Abstract
Background:
Bicondylar tibial plateau fractures have been treated with either plating or external fixation techniques, with conflicting results. A recently introduced technique involving the combined use of intramedullary nailing via a suprapatellar approach and condylar bolts could represent a new pathway toward better treatment of this severe injury.
Methods:
The present report describes a retrospective and prospective study of all 17 patients (age range, 25 to 75 years) who were admitted under the author’s care for the treatment of a closed, bicondylar tibial plateau fracture between 2013 and 2015. All patients consented to undergo fixation of the fracture with intramedullary nailing through a suprapatellar approach and with use of condylar bolts. The reconstructed articular surface was supported with freeze-dried allograft that had been previously soaked in concentrated bone marrow. The patients were followed at regular intervals, and the results were assessed with the Knee injury and Osteoarthritis Outcome Score (KOOS).
Results:
All patients were followed for at least 1 year (average and standard deviation, 25.23 ± 8.95 months; range, 12 to 46 months). All fractures united clinically and radiographically between 10 and 22 weeks (average, 15.1 ± 2.91 weeks), with no instances of neurovascular complication, infection, or implant failure. One patient underwent early revision of the fixation because of unsatisfactory reduction of the articular surface, and 1 patient had secondary fracture displacement. One condylar bolt was removed after fracture healing because of irritation at the insertion site. However, all patients regained knee motion without physiotherapy and all were fully weight-bearing by the fifth postoperative month.
Conclusions:
The short and intermediate-term results associated with the use of the proposed technique appear to be satisfactory. However, the effectiveness of the technique should be reassessed with long-term studies as well as comparative studies involving other fixation techniques.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
A bicondylar fracture of the tibial plateau (AO/OTA type 41C or Schatzker types V and VI)1,2 is a severe injury of the knee joint. Internal fixation with open or minimally invasive plating techniques and circular or hybrid external fixation constructs have been used for the treatment of this injury, with conflicting results3-11.
Efforts to improve the existing implants and techniques and/or to find new options that could offer better outcomes while reducing the morbidity and complication rates have been ongoing for years. A novel surgical technique involving the use of intramedullary nailing and condylar bolts has been proposed and biomechanically tested12-16.
The present report describes the short and intermediate-term results of treatment of bicondylar tibial plateau fractures with use of this new technique. The limitations and potential benefits of the technique are also discussed.
Materials and Methods
Surgical Technique
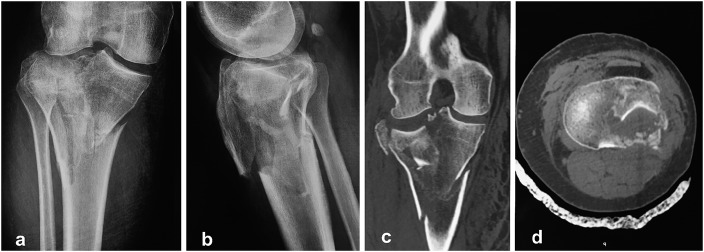
Detailed preoperative planning with use of anteroposterior and lateral radiographs and computed tomography (CT) scans of the knee joint is essential in any case of tibial plateau fracture (Fig. 1).
Fig. 1.
Figs. 1 and 3 through 7 Case 17. Figs 1-A through 1-D Preoperative anteroposterior and lateral radiographs (Figs. 1-A and 1-B) and CT scans (Figs. 1-C and 1-D) showing a complex biocondylar tibial plateau fracture with substantial articular impaction.
