Abstract
Background:
Surgeons have long debated whether advanced or end-stage osteoarthritis of the hip in young patients should be treated with total hip arthroplasty or osteotomy. We reviewed the intermediate-term clinical results of valgus femoral osteotomy combined with Chiari pelvic osteotomy (VCO) for advanced or end-stage osteoarthritis associated with severe acetabular dysplasia of the hip in young patients and analyzed prognostic factors related to conversion to total hip arthroplasty.
Methods:
The study group included 54 hips in 50 patients (5 men and 45 women; average age at the time of surgery, 45.6 years). The minimum and average durations of follow-up were 10 and 17.6 years, respectively. The Japanese Orthopaedic Association hip score (JOA score) was used for clinical evaluation. The probability of survival of the VCO from the time of the operation until the end point of conversion to total hip arthroplasty was calculated with use of the Kaplan-Meier method. We defined prognostic factors of outcome (conversion to total hip arthroplasty) with the Cox proportional hazards model.
Results:
The mean total JOA score increased from 53.0 points preoperatively to 77.1 points at 1 year postoperatively, 81.6 points at 5 years, and 76.8 points at 10 years. The survival rates were 83.3%, 59.7%, and 46.9% at 10, 15, and 20 years, respectively. On univariate and multivariate analyses, patients with a low degree of acetabular roof obliquity had better postoperative results.
Conclusions:
VCO is a surgical approach that preserves joint function in young patients with advanced or end-stage osteoarthritis associated with severe acetabular dysplasia of the hip. The postoperative prognosis of VCO was improved in patients with a low degree of acetabular roof obliquity.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Although total hip arthroplasty has been associated with good results in recent years, it can result in serious postoperative complications after long-term follow-up1,2. Therefore, the benefits of total hip arthroplasty for young patients are uncertain. It has been long debated whether advanced or end-stage hip osteoarthritis in young patients should be treated with total hip arthroplasty or osteotomy. Valgus intertrochanteric osteotomy for the treatment of advanced or end-stage osteoarthritis has recognized benefits3-6. The histological features of repaired tissue following valgus intertrochanteric osteotomy have been investigated previously. In the study by Itoman et al., fibrocartilaginous plugs that were scattered over the exposed bone at the articular surface proliferated to cover the entire bone surface, resulting in improvement of the biomechanics of the hip joint7. Hiranuma et al., in a study evaluating the results of Chiari pelvic osteotomy, reported that the interposed capsule became metaplastic cartilage, which offered adequate weight-bearing support8. In 1979, we began to perform valgus femoral osteotomy for the treatment of advanced or end-stage osteoarthritis of the hip3,6. We also performed valgus osteotomy in combination with Chiari pelvic osteotomy for patients with severe acetabular dysplasia3. In the present study, we reviewed the clinical and radiographic results of combined valgus and Chiari pelvic osteotomies (VCO) that were performed for the treatment of advanced or end-stage osteoarthritis associated with severe acetabular dysplasia of the hip and analyzed prognostic factors that may have affected the postoperative outcome.
Materials and Methods
The study was approved by our institutional review board (study number B15-191), and informed consent was obtained from each participant.
Patients
Between October 1979 and October 2002, we performed valgus femoral osteotomy for the treatment of advanced or end-stage osteoarthritis in 218 hips. In 72 hips (67 patients) that demonstrated severe acetabular dysplasia (as indicated by an acetabular head index of <60%, with inadequate formation of the roof osteophyte after valgus femoral osteotomy), the valgus femoral osteotomy was combined with Chiari osteotomy. Fifteen hips (14 patients) were excluded from the study because they had <10 years of follow-up, and 3 hips (3 patients) were excluded because of a lack of complete preoperative radiographic records for analysis. We attempted to follow up with 17 excluded patients with use of a telephone interview. We were unable to contact 9 patients but did contact 8 patients. Seven of the 8 patients who were contacted successfully for follow-up did not undergo subsequent surgery (including total hip arthroplasty). One patient underwent total hip arthroplasty 34 years after VCO. Therefore, we reviewed 54 hips in 50 patients (5 men and 45 women) with an average age of 45.6 years (range, 21 to 56 years) at the time of surgery. All patients were followed for a minimum of 10 years (average, 17.6 years; range, 10 to 32.8 years), including hips that underwent conversion to total hip arthroplasty; the average duration of follow-up for the 30 hips that did not undergo conversion to total hip arthroplasty was 16.5 years. Twenty patients had unilateral osteoarthritis, 29 patients had bilateral osteoarthritis (with 4 having bilateral surgery), and 1 patient had ankylosis of the contralateral hip joint. We examined preoperative radiographs and classified the stage of disease according to the criteria described by Takatori et al.9. Advanced-stage and end-stage osteoarthritis were determined on the basis of the state of arthritic changes, morphological changes, and loss of joint space. Advanced-stage osteoarthritis was characterized by definite narrowing of the joint space, with a width of <2 mm at the narrowest point. Loss of joint space (with the subchondral bone of the acetabulum being in contact with that of the femoral head) was observed, and the width around the femoral head was >15 mm on anteroposterior radiographs. End-stage osteoarthritis was defined as gross loss of joint space with a width around the femoral head of ≤15 mm on anteroposterior radiographs.
