Abstract
Objective:
To present a modification in the technique of an anterior approach for Bernese periacetabular osteotomy through an oblique inguinal incision.
Introduction:
Reorientation of the acetabulum in Bernese periacetabular osteotomy provides adequate coverage of the femoral head, improving biomechanical conditions of the joint without the risk of osteonecrosis. The principal author modified this procedure through an anterior approach with no detachment of the rectus femoris, allowing early rehabilitation. Evolution of scars is an issue both in the original technique and in our modification in terms of hypertrophy, depression, or hyperpigmentation and dehiscence. We introduce an oblique inguinal incision reducing both static and dynamic tension of the skin, allowing healing and avoiding development of unsatisfactory scars.
Methods:
Thirty-five surgeries with a modified technique were performed in 27 patients between 2014 and 2016. The average patient age was 27.09 years. No patients were excluded. Development of hypertrophic, depressed, and hyperpigmented scars was evaluated in addition to dehiscence.
Results:
The average length of the scar was 14.1 cm, and average diastasis was 1.3 mm. There were no hypertrophic, depressed, or hyperpigmented scars. No patients had dehiscence or resutures of surgical wounds.
Conclusion:
Oblique inguinal incision for the anterior approach in Bernese periacetabular osteotomy is a technique that allows healing of surgical wounds without dehiscence or hypertrophic changes by respecting tension lines. It has a high rate of patient satisfaction, with no complications.
Periacetabular osteotomy described by Ganz et al1 has become the preferred surgery for treating patients with hip dysplasia, triradiate cartilage closure, and no arthritic changes. Reorientation of the acetabulum provides adequate coverage of the femoral head by improving biomechanical conditions of the joint without the risk of osteonecrosis of the femoral head. The original technique was described as a Smith-Petersen approach and included partial detachment of the tensor fascia and gluteus medius and detachment of the tendon of the rectus femoris muscle in its direct and reflected parts.1 Although good results have been reported, this surgical technique can result in complications: neurovascular injuries have been reported, as well as over- or undercorrection, nonunion, heterotopic ossification, acetabular necrosis, and related surgical wounds, such as dehiscence, resuture, and alterations in healing, often generating wide, hypertrophic, and very visible scars.2,3,4
Several modifications have been made to the original surgical approach described for this technique, such as direct anterior, the shortened straight approach, and the double ilioinguinal approach.5,6,7,8,9 The principal author modified this procedure through an anterior approach with no detachment of rectus femoris, allowing early rehabilitation.10 However, none of the modifications fully resolved the complications resulting from the surgical lesions or the cosmetic appearance of the scar, which, in our experience, leads to functional problems as well as other concerns, such as patient satisfaction.
There are different determinants in the process of wound healing. The first relates to innate characteristics of the regenerative process, such as the tendency to produce hypertrophic or keloid scars, which is unpredictable and beyond the surgeon's control.11 Some underlying conditions such as immunodeficiency, chronic diseases, malnutrition, and drugs (eg, systemic corticosteroids) adversely affect the healing process. Furthermore, the surgeon can act on certain determinants and thus influence the esthetic result of the scar. These are relative to the tension of the skin in the area of the incision and must be taken into account when planning the approach. There are two types of tension in the normal skin, and they vary according to the anatomic region. The first is static tension, which follows a predictable pattern that was studied by Langer in 1861.12,13 These lines are defined by the arrangement of the collagen and elastic fibers forming the reticular dermis. The first is the static tension, which follows a predictable pattern that was studied by Langer, an Austrian anatomist, in 1861. These lines are defined by the arrangement of the collagen and elastic fibers forming the reticular dermis.12 Other studies subsequently emerged regarding static tension lines,13,14 such as the studies by Kraissl, which recommends incisions perpendicular to the direction of muscle contraction. In the pelvic region, groin, and proximal third of the thigh, the collagen orientation matches the perpendicular direction of the muscle fiber contraction.
The second type of tension is called dynamic and refers to the skin tension created by the movement of joints and muscles; both wounds that are perpendicular to the static tension and those that cross joints (dynamic pressure) generate wider and unsightly scars.14 Therefore, in the anterior region of the hip, groin, and proximal third of the thigh, the skin incision that would ensure a better esthetic and functional outcome would be the one that follows the tension lines in the same direction of the inguinal fold, ie, in the oblique cephalocaudal direction and from lateral to medial.