The patient is positioned on the operating table in the supine position, with a noninflated tourniquet at the thigh of the injured limb, gentle traction on the foot, and the knee joint in about 10° to 20° of flexion, with the other lower limb flexed and abducted (Fig. 2). After preparation and dressing of the injured limb, the area between the distal part of the femur and the ankle joint should be freely accessible. The metaphyseal-diaphyseal fractured area is usually satisfactorily reduced via traction with ligamentotaxis while a non-impacted articular surface can be reduced percutaneously with the use of a pelvic clamp. If there is articular impaction, the depressed articular surface can be elevated and restored with a lever under image-intensifier control (Fig. 3) through a cortical window (which usually has already been formed as a result of the fracture). Bone graft is then inserted to support the restored articular surface; freeze-dried cancellous allograft that has been soaked in concentrated bone marrow is preferred17. A condylar bolt is then inserted from medial to lateral, 0.5 to 1.0 cm distal to the articular surface in the coronal plane and at the posterior half of the tibial plateau in the sagittal plane. In cases associated with extensive articular involvement, an additional condylar bolt can be used (Fig. 4). The bolt or bolts should support adequately sized posteromedial or posterolateral fragments, and care should be taken not to squeeze the tibial plateau. Intramedullary nailing is then performed through a suprapatellar approach to fix the nonarticular fracture of the proximal part of the tibia and to provide additional support to the articular surface. The entry portal for the intramedullary nail should be as proximal as possible at the anterior corner of the tibial plateau. Marked displacement or angulation at the metaphyseal area can be addressed with blocking or free lag screws (Fig. 5).
Fig. 2.

Photograph showing the positioning of the patient for the fixation of a bicondylar tibial plateau fracture.
Fig. 3.
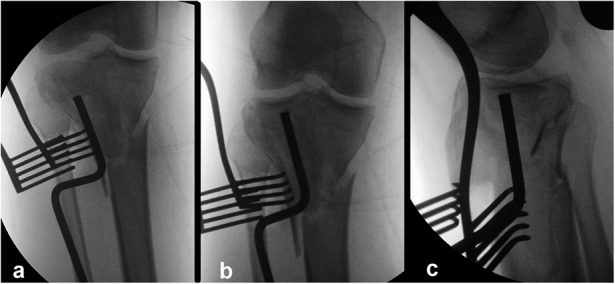
Figs. 3-A, 3-B, and 3-C Intraoperative radiographs. Fig. 3-A Anteroposterior radiograph showing elevation of the depressed articular surface with use of a lever that has been introduced via a lateral cortical window without opening the knee joint. Figs. 3-B and 3-C Anteroposterior (Fig. 3-B) and lateral (Fig. 3-C) radiographs made after the completion of the articular cartilage elevation.
Fig. 4.
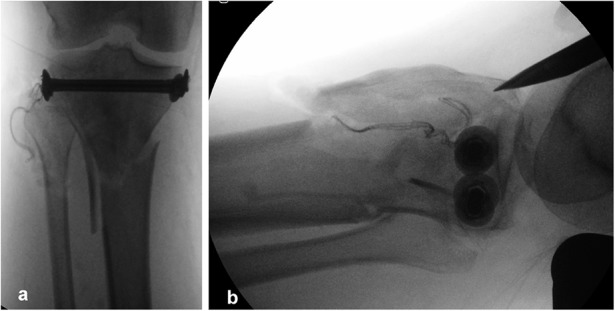
Figs. 4-A and 4-B Intraoperative anteroposterior (Fig. 4-A) and lateral (Fig. 4-B) radiographs made after the insertion of 2 compression bolts. The lateral radiograph also shows the entry point for the intramedullary nail. The fractured anterior metaphyseal area was treated with moderate release of the calcaneal traction and 2 anteroposterior free lag screws at a later stage as shown in Figure 5.
Fig. 5.
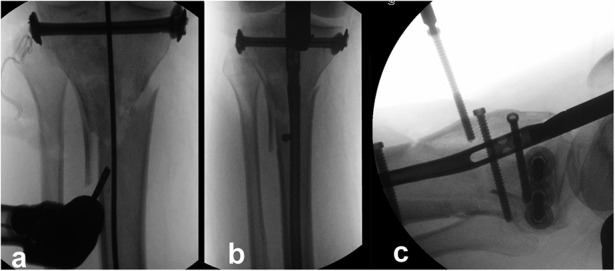
Figs. 5-A and 5-B Intraoperative anteroposterior radiographs showing substantial metaphyseal displacement, which was treated with an anteroposterior blocking screw. Fig. 5-C Fixation of the fractured anterior metaphyseal area was achieved with 2 free lag screws.
Motion of the knee joint and non-weight-bearing walking with crutches are initiated 48 to 72 hours after the operation. In cases of severely comminuted or osteoporotic fractures, a removable knee splint that allows full flexion and extension of the knee joint is provided for 4 to 6 weeks. Progression of weight-bearing depends on fracture severity and comminution. However, in general, partial weight-bearing starts at 6 weeks postoperatively and full weight-bearing starts at 10 to 12 weeks.
