Abstract
Background:
Health-care worker (HCW) hand hygiene (HH) is the cornerstone of efforts to reduce hospital infections but remains low. Real-time mitigation of failures can increase process reliability to > 95% but has been challenging to implement for HH.
Objective:
To sustainably improve HCW HH to > 95%.
Methods:
A hospital-wide quality improvement initiative to improve HH was initiated in February 2012. HCW HH behavior was measured by covert direct observation utilizing multiple-trained HCW volunteers. HH compliance was defined as correct HH performed before and after contact with the patient or the patient’s care area. Interventions focusing on leadership support, HCW knowledge, supply availability, and culture change were implemented using quality improvement science methodology. In February 2014, the hospital began the Speaking Up for Safety Program, which trained all HCWs to identify and mitigate HH failures at the moment of occurrence and addressed known barriers to speaking up.
Results:
Between January 1, 2012, and January 31, 2016, there were 30,514 HH observations, averaging 627 observations per month (9% attending physicians, 12% resident physicians, 46% nurses, 33% other HCW types). HCW HH gradually increased from 75% to > 90% by December 2014. After the Speaking Up for Safety Program, HCW HH has been > 95% for 20 months. Physician HH compliance has been above 90% for over a year.
Conclusion:
Creating a specific process for staff to speak up and prevent HH failures, as part of a multimodal improvement effort, can sustainably increase HCW HH above 95%.
Hand hygiene is the most important action by health-care workers (HCWs) to prevent hospital-associated infections (HAIs).1,2 Despite this, a systematic review showed that average HCW hand hygiene compliance was around 40%.3 Most efforts to improve HCW hand hygiene focus on some combination of education and training, hand hygiene supply availability, workplace reminders, and feedback of compliance data.4,5 Studies have shown that these strategies can improve the hand hygiene behavior of HCWs, but sustained compliance above 90% remains a challenge.6–17 A recent systematic review identified goal setting, incentives, and accountability as interventions that may further improve hand hygiene compliance.4 Real-time identification of hand hygiene failures and direct individual accountability have been shown to improve compliance between 90–95%.18–22 This type of intervention not only identifies individual errors but if feedback is provided at the moment of the error, it also prevents them from reaching the patient. In these studies, real-time feedback was provided by a limited subset of individuals who usually also performed hand hygiene observations.18–21
This process of raising a concern about an observed action by another HCW that may result in a patient safety issue is termed “speaking up.” Although speaking up plays a vital role in providing safe care, HCWs frequently report challenges speaking up to others regarding witnessed errors, which impacts implementation and sustainability of these types of interventions.23–25 Safety culture may play an important role in facilitating or impeding speaking up. Error prevention training (EPT) has been used by a number of health-care organizations to train their employees in a common language and skill set to provide safe care. Organizations that have implemented EPT as part of multifaceted safety programs have significantly reduced medical errors and serious safety events and improved patient safety culture.26,27 Efforts to improve safety culture may catalyze hand hygiene improvement interventions such as speaking up to observed hand hygiene failures. Our goal was to develop a hospital-wide program to sustainably improve HCW hand hygiene to at least 95% using quality improvement methodology and error prevention strategies.
METHODS
Setting
This hand hygiene improvement program was developed at Arkansas Children’s Hospital (ACH), which is a 370-bed tertiary freestanding children’s hospital. There are 14 inpatient units, including 4 critical care units and a hematology–oncology unit. This project was reviewed by the University of Arkansas for Medical Sciences Institutional Review Board and determined to be quality improvement.
Intervention Development
In February 2012, members of the infection prevention program formed the hand hygiene improvement team. The Medical Director of Infection Prevention (W.M.L.) and an infection preventionist (M.H.) led the team. Members of hospital leadership, public relations, environmental services, the hospital’s software development group, frontline nursing, and the pediatric residency program were engaged at various points in the project to assist in development and testing of various interventions. A key driver diagram was developed to show the relationship between the project goal, key factors associated with improvement, and interventions (Figure 1). The key drivers included leadership support, HCW knowledge, supply availability, and culture change. These key drivers were identified based on guideline recommendations and evaluation of our own process.1,28 The final project goal was to improve hand hygiene compliance to ≥ 95% by July 2014. Appropriate hand hygiene practices of HCWs were defined based on published guidelines.1,28 We defined correct hand hygiene as covering the surfaces of the hands with an alcohol-based hand rub or washing hands with soap and water and turning off the faucet without using the fingertips or palms of the hand. For patients on transmission-based isolation precautions, hand hygiene needed to be performed before donning and after doffing personal protective equipment.