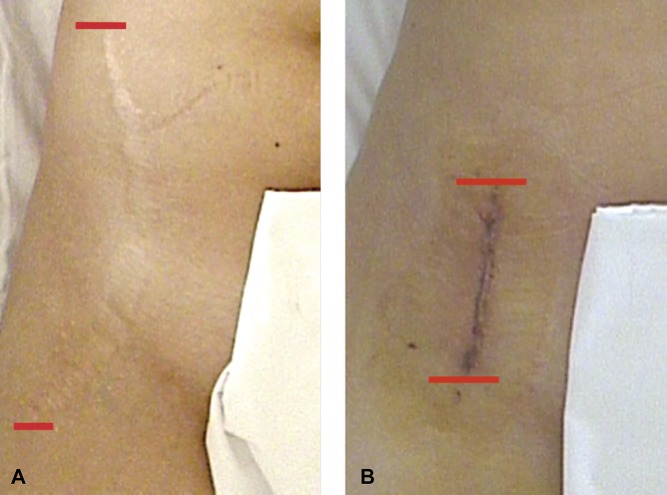
In an effort to solve this issue at our center, we have performed different types of incisions: longitudinal, shortened, and Z-shaped (Figure 1). Although the scars produced were shorter than the first ones, as well as esthetically acceptable, dehiscence and wide, hypertrophic scars persisted in a large number of patients. Following the principles of the tension lines of Langer, the principal author used an oblique inguinal incision, with the same direction of the inguinal crease, reducing both static and dynamic tension of the skin, allowing the edges of the wound to heal without tension, and avoiding the development of dehiscence or hypertrophic or esthetically unsatisfactory scars. In addition, this incision allowed the development of the surgical technique of acetabular reorientation safely and effectively and an adequate and sufficient exposure without increasing the complication rate.
Figure 1.
Intraoperative photographs demonstrating (A) the original incision and (B) the shortened incision.
Methods
Between January 2014 and January 2016, the principal author performed 35 Bernese periacetabular osteotomies in 27 patients (21 women and 6 men) in the Hip and Pelvis Unit of Clínica Alemana of Santiago. Chile. The average age of the patients was 27.09 years (range, 18 to 42 years). They all underwent an oblique inguinal anterior approach with a modified technique. No patients were excluded from the study.
Functional and esthetic results of the scar were assessed by measuring the length of the initial incision and then the diastasis of scar edges, obtaining an average between its widest and the narrowest part. The development of hypertrophic, depressed, and hyperpigmented scars was assessed, in addition to dehiscence and resuture events.
We conducted a survey of patient satisfaction regarding the patient's esthetic and functional opinion of the surgical wound and subsequent scar. AP pelvis and hip radiographs and false profiles were taken to measure the acetabular index, lateral center edge angle, anterior center edge, and medialization of the femoral head obtained after the acetabular reorientation.
Regarding the neurovascular injury, we determined the presence of symptoms related to lateral femoral injury of the cutaneous nerve (LFCN), such as paresthesias and dysesthesias of the lateral thigh. All patients had a minimum follow-up of 6 months (24.6 months).
Surgical Technique
With the patient supine on a radiolucent table, the iliac crest and anterior superior iliac spine (ASIS) are identified and delineated (Figure 2). The inguinal crease is identified and delineated by hip flexion. A line is drawn representing the medial projection of the lower edge of the iliac crest; a bisecting line is drawn between this line and the previously drawn line. An incision is made in the skin over this resulting bisector, leaving two thirds toward lateral and one third toward medial from a longitudinal line that represents the distal projection of the iliac crest. The fascia on the tensor fascia lata is dissected longitudinally, protecting the femoral cutaneous nerve, which moves medially with the sartorius. The tensor fascia lata is retracted laterally to expose the anterior rectus muscle and psoas muscle.
Figure 2.
