Abstract
Background. Many people recognize the potential benefits of advance directives (ADs), yet few actually complete them. It is unknown whether an active choice intervention influences AD completion. Methods. New employees were randomized to an active choice intervention (n = 642) or usual care (n = 637). The active choice intervention asked employees to complete an AD, confirm prior AD completion, or fill out a declination form. In usual care, participants could complete an AD, confirm prior completion, or skip the task. We used multivariable logistic regression to assess the relationship between the intervention arm and both AD completion online and the return of a signed AD by mail, as well as assess interactions between intervention group and age, gender, race, and clinical degree status. Results. Participants assigned to the active choice intervention more commonly completed ADs online (35.1% v. 20.4%, P < 0.001) (odds ratio [OR] = 2.10; 95% confidence interval [CI] = 1.63–2.71; number needed to treat = 6.8) and returned signed ADs by mail (7.8% v. 3.9%, P = 0.003; number needed to treat = 25.6). The effect of the intervention was significantly greater among men (OR = 4.13; 95% CI = 2.32–7.35) than among women (OR = 1.74; 95% CI = 1.30–2.32) (interaction P value < 0.001). Responses to all eight choices made in the ADs were similar between groups (all P > 0.10). Limitations. A young and healthy participant may not benefit from AD completion as an older or seriously ill patient would. Conclusions. The active choice intervention significantly increased the proportion of participants completing an AD without changing the choices in ADs. This relationship was especially strong among men and may be a useful method to increase AD completion rates without altering choices.
Keywords: active choice, advance directive, end of life, forced choice
Approximately 30% of Americans die in the following unenviable position: decisions must be made regarding the use or nonuse of health care services in the final days of their lives, yet the patients are already too sick to guide such choices.1 Surrogate decision making is an imperfect solution because even close family members commonly err in their estimates of patients’ end-of-life preferences,2 despite most patients believing their family members would represent their wishes accurately.3 Furthermore, making decisions regarding the use or nonuse of life support is associated with long-lasting pathological bereavement among surrogates,4–9 contravening most patients’ desires not to burden their loved ones.10–13
For these and other reasons, many national policies and local practices are designed to encourage people to communicate and disseminate their treatment goals in advance, through written advance directives (ADs) or other forms of advance care planning.14 For example, the Patient Self Determination Act of 1990 requires that institutions certified by Medicare document whether or not all patients they see have completed ADs, and offer patients the opportunity to complete ADs. More recently, the Centers for Medicare and Medicaid Services, through the 2016 Physician Fee Schedule Final Rule,15 began reimbursing clinicians for engaging in advance care planning with patients. Although experimental evidence of the benefits of ADs or other forms of advance care planning is sparse,16 several observational studies suggest that patients who choose to complete ADs are more likely to receive the care they desire.1,17–19
Despite these policies and data supporting advance care planning and AD completion for broad populations of Americans, actual AD completion rates are low,20 and interventions to increase AD completion have been disappointing.21,22 For example, a recent randomized trial found that expanding options for patients with end-stage renal disease to complete an AD increased patients’ stated willingness to complete ADs, but did not change actual completion.23 This null result may be attributable to the power of inertia—in this case, the tendency to not actively complete an AD even when people wanted to do so. We therefore reasoned that, by requiring people to act by either completing an AD or declining AD completion, we might overcome tendencies to procrastinate and augment completion rates. Indeed, active choice interventions, in which subjects must actively complete or decline a task, have been shown to increase enrollment in retirement plans,24 HIV screening in the emergency department,25 and employees’ stated willingness to get a flu shot.26 We therefore sought to determine whether an active choice intervention could increase the personal and relatively intractable behavior of AD completion.
Methods
We conducted a randomized trial of an active choice intervention for AD completion among new University of Pennsylvania Health System (UPHS) employees hired between 7 November 2014 and 19 August 2015. This study was approved by the University of Pennsylvania Institutional Review Board (Protocol #818456; ClinicalTrials.gov, NCT02289105).