Fig. 1.
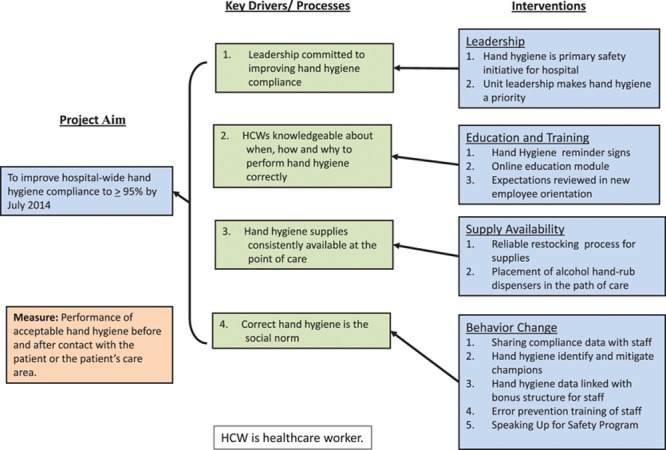
Key driver diagram depicting the relationship between interventions to improve HCW hand hygiene and the improvement goal.
Improvement Activities
The Model for Improvement was the primary improvement framework used. Plan, do, study, act cycles were used to test and refine various interventions.29 Interventions were usually tested on 1 or 2 units. Successful interventions were spread throughout the hospital.
Leadership Commitment.
Leadership at both the senior and unit-based levels was engaged in the improvement project.
Unit leadership makes hand hygiene a priority: unit leadership was expected to support various interventions, review monthly unit-based hand hygiene data with their staff, and reinforce the hospital’s hand hygiene expectations.
Hand hygiene designated as primary safety initiative for the hospital: senior hospital leadership showed their commitment to excellent hand hygiene by designating hand hygiene as the primary safety initiative for the hospital. The goal for 20132014 was 90%, and the goal for 2014–2015 was 95%. This was reinforced by regular messaging from senior hospital and medical leadership.
Education and Training.
HCWs needed to have a clear understanding of how, when, and why to perform hand hygiene correctly.
ACH Moments for Hand Hygiene signs posted: hand hygiene expectations were encapsulated in a reminder sign that was placed by elevators, unit entrances, and other locations throughout the hospital at the onset of the project. In May 2012, we placed additional signs on all doors to patient rooms.
Online education module: we created a brief electronic education module, which reviewed the indications for how, when, and why to perform hand hygiene correctly. Staff, including physicians, accessed the module through the hospital’s online training system, which also allowed unit leaders to track staff completion. Approximately 77% of staff completed the online education module by June 30, 2012.
Hand hygiene expectations incorporated into new employee orientation: we incorporated hand hygiene education and the hospital’s expectations to perform hand hygiene into new employee and new resident physician orientations.
Hand Hygiene Supplies Readily Available.
Hand hygiene supplies must be readily available at the point of care.
Hand hygiene supplies placed in the path of care: with staff input, we standardized the placement of hand hygiene supplies throughout the hospital.
Reliable stocking process developed: the improvement team worked with Environmental Services to ensure there was a reliable restocking process for hand hygiene supplies.
Making Hand Hygiene the Social Norm.
The key to sustained improvement in hand hygiene is to alter the habits of HCWs. Staff had to not only be aware of their own behavior but also feel that consistent correct hand hygiene was the expected social norm.
Sharing of compliance data with staff: in March 2012, monthly reports summarizing inpatient HCW hand hygiene compliance were electronically distributed to hospital leaders, including physician leaders, and visibly posted on each unit.
Hand hygiene data linked with bonus structure for staff: hospital employee bonuses were linked to achieving the annual hand hygiene goal, 90% for fiscal year 2014, 95% for fiscal year 2015. Bonuses were given to all ACH employees only if the overall hand hygiene goal was met. Physicians were not employed by the hospital; therefore, they were not connected to the bonus plan.
