Abstract
Background:
Anatomical variation may represent a challenge in achieving a close fit between a prosthesis and a patient’s osseous geometry in total knee arthroplasty (TKA). The purposes of this study were to determine whether the shape of the distal part of the femur differs among ethnicities, whether these differences affect the fit of the femoral component of a standard prosthesis, and whether the additional availability of a femoral component with a reduced mediolateral dimension for the same anteroposterior dimension improves femoral component fit across ethnicities.
Methods:
Femoral dimensions were measured intraoperatively during 967 TKAs performed using the same type of prosthesis in patients of 5 different ethnicities. Aspect ratios were calculated to determine whether the shapes of the femora differed among ethnicities. The component fit (“perfect,” overhang, or underhang) when only standard prostheses were available was compared with the fit when both standard and narrow prostheses were available in all ethnic groups. This enabled us to determine whether the femoral component fit was improved by the additional availability of the narrow version.
Results:
Wide variations in shape were found among ethnicities as were variations among individuals of the same ethnicity. Differences in shape among ethnicities influenced the rate of overhang. However, overhang was more frequent at the trochlear than at the condylar level across all ethnicities. The availability of both the standard and the narrow femoral components improved the rate of a perfect fit in women in 3 of the 5 ethnic groups and reduced the overhang rate in women in all 5 of the ethnic groups. In contrast, only modest improvements in femoral component fit, which were not statistically significant, were seen in men.
Conclusions:
The shape of the distal part of the femur varies not only among ethnicities but also within ethnic groups, leading to a high prevalence of overhang when only standard prostheses are available. The additional availability of a femoral component with a reduced mediolateral dimension for the same anteroposterior size can reduce overhang and improve component fit across ethnicities.
A close match between the dimensions of the prosthesis and the patient’s osseous geometry is important for an optimal outcome of a total knee arthroplasty (TKA)1-3. Several studies have demonstrated poorer functional outcomes related to overcoverage by the femoral component (overhang)1,3, whereas undercoverage by the femoral component (underhang) leads to increased blood loss through exposed cancellous bone4-6 and in theory could increase the risk of osteolysis secondary to elaboration of wear particles7.
Because TKA is widely performed across diverse ethnic groups, anatomical variation presents a challenge in device design8,9. One of the strategies to improve femoral component fit is to make available a narrow femoral component with the same anteroposterior diameter as the standard option but a reduced mediolateral diameter. However, there is limited information in the literature regarding whether the additional availability of a narrower femoral component improves prosthetic fit among various ethnic groups10.
We sought to address this issue by using direct intraoperative measurements in a prospective cohort of patients of various ethnicities who were undergoing TKA. Our purposes were to determine whether the shape of the distal part of the femur differs between Asians and Caucasians and among different Asian ethnicities; (2) if so, whether these differences affect femoral component fit, resulting in different prevalences of overhang or underhang between Asians and Caucasians and among different Asian ethnicities; (3) whether femoral component overhang is more prevalent at the condylar, junctional, or trochlear level; and (4) whether the additional availability of a femoral component with the same anteroposterior dimension as the standard component but a reduced mediolateral dimension improves femoral component fit across ethnicities.
Materials and Methods
Study Design and Setting
A multicenter, prospective, observational study was conducted at 11 arthroplasty centers in 5 countries (Australia, China, India, Japan, and Korea) from May 2011 to July 2014. Intraoperative knee measurements were collected during 967 TKAs using the same prosthesis (Genesis II; Smith & Nephew) in 119 Caucasians residing in Australia and 212 patients in each of 4 Asian ethnic groups, including Chinese, Indian, Japanese, and Korean. Research ethics approval was obtained from the regional ethics committee of each center, and all patients gave signed informed consent.