Of the 54 hips that were included in the present study, 33 (61.1%) had advanced osteoarthritis and 21 (38.9%) had end osteoarthritis.
Indications for Valgus Femoral Osteotomy Combined with Chiari Pelvic Osteotomy
The operation was performed in patients <60 years of age who had advanced or end-stage osteoarthritis of the hip associated with acetabular dysplasia. The preoperative range of motion in flexion and extension was preferably ≥60°, with a range of adduction of ≥15°. The femoral heads exhibited a mushroom shape, with hinge adduction observable on dynamic radiographs. With adduction, the lateral joint space was required to open wide in the shape of a wedge. The valgus angle was chosen so that the flattened, previously weight-bearing area of the elliptical head became horizontal. Therefore, the valgus angle was ≥30°. When the acetabular head index was <60%, with inadequate formation of the roof osteophyte after valgus femoral osteotomy, the procedure was combined with Chiari pelvic osteotomy.
Surgical Technique and Postoperative Management
All operations were performed by 1 surgeon. Until 1996, femoral osteotomies were performed with the patient in the supine position on a traction table, with use of 2 incisions and with incomplete osteotomy of the greater trochanter (38 hips; 70.4%) (Fig. 1). From 1997 onward, femoral osteotomies were performed with the patient in the lateral position, without a traction table, through an extended lateral approach that was similar to a Watson-Jones approach (16 hips; 29.6%). For that procedure, the greater trochanter was completely osteotomized and elevated. We then proceeded with an osteotomy of the femur with use of an oscillating bone saw. First, the valgus angle was determined by flattening the previous weight-bearing area of the elliptical head to a horizontal position; the resulting valgus angle was at least 30°. Next, the osteotomy site was immobilized with a 130° hip blade-plate. The iliopsoas tendon was released at its insertion into the lesser trochanter. Then, a Chiari pelvic osteotomy was performed for the treatment of severe acetabular dysplasia (as indicated by an acetabular head index of <60% with the hip in adducted position or after valgus femoral osteotomy). If the acetabular head index remained <60% after Chiari pelvic osteotomy, we inserted an autologous iliac-crest bone graft at the acetabular rim (20 hips; 37%) (Fig. 2). Finally, the greater trochanter was reattached by means of suturing (until 1999) or with use of a pin-sleeve system10 (Ai-Medic) (Figs. 2 and 3).
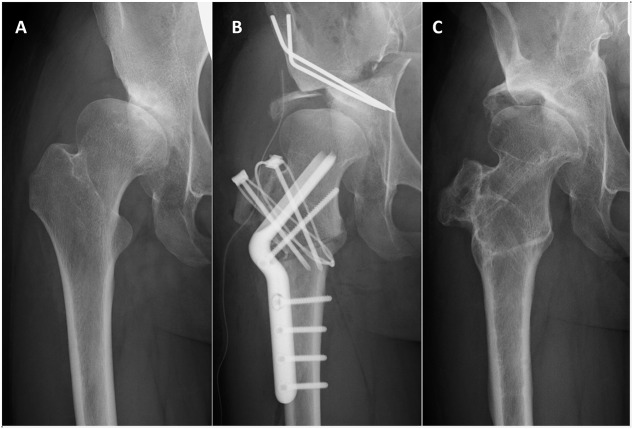
Fig. 1.
Figs. 1-A through 1-D Radiographs of the pelvis and hips of a woman who underwent bilateral VCO. Fig. 1-A Radiograph of the pelvis and hips, made at the age of 40 years, showing advanced-stage osteoarthritis with severe acetabular dysplasia in both hips. Fig. 1-B VCO was performed on the left hip at the age of 40 years. Fig. 1-C VCO was performed on the right hip 1 year later. Fig. 1-D Radiograph showing preserved joint space 24 and 23 years after the operations on the left and right hips, respectively.
Fig. 2.
Figs. 2-A, 2-B, and 2-C Radiographs of the right hip of a woman who underwent VCO with autogenous bone-grafting at the age of 30 years. Fig. 2-A Radiograph of the right hip, showing advanced-stage osteoarthritis with severe acetabular dysplasia. Fig. 2-B Radiograph made after VCO, followed by insertion of an autologous iliac-crest bone graft at the acetabular rim. Fig. 2-C Radiograph, made 2 years postoperatively, showing good joint remodeling.
