Abstract
Introduction:
With increasing utilization of surgery centers, it is important to demonstrate the safety of outpatient shoulder surgery in freestanding ambulatory surgery centers. No studies have specifically looked at the Medicare-age population and the rate of outpatient shoulder procedure complications in these patients at an ambulatory surgery center.
Methods:
Six hundred forty patients were included in our study between 2000 and 2015. The incidence of major complications was identified, including acute infection requiring intravenous antibiotics or irrigation and débridement, postoperative transfer to a hospital, wrong-site surgical procedures, retention of a foreign object, postoperative symptomatic thromboembolism, medication errors, and bleeding/wound complications.
Results:
There was a total of seven occurrence reports in seven patients, for a reported adverse event rate of 1.01%.
Conclusions:
Our findings are consistent with currently reported outpatient hospital-based data and illustrate the safety of outpatient shoulder procedures at a freestanding ambulatory surgery center in Medicare-age patients.
Outpatient shoulder surgeries such as rotator cuff repair and shoulder arthroscopy are some of the most commonly performed procedures in the United States.1 Over the past two decades, there has been a significant shift from inpatient to outpatient surgery for rotator cuff repair—the most commonly performed outpatient shoulder surgery.1,2 Overall, outpatient shoulder surgeries have been shown to be safe, with a low rate of complications ranging from 2.1% for open rotator cuff repair and 0.99% for shoulder arthroscopy in general.3,4,5 A recent article by Rubenstein et al6 found that patients aged 60 years or older who underwent shoulder arthroscopy also have a low overall 30-day postoperative complication rate of 1.6%.
A 2006 survey by the Centers for Disease Control found that 43% of all outpatient surgical procedures were performed in freestanding ambulatory surgery centers.7 The Agency for Healthcare Research and Quality notes that outpatient surgeries made up 65% of all surgeries performed in 2012, up from 54% in 1992.1 Medicare pays higher rates to hospital outpatient departments than to ambulatory surgery centers for equivalent procedures. In 2015, Medicare reimbursed ambulatory surgery centers an overall average of 55% of what it reimbursed hospital outpatient departments for outpatient shoulder procedures based on Current Procedural Terminology coding.8,9
A recent article by Robinson et al notes that because of the cost savings provided by ambulatory surgery centers, California has implemented “reference-based benefit designs,” by which insurers limit the contribution that they will pay, requiring the patient to pay the difference. This policy change resulted in a 9.9% increase in utilization of freestanding ambulatory shoulder centers for shoulder arthroscopy with a corresponding decrease in the use of hospital outpatient departments. The safety of shoulder and of knee arthroscopies at freestanding ambulatory centers was equivalent to hospital outpatient departments.10 A review done at our freestanding ambulatory surgery center demonstrated an adverse event rate of 0.20% for 28,737 outpatient upper extremity procedures done over an 11-year period.11 Of note, the study included all outpatient shoulder, elbow, wrist, and hand procedures but did not stratify for patient age.
Ambulatory surgery centers served 3.3 million Medicare beneficiaries in 2008, a 2.8% increase from 2007. The number of Medicare-certified centers totaled 5,175 in 2008, an increase of 3.7% from 2007.12 With increasing utilization of surgery centers, it is important to demonstrate the safety of outpatient shoulder surgery in freestanding ambulatory surgery centers in patients older than 65 years. The perception in a March 2016 report by the Medicare Payment Advisory Commission to Congress on Medicare and ambulatory surgery centers was that there are insufficient data to evaluate quality of care in ambulatory surgery centers.12 To our knowledge, no studies have specifically looked at the Medicare-age population and the rate of outpatient shoulder procedure complications at an ambulatory surgery center. We hypothesized that a low rate of adverse events can be achieved in the ambulatory setting in Medicare-age patients.