Hand hygiene champions: beginning in October 2012, we identified hand hygiene champions on 2 test units and trained them to identify hand hygiene failures at the time of occurrence and prevent the failure from occurring by speaking with staff in a nonconfrontational way. The intervention was later spread to 2 additional units. We were unable to sustain or further spread this intervention because the hand hygiene champions found it challenging to be the only people speaking up to others.
Formal EPT of all staff: beginning in February 2014, the hospital began formal EPT of all hospital employees and medical staff.30 This was completed in March 2015, with over 5,000 employees and physicians completing the training.
Speaking Up for Safety Program: The Speaking Up for Safety Program utilized the error prevention tool, ask, request, concern, chain of command, as a standardized framework for all staff to speak up and mitigate witnessed hand hygiene errors.30 We developed scripting to provide examples of what to say to colleagues.
Ask: Did you perform hand hygiene?
Request: Can I offer you some hand gel?
Concern: I have a concern that you are not performing hand hygiene
If any resistance was faced by staff when speaking up, the local nursing director or the Medical Director of Infection Prevention spoke with the resistant HCW. Speaking up events were documented on small cards, which served as a tracking system. During early implementation, the tracking cards were also used as raffle tickets for weekly drawings for prizes. The more a person spoke up, the more opportunities they had to win. Data showing the relationship between speaking up and hand hygiene were shared with staff. Between February and June 2014, the Speaking Up for Safety Program was spread to all inpatient units.
Data Collection
For the purpose of observation, hand hygiene compliance was defined as correct hand hygiene preformed before and after contact with the patient or the patient’s care area (patient’s bed, over-the-bed table, and any medical equipment connected to or associated with that patient’s care). Hand hygiene observations were made by over 100 HCW volunteers and recorded covertly during routine care. Observations were made daily on all units and all HCW types and recorded electronically. Data were transferred real-time to an electronic data visualization program viewable by all staff. We have previously reported the details of this observation program.31
Analysis
Run charts were created using Microsoft Excel to display monthly hand hygiene compliance over time.32 We annotated the run charts to show the relationship between interventions and the monthly hand hygiene compliance. Nonrandom changes in the data were detected using standard run chart rules: shift (6 or more points all above or all below the centerline) and trend (5 or more points all going up or all going down).32
RESULTS
Between January 1, 2012, and January 31, 2016, there were 30,514 hand hygiene observations, averaging 627 observations per month (9% attending physicians, 12% resident physicians, 46% nurses, 33% other HCW types). Other HCW types included patient care technicians, respiratory therapists environmental services, medical students, and various other ancillary staff. HCW observations for patients on transmission-based isolation precautions accounted for 28% of observations. Half (54%) of the observations were during day shifts, and 46% were done during night shifts. One quarter (24%) of the observations were on weekends.
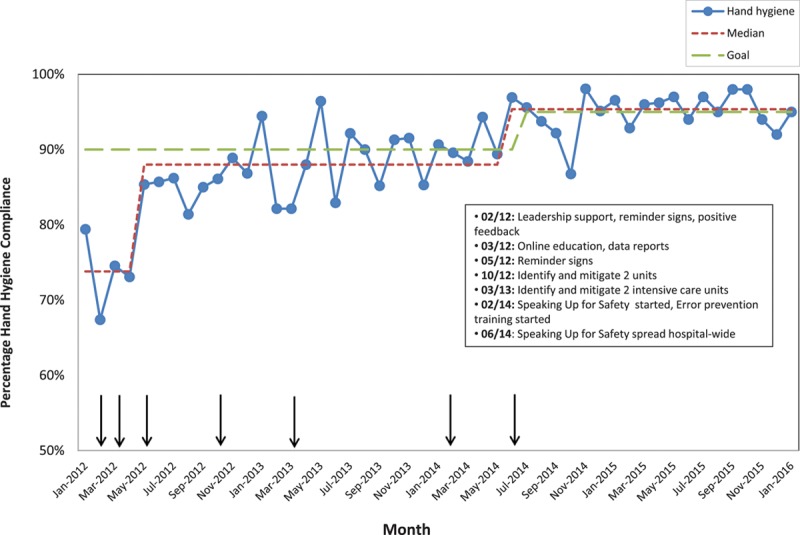
Figure 2 shows the annotated run chart displaying the relationship of interventions to improve hand hygiene and the change in HCW hand hygiene compliance over time. Baseline hand hygiene compliance was 75%. After the initial interventions (education, reminder signs, data feedback), hand hygiene compliance increased to an average of 82%. In association with an ongoing institutional focus on hand hygiene and efforts to identify and mitigate hand hygiene errors, HCW hand hygiene continued to gradually increase to 90% in December 2012 and averaged 91% for the next 18 months. After implementation of the Speaking Up for Safety Program and the start of EPT, overall hand hygiene compliance increased to 95% and has been sustained for 20 months.