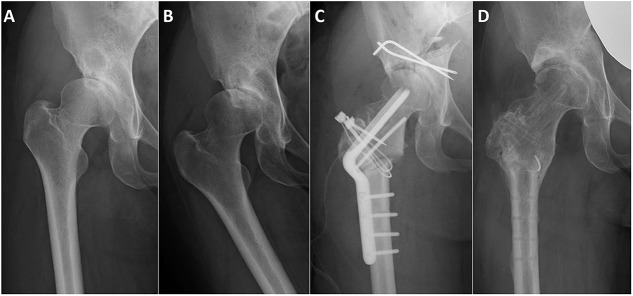
Fig. 3.
Figs. 3-A through 3-D Radiographs of the right hip of a woman who underwent VCO for the treatment of an unstable femoral head at the age of 38 years. Fig. 3-A Radiograph showing advanced-stage osteoarthritis with severe acetabular dysplasia. Fig. 3-B Dynamic radiograph showing the femoral head with hinge adduction, which causes the lateral joint space to open wide and the weight-bearing area of the elliptical head to become horizontal. Fig. 3-C Radiograph made after VCO, showing a high pelvic osteotomy angle. Fig. 3-D Radiograph, made 2 years postoperatively, showing good joint remodeling.
With regard to complications, 2 hips (3.7%) had a superficial infection that resolved with treatment. Two hips (3.7%) in which the joint space was not expanded after the VCO procedure underwent releases of the iliopsoas and adductor muscles at 1 year and 6 years postoperatively. One hip (1.9%) was treated with autologous bone-grafting because of a pseudarthrosis at the site of the femoral osteotomy. One hip (1.9%) was treated with an operative transposition of the greater trochanter and leg-extension operation. One hip (1.9%) had temporary peroneal nerve paralysis after the operation that resolved over time. The frequency of deep vein thrombosis, pulmonary embolism, and lateral femoral cutaneous nerve palsy was assessed by reviewing the medical records; however, because of the incomplete nature of the old medical records, an accurate frequency could not be determined.
Two days after surgery, patients began passive and active range-of-motion exercises and began using a wheelchair. Three weeks after surgery, patients began one-third partial weight-bearing. Five to 6 weeks after surgery, patients began two-thirds partial weight-bearing and were discharged from the hospital on 1 crutch. Full weight-bearing began 3 to 4 months after surgery, when osseous union was expected. The plate and screws were removed 1 to 3 years postoperatively.
Clinical Evaluation
Clinical evaluations were performed according to the Japanese Orthopaedic Association (JOA) hip-scoring system before surgery; at 1, 5, and 10 years postoperatively; and at the time of the latest follow-up. JOA scores range from 0 to 100 points, with points assigned for pain (0 to 40 points), range of motion (0 to 20 points), walking ability (0 to 20 points), and activities of daily living (0 to 20 points). The JOA pain and range-of-motion scores were determined separately for the left and right hips. For patients who were managed with total hip arthroplasty, the hip score was evaluated just prior to the procedure.
Radiographic Evaluations
Radiographic evaluations were used to measure the acetabular head index (expressed as a percentage), the Sharp angle (in degrees) during the preoperative and immediate postoperative periods, and acetabular roof obliquity (in degrees) at 1 year postoperatively. With regard to surgical technique, radiographs were used to measure the height of pelvic osteotomy (in millimeters), the osteotomy angle (in degrees), and the pelvic displacement ratio (the ratio of the displacement distance of the pelvic osteotomy on the anteroposterior radiograph, expressed as a percentage) (Fig. 4).
Fig. 4.
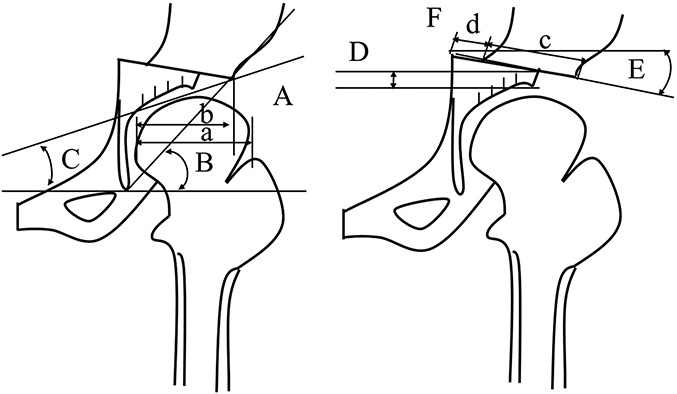
Left image Diagram illustrating the methods used to evaluate preoperative and postoperative radiographic parameters, including the acetabular head index (b/a × 100%) (A), the Sharp angle (in degrees) (B), and the acetabular roof obliquity (in degrees) (C). Right image Diagram illustrating the methods used to evaluate intraoperative radiographic parameters, including the height of pelvic osteotomy (in millimeters) (D), the osteotomy angle (in degrees) (E), and the pelvic displacement ratio (the ratio of displacement distance of the pelvic osteotomy on the anteroposterior view) (d/c × 100%) (F).