Methods
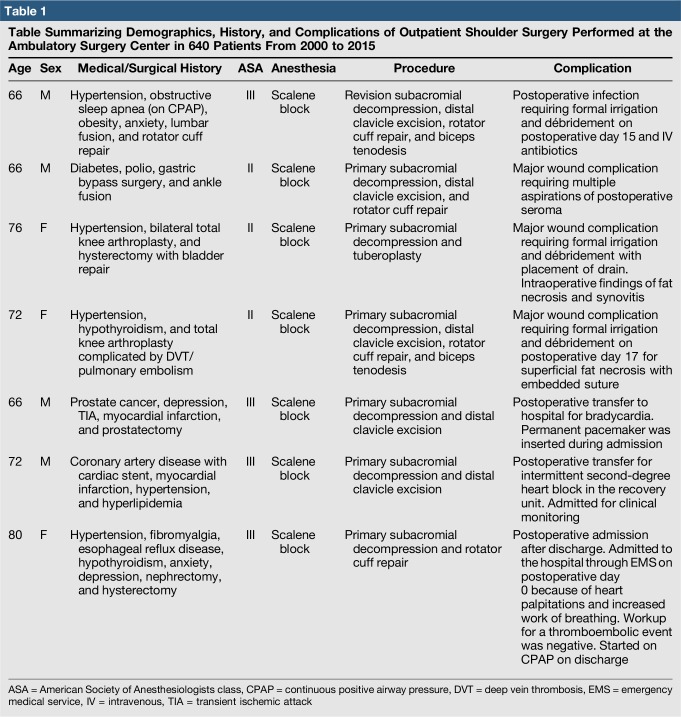
After Institutional Review Board approval was obtained, a retrospective review of shoulder cases in Medicare-age patients aged 65 years and older was performed by two board-certified hand and upper extremity surgeons at a single freestanding ambulatory surgery center over a 15-year period (2000–2015) (Table 1). The procedures included subacromial decompression, distal clavicle excision, biceps tenodesis, primary and revision rotator cuff repair (open and arthroscopic), tuberoplasty, and shoulder arthroscopy.
Table 1.
Table Summarizing Demographics, History, and Complications of Outpatient Shoulder Surgery Performed at the Ambulatory Surgery Center in 640 Patients From 2000 to 2015
Predominantly, upper extremity surgical procedures are performed at this facility. However, ophthalmologic, urologic, and pain management surgical procedures are also performed. The surgery center is an independent, freestanding facility. The two contributing surgeons have partial ownership, and the hand surgery group is academically affiliated with the University of Pittsburgh. They train plastic surgery residents and hand surgery fellows. There are two board-certified anesthesiologists who perform regional and general anesthesia. They simultaneously supervise nurse anesthetists in up to four operating rooms, consistent with the Centers for Medicare & Medicaid Services guidelines. Anesthesia for shoulder procedures is typically an interscalene regional block with sedation. General anesthesia is occasionally required in patients with obstructive sleep apnea.
Depending on the patient's medical comorbidities, the surgeons obtain preoperative clearance by a primary care physician or cardiologist. The anesthesiologists determine the patient's appropriateness for the surgery center. Over the past 15 years, the ambulatory surgery center has relaxed its restrictions based on comorbidities. Although reviewed by the anesthesiologists, most patients with obstructive sleep apnea, therapeutic anticoagulation, and coagulopathies will undergo their procedures at the ambulatory surgery center. The anesthesiologists review chronic kidney disease, morbid obesity with body mass index > 45, or cardiac disease on a case-by-case basis. All patients with a reported latex sensitivity undergo radioallergosorbent testing. Patients with a true latex allergy, severe lung disease with home oxygen dependence, quadriplegia, active infection (ie, methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, or Clostridium difficile), or an American Society of Anesthesiologists (ASA) physical status classification of IV are not permitted to have their procedure performed at the facility. There are no restrictions against patients with a history of methicillin-resistant S aureus.