Fig. 2.
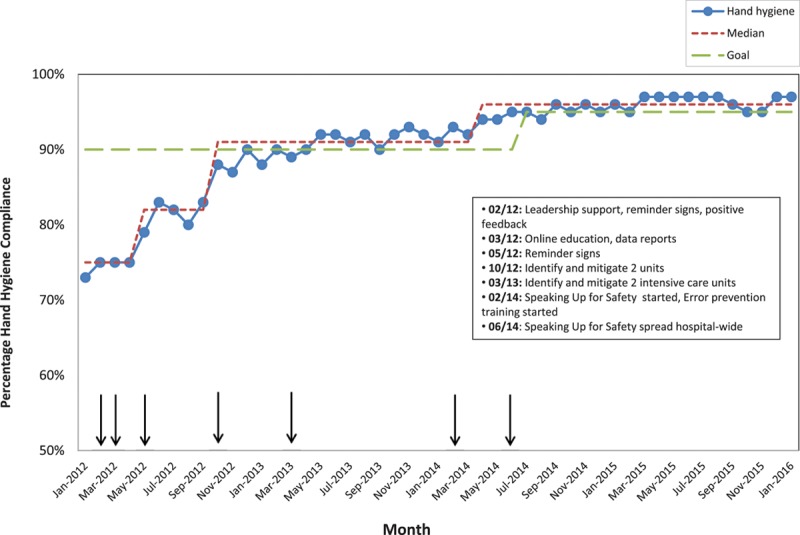
Annotated run chart showing hospital-wide hand hygiene compliance percentage by month from January 2012 through January 2016.
Figures 3–6 show the change in hand hygiene compliance over time for different HCW types in relation to the various improvement efforts. Baseline hand hygiene compliance was highest for nurses (86%) and lowest for resident physicians (62%). Since June 2014, the average hand hygiene compliance of all HCW types, except resident physicians, (nurses, attending physicians, and other HCW types) has been at least 95%. Resident physician hand hygiene compliance increased to an average of 93% by November 2014.
Fig. 3.
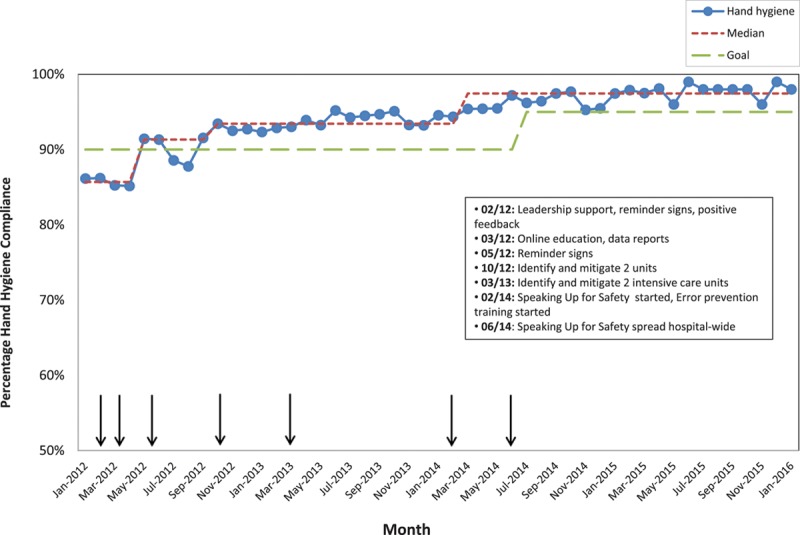
Annotated run chart showing hospital-wide hand hygiene compliance percentage by month for nurses from January 2012 through January 2016.
Fig. 6.