Study Group
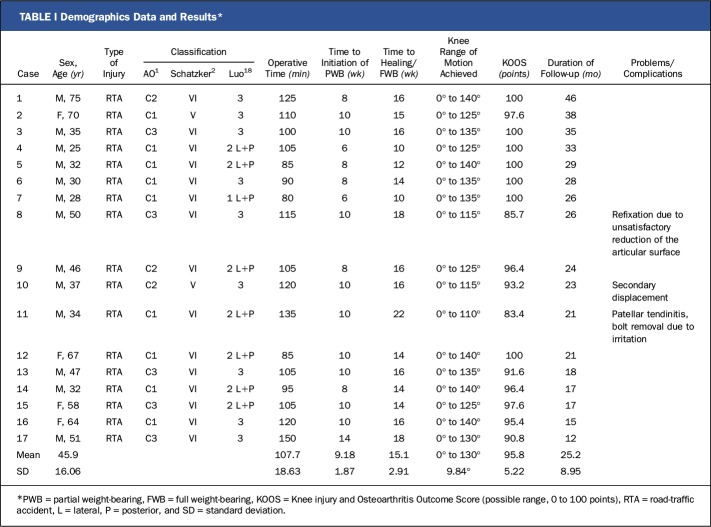
The present report describes a retrospective and prospective study that included all 17 patients (average age, 45.9 years; range, 25 to 75 years ) who were admitted under the author’s care for the treatment of a closed, bicondylar fracture of the tibial plateau from February 2013 to December 2015 (Table I). All patients consented to undergo fixation of the fracture with intramedullary nailing and condylar bolts and, in cases of impacted fractures, to undergo percutaneous aspiration of bone marrow from the iliac wing at the beginning of the operation. The fractures were classified according to the 3 most popular classification systems: AO/OTA1, Schatzker2, and Luo18 (Table I).
TABLE I.
Demographics Data and Results*
The operation was performed 3 to 18 days after the accident; the length of this interval depended predominantly on the severity of concomitant injuries and comorbidities and less on the local soft-tissue condition as the main incisions for the surgical procedure were away from the area where blisters or edema usually occur. The T2 tibial nail (Stryker) and condylar bolts (Stryker) were used in all cases.
Postoperatively, all patients started knee motion as pain allowed and remained non-weight-bearing for 6 weeks. Patients over the age of 60 years and those with complex fractures were provided with a removable hinged splint that could allow unrestricted range of knee motion for a period of 4 to 6 weeks.
Results
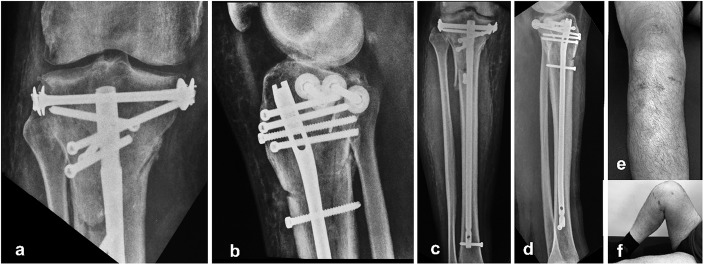
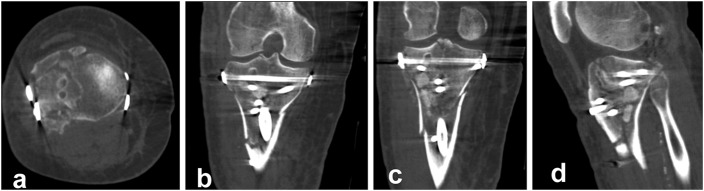
The mean operative time (and standard deviation) was 107.7 ± 18.63 minutes (range, 80 to 150 minutes). There were no intraoperative problems, and no patient received a blood transfusion during or after the operation. There were no instances of neurovascular complications, infection, or implant failure. Apart from the 3 patients who had complications (described below), all other patients regained extension and flexion of the knee joint by the second follow-up appointment at the outpatient clinic at 8 to 10 weeks postoperatively. All fractures healed clinically and radiographically by a mean of 15.1 ± 2.91 weeks (range, 10 to 22 weeks) postoperatively. The restoration of the articular surface and the alignment of the tibia were assessed with postoperative anteroposterior and lateral radiographs of the knee joint and the tibia (from the knee to the ankle). Apart from the case of 1 patient (Case 10), radiographs did not reveal loss of reduction in any of the other patients (Fig. 6). In 1 case, a detailed assessment of the quality of the articular restoration was performed with use of postoperative CT scanning, with the patient’s consent (Fig. 7).