From 2000 to 2015, the anesthesiologists reviewed 682 Medicare-age patients who underwent the aforementioned procedures included in the study. Forty-two patients were risk-stratified to the local hospital. We included all the 640 procedures that were performed at the ambulatory surgery center in our analysis. Of these cases, 100% of the cases were elective. We excluded procedures that were canceled in the preoperative holding area before the administration of anesthesia from our adverse event analysis. Adverse events were defined as serious complications causing harm to a patient or leading to additional treatment. We identified adverse events by reviewing monthly occurrence reports. These are collected from every office at least 30 days from the day of surgery. All these adverse events were reported to the state. As in our previous study11 using state reportable adverse event criteria as a guideline, we divided these into seven main categories: major acute infections (defined as requiring formal irrigation and débridement in the operating room or inpatient admission for intravenous antibiotics), postoperative transfer or admission to a hospital, wrong-site surgical procedures, retention of a foreign object, postoperative symptomatic thromboembolism, medication errors, and noninfectious wound or bleeding complications requiring a subsequent procedure. Infections that required only oral antibiotics were defined as minor and not major adverse events. In addition, because these minor infections were inconsistently reported, we did not include them in our analysis. Medication sensitivities that did not result in hospital admission were defined as minor occurrences and were therefore not included in our analysis. These adverse events were then reviewed. We evaluated whether they led to emergency department visits, further laboratory testing, hospital admission, return to the operating room, and permanent physical or mental disability.
Results
Canceled Cases
From the 640 cases scheduled, there were 5 cases (0.78%) canceled by the anesthesiologist in the preoperative holding area before the administration of anesthesia. Of these cases, 100% were canceled for medical reasons. Two patients were found to have hypertension. One patient was found to have new heart murmur on preoperative physical examination. One patient was found to be in atrial flutter on preoperative electrocardiogram. One patient was canceled for clearance by pain management. In each of these cases, the procedure was rescheduled and successfully completed at a later date at the ambulatory surgery center without complication.
Adverse Events
Of the 640 cases, there was a total of seven occurrence reports in seven patients for a reported major adverse event rate of 1.09% (Figures 1 and 2). The anesthesiologists at the ambulatory surgery center preoperatively evaluated all seven patients. They determined that none of the patients required additional preoperative clearance from a cardiologist or primary care doctor. Three patients were classified as ASA class II. Four patients were classified as ASA class III. Patients in whom an adverse event occurred ranged in age from 66 to 80 years, with a mean age of 71 years. Among the 640 patients included in the study, 21 patients (3.3%) were classified as ASA class I, 330 patients (51.5%) were classified as ASA class II, and 289 patients (45.2%) were classified as ASA class III. The total age range of all 640 patients was 65 to 92 years, with a mean age of 71.7 years.
Figure 1.
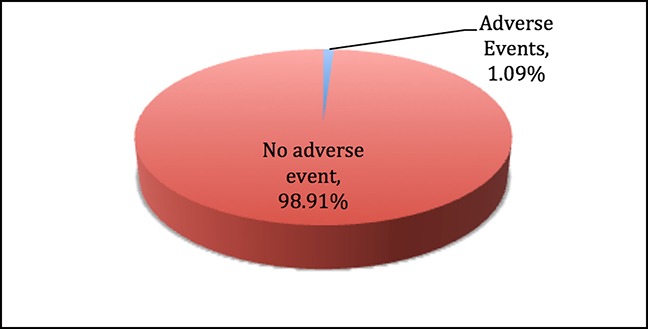
Pie chart showing the overall percentage of adverse events of 640 cases performed.
Figure 2.
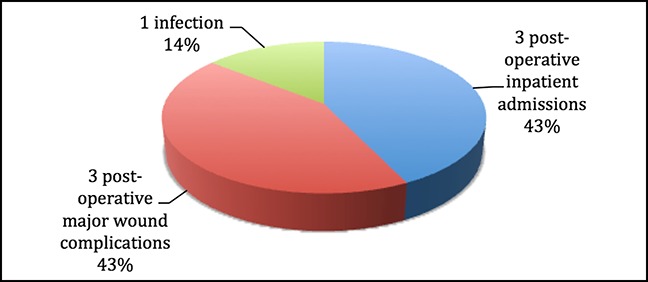
Pie chart showing categorization of a total of 7 adverse events of 640 cases performed.