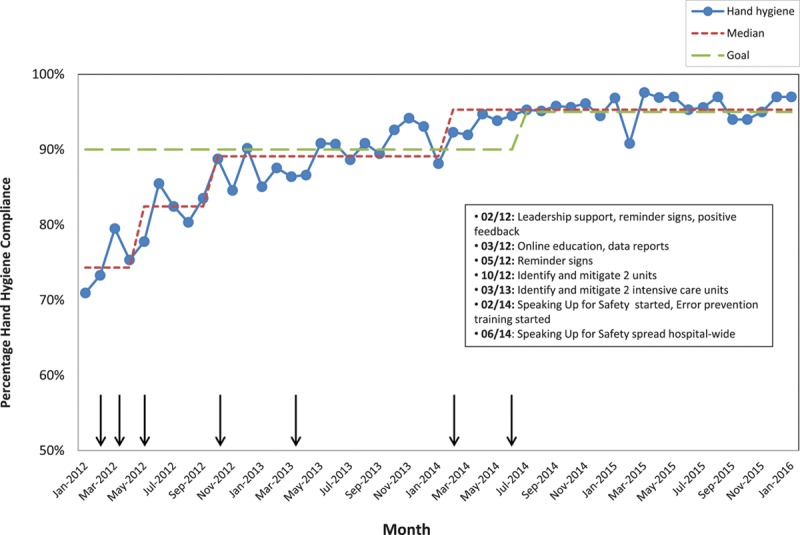
Annotated run chart showing hospital-wide hand hygiene compliance percentage by month for other HCW groups from January 2012 through January 2016. Other HCW groups include patient care technicians, respiratory therapists environmental services, medical students, and various other ancillary staff.
Fig. 4.
Annotated run chart showing hospital-wide hand hygiene compliance percentage by month for attending physicians from January 2012 through January 2016.
Fig. 5.
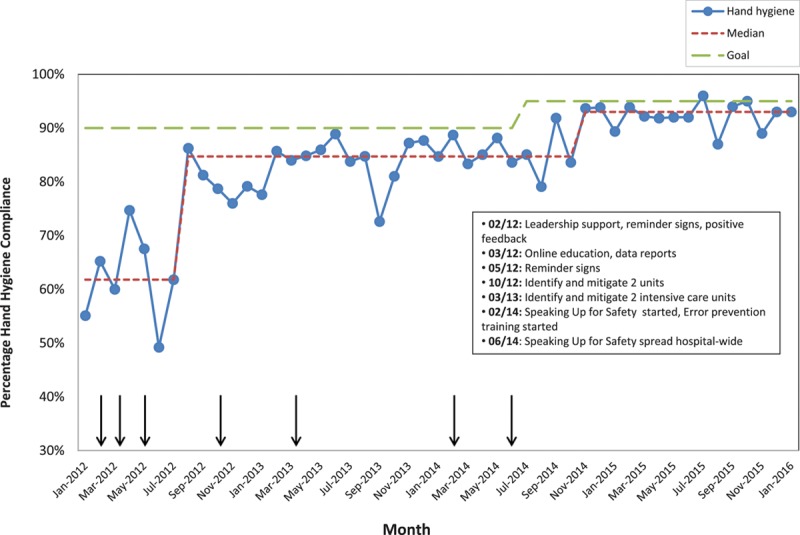
Annotated run chart showing hospital-wide hand hygiene compliance percentage by month for resident physicians from January 2012 through January 2016.
DISCUSSION
Through implementation of a multimodal initiative, we were able to improve HCW hand hygiene compliance to 90% or greater for 38 months and 95% or greater for 20 months. In addition, the average hand hygiene compliance of all physicians has remained above 90% for over a year. Our ability to sustainably improve physician hand hygiene is a noteworthy success.