Participants/Study Subjects
All patients who presented with non-inflammatory degenerative arthritis of the medial compartment determined to be best treated with TKA were screened for eligibility for the present study, and their data were entered into a screening log. Patients who had had major, non-arthroscopic surgery on the involved knee, lateral knee compartment disease (e.g., a valgus knee), or serious medical infirmity (e.g., Parkinson disease, Alzheimer disease, or a cerebrovascular accident with a neurological deficit) were excluded. Preoperative assessments included recording of demographic information and medical history, clinical evaluation with the Knee Society Score (KSS), and use of the Knee injury and Osteoarthritis Outcome Score (KOOS) patient-reported questionnaire. Patients also underwent preoperative radiographic evaluation with anteroposterior, lateral, and Merchant (or skyline) patellar views. Patient demographics are summarized in Table I.
TABLE I.
Demographic Information for the Study Subjects
Surgical Procedure and Data Analysis
All patients underwent TKA with the Genesis II prosthesis. During surgery, anthropometric data were measured for each knee according to a predefined protocol and entered into case report forms. After adequate exposure, all osteophytes were removed from the anterior, medial, and lateral aspects of the femur to ensure accurate measurement of true femoral dimensions. Five dimensions were measured for each knee. The first 2—the anteroposterior heights of the medial and lateral femoral condyles—were measured before bone resection (Fig. 1). The femoral component size was then selected at the discretion of the operating surgeon using predefined guidelines that recommended choosing a component with an anteroposterior dimension closest to the measured anteroposterior dimension, with consideration of gap information if the surgeon measured gaps. The remaining 3 knee measurements, made after bone resection, were the mediolateral width at the level of the condyles (anterior border of the posterior chamfer cut), the mediolateral width of the junction (posterior border of the anterior chamfer cut), and the mediolateral width of the trochlea (anterior border of the anterior chamfer cut) (Fig. 1). The amount of distal femoral resection, which was decided by the surgeon by taking into account component thickness and the degree of flexion contracture, ranged from 7.0 to 13.5 mm. All measurements were made to the nearest 1 mm using special calipers for neurosurgery (item number AA845R; B. Braun-Aesculap).
Fig. 1.
Clinical intraoperative photographs showing the dimensions measured in this study. Before bone resection, the anteroposterior heights of the medial and lateral femoral condyles were measured (Figs. 1-A and 1-B). After bone resection, the mediolateral widths at the level of the condyles (anterior border of the posterior chamfer cut) (Fig. 1-C), junction (posterior border of the anterior chamfer cut) (Fig. 1-D), and trochlea (anterior border of the anterior chamfer cut) (Fig. 1-E) were measured.
Four ratios were calculated from the 5 measurements to determine the shape of the distal part of the femur: the condylar, junctional, and trochlear aspect ratios (calculated by dividing the measured mediolateral widths at these levels by the anteroposterior height of the lateral condyle) and the anteroposterior height of the lateral condyle divided by the anteroposterior height of the medial condyle. These 4 ratios were compared among the different ethnic groups to determine whether the shape of the distal part of the femur differed among these groups.
The mediolateral anthropometric measurements performed intraoperatively were used to calculate the “goodness of fit” of the standard Genesis II femoral component. This calculation was performed postoperatively by subtracting the known mediolateral width of the Genesis II component from the mediolateral width at each of the 3 levels of the femur after resection. A cutoff value of 3 mm was used to define the goodness of fit1, with a positive value of ≥3 mm denoting underhang (the femoral component is narrower than the distal part of the femur) and a negative value of ≥3 mm denoting overhang (the component is wider than the distal part of the femur). Values between −3 mm and +3 mm denoted the “perfect fit” scenario. A knee was labeled as having overhang if overhang was seen at any of the 3 regions (condylar, junction, or trochlear), as having a perfect fit if it had perfect fit at all 3 levels or perfect fit at 2 levels and underhang at 1, and as having underhang if there was underhang at all 3 levels or underhang at 2 levels and a perfect fit at 1. We also calculated the “goodness of fit” for scenarios in which, in addition to the standard femoral component, a narrow version (mediolateral dimension decreased by 3 to 4 mm) was available for selection and the narrow version was chosen only when there was overhang at any of the 3 levels. To do this, we virtually treated, using the narrow version, only those knees that had overhang with the standard version. The knees that showed “perfect fit” with the narrow version were then added to the pool of knees with “perfect fit” of the standard prosthesis to determine the perfect-fit rate when both standard and narrow versions were available.
