Abstract
Objective
Endoscopic/colonoscopic procedures are either done with gastroenterologist-administered conscious sedation or with anesthesia-administered sedation with propofol. There are potential benefits to anesthesia-administered sedation, but the concern has been the associated increased cost.
Methods
To perform this study, we used the time-derived activity-based costing (TDABC) technique to accurately assess the true cost of gastrointestinal procedures done with gastroenterologist-administered conscious sedation vs anesthesia-administered sedation in 2 areas of our practice that use predominantly conscious sedation or anesthesia-administered sedation. This type of study has never been reported using such an integrated approach. This study was performed on 2 different days in June 2015.
Results
The true cost associated with anesthesia-administered sedation in our practice was associated with only 9% to 24% greater cost when the TDABC technique was applied.
Conclusion
Gastrointestinal procedures with anesthesia-administered sedation are not as costly when all factors are considered. Using novel approaches to cost measurement, such as the TDABC, allows a total cost measurement approach across an episode of care that existing cost measurements in health care are incapable of.
Abbreviations and Acronyms: CRNA, certified nurse anesthetist; EGD, esophagogastroduodenoscopy; GI, gastrointestinal; RVU, relative value unit; TDABC, time-derived activity-based costing
Conscious sedation has been used to improve the patient experience in endoscopic procedures for more than 30 years. An increasing trend seen in endoscopic practices has been the utilization of propofol, administered by either anesthesiologists or certified nurse anesthetists (CRNAs), and this trend has impacted how endoscopists and patients view endoscopic sedation. During the past 15 years, propofol has become the drug of choice among many endoscopists due to its favorable pharmaceutical properties and safety profile.1, 2, 3 Propofol has hypnotic, antiemetic, and amnestic properties with the advantage of a rapid onset of action and a short recovery period. The depth of sedation increases in a dose-dependent manner.4 Emergence from sedation is also rapid because of its fast redistribution into peripheral tissues. Recovery from propofol will occur within 10 to 20 minutes after discontinuation. Studies demonstrate significantly shorter recovery times and faster recovery of cognitive function with propofol compared with traditional sedation.5, 6 A recent Cochrane review found that the use of propofol for sedation during colonoscopy can lead to faster recovery after the procedure and higher patient satisfaction, without any increase in adverse effects as compared with the use of drugs traditionally used (narcotics and/or benzodiazepines) for endoscopic procedure sedation.7 Polyp detection during colonoscopy does not appear to be improved by deeper sedation, although one study suggested a higher rate of detection of advanced lesions with deep sedation,8, 9, 10, 11 and speculation suggests that this is a result of the endoscopist being able to better focus on the examination rather than on the comfort and safety of the patient.
Importantly, titrating propofol to achieve conscious sedation without inducing general anesthesia requires significant clinical expertise.12 Although controversial, it is generally accepted that propofol-based sedation should be administered by appropriately trained anesthesiology personnel. There has been an increasing use of propofol and/or anesthesiology services in colonoscopy practice. Studies report a rise in the use of anesthesiology assistance from 11.0% in 2000 to 23.4% in 2006 in a Medicare cohort and from 13.6% to 35.5% in 2009 in a commercially insured group.13 It has been estimated that a nationwide conversion to monitored anesthesia care could result in as much as $5 billion per year in new US health care costs for gastrointestinal (GI) procedures and that the estimated cost per life-year saved to substitute anesthesia specialists in endoscopic procedures is approximately $5 million.14, 15
Recently, a provider-perspective economic model assessed the ability of rapid recovery agents (propofol and a closely related drug fospropofol) to increase practice efficiency.16 In the time to complete 1 colonoscopy with midazolam/meperidine, 1.76 colonoscopies can be completed with propofol and 1.91 colonoscopies can be completed with fospropofol.16 In addition to this time saving, we believed that the Mayo Clinic model of anesthesia care teams of anesthesiologists and CRNAs would lower total costs of using propofol relative to those reported by similar studies at other institutions.
