed August 15, 2011.
- 16.Chew L.D., Bradley K.A., Boyko E.J. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594. [PubMed] [Google Scholar]
- 17.National Coordinating Council for Medication Error Reporting and Prevention NCC MERP Index for Categorizing Medication Errors. http://www.nccmerp.org/sites/default/files/indexColor2001-06-12.pdf National Coordinating Council for Medication Error Reporting and Prevention website. Published 2001. Accessed April 20, 2015. [DOI] [PubMed]
- 18.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fried L.P., Tangen C.M., Walston J., et al. Cardiovascular Health Study Collaborative Research Group Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 20.Nasreddine Z.S., Phillips N.A., Bédirian V., et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 21.Singh M., Stewart R., White H. Importance of frailty in patients with cardiovascular disease. Eur Heart J. 2014;35(26):1726–1731. doi: 10.1093/eurheartj/ehu197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uchmanowicz I., Łoboz-Rudnicka M., Szelag P., Jankowska-Polañska B., Łoboz-Grudzieñ K. Frailty in heart failure. Curr Heart Fail Rep. 2014;11(3):266–273. doi: 10.1007/s11897-014-0198-4. [DOI] [PubMed] [Google Scholar]
- 23.Patel A., Parikh R., Howell E.H., Hsich E., Landers S.H., Gorodeski E.Z. Mini-cog performance: novel marker of post discharge risk among patients hospitalized for heart failure. Circ Heart Fail. 2015;8(1):8–16. doi: 10.1161/CIRCHEARTFAILURE.114.001438. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.