Statistical Analysis
In the analysis of whether the shape of the distal part of the femur differed among ethnicities, female aspect ratios were compared among the ethnicities to negate the confounding effect of sex and size on aspect ratios. The size distribution of the femoral components in the men differed between the Australian and Asian groups, with the vast majority of Australian males being treated with size 7 or 8 while very few Asian males were treated with size 7 and none were treated with size 8 (Table II). Additionally, the numbers of male patients in the Japanese and Korean groups were small. One-way analysis of variance (ANOVA) and Kruskal-Wallis tests were used to compare continuous variables among ethnicities. The Tukey test in conjunction with post hoc analysis was used for comparing pairs of means within ethnic groups. The prevalences of component fit were compared among ethnicities using the Fisher exact test.
TABLE II.
Distribution of Sizes of Final Femoral Components for Females and Males in Ethnic Groups
Results
The sizes and shapes of the knee differed not only between Caucasians and Asians but also among the different Asian ethnicities (Table III). The Caucasian group had larger anteroposterior dimensions of the lateral condyle and larger mediolateral dimensions at the condyles and junction than the Asian group. In contrast, the mediolateral dimensions at the trochlear level were larger in the Asian group, in particular in the Chinese and Japanese patients, compared with the Caucasian group. In terms of shape, Asian patients had wider femora (a higher aspect ratio) at all 3 levels, but more so at the trochlea, compared with the Caucasian patients. There was wide interindividual variability in the mediolateral widths within ethnicities.
TABLE III.
Comparisons of Various Anthropometric Dimensions for Female Patients in 5 Ethnic Groups
Prevalences of overhang or underhang differed between Asians and Caucasians and among different Asian ethnicities. Differences in shape among ethnicities somewhat accounted for these differences (Figs. 2, 3, and 4). Caucasian patients’ knees displayed the maximum percentage of overhang while the knees in the Japanese group displayed the minimum, in line with their corresponding aspect ratios. Overhang was more frequent at the trochlea and the junction than at the condylar level (Figs. 2, 3, and 4).
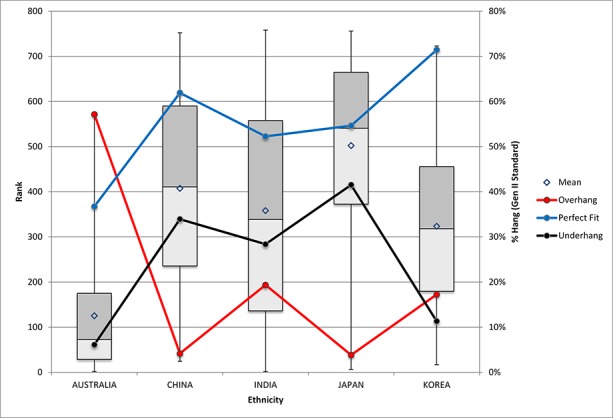
Fig. 2.

Figs. 2, 3, and 4 Aspect ratios (presented as Wilcoxon scores) in females across ethnicities presented as box plots (x axis) and corresponding prevalences of overhang (red), “perfect fit” (blue), and underhang (black) of the standard prosthesis (y axis). Ranked Wilcoxon scores are presented as surrogates for aspect ratios because the numerical differences between the aspect ratios were too small to be plotted. On the box plots, the horizontal lines indicate the medians, the tops and bottoms of the boxes indicate the interquartile ranges, the diamonds indicate the means, and the whiskers indicate the maximum and minimum. Fig. 2 Pairwise comparisons of values at the condylar level revealed the following significant differences. Aspect ratio: Australia versus India, Japan, and Korea; China versus India and Japan; India versus Australia and China; Japan versus Australia and China; and Korea versus Australia. Overhang: Australia versus China, India, Japan, and Korea. Perfect fit: Australia versus India and Korea; China versus India and Korea; India versus Australia, China, Japan, and Korea; Japan versus India and Korea; and Korea versus Australia, China, India, and Japan. Underhang: Australia versus China, India, and Japan; China versus Australia, India, and Korea; India versus Australia, China, Japan, and Korea; Japan versus Australia, India, and Korea; and Korea versus China, India, and Japan.