The goal of this study was to compare the true overall cost difference between endoscopic procedures performed with conventional sedation and those performed with propofol. Although the use of propofol requires additional resources for anesthesia support, it offers cost-saving benefits from reduced procedure times for clinicians and staff. We used time-driven activity-based costing (TDABC) technique to measure accurately the costs of endoscopies under the 2 sedation regimens. The TDABC technique combines process mapping from industrial engineering and activity-based costing from accounting.17 Clinical teams direct and develop the process mapping by identifying the high-level events in a procedure or care cycle and then drill down into the process steps that occur within each event; in parallel, the finance staff develops the cost component by constructing a dollar-per-minute capacity cost rate for each clinical resource.14 By mapping processes and measuring the costs of the resources involved in clinical processes, health care organizations can better compare the true cost of providing care under alternative treatment regimens, such as traditional sedation vs propofol.18
Methods
Our goal was to work collaboratively with the departments of gastroenterology and anesthesiology to ascertain as accurately as possible the true costs to the institution of procedures done under the 2 types of sedation for GI endoscopy. We determined that the TDABC technique, a modern approach for accurate/transparent patient-level costing, offered the best way to measure the true cost of the procedure(s). We identified 2 geographically separate areas within the Mayo Clinic Rochester practice of endoscopy: one that uses only sedation with versed/fentanyl directed by an endoscopist and a second that uses predominantly sedation with propofol administered by a CRNA with staff anesthesiologist support. Over the same time period, we studied all patients in both clinical areas. The clinical processes and monitoring methods and standard monitoring techniques were not changed at any time during the study period. This study is not a randomized clinical trial; we studied consecutive patients who underwent procedures in 2 geographically separate areas that used these different practices.
We met with the clinical leaders and the administrative and finance staff of the gastroenterology and anesthesia departments and enlisted their support to objectively study the costs of endoscopies in the 2 different areas. In each location, 10 consecutive colonoscopy patients and 10 consecutive endoscopy patients (40 total patients) were studied. These studies were performed on 2 days (separated by 48 hours) in June 2015. In each location, the costs of both colonoscopies and upper GI tract endoscopies (esophagogastroduodenoscopy [EGD]) were measured. All groups agreed that TDABC would be the most valid costing approach for measuring cost differences. A steering group consisting of members of the 2 clinical departments, the Mayo TDABC team, and Harvard Business School staff codeveloped a work plan. The steering group met on a regular basis during the study to review workflow process maps and TDABC cost measurements. This study was conducted to illustrate the value framework, in which total cost of resources used by 2 different treatment protocols, which lead to similar patient outcomes, are measured and compared.
Clinical, administrative, and finance staff prepared the initial workflow process maps, including estimating the quantity of time that each clinical person spent at each process step for each type of procedure in each location. Many of the time estimates came from electronic time stamps in the electronic medical record system. The process flows included different scenarios, such as whether the procedures were performed with or without residents. The steering committee reviewed the process flows to ensure that they accurately represented the actual clinical workflow processes. In addition to the process flows, data on the costs of the various drugs and supplies used as part of each case were pulled from Mayo Clinic information systems so that we could compare the total direct personnel and supply costs across sedation methods.
The workflow process maps for colonoscopy with versed-fentanyl and colonoscopy with propofol are demonstrated in Figures 1 and 2.
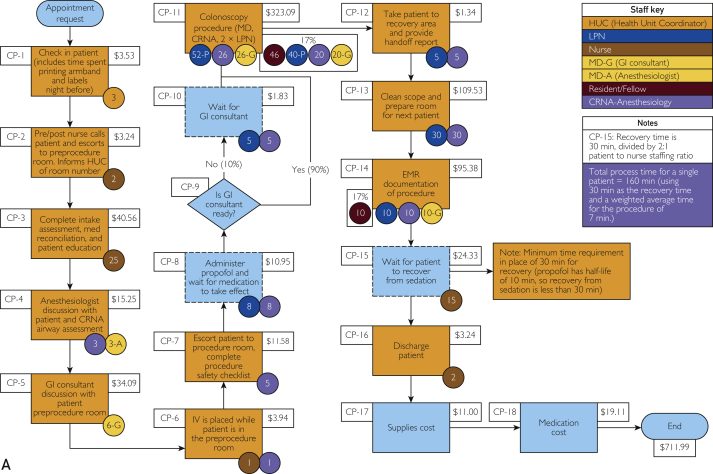
Figure 1.