Fig. 6.
Figs. 6-A through 6-F Images made at the time of the latest follow-up. Figs. 6-A and 6-B Anteroposterior (Fig. 6-A) and lateral (Fig. 6-B) radiographs of the knee joint. Figs. 6-C and 6-D Anteroposterior (Fig. 6-C) and lateral (Fig. 6-D) radiographs showing the entire tibia. Figs. 6-E and 6-F Photographs of the lower extremity, showing the restoration of the anatomy and the function of the knee joint as well as the minimal invasiveness of the technique.
Fig. 7.
Figs. 7-A through 7-D Postoperative CT scans showing almost anatomical reduction of the articular surface of the tibial plateau as shown on the transverse (Fig. 7-A), coronal (Figs. 7-B and 7-C) and sagittal (Fig. 7-D) views.
The patients were followed clinically and radiographically at 4 to 6-week intervals until fracture union and full mobilization and were re-examined at 6, 12, and 24 months thereafter. The mean duration of follow-up was 25.2 ± 8.95 months (range, 12 to 46 months). The mean range of motion of the knee joint at the time of the latest follow-up was 130° ± 9.84° (range, 110° to 140°).
In 1 patient (Case 8), refixation of the fracture was necessary because of unsatisfactory reduction of the articular surface, as shown on radiographs made 5 days after the initial operation (Table I). In another patient (Case 11), the condylar bolt was removed 1 year after fixation because of irritation at the posteromedial insertion site (Table I). The same patient had development of patellar tendinitis, Achilles tendinitis, and tenderness alongside the peroneal tendons of the ipsilateral leg when he started partial weight-bearing. These symptoms resolved 2 months later with physiotherapy treatment. In a third patient (Case 10), secondary displacement in the form of translation and varus angulation (10°) of the metaphyseal fractured area was noticed after the patient tried to bear weight early on his own initiative (Table I). All other patients regained extension and flexion of the knee joint by the second follow-up appointment at the outpatient clinic (8 to 10 weeks after surgery). Toe-touch to partial weight-bearing was allowed from the sixth to the fourteenth postoperative week, depending on the fracture pattern and the age of the patient. All patients were fully weight-bearing by the fifth postoperative month.
Function was assessed with use of the Knee injury and Osteoarthritis Outcome Score (KOOS)19. The mean score at the time of the latest follow-up was 95.8 ± 5.22 points (range, 83.4 to 100 points). At the time of the latest follow-up, all patients had resumed their preinjury activities and, apart from the patient who underwent removal of the compression bolt because of irritation on the medial site of the knee, no patient had removal of the internal fixation after fracture union.
Discussion
While it is generally accepted that bicondylar fractures of the tibial plateau should be operatively treated in order to minimize the risks of stiffness, deformity, and arthritis of the knee joint, there is no consensus about the optimal surgical technique10,20-22.
Conventional open reduction and internal fixation with dual plating has produced conflicting results as the extensive soft-tissue stripping can create problems that overshadow the benefits of satisfactory reduction of the articular surface and early mobilization of the knee joint5,23,24. The initial enthusiasm created by the introduction of minimally invasive plate osteosynthesis (MIPO) with locking plates was replaced by skepticism because of the high rates of complications such as deep infection (up to 18%), poor fracture reduction (up to 23%), the need for implant removal (up to 30%), and irritation at the implant site (up to 12%)8,9,25-28. In addition, clinical and biomechanical studies have shown that osteosynthesis with 1 lateral locking plate is not superior to the conventional double-plating technique, whereas removal of a locking plate and screws, whenever needed, always could be problematic16,29-31. Finally, lateral and/or medial incisions, bulky metalwork and its removal, and a substantial infection rate could create problems with wound-healing following a total knee arthroplasty procedure in the future32,33.