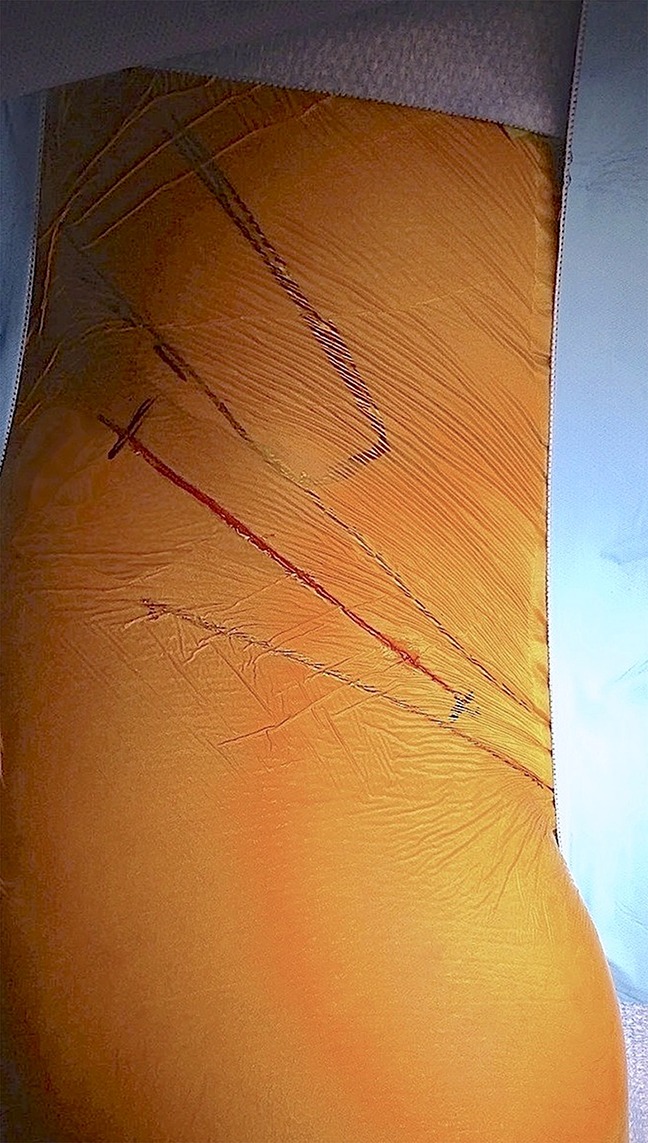
Intraoperative photograph demonstrating the oblique inguinal approach.
Using the moving window concept, the subcutaneous tissue and skin are moved proximally, exposing the ASIS and the insertion of the sartorius. An osteotomy of 1.5 × 2 cm is done at the level of the spine with an oscillating saw and a straight osteotome to move the insertion of the sartorius muscle and medially expose the region between the ASIS and anterior inferior iliac spine. The interval between the rectus femoris and psoas is dissected, medially retracting the lateral rectus femoris (in its direct and reflected portions) and the psoas muscle. When viewing the iliocapsularis muscle, it is retracted, exposing the joint capsule. From this point, as described in the original technique, the bone structures are identified and the corresponding osteotomies are performed.
Results
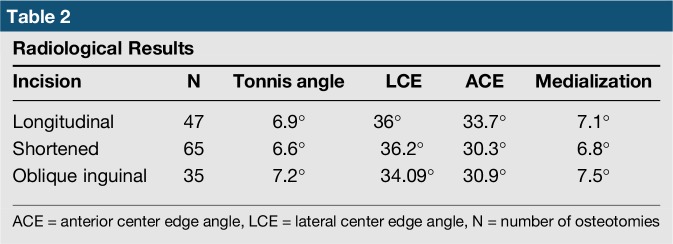
The average length of the scar was 14.1 cm (range, 11 to 16 cm), whereas the width (average diastasis) was 1.3 mm (range, 0.5 to 1,8 mm) (Figure 3). There were no hypertrophic, depressed, or hyperpigmented scars. No patients had dehiscence or resutures of the surgical wound. No patients with LFCN injuries were recorded (Table 1).
Figure 3.