A, Gonda 2: Colonoscopy with propofol (September 29, 2014). B, Gonda 2: EGD with propofol (September 24, 2014). Cost data only include certain direct patient care contact costs identified in the process flow maps; does NOT include estimates for consumable supplies, transcription, overhead, pharmacy, laboratory tests, etc. Gonda 2 refers to the area where anesthesia is involved in the procedures. The numbers included in circles are minutes that each provider was involved performing that step by various providers; see staff key in figure. CRNA = certified nurse anesthetist; EGD = esophagogastroduodenoscopy; EMR = electronic medical record; GI = gastrointestinal; HUC = Health Unit Coordinator; IV = intravenous; LPN = licensed practice nurse; MD = doctor of medicine; med = medications.
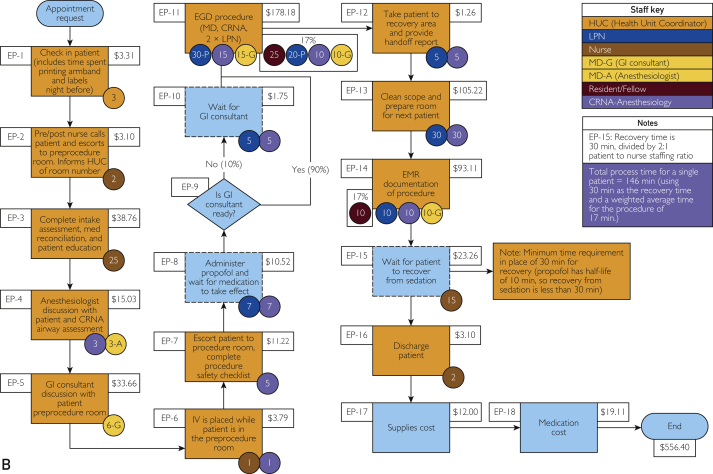
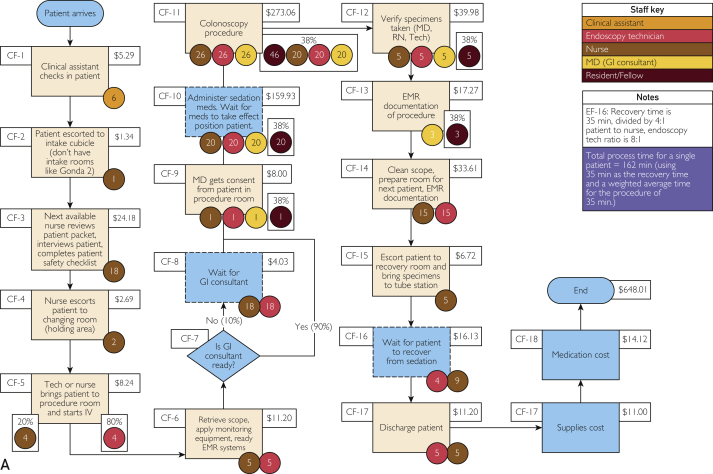
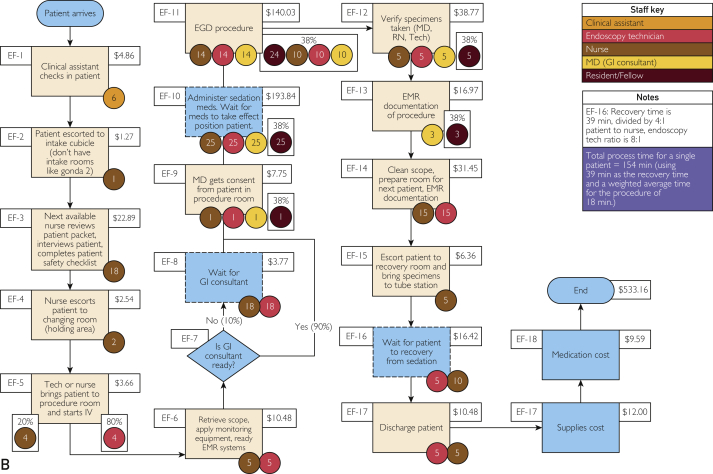
Figure 2.