Use of a multimodal approach is recommended to improve HCW hand hygiene. The World Health Organization recommends a combination of education and training, supply availability, feedback of compliance data, workplace reminders, and an institutional focus on improving hand hygiene.28 Two recent systematic reviews support the effectiveness of this combination of interventions to improve hand hygiene.4,5 Although this bundle consistently improves HCW hand hygiene, compliance rarely exceeds 85%.6,9–17 In addition, physician compliance usually lags, averaging 10–15% below overall compliance.6,9,11,12,16,17 Our initial interventions (education, reminder signs, institutional focus, and data feedback) were similar to the WHO bundle, and consistent with other studies, our average hand hygiene compliance between May and September 2012 improved to only 82%. In general, interventions such as education, increased awareness, reminders, and feedback help create a standardized process and increase awareness of that new process but typically only improve process reliability to 80–90%.33,34
Multiple studies that measure hand hygiene compliance by self-reporting have shown that HCWs believe their hand hygiene behavior is better than it actually is.28,35,36 Providing individual real-time feedback has been shown to increase hand hygiene compliance above 90%.18–20 Despite awareness that speaking up can prevent unsafe care, research shows HCWs frequently remain silent when faced with an opportunity to speak up and prevent an error.23–25 In a case vignette study of HCWs on an oncology unit, only 68% expressed a high likelihood of speaking up about a hand hygiene error, but actual speaking up behavior would likely be less.23 Factors influencing a HCW’s decision to speak up include the perceived safety risk, clarity of when to speak up, fear of reprisal, perceived efficacy of speaking up, leadership support, presence of an audience, and prior experiences.23–25 The hand hygiene champion intervention was our first attempt to have HCWs speak up to prevent witnessed hand hygiene errors. This intervention utilized only a few trained HCWs (not necessarily observers). The hand hygiene champions found it challenging to be the only people speaking up. The inability to sustain this intervention was likely impacted by failure to address factors known to influence speaking up.23–25 Although hand hygiene compliance increased to 90% after starting the hand hygiene champion intervention, the sustained increase was also a result of continued leadership focus on hand hygiene, regular data feedback to employees, clear hospital-wide goals, and employee incentives. Our program later implemented the Speaking Up for Safety Program, which created a standardized process using error prevention principles designed to address common barriers to speaking up such as fear of reprisal and perceived efficacy. Addressing these barriers likely contributed to the success of this program. Initially, HCWs had to speak up more frequently to not only address more frequent failures but also set the behavioral expectation. Over time, less frequent speaking up was necessary to sustain compliance above 95%. This is likely due to hand hygiene becoming the social norm.
Social norms are informal understandings that dictate the behavior of society or groups.37 Hand hygiene, like many behaviors, is guided by ingrained habits and social norms.21 There is a social dilemma associated with HCW hand hygiene. Because it is easier to omit hand hygiene, this drives individual HCW behavior toward noncompliance. Conversely, the benefits associated with hand hygiene (reduced HAIs) are only achieved if all HCWs consistently perform hand hygiene. To create a social norm in which HCWs consistently perform hand hygiene requires not only changing personal attitudes but also social expectations.37 Although education and supply availability can change HCW attitudes about hand hygiene and increase their perceived self-efficacy, these interventions do not adequately alter the social expectation to perform hand hygiene. By demonstrating that enough HCWs are performing hand hygiene correctly and that enough HCWs believe hand hygiene should be performed and would negatively sanction the omission of hand hygiene, consistent HCW hand hygiene can become the new social norm.37 In our initiative, by providing regular feedback of hand hygiene behavior, HCWs were made aware that the majority of HCWs were performing hand hygiene. The Speaking Up for Safety Program created the normative expectation to perform hand hygiene. Hand hygiene improvement efforts frequently include education, supply availability, and data feedback. The addition of a process to speak up to prevent hand hygiene errors may be important to alter social expectations and make HCW hand hygiene the social norm.
There were a few limitations associated with this project. This project was performed at a single children’s hospital, and interventions may not be readily applied to other health-care settings. Despite efforts to ensure accurate and consistent hand hygiene data collection, observers may have recorded some observations incorrectly or may have been subject to observer bias. In addition, Hawthorne effect may have resulted in HCWs adjusting their behavior due to awareness that their hand hygiene was being observed.38 Based on surveys of our staff, most HCWs were unaware when they were being observed; therefore, Hawthorne effect was likely limited.31 It is possible that the improvements in hand hygiene were not directly related to our interventions. This is unlikely as hand hygiene improvements were temporally associated with the various interventions implemented, and the degree of improvement associated with each intervention was consistent with published literature.34 Although resident physician hand hygiene improved, it was less than other HCW groups and failed to meet the hospital’s goals. The reason for this is unclear. It is possible that some resident hand hygiene opportunities occurred separate from team rounds and, therefore, lacked the positive influence of peer behavior and attending physician role modeling. It is also possible that nurses still may have been less likely to speak up to resident physicians, despite the Speaking Up for Safety Program. We were not able to show a relationship between increased hand hygiene and a reduction in HAIs. During this project, the hospital implemented a new diagnostic test for respiratory viruses. This resulted in increased detection with a subsequent increase in respiratory viral HAIs and an increase in overall HAIs.