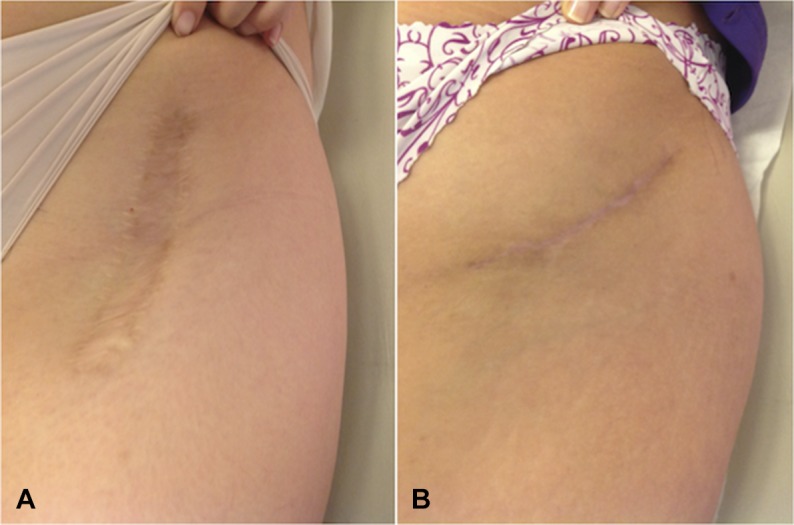
Postoperative photographs demonstrating scar diastasis after anterior (A) and inguinal (B) approaches.
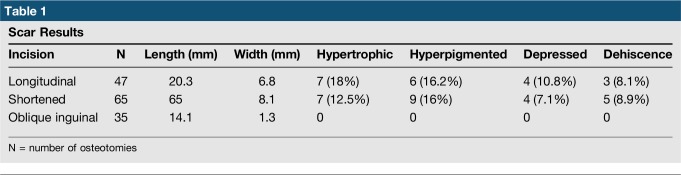
Table 1.
Scar Results
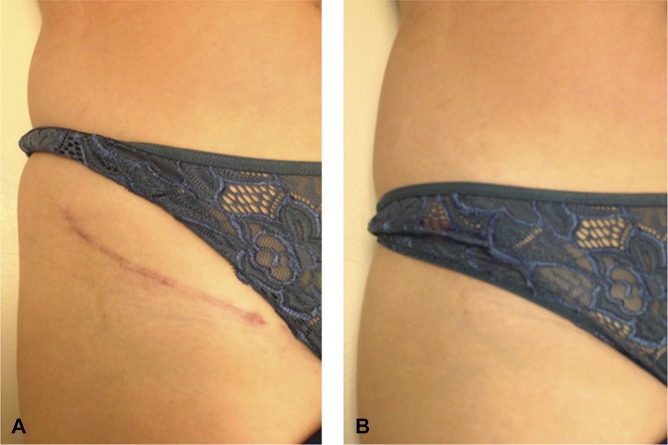
In the radiological assessment, the average Tonnis angle was 7.2° (range, 4.1° to 10.5°), lateral center edge angle, 34.09° (range, 29.7° to 38.3°), and anterior center edge angle, 30.9° (range, 28.8° to 34.2°). The average was 7.5 mm medialization2,3,4,5,6,7,8,9,10,11,12 (Figure 4, Table 2). In a targeted survey, 100% of patients confirmed being very satisfied with the esthetic appearance of the scar (Figure 5).
Figure 4.
Anteroposterior postoperative radiograph.
Table 2.
Radiological Results
Figure 5.
Preoperative (A) and postoperative (B) esthetic appearance of the scars.
Discussion
Several modifications to the original approach of Bernese periacetabular osteotomy have been described, which focused on decreasing the intraoperative bleeding and surgical time, exposing deep tissue, and shortening scars. Less intraoperative bleeding, transfusion requirement, and shorter scars have been reported with the shortened straight approach or minimally invasive approach. The dual approach is undertaken to minimize exposure of tissues and gain better access to the ischium and pubis sections. However, except for the work of Bernstein et al,8,9 who use the Vancouver scale to reflect the quality of the scar in a minimally invasive approach, we did not find publications in the literature focusing on the esthetics of the scar, morphological characteristics, and degree of patient satisfaction. Either way, the tendency to make incisions with a vertical orientation independent of its length and location results in wounds with tight edges that tend to separate, predisposing it to dehiscence and diastasis of the edges, with wide scars that are difficult to hide with regular clothing.
The oblique inguinal incision allows the natural coping with the edges of the surgical wound, thanks to its parallel orientation regarding voltage lines, avoiding dehiscence by decreasing both static and dynamic tension of the skin. This results in narrow scars without trophic changes or pigmentation in the absence of baseline alterations that could affect the normal healing process. On average, our patients had a scar width of 1.3 mm (range, 0.5 to 1.8 mm). Besides its location near the inguinal crease, this incision allows the scar to be completely hidden under the underwear, with a high rate of patient satisfaction.