External fixators in the form of circular frames or hybrid constructs also have been used for the definitive treatment of bicondylar fractures of the tibial plateau5,34,35. However, patients do not tolerate bulky external devices that can interfere adversely with the mobilization of the knee and the rehabilitation program. Furthermore, fixators require continuous pin-track care and are associated with additional concerns related to the approximation of the wires to the knee joint, while loss of reduction and fracture malunion are not infrequent problems in patients with osteoporotic fractures36-38.
Combined use of intramedullary nailing and condylar bolts for the treatment of bicondylar tibial plateau fractures without severe articular depression has been described in 2 previous studies12,13. Intramedullary implants, being load-sharing devices, distribute axial forces evenly and allow early mobilization and weight-bearing, an important consideration especially for older patients. Furthermore, the infection rate after nailing is lower than that after plating or external fixation39. In the event of an open fracture, intramedullary nailing facilitates soft-tissue care better than a plate or a circular frame does. Finally, removal of an intramedullary nail and the condylar bolt is usually a straightforward procedure.
The initial suspicion that 3 proximal screws may not support the fractured articular surface adequately was not confirmed as there was no instance of articular displacement or collapse. Nevertheless, it seems that the condylar bolts, apart from reducing the articular surface and enhancing the fixation, act as a supportive adjunct for the articular surface. The T2 tibial nail (Stryker) that was used in all cases provided a very proximal bend and 3 proximal divergent screws for supporting the tibial plateau. However, a dedicated nail with more proximal locking screws that should be configured for supporting the restored tibial plateau, at the nearest distance to the proximal end of the nail, would have been a desirable design adjunct.
The patient’s positioning on the operating table for the suprapatellar approach not only enables closed reduction of the extra-articular part of the fracture (via traction) but also facilitates undisturbed and reproducible anteroposterior and lateral radiographs of the knee joint with the image intensifier during the operation. It also allows uneventful insertion of the nail through the fracture site at the proximal part of the tibia without displacing the fracture12. The suprapatellar (or retropatellar) nailing technique has been described recently as an alternative approach for the treatment of extra-articular proximal and diaphyseal tibial fractures40-44. Although it has been noted that there may be a substantive risk of damage to the articular cartilage of both the femoral condyles and the patella, the menisci, and the intermeniscal ligament, it has been acknowledged that the suprapatellar approach facilitates a correct starting point for the insertion of the tibial nail. In addition, with the suprapatellar approach, the patellar tendon is not under tension and therefore does not apply distractive forces that could further displace the fracture site anteriorly. With regard to the patellofemoral joint, Eastman et al. reported that no visual damage of the articular cartilage was observed in cadaveric knees following the insertion of a tibial nail through a retropatellar portal with the use of protective sleeves and careful surgical technique41. However, long-term studies of patients who have undergone intramedullary nailing with the suprapatellar technique may or may not confirm the initial observations regarding this technique.
Of the 3 studies that have confirmed the biomechanical advantages of the proposed technique, 2 investigated proximal tibial fractures with a metaphyseal-diaphyseal gap14,15, whereas the third16, with the participation of the author of the present study, involved the fixation technique described in the current report. The models in the third study were commercially prepared plastic bones with fracture planes that could be reduced with excellent contact; these models lacked articular or fracture-plane impaction or comminution. Because the fracture planes were sagittally or parasagittally oriented, such that transverse-locking bolts would be approximately perpendicular to the fracture plane, it would seem that similar bicondylar fractures in the clinical scenario might be associated with greater comminution, lower bone density, more impaction, and/or less-favorable fracture-plane location and orientation. However, it should be mentioned that the plastic models that were used in that study had biomechanical properties similar to good-quality cadaveric bones. The fracture pattern was selected to resemble a Schatzker type-VI fracture without articular depression, as at that time only fractures without articular depression were selected for treatment with suprapatellar nailing and condylar bolts. Following the favorable results of that biomechanical study and the encouraging outcomes for patients with non-impacted fractures, it was decided to expand the indications for the use of the proposed technique to all complex bicondylar fractures of the tibial plateau, regardless of the existence of articular depression.