Recruitment
UPHS’s Human Resources Department customarily sends new employees emails to provide them with information and login credentials for completing their online new employee intake. During this trial’s recruitment period, the email contained additional information notifying employees that they would be participating in a study evaluating the completion of employment paperwork. Employees could opt out of the study by contacting the research team.
Randomization
All participants were assigned a “Future Healthcare Planning” task in their online employee intake portal in addition to other tasks germane to new employees (Online Appendix Figures 1–3). Although the presentation of this task in the portal was intended to imply that its completion was required, in truth employees were not forced to click on it in order to complete their new employee intake. Participants opening the Future Healthcare Planning task were taken to a website that randomized them to the active choice intervention or control.
Interventions
All participants were provided with educational information about ADs. Control participants were told that completion of the Future Healthcare Planning task was optional. They could choose to complete an AD, confirm prior AD completion, or skip AD completion. Skipping AD completion is consistent with standard approaches to offering people the opportunity to complete ADs, such as that endorsed by the Patient Self Determination Act.27 Participants randomized to the active choice arm were instructed that completion of the Future Healthcare Planning task was required for employment. These participants could complete an AD, confirm prior AD completion, or complete a form declining AD completion and indicating their reason(s) for doing so.
AD Completion and Follow-Up
The primary and secondary outcomes were the proportions of participants who completed an AD online and returned a signed and witnessed AD by mail, respectively. Participants choosing to complete an AD could do so online. However, because Pennsylvania law requires two witness signatures or notarization to make ADs legally valid, we mailed two copies of ADs completed online to the participant with instructions to return one copy signed by the participant plus a notary or two witnesses.
Data Collection
Outcomes data were collected via the advance care planning website, and participant characteristics were collected through regular UPHS Human Resources Department’s procedures (Table 1).
Table 1.
Baseline Demographics of Study Participants
| Characteristic | Participants |
||
|---|---|---|---|
| Active Choice Intervention (n = 642) | Control (n = 637) | Total (N = 1,279) | |
| Age, median (IQR) | 29 (25–39) | 29 (25–37) | 29 (25–38) |
| Gender, n (%)a | |||
| Female | 446 (69.5%) | 472 (74.1%) | 918 (71.8%) |
| Male | 186 (29.0%) | 147 (23.1%) | 333 (26.0%) |
| Prefer not to answer or missing | 10 (1.6%) | 18 (2.8%) | 28 (2.2%) |
| Race, n (%) | |||
| White | 333 (51.9%) | 345 (54.2%) | 678 (53.0%) |
| Black | 177 (27.6%) | 167 (26.2%) | 344 (26.9%) |
| Asian | 51 (7.9%) | 41 (6.4%) | 92 (7.2%) |
| Mixed or other | 55 (8.6%) | 50 (7.9%) | 105 (8.2%) |
| Prefer not to answer or missing | 26 (4.1%) | 34 (5.3%) | 60 (4.7%) |
| Employment status, n (%) | |||
| Full-time | 464 (72.3%) | 469 (73.6%) | 933 (73.0%) |
| Part-time | 178 (27.7%) | 168 (26.4%) | 346 (27.1%) |
| Highest level of education, n (%) | |||
| Graduate degree | 115 (17.9%) | 109 (17.1%) | 224 (17.5%) |
| College degree | 304 (47.4%) | 298 (46.8%) | 602 (47.1%) |
| Some college | 136 (21.2%) | 133 (20.9%) | 269 (21.0%) |
| High school or less | 57 (8.9%) | 51 (8.0%) | 108 (8.4%) |
| Missing | 30 (4.7%) | 46 (7.2%) | 76 (5.9%) |
| Clinical degree, n (%)b | |||
| No | 500 (77.9%) | 510 (80.1%) | 1010 (79.0%) |
| Yes | 142 (22.1%) | 127 (19.9%) | 269 (21.0%) |
IQR, interquartile range.
There were significantly more women assigned to the control group (P = 0.023); no other participant characteristic differed by group (all other P > 0.05).