A, Gonda 9: Colonoscopy with versed/fentanyl (September 29, 2014). B, Gonda 9: EGD with versed/fentanyl (September 29, 2014). Cost data only include certain direct patient care contact costs identified in the process flow maps; does NOT include estimates for consumable supplies, transcription, overhead, pharmacy, laboratory tests, etc. Gonda 2 refers to the area where anesthesia is involved in the procedures. The numbers included in circles are minutes that each provider was involved performing that step by various providers; see staff key in figure. EMR = electronic medical record; GI = gastrointestinal; IV = intravenous; MD = doctor of medicine; meds = medications; RN = registered nurse; Tech = technician.
Results
The existing operations with each model in place allowed for a direct comparison of the staffing, task times, supply costs, room times and utilization and turnover, and patient wait times.
The EGD process time with fentanyl was on average 154 minutes, which includes 18 minutes for the procedure and 39 minutes in the recovery room. The EGD process time with propofol was 146 minutes, which includes 17 minutes for the procedure and 30 minutes of recovery room time. Colonoscopy process time with fentanyl was 162 minutes, which includes 35 minutes for the procedure and 35 minutes in the recovery room. Colonoscopy process time with propofol was 160 minutes, which includes 29 minutes for the procedure and 30 minutes for the recovery room. Adverse events data were not collected, but there was no change in any of the clinical processes or monitoring during the time this cost study was performed. Applying the TDABC components and calculations to these flows revealed that the overall total costs of colonoscopy (without resident support) with propofol/anesthesia support was in total 24% more than with fentanyl/versed sedation. In the EGD practice, the overall total costs (without resident support) with propofol/anesthesia support were only 9% more than with fentanyl/versed. With resident support, the total costs of colonoscopy/EGD with propofol anesthesia support were 10% and 4% more than with fentanyl/versed. The increased cost of having anesthesia support with every case with propofol/anesthesia support was partially offset by the shorter time for sedation (8 minutes vs 20 minutes) and shorter time in the recovery room (30 minutes vs 35 minutes), which enabled higher room utilization and turnaround. Determining total cost in this manner provided by the TDABC technique provides the most accurate information on the true cost difference in the existing practice environment. Although the cost is greater with propofol and anesthesia support, we now have an accurate overall measurement of the difference.
Discussion
Value-based health care delivery offers a transformational opportunity to deliver improved patient outcomes at lower total costs.18 This study was performed to illustrate the value framework—measuring and comparing the total cost of resources used by 2 different treatment protocols with similar patient outcomes. The TDABC technique allows a much more accurate determination of the true cost of providing care for procedures or conditions. The Table contrasts TDABC and relative value unit (RVU) costing systems.18 Most important, TDABC is bottom-up, compared with the top-down allocations based on RVU metrics. The TDABC technique includes facility/hospital costs and physician costs instead of hospital/facility costs only. The TDABC technique includes costs of all processes included in a care cycle, not just the costs of reimbursable processes such as RVU metrics. Other important differences are listed in the Table.18
Table.