Survival Rate
Following surgery, if the pain level increased or if the range of motion of the hip joint decreased to the extent that daily life was hindered, we performed total hip arthroplasty. We calculated the probability of survival of the hip from the time of the VCO operation until the end point of conversion to total hip arthroplasty with use of the Kaplan-Meier method. The 95% confidence intervals (CIs) were also calculated. Furthermore, we assessed the conversion rate of VCO to total hip arthroplasty and the time interval between VCO and conversion to total hip arthroplasty.
Prognostic Factors
To examine prognostic factors, all 54 hips with a minimum duration of follow-up of 10 years after VCO were evaluated. We investigated several possible prognostic factors of conversion to total hip arthroplasty, including age, body mass index (BMI), affected side (unilateral versus bilateral), range of motion (flexion-extension) on the affected side, presence of a bone cyst (on femoral head or acetabular side), preoperative femoral head morphology (transverse:vertical diameter ratio), acetabular head index, Sharp angle, pelvic osteotomy height, Chiari osteotomy angle, pelvic displacement ratio, the need for bone-grafting immediately after the VCO operation, and acetabular roof obliquity at 1 year postoperatively.
Statistical Analysis
The preoperative JOA scores were compared with postoperative scores (at 1, 5, and 10 years and at the latest follow-up) with use of the Student t test. Surgical technique parameters and preoperative and postoperative radiographic measurements were compared with use of the Wilcoxon signed-rank test. The level of significance was set at p < 0.05. We assessed prognostic factors for conversion to total hip arthroplasty with use of the univariate Cox proportional hazards model. Moreover, the multivariate Cox hazard statistical analysis was performed to analyze the significant prognostic factors and the factors likely to be involved in conversion to total hip arthroplasty. Differences were defined as significant when the p value was <0.05. Statistical analyses were performed with use of JMP Pro 12 software (SAS Institute).
Results
The average total JOA score was 53.0 points preoperatively (n = 54 hips), 77.1 points at 1 year (n = 54 hips), 81.6 points at 5 years (n = 48 hips, excluding the 6 that underwent total hip arthroplasty), 76.8 points at 10 years (n = 45 hips, excluding the 9 that underwent total hip arthroplasty), and 59.7 points at the latest follow-up (n = 54 hips) (Fig. 5). Over the first 10 years, significant improvement in the JOA score was observed in comparison with the preoperative score (p < 0.0001). Of the clinical evaluation criteria, the pain score improved most markedly. The average total JOA score at the latest follow-up observation (average, 17.6 years) was significantly better than the preoperative score (59.7 compared with 53.0; p < 0.05). The average total JOA score for the 30 hips that did not undergo conversion to total hip arthroplasty increased from 54.9 points preoperatively to 72.5 points at the time of the latest follow-up evaluation (p < 0.0001), and this score was significantly higher than the average score of 43.9 points for the 24 hips that underwent total hip arthroplasty (p < 0.0001).
Fig. 5.
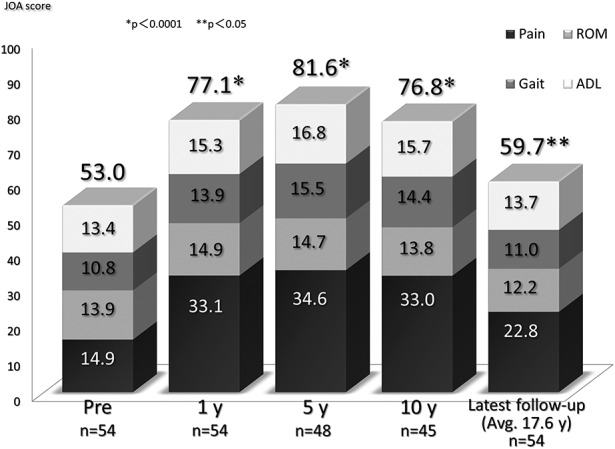
Bar graph showing mean JOA hip scores before and after VCO. The p values pertain to the differences between the postoperative scores and the preoperative score as determined with the Student t test. ADL = activities of daily living, and ROM = range of motion.
The surgical technique was evaluated postoperatively on the basis of radiographic measurements. The mean pelvic osteotomy height (and standard deviation) was 5.8 ± 3.0 mm, the mean osteotomy angle in the superior direction was 1.8° ± 8.3°, and the mean pelvic displacement ratio was 40.3% ± 11.0% (Table I). Postoperatively, the acetabular head index, Sharp angle, and acetabular roof obliquity all improved significantly (Table II).
TABLE I.
Radiographic Evaluation of Surgical Technique Parameters

TABLE II.