Participants were considered to have clinical degrees if they had any of the following designations: MD, MSN, BSN, RN, LPN, DO, NP, PA, DPT, PharmD, DVM, CRNA, speech pathology, CNA, CMA, surgical tech, medical assistant, nurse assistant, or medical tech.
The AD form was a modified version of the Allegheny County Medical Society’s28 AD that we have used in prior work.29 The form allows participants to name a health care agent and to indicate whether they prefer that their agents follow the instructions on the AD strictly or as a guide. In addition, the form solicited participants’ preferences for their overall goals of care (life-extending, comfort-oriented, or do not specify), care on hospital discharge, and, in the event of terminal illness or permanent unconsciousness, preferences to receive a feeding tube, cardiopulmonary resuscitation, mechanical ventilation, or dialysis (Online Appendix Figure 4).
Analysis
We used logistic regression to compare baseline patient demographics and the outcomes after assessing continuous variables in locally weighted scatterplot smoothing graphs for linearity. To arrive at a final, fully adjusted model, we included randomization group, age, and any baseline demographic variables that had a bivariable relationship with the primary outcome of P < 0.20. We used backward selection guided by the Wald test to eliminate variables one-by-one to arrive at a final parsimonious model. We included interaction terms individually in the final model to assess modification of the intervention’s effects by four prespecified participant characteristics: age, gender, race, and clinical education. All analyses followed a prespecified analytic plan and were performed using Stata Version 14 (StataCorp, College Station, TX).
Statistical Power
To achieve 80% power to detect a raw difference of 10% in rates of online AD completion between the control arm and the intervention arm, assuming a 20% completion rate in the control arm, it was required that we enroll 588 participants. To test the robustness of the results to a slight wording change in the intervention arm (Online Appendix Figures 2–5), we aimed to recruit an additional 588 participants in a second phase of the trial to achieve independently adequate power in that phase. Due to limitations on our ability to precisely control the timing of the change in the language, and to terminate the second phase of the trial, we actually recruited 481 patients in the first phase and 798 patients in the second phase. Because the distributions of all participant characteristics and outcomes were similar in the two phases, we report combined results among the 1,279 patients randomized in primary analyses, and the results stratified by phase in the Technical Appendix.
This study was supported by a grant from the Otto Haas Charitable Trust and through in-kind research support from the University of Pennsylvania Health System. The funding sources had no role in study design, data acquisition, analysis, or decision to publish.
Ethical Considerations
UPHS employees were not informed about the goals of the study until after they had participated because doing so would likely have influenced their behavior, skewing the results of our primary and secondary outcomes. Instead, the institutional review board authorized the conduct of this study with a waiver from the requirement from prospective informed consent, deeming an intervention designed to increase AD completion to be minimal risk. Instead of prospective informed consent, all participants were debriefed about the study by mail at its conclusion. The debriefing letter notified employees of their participation in the study, explained the purpose of the study, and provided contact information for the research team as well as the University of Pennsylvania Institutional Review Board.