Infection
One patient with a major infection required intravenous antibiotics or return to the operating room, for a rate of 0.16%. This patient underwent irrigation and débridement in the operating room after wound breakdown 15 days after revision arthroscopic rotator cuff repair, subacromial decompression, distal clavicle excision, and biceps tenodesis. In the setting of low-grade fevers and intraoperative findings of fat necrosis and devitalized muscle, the patient was admitted to the hospital for intravenous antibiotics, infectious disease evaluation, and insertion of a PICC line.
Major Wound-healing Complications
There were three patients (0.47%) with postoperative collection formation. One patient developed a postoperative seroma after mini-open rotator cuff repair and subacromial decompression that was aspirated multiple times in the office (culture negative) and resolved. Two patients were taken back to the operating room (0.31%) for complications related to persistent wound drainage. One underwent superficial irrigation and débridement of fat necrosis and Vicryl suture removal after mini-open rotator cuff repair. The other underwent irrigation and débridement of synovitis and fat necrosis with placement of a Jackson-Pratt drain due to continued drainage from arthroscopy incision after tuberoplasty.
Postoperative Transfer or Admission to a Hospital
Two patients required postoperative transfer to the hospital from the ambulatory surgery center. This led to a postoperative total transfer rate of 0.31%. Both patients were transferred from the postanesthesia care unit to the hospital for cardiac abnormalities. Both patients were classified as ASA class III and underwent regional nerve block with monitored anesthesia care sedation. Both underwent primary open distal clavicle excision and subacromial decompression. One patient was a 66-year-old man with a history of myocardial infarction, prostate cancer, and transient ischemic attack who developed postoperative bradycardia in the recovery unit. This patient required insertion of a permanent pacemaker while an inpatient. The other patient was a 72-year-old man with a history of myocardial infarction after percutaneous stent, hypertension, and hyperlipidemia who underwent primary subacromial decompression and distal clavicle excision. He was found to be in intermittent second-degree heart block in the recovery room.
One patient was admitted to the hospital in the immediate postoperative period (within 7 days of the surgical procedure), leading to a rate of 0.16% of postoperative admissions. The patient was classified as ASA class III and underwent regional nerve block. She was an 80-year-old woman with a history of hypertension, fibromyalgia, anxiety, depression, hypothyroidism, esophageal reflux disease, and hysterectomy complicated by bladder injury, necessitating repair. She underwent mini-open rotator cuff repair and subacromial decompression. On returning home the same day, she developed palpitations and shortness of breath. She was transported from home to the emergency department using an ambulance and admitted for hypoxia requiring oxygen and continuous positive airway pressure. A chest CT was negative for pulmonary embolism. All other workup was negative.
Wrong-site Surgical Procedure
There were no cases of wrong-site surgical procedures reported among 640 cases performed.
Medication Error
There were no cases of medication administration errors reported among 640 cases performed.
Postoperative Symptomatic Thromboembolism
There were no cases of postoperative symptomatic thromboembolism among 640 cases performed.
Retention of a Foreign Object
There were no cases of retained foreign objects.
Discussion
Our results demonstrate that outpatient shoulder surgery performed at an ambulatory surgery center in a population older than 65 years is safe. A total of 93.8% of Medicare-age patients (640/682) had their procedures performed at the ambulatory surgery center rather than as an outpatient procedure at the local hospital. Our adverse event rate of 1.09% is consistent with existing data. In particular, our data compare with recent results published by Rubenstein et al,6 which found an overall 1.6% rate of any adverse event in shoulder arthroscopy in patients older than 60 years in a hospital-based data set of 7,867 patients of the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP). In contrast to categorizing by state reportable events, they categorized adverse events by severe adverse events (1.1%), minor adverse events (1.1%), infectious adverse events (0.2%), and any adverse events (1.6%). Our infection event rate of 0.16% is comparable with their rate of 0.2% and with those of other studies, which range from 0% to 3.4%.4,13 Our rate of return to the operating room of 0.47% was comparable with that of an NSQIP study of 9,410 patients who underwent shoulder arthroscopy (0.31%) and to a hospital-based study on open versus arthroscopic rotator cuff repair in veterans by Owens et al3 and Martin et al.14 They found a rate of return to the operating room within 30 days at 1.1% in open repair and 0.5% in arthroscopic.