One limitation of the present study is that the quality of reduction of the articular surfaces and tibial alignment were evaluated by means of visual assessment of intraoperative and postoperative radiographs. As inadequate articular restoration and malalignment can compromise function and long-term outcomes, measuring and correcting these parameters, predominantly intraoperatively, might be considered as future research for achieving better results45. Other limitations of the present study include the unblinded analysis of the results, the absence of a comparison group of patients managed with a traditional operative technique, and the relatively short duration of follow-up. Large studies comparing this technique with other surgical techniques over a longer period of time are needed.
The treatment of bicondylar fractures of the tibial plateau with intramedullary nailing and a condylar bolt or bolts via the suprapatellar approach requires good experience with intramedullary nailing. Therefore, adequate training is required before the adoption of this technique.
Overview
The combined use of intramedullary nailing and a condylar bolt (or bolts) can offer a reliable option for the treatment of bicondylar fractures of the tibial plateau and is associated with specific advantages. The next step is to perform clinical comparison studies involving other traditional fixation techniques in order to obtain further validation and assessment of the technique described in the present study.
Disclosure of Potential Conflicts of Interest
Footnotes
Investigation performed at the Orthopaedic Department, “Evangelismos” General Hospital, Athens, Greece
Disclosure: There was no external funding source for this study. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, the author checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJSOA/A9).
References
- 1.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007. Nov-Dec;21(10)(Suppl):S1-133. [DOI] [PubMed] [Google Scholar]
- 2.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968–1975. Clin Orthop Relat Res. 1979. Jan-Feb;138:94-104. [PubMed] [Google Scholar]
- 3.Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN. Complications after tibia plateau fracture surgery. Injury. 2006. June;37(6):475-84. Epub 2005 Aug 22. [DOI] [PubMed] [Google Scholar]
- 4.Mahadeva D, Costa ML, Gaffey A. Open reduction and internal fixation versus hybrid fixation for bicondylar/severe tibial plateau fractures: a systematic review of the literature. Arch Orthop Trauma Surg. 2008. October;128(10):1169-75. Epub 2008 Jan 4. [DOI] [PubMed] [Google Scholar]
- 5.Canadian Orthopaedic Trauma Society. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures. Results of a multicenter, prospective, randomized clinical trial. J Bone Joint Surg Am. 2006. December;88(12):2613-23. [DOI] [PubMed] [Google Scholar]
- 6.Babis GC, Evangelopoulos DS, Kontovazenitis P, Nikolopoulos K, Soucacos PN. High energy tibial plateau fractures treated with hybrid external fixation. J Orthop Surg Res. 2011. July 14;6:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stannard JP, Wilson TC, Volgas DA, Alonso JE. The less invasive stabilization system in the treatment of complex fractures of the tibial plateau: short-term results. J Orthop Trauma. 2004. September;18(8):552-8. [DOI] [PubMed] [Google Scholar]
- 8.Phisitkul P, McKinley TO, Nepola JV, Marsh JL. Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma. 2007. February;21(2):83-91. [DOI] [PubMed] [Google Scholar]
- 9.Jiang R, Luo CF, Wang MC, Yang TY, Zeng BF. A comparative study of Less Invasive Stabilization System (LISS) fixation and two-incision double plating for the treatment of bicondylar tibial plateau fractures. Knee. 2008. March;15(2):139-43. Epub 2008 Jan 24. [DOI] [PubMed] [Google Scholar]