Results
Baseline Characteristics of Participants
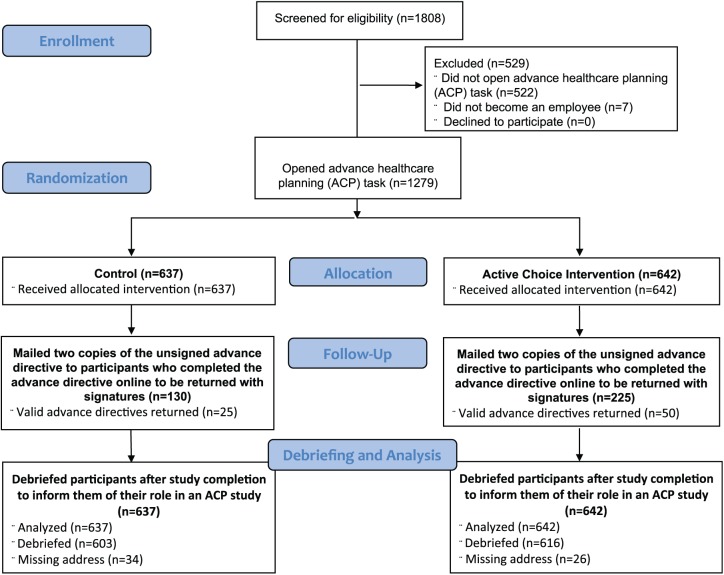
There were 1,808 new hires between 7 November 2014 and 19 August 2015. None opted out of the research study, but 529 (29.3%) were not randomized because 522 did not click on the ACP task within the OnBoarding portal, and 7 did not proceed to become employees (Figure 1). Of the 1,279 eligible participants, 642 were randomized to the active choice intervention and 637 were assigned to control. Participant characteristics were evenly distributed between groups except for gender, with more women assigned to the control arm (Table 1). Modal participant characteristics were age 25 to 38 years, female, white, and full-time employees who were college educated but did not hold clinical degrees.
Figure 1.
CONSORT diagram.
Advance Directive Completion
Participants in the active choice arm were more likely to complete ADs online (35.1% v. 20.4%, P < 0.001) (odds ratio [OR] = 2.10; 95% confidence interval [CI] = 1.63–2.71; number needed to treat [NNT] = 6.8) and to return signed and witnessed ADs by mail (7.8% v. 3.9%, P = 0.003; NNT = 25.6) than those in the control arm (Figure 2). Forty-two (6.5%) participants in the active choice arm and 40 (6.3%) participants in the control arm confirmed prior AD completion (Table 2). In bivariable analyses, participant race, employment status, age, and highest level of education were associated with AD completion at P < 0.20 and eligible for inclusion in the adjusted model; participant gender and clinician status were not.
Figure 2.
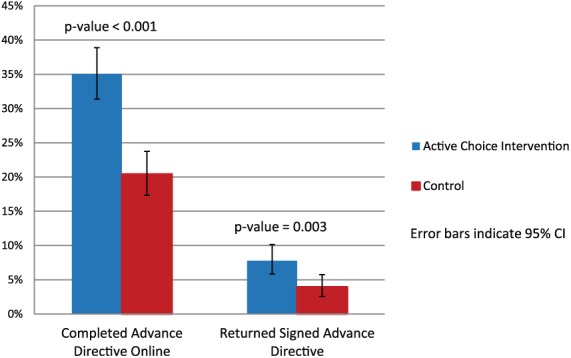
Proportion of participants who completed and returned an advance directive.
Table 2.
Participant Responses to Active Choice or Control Intervention
| Participant response, n (%) | Participants |
||
|---|---|---|---|
| Active Choice Intervention (n = 642) | Control (n = 637) | Total (N = 1,279) | |
| Complete an advance directive | 225 (35.1%) | 130 (20.4%) | 355 (27.8%) |
| Decline advance directive completion | 310 (48.3%) | — | 310 (24.2%) |
| Skip task | — | 449 (70.5%) | 449 (35.1%) |
| Confirm prior advance directive completion | 42 (6.5%) | 40 (6.3%) | 82 (6.4%) |
| Close out of window | 65 (10.1%) | 18 (2.8%) | 83 (6.5%) |
Exploratory Subgroup Effects
The active choice intervention was significantly more effective among men (OR = 4.13; 95% CI = 2.32–7.35) than among women (OR = 1.74; 95% = 1.30–2.32) (interaction P < 0.001). Participant age, race, and clinical degree status did not significantly modify the intervention’s effect on AD completion (all interaction P > 0.10; Table 3).
Table 3.