Comparison of Preoperative and Postoperative Radiographic Measurements*
Twenty-four hips (44.4%) were converted to total hip arthroplasty. The average period from the initial osteotomy operation until conversion to total hip arthroplasty was 10.8 years (range, 1.7 to 21.3 years). Survival was analyzed with the time of conversion to total hip arthroplasty as the end point; the cumulative rates of survival were 83.3% at 10 years, 59.7% at 15 years, 46.9% at 20 years, and 39.1% at 25 years (Fig. 6).
Fig. 6.
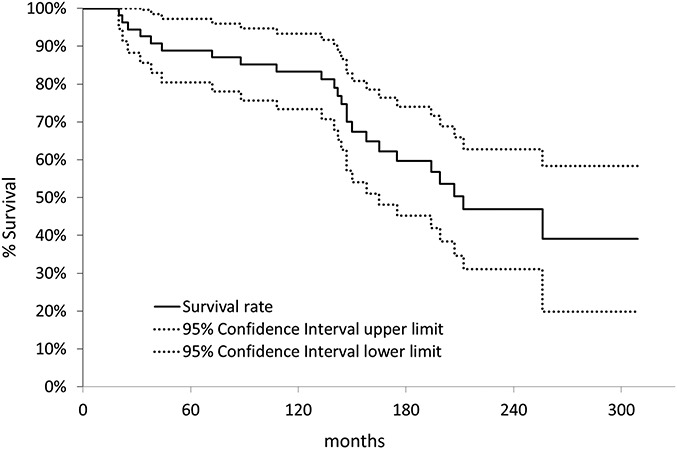
Kaplan-Meier survivorship curves indicating the probability of survival from the time of the operation until the end point of conversion to total hip arthroplasty.
We analyzed prognostic factors for conversion to total hip arthroplasty by means of univariate Cox proportional hazards analysis (Table III). A high degree of acetabular roof obliquity at 1 year postoperatively was found to be a significant prognostic factor for conversion to total hip arthroplasty (p = 0.0084). When we selected the most significant prognostic factor (a high degree of acetabular roof obliquity at 1 year postoperatively) and the factors most likely to be involved in total hip arthroplasty (age and postoperative acetabular head index) to perform a multivariate Cox hazard analysis with forced input, a high-degree acetabular roof obliquity at 1 year postoperatively was found to be a significant prognostic factor (p = 0.0273), whereas age and postoperative acetabular head index were not (Table IV).
TABLE III.
Univariate Cox Proportional Hazards Analysis of Prognostic Factors for Conversion to Total Hip Arthroplasty
TABLE IV.
Multivariate Cox Hazard Analysis
Discussion
Secondary osteoarthritis of the hip caused by acetabular dysplasia is common among Japanese women, and acetabular dysplasia occurs in association with approximately 80% of all cases of hip osteoarthritis11.
A characteristic secondary feature of osteoarthritis caused by acetabular dysplasia is changed femoral head shape, observed as a large capital drop that forms on the posteromedial side, presumably as the result of a biological response to the repair process. Conveniently, the formation of a flat femoral head and a double floor is adequate for valgus femoral osteotomy. The goal of valgus femoral osteotomy is not to achieve joint congruity but rather to induce the body’s inherent self-repair ability by changing the load environment of the hip joint as a result of the hinge adduction position3,6,7.
Several authors have reported satisfactory results after valgus osteotomy for the treatment of advanced or end-stage osteoarthritis associated with acetabular dysplasia of the hip in young patients3-6,12-20. For patients with severe acetabular dysplasia in whom acetabular coverage remained insufficient after valgus osteotomy, some of those authors recommended additional acetabuloplasty operations such as a shelf procedure12,13,21 or the Chiari pelvic osteotomy3 in order to allow further lateralization of the affected femoral head. Our experience suggested that Chiari pelvic osteotomy was more advantageous because it allowed a larger weight-bearing surface to be created with the osteotomized proximal fragment and because it resulted in greater medialization of the hip center22-30 than other procedures.
Toyama et al., in a study of 67 hips that underwent valgus-extension femoral osteotomy with or without an additional shelf procedure for the treatment of advanced osteoarthritis, reported that hips that were treated with an additional shelf procedure (n = 31) experienced longer-lasting pain relief compared with those that were treated with valgus osteotomy alone (n = 36)13. We began to perform valgus intertrochanteric femoral osteotomy as well as valgus osteotomy combined with Chiari pelvic osteotomy to treat severe acetabular dysplasia in 19793,6,31. Takasaki et al. treated 256 hips with valgus osteotomy, including 88 hips in which valgus osteotomy was combined with Chiari pelvic osteotomy3. In that report, the 10-year survival rates for the hips that were treated with and without Chiari pelvic osteotomy were 93% and 87%, respectively; this difference was not significant. This result suggested that, for patients with more severe dysplasia (acetabular head index, <60%), it was possible to achieve similar results with VCO as compared with valgus osteotomy alone.