We had no thromboembolic complications within our study, which further demonstrates the extreme rarity of deep vein thrombosis and pulmonary embolism in outpatient surgery, as shown by Randelli et al,15 with a rate of 0.16% in 9,385 shoulder arthroscopies. There were no cases of wrong-site surgical procedures or medication errors reported. In this ambulatory surgery center, the attending surgeon marks the patient in preoperative holding. A surgical timeout reconfirming the laterality is done in the operating room before incision. All allergies and antibiotic dosing are confirmed with the surgical team in the timeout before incision.
There are relatively few studies that analyze data from ambulatory surgery centers. Policies such as those enacted in California have pushed patients and payers toward the cost efficiency of ambulatory surgery centers. Thus, it behooves the academic community to look at data beyond hospital-based data repositories. We have demonstrated in a previous study the safety of outpatient upper extremity procedures at an ambulatory surgery center.11 The present study further illustrates safety in a Medicare-age population, a group traditionally higher risk for complications in the setting chronic medical comorbidities. Our study demonstrates the safety of outpatient shoulder surgery in a freestanding ambulatory surgery center in Medicare-age patients. As previously acknowledged, the specialization of ambulatory surgery centers in a specific set of procedures lends itself to increased efficiency and familiarity with their routine performance. With greater specialization and efficiency come better communication and coordination among staff.13,16 A small staff at a sub-specialty ambulatory surgery center lends itself to developing better performance and efficiency. Hair et al17 found that procedures performed in freestanding ambulatory surgery centers take 39% less total time than do those in hospital-based outpatient departments.
There are limitations to our retrospective study. In comparison with the NSQIP database used by other studies, the power of our 640 cases is somewhat limiting. However, our adverse event rates are reflective of those other, higher-powered studies.
This study raises questions regarding the necessity of inpatient admission for other shoulder surgeries in the Medicare population. Brolin et al18 have demonstrated the safety of outpatient total shoulder arthroplasty in a select population with an average of 52.6 years old (range, 33 to 68 years). Total shoulder arthroplasty is a procedure that is frequently performed in the Medicare-age population. Previous studies focused on complications in the Medicare patient demonstrate a 0.09% risk of in-patient mortality and a venous thromboembolus risk of 0.53% after shoulder arthroplasty.19 In demonstrating the safety of outpatient shoulder arthroscopy and rotator cuff repairs in patients older than 65 years, our study raises questions about the potential for outpatient shoulder arthroplasty in patients older than 65 years.
Footnotes
Dr. Imbriglia or an immediate family member serves as a board member, owner, officer, or committee member of American Academy of Orthopaedic Surgeons and the American Society for Surgery of the Hand; is a member of a speakers' bureau or has made paid presentations on behalf of Auxilium; and has stock or stock options held in MiMedx. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. K. L. Buterbaugh, Dr. Liu, Dr. Krajewski, and Dr. G. A. Buterbaugh.