Modification of the Active Choice Intervention Effect on Advance Directive Completion by Baseline Demographics Characteristics
| Characteristic, n (%) | Completed Advance Directive, Active Choice Intervention | Completed Advance Directive, Control | OR (95% CI) | Interaction P Value |
|---|---|---|---|---|
| Age | 0.50 | |||
| <26 | 57 (29.2%) | 33 (17.5%) | 1.95 (1.20-3.17) | |
| 26-35 | 91 (37.8%) | 57 (21.1%) | 2.27 (1.53-3.35) | |
| 36-45 | 47 (37.9%) | 24 (23.5%) | 1.98 (1.11-3.56) | |
| >45 | 30 (36.6%) | 16 (21.1%) | 2.16 (1.06-4.41) | |
| Gendera | <0.001 | |||
| Female | 154 (34.5%) | 110 (23.3%) | 1.74 (1.30-2.32) | |
| Male | 68 (36.6%) | 18 (12.2%) | 4.13 (2.32-7.35) | |
| Race | 0.46 | |||
| White | 96 (28.8%) | 65 (18.8%) | 1.74 (1.22-2.50) | |
| Black | 69 (39.0%) | 39 (23.4%) | 2.09 (1.31-3.35) | |
| Asian | 21 (41.2%) | 8 (19.5%) | 2.89 (1.11-7.49) | |
| Mixed or other | 29 (52.7%) | 11 (22.0%) | 3.95 (1.68-9.28) | |
| Prefer not to answer or missing | 10 (38.5%) | 7 (20.6%) | 2.41 (0.77-7.59) | |
| Clinical degree | 0.183 | |||
| No | 184 (36.8%) | 103 (20.2%) | 2.30 (1.73-3.05) | |
| Yes | 41 (28.9%) | 27 (21.3%) | 1.50 (0.86-2.63) |
CI, confidence interval; OR, odds ratio.
Participants with missing gender were excluded from analysis (n = 5).
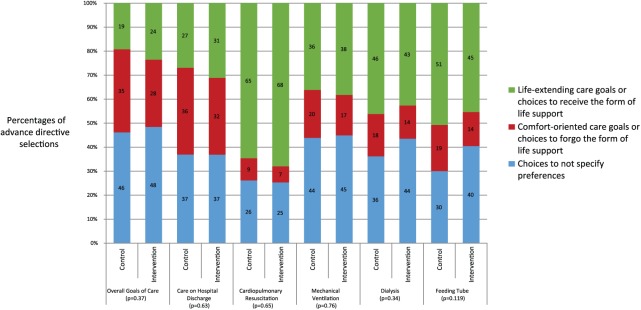
Intervention Effects on Advance Directive Choices
The intervention was not associated with differences in the distributions of responses to any of the eight selections that participants made in their ADs, including overall preferences for care and choices regarding use of specific interventions (all P > 0.10; Figure 3).
Figure 3.
Selections within completed advance directives among participants assigned to the active choice intervention or control. This figure presents data for six of the eight choices made by participants in their advance directives. Not shown are the proportions of participants who chose to designate a power of attorney or the proportions who chose to have that agent follow the preferences in the advance directive strictly vs. as a guide. The intervention did not affect either of these other two choices (p = 0.36 and p = 0.84, respectively).
Discussion
This randomized trial demonstrates that simply requiring people to actively choose to complete an AD or decline to do so increases completion rates nearly twofold relative to offering people the opportunity to complete an AD, as is promoted by the Patient Self Determination Act.27 Requiring people to make active choices increases rates of target behaviors by preventing procrastination and overcoming inertia rather than by manipulating people to do things they prefer not to do.24,26 It is an attractive way to increase AD completion because it motivates active engagement. As with prior proposals to require people to actively choose whether or not to be organ donors,30,31 promoting engagement in the act of choosing whether or not to complete an AD may later help clinicians and family members believe that the choices made reflected authentic preferences.26 Furthermore, requiring active choice for AD completion appears to resonate with the American public. In a recent survey of 883 Americans, we found that a majority supported a proposal that would require people to actively choose whether or not to complete an AD as a condition of obtaining health insurance.32
That such a simple, easily scalable intervention could double AD completion rates is important because most interventions tested to date have not been experimentally shown to improve rates of AD completion.22 And the prior interventions that have succeeded were resource-intensive to deliver.33 By contrast, this large randomized trial shows that a low-cost intervention that can be delivered without any human involvement can substantially increase AD completion rates.