There have been several studies on the use of osteotomy for the treatment of advanced or end-stage osteoarthritis of the hip in young patients. Ito et al., in a study of 32 Tönnis grade-3 hips that underwent Chiari pelvic osteotomy for the treatment of osteoarthritis, reported a cumulative 10-year survival rate of 72% with a Harris hip score of <70 points as the end point27. They concluded that Chiari pelvic osteotomy may be an option for young patients with advanced osteoarthritis who prefer a joint-preserving procedure to total hip arthroplasty and who accept a clinical outcome that is predicted to be less optimal than that of total hip arthroplasty. Okano et al., in a study of 42 patients (44 hips) who underwent rotational acetabular osteotomy for the treatment of advanced osteoarthritis secondary to developmental dysplasia, reported a cumulative 10-year survival rate of 75.0% with radiographic signs of progression of osteoarthritis as the end point and observed that osteoarthritis with a round femoral head was an indication for rotational acetabular osteotomy, even for patients with advanced-stage disease (Table V)32. However, patients who have a deformed femoral head in association with advanced osteoarthritis may experience progression to end-stage disease with this procedure. We then considered that VCO may be suitable for preserving joint function in patients with advanced or end-stage osteoarthritis associated with severe dysplasia because of the flat shape of the femoral head.
TABLE V.
Survival Rate of Osteotomy for Young Patients with Advanced or End-Stage Arthritis of the Hip
Toyama et al. reported acceptable results following valgus osteotomy combined with an additional shelf operation for the treatment of hips with a lower preoperative acetabular roof obliquity value, demonstrating that such a method is better for preventing the superolateral displacement of the femoral head (subluxation)13. Our results showed that a high degree of acetabular roof obliquity at 1 year postoperatively was a significant prognostic factor for conversion to total hip arthroplasty. The insertion of an autologous iliac-crest bone graft at the acetabular rim is thought to improve the acetabular roof obliquity by increasing the pelvic osteotomy angle superior direction, but there was no significant difference in acetabular roof obliquity when patients with autologous iliac crest bone graft at the acetabular rim were compared with patients without bone graft.
Twenty-four hips (44.4%) underwent conversion to total hip arthroplasty at an average of 10.8 years following the initial osteotomy. Acceptable intermediate-term results following total hip arthroplasty performed after intertrochanteric femoral osteotomy33 and after Chiari pelvic osteotomy34 have been reported previously. However, in some cases, total hip arthroplasty after osteotomy is more difficult than normal total hip arthroplasty because the altered bone morphology makes it difficult to insert the stem into the femur. In addition, there are cases in which the range of motion does not improve after total hip arthroplasty because it was previously decreased following the osteotomy. In recent years, there have been reports of periprosthetic fractures at the time of stem insertion after femoral osteotomy34. These results indicate that total hip arthroplasty is a technically demanding operation in patients who were previously managed with femoral osteotomy. To prevent periprosthetic fractures, clinicians should be attentive to the needs of patients during planning and implant selection. Moreover, it is better to perform total hip arthroplasty before the range of motion decreases.
VCO is a surgical approach that preserves joint function for advanced or end-stage osteoarthritis associated with severe acetabular dysplasia of the hip in young patients. The postoperative prognosis of VCO was improved in patients with a low degree of acetabular roof obliquity.
Disclosure of Potential Conflicts of Interest
Acknowledgments
Note: The authors thank emeritus professor Moritoshi Itoman for offering continuing support and constant encouragement.
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, School of Medicine and School of Allied Health Sciences, Kitasato University, Kanagawa, Japan
Disclosure: There was no outside funding in support of our study. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A8).