References
- 1.Wier LM, Steiner CA, Owens PL: Surgeries in Hospital-Owned Outpatient Facilities, 2012. Statistical Brief #188. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality, Rockville, MD, 2015. www.hcup-us.ahrq.gov/reports/statbriefs/sb188-Surgeries-Hospital-Outpatient-Facilities-2012.jsp. [Google Scholar]
- 2.Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL: National trends in rotator cuff repair. J Bone Joint Surg Am 2012;94:227-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Owens BD, Williams AE, Wolf JM: Risk factors for surgical complications in rotator cuff repair in a veteran population. J Shoulder Elbow Surg 2015;24:1707-1712. [DOI] [PubMed] [Google Scholar]
- 4.Moen TC, Rudolph GH, Caswell K, Espinoza C, Burkhead WZ, Krishnan SG: Complications of shoulder arthroscopy. J Am Acad Orthop Surg 2014;22:410-419. [DOI] [PubMed] [Google Scholar]
- 5.Shields E, Thirukumaran C, Thorsness R, Noyes K, Voloshin I: An analysis of adult patient risk factors and complications within 30 days after arthroscopic shoulder surgery. Arthroscopy 2015;31:807-815. [DOI] [PubMed] [Google Scholar]
- 6.Rubenstein WJ, Pean CA, Colvin AC: Shoulder arthroscopy in adults 60 or older: Risk factors that correlate with postoperative complications in the first 30 days. Arthroscopy 2017;33:49-54. [DOI] [PubMed] [Google Scholar]
- 7.Cullen KA, Hall MJ, Golosinskiy A: Ambulatory surgery in the United States, 2006. Natl Health Stat Rep 2009:1-25. [PubMed] [Google Scholar]
- 8.CMS Fee for Schedule Report: CMS-1613-CN (2-24-15) HOPPS Addendum A and B. U.S. Centers for Medicare & Medicaid Services, Baltimore, MD, 2015. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ASCPayment/ASC-Regulations-and-Notices-Items/CMS-1613-CN.html?DLPage=1&DLSort=2&DLSortDir=descending. [Google Scholar]
- 9.CMS Fee for Schedule Report: CMS-1613-CN (2-24-15) ASC Addendum AA, BB, DD1, DD2, and EE. U.S. Centers for Medicare & Medicaid Services, Baltimore, MD, 2015. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ASCPayment/ASC-Regulations-and-Notices-Items/CMS-1613-CN.html?DLPage=1&DLSort=2&DLSortDir=descending. [Google Scholar]
- 10.Robinson JC, Brown TT, Whaley C, Bozic KJ: Consumer choice between hospital-based and freestanding facilities for arthroscopy: Impact on prices, spending, and surgical complications. J Bone Joint Surg Am 2015;97:1473-1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goyal KS, Jain S, Buterbaugh GA, Imbriglia JE: The safety of hand and upper-extremity surgical procedures at a freestanding ambulatory surgery center: A review of 28,737 cases. J Bone Joint Surg Am 2016;98:700-704. [DOI] [PubMed] [Google Scholar]
- 12.U.S. Department of Health and Human Services: Medicare Ambulatory Surgical Center Value-Based Purchasing Implementation Plan. U.S. Centers for Medicare & Medicaid Services, Baltimore, MD, 2016. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ASCPayment/Downloads/C_ASC_RTC-2011.pdf. [Google Scholar]
- 13.Munnich EL, Parente ST: Procedures take less time at ambulatory surgery centers, keeping costs down and ability to meet demand up. Health Aff (Millwood) 2014;33:764-769. [DOI] [PubMed] [Google Scholar]
- 14.Martin CT, Gao Y, Pugely AJ, Wolf BR: 30-day morbidity and mortality after elective shoulder arthroscopy: A review of 9410 cases. J Shoulder Elbow Surg 2013;22:1667-1675.e1. [DOI] [PubMed] [Google Scholar]
- 15.Randelli P, Castagna A, Cabitza F, Cabitza P, Arrigoni P, Denti M: Infectious and thromboembolic complications of arthroscopic shoulder surgery. J Shoulder Elbow Surg 2010;19:97-101. [DOI] [PubMed] [Google Scholar]
- 16.Gawande A: Better: A Surgeon's Notes on Performance. New York, Picador, 2007. [Google Scholar]
- 17.Hair B, Hussey P, Wynn B: A comparison of ambulatory perioperative times in hospitals and freestanding centers. Am J Surg 2012;204:23-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brolin TJ, Mulligan RP, Azar FM, Throckmorton TW: Neer award 2016: Outpatient total shoulder arthroplasty in an ambulatory surgery center is a safe alternative to inpatient total shoulder arthroplasty in a hospital: A matched cohort study. J Shoulder Elbow Surg 2016;26:204-208. [DOI] [PubMed] [Google Scholar]
- 19.McCormick F, Nwachukwu BU, Kiriakopoulos EB, Schairer WW, Provencher MT, Levy J: In-hospital mortality risk for total shoulder arthroplasty: A comprehensive review of the medicare database from 2005 to 2011. Int J Shoulder Surg 2015;9:110-113. [DOI] [PMC free article] [PubMed] [Google Scholar]