CONCLUSIONS
Sustained improvement in HCW hand hygiene requires both infrastructure, such as education, reminders and supply availability, and interventions to drive social expectation toward the desired social norm. Our Speaking Up for Safety Program facilitated staff speaking up to prevent hand hygiene failures. Over time, speaking up helped successfully create a new social norm and helped us sustain HCW hand hygiene above 95%. Additional work is needed to determine whether interventions like Speaking Up for Safety can be implemented in other health-care settings or applied to improve other HCW behaviors.
ACKNOWLEDGMENTS
The authors would like to thank the numerous health-care worker volunteers who made our hand hygiene program possible. The authors would also like to thank the software development group at Arkansas Children’s Hospital for their assistance in development of the electronic data collection and observation programs.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Presented in part at the SHEA Spring Conference, May 14–17, 2015, Orlando, FL.
REFERENCES
- 1.Boyce JM, Pittet D; Healthcare Infection Control Practices Advisory Committee. Society for Healthcare Epidemiology of America. Association for Professionals in Infection Control. Infectious Diseases Society of America. Hand Hygiene Task Force. Guideline for hand hygiene in health-care settings: recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Infect Control Hosp Epidemiol. 2002;23:S3–40.. [DOI] [PubMed] [Google Scholar]
- 2.Allegranzi B, Pittet D. Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect. 2009;73:305–315.. [DOI] [PubMed] [Google Scholar]
- 3.Erasmus V, Daha TJ, Brug H, et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 2010;31:283–294.. [DOI] [PubMed] [Google Scholar]
- 4.Luangasanatip N, Hongsuwan M, Limmathurotsakul D, et al. Comparative efficacy of interventions to promote hand hygiene in hospital: systematic review and network meta-analysis. BMJ. 2015;351:h3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schweizer ML, Reisinger HS, Ohl M, et al. Searching for an optimal hand hygiene bundle: a meta-analysis. Clin Infect Dis. 2014;58:248–259.. [DOI] [PubMed] [Google Scholar]
- 6.Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet. 2000;356:1307–1312.. [DOI] [PubMed] [Google Scholar]
- 7.Zerr DM, Allpress AL, Heath J, et al. Decreasing hospital-associated rotavirus infection: a multidisciplinary hand hygiene campaign in a children’s hospital. Pediatr Infect Dis J. 2005;24:397–403.. [DOI] [PubMed] [Google Scholar]
- 8.Pessoa-Silva CL, Hugonnet S, Pfister R, et al. Reduction of health care associated infection risk in neonates by successful hand hygiene promotion. Pediatrics. 2007;120:e382–e390.. [DOI] [PubMed] [Google Scholar]
- 9.Aboumatar H, Ristaino P, Davis RO, et al. Infection prevention promotion program based on the PRECEDE model: improving hand hygiene behaviors among healthcare personnel. Infect Control Hosp Epidemiol. 2012;33:144–151.. [DOI] [PubMed] [Google Scholar]
- 10.Brown SM, Lubimova AV, Khrustalyeva NM, et al. Use of an alcohol-based hand rub and quality improvement interventions to improve hand hygiene in a Russian neonatal intensive care unit. Infect Control Hosp Epidemiol. 2003;24:172–179.. [DOI] [PubMed] [Google Scholar]
- 11.Dierssen-Sotos T, Brugos-Llamazares V, Robles-García M, et al. Evaluating the impact of a hand hygiene campaign on improving adherence. Am J Infect Control. 2010;38:240–243.. [DOI] [PubMed] [Google Scholar]
- 12.Grayson ML, Russo PL, Cruickshank M, et al. Outcomes from the first 2 years of the Australian National Hand Hygiene Initiative. Med J Aust. 2011;195:615–619.. [DOI] [PubMed] [Google Scholar]
- 13.Ho ML, Seto WH, Wong LC, et al. Effectiveness of multifaceted hand hygiene interventions in long-term care facilities in Hong Kong: a cluster-randomized controlled trial. Infect Control Hosp Epidemiol. 2012;33:761–767.. [DOI] [PubMed] [Google Scholar]