References
- 1.McAuley JP, Szuszczewicz ES, Young A, Sr Engh CA. Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. 2004. January;418:119-25. [DOI] [PubMed] [Google Scholar]
- 2.Duffy GP, Berry DJ, Rowland C, Cabanela ME. Primary uncemented total hip arthroplasty in patients <40 years old: 10- to 14-year results using first-generation proximally porous-coated implants. J Arthroplasty. 2001. December;16(8)(Suppl 1):140-4. [DOI] [PubMed] [Google Scholar]
- 3.Takasaki S, Uchiyama K, Takahira N, Itoman M. Results and prognostic factors of valgus osteotomy in middle-aged patients with advanced or terminal osteoarthritis of the hip. J Orthop Sci. 2010. January;15(1):20-9. Epub 2010 Feb 12. [DOI] [PubMed] [Google Scholar]
- 4.Kawate K, Tanaka Y, Ohmura T, Hiyoshi N, Yajima H, Tomita Y, Takakura Y. Twenty-five years followup of patients who had valgus osteotomy for arthritic hips. Clin Orthop Relat Res. 2004. September;426:151-8. [DOI] [PubMed] [Google Scholar]
- 5.Jingushi S, Sugioka Y, Noguchi Y, Miura H, Iwamoto Y. Transtrochanteric valgus osteotomy for the treatment of osteoarthritis of the hip secondary to acetabular dysplasia. J Bone Joint Surg Br. 2002. May;84(4):535-9. [DOI] [PubMed] [Google Scholar]
- 6.Itoman M, Yonemoto K, Sekiguchi M, Yamamoto M. Valgus-flexion osteotomy for middle-aged patients with advanced osteoarthritis of the hip: a clinical and radiological evaluation. Nihon Seikeigeka Gakkai Zasshi. 1992. April;66(4):195-204. [PubMed] [Google Scholar]
- 7.Itoman M, Yamamoto M, Yonemoto K, Sekiguchi M, Kai H. Histological examination of surface repair tissue after successful osteotomy for osteoarthritis of the hip joint. Int Orthop. 1992;16(2):118-21. [DOI] [PubMed] [Google Scholar]
- 8.Hiranuma S, Higuchi F, Inoue A, Miyazaki M. Changes in the interposed capsule after Chiari osteotomy. An experimental study on rabbits with acetabular dysplasia. J Bone Joint Surg Br. 1992. May;74(3):463-7. [DOI] [PubMed] [Google Scholar]
- 9.Takatori Y, Ito K, Sofue M, Hirota Y, Itoman M, Matsumoto T, Hamada Y, Shindo H, Yamada H, Yasunaga Y, Ito H, Mori S, Owan I, Fujii G, Ohashi H, Mawatari T, Iga T, Takahira N, Sugimori T, Sugiyama H, Okano K, Karita T, Ando K, Hamaki T, Hirayama T, Iwata K, Matsuura M, Jingushi S; Investigation Group into Coxarthrosis and Acetabular Dysplasia in Japan. Analysis of interobserver reliability for radiographic staging of coxarthrosis and indexes of acetabular dysplasia: a preliminary study. J Orthop Sci. 2010. January;15(1):14-9. Epub 2010 Feb 12. [DOI] [PubMed] [Google Scholar]
- 10.Takahira N, Itoman M, Uchiyama K, Takasaki S, Fukushima K. Reattachment of the greater trochanter in total hip arthroplasty: the pin-sleeve system compared with the Dall-Miles cable grip system. Int Orthop. 2010. August;34(6):793-7. Epub 2010 Mar 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jingushi S, Ohfuji S, Sofue M, Hirota Y, Itoman M, Matsumoto T, Hamada Y, Shindo H, Takatori Y, Yamada H, Yasunaga Y, Ito H, Mori S, Owan I, Fujii G, Ohashi H, Iwamoto Y, Miyanishi K, Iga T, Takahira N, Sugimori T, Sugiyama H, Okano K, Karita T, Ando K, Hamaki T, Hirayama T, Iwata K, Nakasone S, Matsuura M, Mawatari T. Multiinstitutional epidemiological study regarding osteoarthritis of the hip in Japan. J Orthop Sci. 2010. September;15(5):626-31. Epub 2010 Oct 16. [DOI] [PubMed] [Google Scholar]
- 12.Mori R, Yasunaga Y, Yamasaki T, Hamanishi M, Shoji T, Ochi M. Ten year results of transtrochanteric valgus osteotomy with or without the shelf procedure. Int Orthop. 2013. April;37(4):599-604. Epub 2013 Feb 6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Toyama H, Endo N, Sofue M, Dohmae Y, Takahashi HE. Relief from pain after Bombelli’s valgus-extension osteotomy, and effectiveness of the combined shelf operation. J Orthop Sci. 2000;5(2):114-23. [DOI] [PubMed] [Google Scholar]
- 14.Haverkamp D, Eijer H, Patt TW, Marti RK. Multi directional intertrochanteric osteotomy for primary and secondary osteoarthritis—results after 15 to 29 years. Int Orthop. 2006. February;30(1):15-20. Epub 2005 Dec 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kubo T, Fujioka M, Yamazoe S, Ueshima K, Inoue S, Horii M, Ando K, Imai R, Hirasawa Y. Bombelli’s valgus-extension osteotomy for osteoarthritis due to acetabular dysplasia: results at 10 to 14 years. J Orthop Sci. 2000;5(5):457-62. [DOI] [PubMed] [Google Scholar]