Fig. 3.

Pairwise comparisons of values at the junction level revealed the following significant differences. Aspect ratio: Australia versus China, Japan, and Korea; China versus Australia and Japan; India versus Japan; Japan versus Australia, China, and India; and Korea versus Australia. Overhang: Australia versus China, Japan, and Korea; China versus Australia and India; India versus China, Japan, and Korea; Japan versus Australia and India; and Korea versus Australia and India. Perfect fit: Australia versus Korea; China versus India and Korea; India versus China, Japan, and Korea; Japan versus India and Korea; and Korea versus Australia, China, India, and Japan. Underhang: Australia versus China, India, and Japan; China versus Australia and Korea; India versus Australia and Korea; Japan versus Australia and Korea; and Korea versus China, India, and Japan.
Fig. 4.
Pairwise comparisons of values at the trochlear level revealed the following significant differences. Aspect ratio: Australia versus China, India, Japan, and Korea; China versus Australia, Japan, and Korea; India versus Australia and Japan; Japan versus Australia, China, India, and Korea; and Korea versus Australia, China, and Japan. Overhang: Australia versus China, India, Japan, and Korea; China versus Australia, India, and Korea; India versus Australia, China, and Japan; Japan versus Australia, India, and Korea; and Korea versus Australia, China, and Japan. Perfect fit: Australia versus China, Japan, and Korea; China versus Australia; India versus Korea; Japan versus Australia and Korea; and Korea versus Australia, India, and Japan. Underhang: Australia versus China, India, and Japan; China versus Australia and Korea; India versus Australia, Japan, and Korea; Japan versus Australia, India, and Korea; and Korea versus China, India, and Japan.
The additional availability of a narrow femoral component improved the component fit more in females than in males. The availability of both the standard and the narrow versions for females improved the perfect-fit rate from 34.7% (with the standard version alone) to 55.1% (p = 0.03) in the Australian group, from 61.9% to 67.9% (p = 0.15) in the Chinese group, from 37.4% to 47.7% (p = 0.04) in the Indian group, from 55.7% to 59.6% (p = 0.26) in the Japanese group, and from 68.5% to 83.7% (p < 0.01) in the Korean group. In contrast, the availability of both the standard and the narrow versions improved the perfect-fit rate only marginally in the Australian, Chinese, and Indian males. The narrow version was not required for any males in the Japanese and Korean groups (Table IV).
TABLE IV.
Prevalences of “Perfect Fit,” Overhang, and Underhang When Standard and Narrow Components Available Compared with When Only Standard Component Available for all Ethnicities
Discussion
We found significant differences in the shape of the distal part of the femur between Asians and Caucasians and among different Asian ethnicities even after using a robust statistical test. Several authors have compared the morphology of Asian patients’ knees with the dimensions of TKA prostheses and suggested that currently available prostheses do not fit Asian patients well because of differences in knee shape between Caucasians and Asians3,11-15. However, there have been few direct comparisons of osseous morphology between Caucasians and Asians8,16. Our finding of larger aspect ratios in Asian populations compared with a Caucasian population differs from that of Yue et al.16 but is in line with that of Mahfouz et al.8. It is also in agreement with a recent systematic review comparing morphologic features of the knee among patients of various races9. We found that the knees of Caucasian patients were narrower at the condylar and trochlear levels, although more so at the trochlear level, giving them a more triangular shape as compared with a more rectangular shape in the Asian ethnic groups.