Comparison of TDABC and Typical RVU Costing Systems
| Process | TDABC | Typical RVU systems |
|---|---|---|
| Direct costs | Bottom-up, based on actual processes and resources used to treat patients | Top-down allocations based on derived (RVU) metrics |
| Scope | Includes hospital physician costs in an integrated calculation | Hospital costs only |
| Type of costing system | Standard costs based on estimates of resource's capacity cost rates | Actual costs; general ledger expenses allocated to procedures; easy reconciliation |
| Clinical input | Performed by teams of clinicians, administrators, and finance staff; highly actionable | Led and updated by finance; clinicians do not understand how costs are assigned |
| Care cycle | Assigns costs to all processes used during a patient's complete cycle of care | Costs assigned only to reimbursable processes; all other costs in allocated “overhead” |
| Pricing | Supports transparent and defensible pricing | Pricing unrelated to actual costs |
| Process improvement | Links naturally to lean and performance improvement initiatives | No connection to lean and process improvements |
| Benchmarking | Compares efficiency and resource costs across different units by clinical condition | Not used for benchmark (no visibility into underlying processes and personnel) |
| Unused capacity | Measures cost of unused capacity | All costs allocated to billable volume; no visibility into used vs unused capacity |
| Updating | Requires clinical teams to keep up-to-date maps of their processes | Requires finance to update RVU complexity metrics |
RVU = relative value unit; TDABC = time-derived activity-based costing.
The TDABC technique enabled us to determine the true overall costs of different endoscopic procedures when using different types of sedation in the Mayo Clinic practice environment. This integrated approach to evaluating the use of a purchased supply (eg, an alternative drug/sedative) has not been previously reported. This study demonstrates that increased spending/cost on one type of resource may be justified in terms of considerable savings in other resources used to treat patients over a complete episode or care cycle. Although the cost with propofol/anesthesia was greater, we now have a much more accurate measurement of the difference. We determined, by this method of true overall costs, that the cost difference between endoscopic procedures with propofol sedation and anesthesia support and those without was not nearly as great as anticipated by standard RVU cost measurements. Current existing cost measurements in health care, such as RVU allocations, are not capable of calculating accurate cost differences when new drugs and devices are introduced for patients' treatments. The TDABC method, as we demonstrated, does allow those cost comparisons to be accurately measured through a complete cycle of care.
Accurate costing helped us identify several opportunities for process improvement and cost reduction:
-
1.
We can further identify what incremental savings would be necessary to fully level the cost of the 2 methods of endoscopic procedures. These savings might come from further process improvements or cost reductions in staff.
-
2.
We now have accurate baseline data with which to make further decisions regarding our endoscopic/colonoscopic practice. Both patient and staff experience with propofol sedation and anesthesia support was much better and may be worth the additional cost because it is not as great as we had previously thought. This has led to our decision that all further GI procedure rooms built in the future should be outfitted to allow full anesthetic support. This difference in cost can now be used to better understand trade-offs with safety, patient satisfaction, staff satisfaction, and potential impact on contracting bundles.
-
3.
This project required teamwork and cooperation of several groups with the overall results encouraging to all involved. This has resulted in acceptance through the practice of other such TDABC projects.
Conclusion
We have demonstrated for the first time a total cost measurement approach not possible with existing cost measurement approaches; this has allowed us to make more informed decisions regarding the GI procedure practice at Mayo Clinic.
Footnotes
Dr Helmers is currently affiliated with the Northwest Wisconsin Region of the Mayo Clinic Health System, Eau Claire, WI.
Potential Competing Interests: The authors report no competing interests.