A second important finding of this study is that although the active choice intervention increases AD completion, it does not alter the choices people make within ADs. The absence of significant differences in the selections made in participants’ ADs between randomization arms suggests that participants who are influenced by the intervention to complete ADs nonetheless engage in the act of selecting treatment preferences to the same extent as those who would complete an AD without this nudge. Importantly, among participants who completed ADs, those in the intervention group were no more likely than those in the control group to choose not to specify choices for any of their AD responses. Thus, the intervention may increase AD completion without changing the quality of information contained in such documents.
Third, we found that the active choice intervention was effective among all subgroups studied. Although participants in this study were younger and less sick than cohorts that are perhaps best suited for advance care planning,34 the relative effect of the intervention versus control was nearly identical across all participant age groups. If this relative effect were preserved among the elderly, who tend to have higher baseline rates of AD completion,35 then the absolute increases in AD completion attributable to active choice would be greater still.
Whereas age did not modify the effect of the intervention, the intervention was substantially more effective among men than among women. Men were less likely to complete ADs in the control group than were women (12.2% and 23.3%, respectively), yet this gap was eliminated in the intervention group (36.6% of men and 34.5% of women completed ADs in that group). This finding is similar to Carroll and colleagues’ report that an active choice intervention induced greater contributions to 401(k) plans among men than among women.24 However, future research is needed to elucidate potential mechanisms accounting for this gender difference.
Finally, although the intervention nearly doubled AD completion, as measured by both the primary outcome of completion of ADs online and by the secondary outcome of returning signed and legally valid ADs by mail, the absolute rates of these outcomes differed substantially. Specifically, fewer than half of participants who were sufficiently interested in advance care planning to have completed an AD online followed through by returning a signed and valid directive. This drop-off between ADs completed by web and those returned by mail may be explained, in part, by the lack of incentives participants had to return a signed AD to the study team. However, this result could also indicate that the requirements for witnessed signatures or notarization are substantive barriers that contravene patients’ true goals of completing ADs. This finding also requires verification but, if replicated, may provide empirical support for the suggestion that loosening the signatory requirements of ADs, which have dubious clinical importance, might help increase completion rates.36
Strengths of this study include the large sample size, the absence of postrandomization losses, and the capacities to assess modification of the intervention’s effects as well as the effects of the intervention on the choices made within ADs. An important limitation of this study is that it was conducted among relatively young and presumably healthy Americans. The benefits of advance directives, and the stability of preferences indicated in such documents, are likely greater for older and more seriously ill patients.34,37 Thus, while this study establishes the principles that requiring active choice can meaningfully improve AD completion without degrading the quality of information contained within ADs, future work is needed in more seriously ill populations to replicate the findings and determine the clinical impact of this intervention. In this regard, the complementary finding that most Americans support requiring active choice to complete an AD or not as a condition of acquiring health insurance32 suggests a clear opportunity for future work. Specifically, a policy requiring older, seriously ill patients to decide whether or not to complete an AD before enrolling in or renewing Medicare or other forms of health insurance merits evaluation.
A second limitation is that 529 employees skipped the health care planning task. Although we attempted to message that the task was part of the employment process, we could not truly prevent employment if participants did not complete the task. If a truly “forced” active choice intervention had been used, the observed effects may have been larger.
Conclusion
Our results indicate that a simple, active choice intervention may help surmount procrastination and inertia—both common barriers to AD completion. Furthermore, similar AD choices in both intervention and control arms indicated that participants maintained autonomy to freely choose AD selections and that the intervention did not influence actual AD selections. This scalable intervention signals a promising strategy to increase AD completion while maintaining individual autonomy. More research is needed in populations of patients who have experience living with serious illness, or others, such as the elderly, who are likely to benefit from AD completion in the foreseeable future.