- 16.D’Souza SR, Sadiq S, New AM, Northmore-Ball MD. Proximal femoral osteotomy as the primary operation for young adults who have osteoarthrosis of the hip. J Bone Joint Surg Am. 1998. October;80(10):1428-38. [DOI] [PubMed] [Google Scholar]
- 17.Gotoh E, Inao S, Okamoto T, Ando M. Valgus-extension osteotomy for advanced osteoarthritis in dysplastic hips. Results at 12 to 18 years. J Bone Joint Surg Br. 1997. July;79(4):609-15. [DOI] [PubMed] [Google Scholar]
- 18.Iwase T, Hasegawa Y, Kawamoto K, Iwasada S, Yamada K, Iwata H. Twenty years’ followup of intertrochanteric osteotomy for treatment of the dysplastic hip. Clin Orthop Relat Res. 1996. October;331:245-55. [DOI] [PubMed] [Google Scholar]
- 19.Maistrelli GL, Gerundini M, Fusco U, Bombelli R, Bombelli M, Avai A. Valgus-extension osteotomy for osteoarthritis of the hip. Indications and long-term results. J Bone Joint Surg Br. 1990. July;72(4):653-7. [DOI] [PubMed] [Google Scholar]
- 20.Langlais F, Roure JL, Maquet P. Valgus osteotomy in severe osteoarthritis of the hip. J Bone Joint Surg Br. 1979. November;61-B(4):424-31. [DOI] [PubMed] [Google Scholar]
- 21.Haverkamp D, Marti RK. Intertrochanteric osteotomy combined with acetabular shelfplasty in young patients with severe deformity of the femoral head and secondary osteoarthritis. A long-term follow-up study. J Bone Joint Surg Br. 2005. January;87(1):25-31. [PubMed] [Google Scholar]
- 22.Nakata K, Masuhara K, Sugano N, Sakai T, Haraguchi K, Ohzono K. Dome (modified Chiari) pelvic osteotomy: 10- to 18-year followup study. Clin Orthop Relat Res. 2001. August;389:102-12. [PubMed] [Google Scholar]
- 23.Sakai T, Nishii T, Takao M, Ohzono K, Sugano N. High survival of dome pelvic osteotomy in patients with early osteoarthritis from hip dysplasia. Clin Orthop Relat Res. 2012. September;470(9):2573-82. Epub 2012 Feb 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li L, Jia J, Zhao Q, Zhang L, Ji S, Wang E. Evaluation of femoral head coverage following Chiari pelvic osteotomy in adolescents by three-dimensional computed tomography and conventional radiography. Arch Orthop Trauma Surg. 2012. May;132(5):599-605. [DOI] [PubMed] [Google Scholar]
- 25.Ito H, Tanino H, Yamanaka Y, Nakamura T, Minami A, Matsuno T. The Chiari pelvic osteotomy for patients with dysplastic hips and poor joint congruency: long-term follow-up. J Bone Joint Surg Br. 2011. June;93(6):726-31. [DOI] [PubMed] [Google Scholar]
- 26.Karami M, Gouran Savadkoohi D, Ghadirpoor A, Rahimpour S, Azghani M, Farahmand F. A computer model for evaluating the osteotomy parameters of Chiari pelvic osteotomy. Int Orthop. 2010. March;34(3):329-33. Epub 2009 Apr 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ito H, Matsuno T, Minami A. Chiari pelvic osteotomy for advanced osteoarthritis in patients with hip dysplasia. J Bone Joint Surg Am. 2005. September;87(Pt 2)(Suppl 1):213-25. [DOI] [PubMed] [Google Scholar]
- 28.Macnicol MF, Lo HK, Yong KF. Pelvic remodelling after the Chiari osteotomy. A long-term review. J Bone Joint Surg Br. 2004. July;86(5):648-54. [DOI] [PubMed] [Google Scholar]
- 29.Rozkydal Z, Kovanda M. Chiari pelvic osteotomy in the management of developmental hip dysplasia: a long term follow-up. Bratisl Lek Listy. 2003;104(1):7-13. [PubMed] [Google Scholar]
- 30.Ito H, Matsuno T, Minami A. Comparison of the surgical approaches for a Chiari pelvic osteotomy. J Bone Joint Surg Br. 2003. March;85(2):204-8. [DOI] [PubMed] [Google Scholar]
- 31.Chiari K. Medial displacement osteotomy of the pelvis. Clin Orthop Relat Res. 1974. Jan-Feb;98:55-71. [DOI] [PubMed] [Google Scholar]
- 32.Okano K, Enomoto H, Osaki M, Shindo H. Rotational acetabular osteotomy for advanced osteoarthritis secondary to developmental dysplasia of the hip. J Bone Joint Surg Br. 2008. January;90(1):23-6. [DOI] [PubMed] [Google Scholar]
- 33.Ohishi M, Nakashima Y, Yamamoto T, Motomura G, Fukushi J, Hamai S, Kohno Y, Iwamoto Y. Cementless total hip arthroplasty for patients previously treated with femoral osteotomy for hip dysplasia: the incidence of periprosthetic fracture. Int Orthop. 2016. August;40(8):1601-6. Epub 2015 Sep 19. [DOI] [PubMed] [Google Scholar]
- 34.Hashemi-Nejad A, Haddad FS, Tong KM, Muirhead-Allwood SK, Catterall A. Does Chiari osteotomy compromise subsequent total hip arthroplasty? J Arthroplasty. 2002. September;17(6):731-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.