- 10.Koval KJ, Helfet DL. Tibial plateau fractures: evaluation and treatment. J Am Acad Orthop Surg. 1995. March;3(2):86-94. [DOI] [PubMed] [Google Scholar]
- 11.Gosling T, Schandelmaier P, Muller M, Hankemeier S, Wagner M, Krettek C. Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin Orthop Relat Res. 2005. October;439:207-14. [DOI] [PubMed] [Google Scholar]
- 12.Garnavos C. Retropatellar nailing and condylar bolts for complex fractures of the tibial plateau: technique, pilot study and rationale. Injury. 2014. July;45(7):1099-104. Epub 2014 Jan 14. [DOI] [PubMed] [Google Scholar]
- 13.Garnavos C, Lasanianos NG. The management of complex fractures of the proximal tibia with minimal intra-articular impaction in fragility patients using intramedullary nailing and compression bolts. Injury. 2011. October;42(10):1066-72. Epub 2011 Apr 13. [DOI] [PubMed] [Google Scholar]
- 14.Högel F, Hoffmann S, Panzer S, Wimber J, Bühren V, Augat P. Biomechanical comparison of intramedullar versus extramedullar stabilization of intra-articular tibial plateau fractures. Arch Orthop Trauma Surg. 2013. January;133(1):59-64. Epub 2012 Oct 18. [DOI] [PubMed] [Google Scholar]
- 15.Lee SM, Oh CW, Oh JK, Kim JW, Lee HJ, Chon CS, Lee BJ, Kyung HS. Biomechanical analysis of operative methods in the treatment of extra-articular fracture of the proximal tibia. Clin Orthop Surg. 2014. September;6(3):312-7. Epub 2014 Aug 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lasanianos NG, Garnavos C, Magnisalis E, Kourkoulis S, Babis GC. A comparative biomechanical study for complex tibial plateau fractures: nailing and compression bolts versus modern and traditional plating. Injury. 2013. October;44(10):1333-9. Epub 2013 Apr 16. [DOI] [PubMed] [Google Scholar]
- 17.Lasanianos N, Mouzopoulos G, Garnavos C. The use of freeze-dried cancelous allograft in the management of impacted tibial plateau fractures. Injury. 2008. October;39(10):1106-12. [DOI] [PubMed] [Google Scholar]
- 18.Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010. November;24(11):683-92. [DOI] [PubMed] [Google Scholar]
- 19.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998. August;28(2):88-96. [DOI] [PubMed] [Google Scholar]
- 20.McNamara IR, Smith TO, Shepherd KL, Clark AB, Nielsen DM, Donell S, Hing CB. Surgical fixation methods for tibial plateau fractures. Cochrane Database Syst Rev. 2015. September 15;9:CD009679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kokkalis ZT, Iliopoulos ID, Pantazis C, Panagiotopoulos E. What’s new in the management of complex tibial plateau fractures? Injury. 2016. June;47(6):1162-9. Epub 2016 Mar 3. [DOI] [PubMed] [Google Scholar]
- 22.Waddell JP, Johnston DW, Neidre A. Fractures of the tibial plateau: a review of ninety-five patients and comparison of treatment methods. J Trauma. 1981. May;21(5):376-81. [DOI] [PubMed] [Google Scholar]
- 23.Young MJ, Barrack RL. Complications of internal fixation of tibial plateau fractures. Orthop Rev. 1994. February;23(2):149-54. [PubMed] [Google Scholar]
- 24.Stokel EA, Sadasivan KK. Tibial plateau fractures: standardized evaluation of operative results. Orthopedics. 1991. March;14(3):263-70. [PubMed] [Google Scholar]
- 25.Barei DP, Nork SE, Mills WJ, Henley MB, Benirschke SK. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma. 2004. Nov-Dec;18(10):649-57. [DOI] [PubMed] [Google Scholar]
- 26.Partenheimer A, Gösling T, Müller M, Schirmer C, Kääb M, Matschke S, Ryf C, Renner N, Wiebking U, Krettek C. [Management of bicondylar fractures of the tibial plateau with unilateral fixed-angle plate fixation]. Unfallchirurg. 2007. August;110(8):675-83. German. [DOI] [PubMed] [Google Scholar]
- 27.Schütz M, Kääb MJ, Haas N. Stabilization of proximal tibial fractures with the LIS-System: early clinical experience in Berlin. Injury. 2003. August;34(Suppl 1):A30-5. [DOI] [PubMed] [Google Scholar]