Supplementary Material
Acknowledgments
We thank Erich Hall, Margaret Alford, and Judy Schueler from the UPHS Human Resources Department for helping collect demographic data and building the advance directive website for this project.
Footnotes
Financial support for this study was provided by a grant from the Otto Haas Charitable Trust and through in-kind research support from the University of Pennsylvania Health System. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Registration: ClinicalTrials.gov (NCT02289105).
Supplementary Material: The online supplementary appendixes for this article are available on the Medical Decision Making Policy & Practice Web site at http://journals.sagepub.com/doi/suppl/10.1177/2381468317753127.
References
- 1. Silveira MJ, Kim SYH, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: a systematic review. Arch Intern Med. 2006;166(5):493–7. doi: 10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- 3. Seckler AB, Meier DE, Mulvihill M, Paris BE. Substituted judgment: how accurate are proxy predictions? Ann Intern Med. 1991;115(2):92–8. [DOI] [PubMed] [Google Scholar]
- 4. Wright AA, Keating NL, Balboni TA, Matulonis UA, Block SD, Prigerson HG. Place of death: correlations with quality of life of patients with cancer and predictors of bereaved caregivers’ mental health. J Clin Oncol. 2010;28(29):4457–64. doi: 10.1200/jco.2009.26.3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171(9):987–94. doi: 10.1164/rccm.2000409-1295OC. [DOI] [PubMed] [Google Scholar]
- 7. Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154(5):336–46. doi: 10.1059/0003-4819-154-5-201103010-00008. [DOI] [PubMed] [Google Scholar]
- 9. Siegel MD, Hayes E, Vanderwerker LC, Loseth DB, Prigerson HG. Psychiatric illness in the next of kin of patients who die in the intensive care unit. Crit Care Med. 2008;36(6):1722–8. doi: 10.1097/CCM.0b013e318174da72. [DOI] [PubMed] [Google Scholar]
- 10. Terry PB, Vettese M, Song J, et al. End-of-life decision making: when patients and surrogates disagree. J Clin Ethics. 1999;10(4):286–93. [PubMed] [Google Scholar]
- 11. Singer PA, Martin DK, Lavery JV, Thiel EC, Kelner M, Mendelssohn DC. Reconceptualizing advance care planning from the patient’s perspective. Arch Intern Med. 1998;158(8):879–84. [DOI] [PubMed] [Google Scholar]
- 12. Mead GE, O’Keeffe ST, Jack CI, Maèstri-Banks AM, Playfer JR, Lye M. What factors influence patient preferences regarding cardiopulmonary resuscitation? J R Coll Physicians Lond. 1995;29(4):295–8. [PMC free article] [PubMed] [Google Scholar]
- 13. Steinhauser AE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284(19):2476–82. [DOI] [PubMed] [Google Scholar]
- 14. Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med. 2010;153(4):256–61. doi: 10.1059/0003-4819-153-4-201008170-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Centers for Medicare & Medicaid Services. Medicare program; Revisions to payment policies under the physician fee schedule and other revisions to Part B for CY 2016. Final rule with comment period. Fed Regist. 2015;80(220):70885–1386. [PubMed] [Google Scholar]
- 16. Halpern SD. Toward evidence-based end-of-life care. N Engl J Med. 2015;373(21):2001–3. doi: 10.1056/NEJMp1509664. [DOI] [PubMed] [Google Scholar]
- 17. Degenholtz HB, Rhee Y, Arnold RM. Brief communication: the relationship between having a living will and dying in place. Ann Intern Med. 2004;141(2):113–7. [DOI] [PubMed] [Google Scholar]
- 18. Nicholas LH, Langa KM, Iwashyna TJ, Weir DR. Regional variation in the association between advance directives and end-of-life Medicare expenditures. JAMA. 2011;306:1447–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc. 2007;55(2):189–94. doi: 10.1111/j.1532-5415.2007.01045.x. [DOI] [PubMed] [Google Scholar]