We wished to determine whether these differences in knee shape among ethnicities resulted in different prevalences of component fit. While the prevalences of component fit did differ between Asians and Caucasians and among different Asian ethnicities, differences in shape only partly accounted for those findings. For example, the Caucasian patients’ knees displayed the maximum prevalence of overhang while the Japanese patients’ knees displayed the minimum, in line with their corresponding aspect ratios. However, despite similar aspect ratios, the knees of the Chinese and Indian patients displayed significant differences in the prevalences of overhang as well as of perfect fit (Figs. 2, 3, and 4). We believe 2 factors may explain these differences. First, component-size selection may vary by surgeon technique. The prevalence of overhang would be lower if a surgeon downsizes more often and higher if he/she is more likely to upsize. Surgeons may tend to downsize the femoral component in some female patients because of difficulties in accommodating the mediolateral dimension of the prosthesis to the optimal anteroposterior dimension17. Second, this decision may vary depending on whether a posterior-stabilized or cruciate-retaining prosthesis is used. Surgeons using a posterior-stabilized prosthesis are more likely to upsize the femoral component to manage the relatively large flexion gap caused by sacrificing the posterior cruciate ligament (Table V and Fig. 5). At present, we cannot clearly identify the level along the femur at which anteroposterior overhang is most frequent or most clinically relevant. On the basis of the literature and our own observations, the anterior portion of the femur seems to have a higher prevalence of overhang than the posterior portion1,2,18,19 (Table VI) and, on the basis of a recent study, it seems that the anterior portion (trochlear level) may also be the most clinically relevant20.
Fig. 5.
Bar graph showing the sizes and types (posterior-stabilized [PS] or cruciate-retaining [CR]) of implants used in the study as well as the percentages that were upsized (blue bar), just fit (green bar), or were downsized (red bar). A higher percentage of posterior-stabilized TKAs were upsized, especially sizes 4 and 5, while a higher percentage of cruciate-retaining TKAs were downsized, especially sizes 3 and 4. Most of the study subjects had the posterior-stabilized configuration (n = 791) rather than the cruciate-retaining configuration (n = 174).
TABLE V.
Comparison of Upsizing and Downsizing of Posterior-Stabilized and Cruciate-Retaining TKAs
TABLE VI.
Studies Reporting on Prevalences of Overhang Along the Femur from Anterior to Posterior
Whether the narrow version of the femoral component adequately addresses overhang and whether it is required for both males and females are subjects of debate. Some authors have reported that using the narrow version when appropriate could almost completely eliminate the occurrence of overhang18. However, others have found that use of the narrow (sex-specific) version does not completely eliminate overhang in female patients17,19. They have thus suggested that additional geometric modifications of the narrow version may be required to accurately match female femoral anatomy. We found that although use of the narrow version significantly reduced the overhang rate in females in all 5 of the ethnic groups, there was still scope for further reduction.
While several authors have found the prevalence of overhang with the standard prosthesis to be negligible in males17,18, and therefore suggested that a narrower version may not be required for male patients at all, others have found that the narrow version would be required in 30% to 67% of males19,21. We found that up to 19% of males had ≥3 mm of overhang and would therefore need the narrow version.
There are concerns that always using the narrow sex-specific prosthesis in women as a strategy to prevent overhang results in a substantial percentage of underhang, with an 89% underhang rate reported in 1 study4. The current study demonstrates, however, that having both options available, and using the narrow version only when overhang is encountered with the standard version, can prevent overhang in a sizeable percentage of the population without unduly increasing the prevalence of underhang. These findings are in line with those of 2 recent studies10,21. In 1 of them, Dai et al. compared the fit of 6 different prosthetic designs in 3 ethnic groups and found that prostheses that offered multiple mediolateral/anteroposterior shape options reduced the overhang prevalence to zero10. In the other study, performed to evaluate how sex-specific or morphology-specific TKA prostheses improve component fit in the distal part of the femur in a Chinese population21, the highest perfect-fit rate was achieved when both the standard and the corresponding sex or morphology-specific knee prostheses were available. One of the potential drawbacks of providing additional mediolateral shape options is the increase in inventory, but we found that most cases of overhang involved sizes 5 to 8. This finding is supported by previous studies that also showed overhang to be more prevalent with larger sizes1,13. Therefore, we propose that the narrow version be made available only for these sizes.