References
- 1.Lewis J.R., Cohen L.B. Update on colonoscopy preparation, premedication and sedation. Expert Rev Gastroenterol Hepatol. 2013;7(1):77–87. doi: 10.1586/egh.12.68. [DOI] [PubMed] [Google Scholar]
- 2.Okholm C., Hadikhadem T., Andersen L.T., Donatsky A.M., Vilmann P., Achiam M.P. No increased risk of perforation during colonoscopy in patients undergoing nurse administered propofol sedation. Scand J Gastroenterol. 2013;48(11):1333–1338. doi: 10.3109/00365521.2013.837951. [DOI] [PubMed] [Google Scholar]
- 3.Qadeer M.A., Vargo J.J., Khandwala F., Lopez R., Zuccaro G. Propofol versus traditional sedative agents for gastrointestinal endoscopy: a meta-analysis. Clin Gastroenterol Hepatol. 2005;3(11):1049–1056. doi: 10.1016/s1542-3565(05)00742-1. [DOI] [PubMed] [Google Scholar]
- 4.Triantafillidis J.K., Merikas E., Nikolakis D., Papalois A.E. Sedation in gastrointestinal endoscopy: current issues. World J Gastroenterol. 2013;19(4):463–481. doi: 10.3748/wjg.v19.i4.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen L.B. Sedation issues in quality colonoscopy. Gastrointest Endosc Clin N Am. 2010;20(4):615–627. doi: 10.1016/j.giec.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Watkins T.J., Bonds R.L., Hodges K., Goettle B.B., Dobson D.A., Maye J.P. Evaluation of postprocedure cognitive function using 3 distinct standard sedation regimens for endoscopic procedures. AANA J. 2014;82(2):133–139. [PubMed] [Google Scholar]
- 7.Singh H., Poluha W., Cheung M., Choptain N., Baron K.I., Taback S.P. Propofol for sedation during colonoscopy. Cochrane Database Syst Rev. 2008;(4):CD006268. doi: 10.1002/14651858.CD006268.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Metwally M., Agresti N., Hale W.B., et al. Conscious or unconscious: the impact of sedation choice on colon adenoma detection. World J Gastroenterol. 2011;17(34):3912–3915. doi: 10.3748/wjg.v17.i34.3912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paspatis G.A., Tribonias G., Manolaraki M.M., et al. Deep sedation compared with moderate sedation in polyp detection during colonoscopy: a randomized controlled trial. Colorectal Dis. 2011;13(16):e137–e144. doi: 10.1111/j.1463-1318.2011.02555.x. [DOI] [PubMed] [Google Scholar]
- 10.Rex D.K. Does the use of sedation, or the level of sedation, affect detection during colonoscopy? Am J Gastroenterol. 2012;107(12):1849–1851. doi: 10.1038/ajg.2012.354. [DOI] [PubMed] [Google Scholar]
- 11.Wang A., Hoda K.M., Holub J.L., Eisen G.M. Does level of sedation impact detection of advanced neoplasia? Dig Dis Sci. 2010;55(8):2337–2343. doi: 10.1007/s10620-010-1226-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gasparovic S., Rustemovic N., Opacic M., et al. Clinical analysis of propofol deep sedation for 1,104 patients undergoing gastrointestinal endoscopic procedures: a three year prospective study. World J Gastroenterol. 2006;12(2):327–330. doi: 10.3748/wjg.v12.i2.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cooper G.S., Kou T.D., Rex D.K. Complications following colonoscopy with anesthesia assistance: a population-based analysis. JAMA Intern Med. 2013;173(7):551–556. doi: 10.1001/jamainternmed.2013.2908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rex D.K. Effect of the Centers for Medicare & Medicaid Services policy about deep sedation on use of propofol. Ann Intern Med. 2011;154(9):622–626. doi: 10.7326/0003-4819-154-9-201105030-00007. [DOI] [PubMed] [Google Scholar]
- 15.Rex D.K., Deenadayalu V.P., Eid E., et al. Endoscopist-directed administration of propofol: a worldwide safety experience. Gastroenterology. 2009;137(4):1229–1237. doi: 10.1053/j.gastro.2009.06.042. [DOI] [PubMed] [Google Scholar]
- 16.Vargo J.J., Bramley T., Meyer K., Nightengale B. Practice efficiency and economics: the case for rapid recovery sedation agents for colonoscopy in a screening population. J Clin Gastroenterol. 2007;41(6):591–598. doi: 10.1097/01.mcg.0000225634.52780.0e. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan R.S., Witkowski M., Abbott M., et al. Using time-driven activity-based costing to identify value improvement opportunities in healthcare. J Healthc Manag. 2014;59(6):399–412. [PubMed] [Google Scholar]
- 18.Kaplan R.S. Improving value with TDABC. Healthc Financ Manage. 2014;68(6):76–83. [PubMed] [Google Scholar]