Regarding the periacetabular osteotomy technique, we did not observe changes from the acetabular reorientation, allowing adequate exposure and access to the realization of the ASIS osteotomy and four periacetabular osteotomies. Our series showed a Tonnis index of 4.2° and lateral center edge angle of 34.09° on average. There were no patients with neurologic symptoms related to LFCN, which is related to proper identification and protection of this nerve when performing this technique.
Conclusion
Oblique inguinal incision for an anterior approach in Bernese periacetabular osteotomy is a technique that allows healing of surgical wounds without dehiscence or hypertrophic changes by respecting tension lines. It has a high rate of patient satisfaction, with no complications resulting from this modification. This technique also allows acetabular reorientation with an adequate tissue exposure, providing radiological and clinical results comparable to those of the original technique.
Footnotes
Dr. Lara or an immediate family member serves as a paid consultant to Stryker. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Villegas, Dr. Besomi, and Dr. Tobar.
References
- 1.Ganz R, Klaue K, Vinh TS, Mast JW: A new periacetabular osteotomy for the treatment of hip dysplasias: Technique and preliminary results. Clin Orthop 1988;232:26-36. [PubMed] [Google Scholar]
- 2.Davey JP, Santore RF: Complications of periacetabular osteotomy. Clin Orthop Relat Res 1999;363:33-37. [PubMed] [Google Scholar]
- 3.Biedermann R, Donnan L, Gabriel A, Wachter R, Krismer M, Behensky H: Complications and patient satisfaction after periacetabular pelvic osteotomy. Int Orthop 2008;32:611-617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thawrani D, Sucato DJ, Podeszwa DA, DeLaRocha A: Complications associated with the Bernese periacetabular osteotomy for hip dysplasia in adolescents. J Bone Joint Surg Am 2010;92:1707-1714. [DOI] [PubMed] [Google Scholar]
- 5.Hussell JG, Mast JW, Mayo KA, Howie DW, Ganz R: A comparison of different surgical approaches for the periacetabular osteotomy. Clin Orthop Relat Res 1999;363:64-72. [PubMed] [Google Scholar]
- 6.Pogliacomi F, Stark A, Vaienti E, Wallensten R: Periacetabular osteotomy of the hip: The ilioinguinal approach. Acta Biomed 2003;74:38-46. [PubMed] [Google Scholar]
- 7.Ko JY, Wang CJ, Lin CF, Shih CH: Periacetabular osteotomy through a modified ollier transtrochanteric approach for treatment of painful dysplastic hips. J Bone Joint Surg Am 2002;84:1594-1604. [DOI] [PubMed] [Google Scholar]
- 8.Bernstein P, Thielemann F, Günther K-P: A modification of periacetabular osteotomy using a two-incision approach. Open Orthopaedics J 2007;1:13-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernstein P, Thielemann F, Ghunter K: A less-invasive approach to periacetabular osteotomy in DDH. J Bone Joint Surg Br. Orthopaedic Proceedings 2009; vol. 91-B no. SUPP I 29. [Google Scholar]
- 10.Lara J, Tobar C, Besomi J: Bernese periacetabular osteotomy for hip dysplasia: A modification to original technique and South American perspective. Curr Rev Musculoskelet Med 2014;7:337-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Son D, Harijan A: Overview of surgical scar prevention and management. J Korean Med Sci 2014;29:751-757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Langer K: On the anatomy and physiology of the skin. I. The cleavability of the cutis. Br J Plast Surg. 1978;31:3–8 (Translation of).Zur Anatomie und Physiologie der Haut. I. Uber die Spaltbarkeit der Cutis. Sitzungsbericht der Mathematisch-naturwissenschaftlichen Classe der Kaiserlichen Academie der Wissenschaften. 1861;44:19. [PubMed] [Google Scholar]
- 13.Wilhelmi BJ, Blackwell SJ, Phillips LG: Langer's lines: To use or not to use. Plast Reconstr Surg 1999;104:208-214. [PubMed] [Google Scholar]
- 14.Kraissl CJ: The selection of appropriate lines for elective surgical incisions. Plast Reconstr Surg 1946;81:1-28. [DOI] [PubMed] [Google Scholar]