This study had a number of limitations. First, only 1 design of TKA was used and it is not clear whether our conclusions can be extended to other designs. Second, as the study involved multiple centers and surgeons, surgical techniques and preferences may have biased the results. However, this is unlikely as all TKAs were performed by experienced surgeons who were diligent about balance and joint height. Third, we measured mediolateral widths after bone resection, and the amounts of distal femoral resection might have influenced measurements. However, since the mediolateral widths left after bone resection are more relevant to the design of femoral components, we believe that our measurement protocol provided more relevant information. Fourth, we restricted our study cohort to patients with medial compartment osteoarthritis and our results may not be applicable to those with predominantly lateral compartment or patellofemoral osteoarthritis. Fifth, all of our Caucasian patients were from Australia and may not have the same knee dimensions as patients from Europe or North America. Finally, outcomes for patients with overhang were not evaluated in this study so we cannot make any conclusions about the clinical implications of overhang.
In conclusion, the shape of the distal part of the femur differed between Caucasian patients residing in Australia and Asian patients and among Asian ethnicities. These differences along with interindividual variations and surgeon factors account for different prevalences of component fit across ethnicities with the same prosthesis. The additional availability of a femoral component with a reduced mediolateral dimension for the same anteroposterior size has the potential to reduce overhang and improve component fit across ethnicities.
Appendix
Acknowledgment List (Does Not Include Authors)
Disclosure of Potential Conflicts of Interest
Disclosure: Smith & Nephew provided funding for this study. The funding sources did not play a role in the investigation. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work and “yes” to indicate that the author had other relationships or activities that could be perceived to influence, or have the potential to influence, what was written in this work (http://links.lww.com/JBJSOA/A11).
The Asia Knee Research Team included Dr. Parag Sancheti, Professor Warwick Bruce, Dr. Tokifumi Majima, Dr. Hiroshi Ono, Dr. Tomohiro Onodera, Dr. Tatsuya Igarashi, and Young Gon Na, all of whom were coauthors of this paper. See the Appendix for a full acknowledgment list.
References
- 1.Mahoney OM, Kinsey T. Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences. J Bone Joint Surg Am. 2010. May;92(5):1115-21. [DOI] [PubMed] [Google Scholar]
- 2.Bonnin MP, Schmidt A, Basiglini L, Bossard N, Dantony E. Mediolateral oversizing influences pain, function, and flexion after TKA. Knee Surg Sports Traumatol Arthrosc. 2013. October;21(10):2314-24. Epub 2013 Feb 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung BJ, Kang JY, Kang YG, Kim SJ, Kim TK. Clinical implications of femoral anthropometrical features for total knee arthroplasty in Koreans. J Arthroplasty. 2015. July;30(7):1220-7. Epub 2015 Feb 18. [DOI] [PubMed] [Google Scholar]
- 4.Kim YH, Choi Y, Kim JS. Comparison of standard and gender-specific posterior-cruciate-retaining high-flexion total knee replacements: a prospective, randomised study. J Bone Joint Surg Br. 2010. May;92(5):639-45. [DOI] [PubMed] [Google Scholar]
- 5.Kim YH, Choi Y, Kim JS. Comparison of a standard and a gender-specific posterior cruciate-substituting high-flexion knee prosthesis: a prospective, randomized, short-term outcome study. J Bone Joint Surg Am. 2010. August 18;92(10):1911-20. [DOI] [PubMed] [Google Scholar]