- 28.Cole PA, Zlowodzki M, Kregor PJ. Less Invasive Stabilization System (LISS) for fractures of the proximal tibia: indications, surgical technique and preliminary results of the UMC Clinical Trial. Injury. 2003. August;34(Suppl 1):A16-29. [DOI] [PubMed] [Google Scholar]
- 29.Horwitz DS, Bachus KN, Craig MA, Peters CL. A biomechanical analysis of internal fixation of complex tibial plateau fractures. J Orthop Trauma. 1999. November;13(8):545-9. [DOI] [PubMed] [Google Scholar]
- 30.Higgins TF, Klatt J, Bachus KN. Biomechanical analysis of bicondylar tibial plateau fixation: how does lateral locking plate fixation compare to dual plate fixation? J Orthop Trauma. 2007. May;21(5):301-6. [DOI] [PubMed] [Google Scholar]
- 31.Egol KA, Su E, Tejwani NC, Sims SH, Kummer FJ, Koval KJ. Treatment of complex tibial plateau fractures using the Less Invasive Stabilization System plate: clinical experience and a laboratory comparison with double plating. J Trauma. 2004. August;57(2):340-6. [DOI] [PubMed] [Google Scholar]
- 32.Vince KG, Abdeen A. Wound problems in total knee arthroplasty. Clin Orthop Relat Res. 2006. November;452:88-90. [DOI] [PubMed] [Google Scholar]
- 33.Garbedian S, Sternheim A, Backstein D. Wound healing problems in total knee arthroplasty. Orthopedics. 2011. September 9;34(9):e516-8. [DOI] [PubMed] [Google Scholar]
- 34.Gaudinez RF, Mallik AR, Szporn M. Hybrid external fixation of comminuted tibial plateau fractures. Clin Orthop Relat Res. 1996. July;328:203-10. [DOI] [PubMed] [Google Scholar]
- 35.Mallik AR, Covall DJ, Whitelaw GP. Internal versus external fixation of bicondylar tibial plateau fractures. Orthop Rev. 1992. December;21(12):1433-6. [PubMed] [Google Scholar]
- 36.Ali AM, Burton M, Hashmi M, Saleh M. Treatment of displaced bicondylar tibial plateau fractures (OTA-41C2&3) in patients older than 60 years of age. J Orthop Trauma. 2003. May;17(5):346-52. [DOI] [PubMed] [Google Scholar]
- 37.Hutson JJ, Jr, Zych GA. Infections in periarticular fractures of the lower extremity treated with tensioned wire hybrid fixators. J Orthop Trauma. 1998. Mar-Apr;12(3):214-8. [DOI] [PubMed] [Google Scholar]
- 38.Su EP, Westrich GH, Rana AJ, Kapoor K, Helfet DL. Operative treatment of tibial plateau fractures in patients older than 55 years. Clin Orthop Relat Res. 2004. April;421:240-8. [DOI] [PubMed] [Google Scholar]
- 39.Bhandari M, Audige L, Ellis T, Hanson B; Evidence-Based Orthopaedic Trauma Working Group. Operative treatment of extra-articular proximal tibial fractures. J Orthop Trauma. 2003. September;17(8):591-5. [DOI] [PubMed] [Google Scholar]
- 40.Eastman J, Tseng S, Lo E, Li CS, Yoo B, Lee M. Retropatellar technique for intramedullary nailing of proximal tibia fractures: a cadaveric assessment. J Orthop Trauma. 2010. November;24(11):672-6. [DOI] [PubMed] [Google Scholar]
- 41.Eastman JG, Tseng SS, Lee MA, Yoo BJ. The retropatellar portal as an alternative site for tibial nail insertion: a cadaveric study. J Orthop Trauma. 2010. November;24(11):659-64. [DOI] [PubMed] [Google Scholar]
- 42.Gelbke MK, Coombs D, Powell S, DiPasquale TG. Suprapatellar versus infra-patellar intramedullary nail insertion of the tibia: a cadaveric model for comparison of patellofemoral contact pressures and forces. J Orthop Trauma. 2010. November;24(11):665-71. [DOI] [PubMed] [Google Scholar]
- 43.Gaines RJ, Rockwood J, Garland J, Ellingson C, Demaio M. Comparison of insertional trauma between suprapatellar and infrapatellar portals for tibial nailing. Orthopedics. 2013. September;36(9):e1155-8. [DOI] [PubMed] [Google Scholar]
- 44.Jones M, Parry M, Whitehouse M, Mitchell S. Radiologic outcome and patient-reported function after intramedullary nailing: a comparison of the retropatellar and infrapatellar approach. J Orthop Trauma. 2014. May;28(5):256-62. [DOI] [PubMed] [Google Scholar]
- 45.Paley D. Principles of deformity correction. New York: Springer; 2002. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.