- 20. Yadav KN, Gabler NB, Cooney E, et al. Approximately one in three U.S. adults completes any type of advance directive for end-of-life care. Health Aff (Millwood). 2017;36:1244–51. [DOI] [PubMed] [Google Scholar]
- 21. Jezewski MA, Meeker MA, Sessanna L, Finnell DS. The effectiveness of interventions to increase advance directive completion rates. J Aging Health. 2007;19(3):519–36. doi: 10.1177/08982643073000198. [DOI] [PubMed] [Google Scholar]
- 22. Ramsaroop SD, Reid MC, Adelman RD. Completing an advance directive in the primary care setting: what do we need for success? J Am Geriatr Soc. 2007;55(2):277–83. doi: 10.1111/j.1532-5415.2007.01065.x. [DOI] [PubMed] [Google Scholar]
- 23. Courtright KR, Madden V, Gabler NB, et al. Expanded choice sets increase patients’ willingness to complete advance directives. Med Decis Making. 2016;36(5):E171–2. [Google Scholar]
- 24. Carroll GD, Choi JJ, Laibson D, Madrian BC, Metrick A. Optimal defaults and active decisions. Q J Econ. 2009;124(4):1639–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Montoy JCC, WH Dow, Kaplan BC. Patient choice in opt-in, active choice, and opt-out HIV screening: randomized clinical trial. BMJ. 2016;352:9. doi: 10.1136/bmj.h6895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Keller PA, Harlam B, Loewenstein G, Volpp KG. Enhanced active choice: a new method to motivate behavior change. J Consumer Psychol. 2011;21(4):376–83. doi: 10.1016/j.jcps.2011.06.003. [DOI] [Google Scholar]
- 27. Patient Self Determination Act (1990). Available from: https://www.congress.gov/bill/101st-congress/house-bill/4449
- 28. Allegheny County Medical Society. Healthcare power of attorney and living will. Available from: https://www.acba.org/portals/1/pdf/LivingWillPowerofAttorney.pdf
- 29. Halpern SD, Loewenstein G, Volpp KG, et al. Default options in advance directives influence how patients set goals for end-of-life care. Health Aff (Millwood). 2013;32(2):408–17. doi: 10.1377/hlthaff.2012.0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Spital A. Mandated choice—a plan to increase public commitment to organ donation. JAMA. 1995;273(6):504–6. doi: 10.1001/jama.273.6.504. [DOI] [PubMed] [Google Scholar]
- 31. Spital A. Mandated choice for organ donation: time to give it a try. Ann Intern Med. 1996;125(1):66–9. [DOI] [PubMed] [Google Scholar]
- 32. Auriemma CL, Chen L, Olorunnisola M, et al. Public opinion regarding financial incentives to engage in advance care planning and complete advance directives. Am J Hosp Palliat Care. 2017;34(8):721–8. doi:10.1177/104990911665 2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Song J, Ratner ER, Wall MM, et al. Effect of an end-of-life planning intervention on the completion of advance directives in homeless persons: a randomized trial. Ann Intern Med. 2010;153(2):76–84. doi: 10.7326/0003-4819-153-2-201007200-00003. [DOI] [PubMed] [Google Scholar]
- 34. Halpern SD. Shaping end-of-life care: behavioral economics and advance directives. Semin Respir Crit Care Med. 2012;33:393–400. [DOI] [PubMed] [Google Scholar]
- 35. Bradley EH, Wetle T, Horwitz SM. The Patient Self-Determination Act and advance directive completion in nursing homes. Arch Fam Med. 1998;7(5):417–23. doi: 10.1001/archfami.7.5.417. [DOI] [PubMed] [Google Scholar]
- 36. Lo B, Steinbrook R. Resuscitating advance directives. Arch Intern Med. 2004;164(14):1501–6. [DOI] [PubMed] [Google Scholar]
- 37. Auriemma CL, Nguyen CA, Bronheim R, et al. Stability of end-of-life preferences: a systematic review of the evidence. JAMA Intern Med. 2014;174:1085–92. doi: 10.1001/jamainternmed.2014.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.