- 6.Gao F, Guo W, Sun W, Li Z, Wang W, Wang B, Cheng L, Kush N. Correlation between the coverage percentage of prosthesis and postoperative hidden blood loss in primary total knee arthroplasty. Chin Med J (Engl). 2014;127(12):2265-9. [PubMed] [Google Scholar]
- 7.Hitt K, Shurman JR, 2nd, Greene K, McCarthy J, Moskal J, Hoeman T, Mont MA. Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am. 2003;85(Suppl 4):115-22. [PubMed] [Google Scholar]
- 8.Mahfouz M, Abdel Fatah EE, Bowers LS, Scuderi G. Three-dimensional morphology of the knee reveals ethnic differences. Clin Orthop Relat Res. 2012. January;470(1):172-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim TK, Phillips M, Bhandari M, Watson J, Malhotra R. What differences in morphologic features of the knee exist among patients of various races? A systematic review. Clin Orthop Relat Res. 2017. January;475(1):170-82. Epub 2016 Oct 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dai Y, Scuderi GR, Penninger C, Bischoff JE, Rosenberg A. Increased shape and size offerings of femoral components improve fit during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014. December;22(12):2931-40. Epub 2014 Jul 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ho WP, Cheng CK, Liau JJ. Morphometrical measurements of resected surface of femurs in Chinese knees: correlation to the sizing of current femoral implants. Knee. 2006. January;13(1):12-4. Epub 2005 Aug 24. [DOI] [PubMed] [Google Scholar]
- 12.Cheng FB, Ji XF, Lai Y, Feng JC, Zheng WX, Sun YF, Fu YW, Li YQ. Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee. 2009. October;16(5):341-7. Epub 2009 Feb 20. [DOI] [PubMed] [Google Scholar]
- 13.Ha CW, Na SE. The correctness of fit of current total knee prostheses compared with intra-operative anthropometric measurements in Korean knees. J Bone Joint Surg Br. 2012. May;94(5):638-41. [DOI] [PubMed] [Google Scholar]
- 14.Urabe K, Miura H, Kuwano T, Matsuda S, Nagamine R, Sakai S, Masuda K, Iwamoto Y. Comparison between the shape of resected femoral sections and femoral prostheses used in total knee arthroplasty in Japanese patients: simulation using three-dimensional computed tomography. J Knee Surg. 2003. January;16(1):27-33. [PubMed] [Google Scholar]
- 15.Chaichankul C, Tanavalee A, Itiravivong P. Anthropometric measurements of knee joints in Thai population: correlation to the sizing of current knee prostheses. Knee. 2011. January;18(1):5-10. Epub 2010 Feb 4. [DOI] [PubMed] [Google Scholar]
- 16.Yue B, Varadarajan KM, Ai S, Tang T, Rubash HE, Li G. Differences of knee anthropometry between Chinese and white men and women. J Arthroplasty. 2011. January;26(1):124-30. Epub 2010 Feb 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clarke HD, Hentz JG. Restoration of femoral anatomy in TKA with unisex and gender-specific components. Clin Orthop Relat Res. 2008. November;466(11):2711-6. Epub 2008 Aug 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guy SP, Farndon MA, Sidhom S, Al-Lami M, Bennett C, London NJ. Gender differences in distal femoral morphology and the role of gender specific implants in total knee replacement: a prospective clinical study. Knee. 2012. January;19(1):28-31. Epub 2011 Jan 28. [DOI] [PubMed] [Google Scholar]
- 19.Kawahara S, Okazaki K, Okamoto S, Iwamoto Y, Banks SA. A lateralized anterior flange improves femoral component bone coverage in current total knee prostheses. Knee. 2016. February 04 Aug;23(4):719-24. [DOI] [PubMed] [Google Scholar]
- 20.Pinskerova V, Nemec K, Landor I. Gender differences in the morphology of the trochlea and the distal femur. Knee Surg Sports Traumatol Arthrosc. 2014. October;22(10):2342-9. Epub 2014 Aug 6. [DOI] [PubMed] [Google Scholar]
- 21.Yue B, Wang J, Wang Y, Yan M, Zhang J, Zeng Y. How the gender or morphological specific TKA prosthesis improves the component fit in the Chinese population? J Arthroplasty. 2014. January;29(1):71-4. Epub 2013 May 22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.