- 14.Helder OK, Brug J, Looman CW, et al. The impact of an education program on hand hygiene compliance and nosocomial infection incidence in an urban neonatal intensive care unit: an intervention study with before and after comparison. Int J Nurs Stud. 2010;47:1245–1252.. [DOI] [PubMed] [Google Scholar]
- 15.Trick WE, Vernon MO, Welbel SF, et al. ; Chicago Antimicrobial Resistance Project. Multicenter intervention program to increase adherence to hand hygiene recommendations and glove use and to reduce the incidence of antimicrobial resistance. Infect Control Hosp Epidemiol. 2007;28:42–49.. [DOI] [PubMed] [Google Scholar]
- 16.Tromp M, Huis A, de Guchteneire I, et al. The short-term and long-term effectiveness of a multidisciplinary hand hygiene improvement program. Am J Infect Control. 2012;40:732–736.. [DOI] [PubMed] [Google Scholar]
- 17.Kirkland KB, Homa KA, Lasky RA, et al. Impact of a hospital-wide hand hygiene initiative on healthcare-associated infections: results of an interrupted time series. BMJ Qual Saf. 2012;21:1019–1026.. [DOI] [PubMed] [Google Scholar]
- 18.Linam WM, Margolis PA, Atherton H, et al. Quality-improvement initiative sustains improvement in pediatric health care worker hand hygiene. Pediatrics. 2011;128:e689–e698.. [DOI] [PubMed] [Google Scholar]
- 19.White CM, Statile AM, Conway PH, et al. Utilizing improvement science methods to improve physician compliance with proper hand hygiene. Pediatrics. 2012;129:e1042–e1050.. [DOI] [PubMed] [Google Scholar]
- 20.Talbot TR, Johnson JG, Fergus C, et al. Sustained improvement in hand hygiene adherence: utilizing shared accountability and financial incentives. Infect Control Hosp Epidemiol. 2013;34:1129–1136.. [DOI] [PubMed] [Google Scholar]
- 21.Cumbler E, Castillo L, Satorie L, et al. Culture change in infection control: applying psychological principles to improve hand hygiene. J Nurs Care Qual. 2013;28:304–311.. [DOI] [PubMed] [Google Scholar]
- 22.Cunningham D, Brilli RJ, McClead RE, Jr., et al. The safety stand-down: a technique for improving and sustaining hand hygiene compliance among health care personnel. J Patient Saf. 2015. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 23.Schwappach DL, Gehring K. Silence that can be dangerous: a vignette study to assess healthcare professionals’ likelihood of speaking up about safety concerns. PLoS One. 2014;9:e104720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okuyama A, Wagner C, Bijnen B. Speaking up for patient safety by hospital-based health care professionals: a literature review. BMC Health Serv Res. 2014;14:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lyndon A, Sexton JB, Simpson KR, et al. Predictors of likelihood of speaking up about safety concerns in labour and delivery. BMJ Qual Saf. 2012;21:791–799.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brilli RJ, McClead RE, Jr, Crandall WV, et al. A comprehensive patient safety program can significantly reduce preventable harm, associated costs, and hospital mortality. J Pediatr. 2013;163:1638–1645.. [DOI] [PubMed] [Google Scholar]
- 27.Muething SE, Goudie A, Schoettker PJ, et al. Quality improvement initiative to reduce serious safety events and improve patient safety culture. Pediatrics. 2012;130:e423–e431.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pittet D, Allegranzi B, Boyce J. The World Health Organization guidelines on hand hygiene in health care and their consensus recommendations. Infect Control Hosp Epidemiol. 2009;30:611–622.. [DOI] [PubMed] [Google Scholar]
- 29.Langley GJ, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 19961st ed. San Francisco: Jossey-Bass Publishers. [Google Scholar]
- 30.Healthcare Performance Improvement. Safety culture intervention implementation. Available at http://hpiresults.com/index.php/intro/what-we-do/30. Accessed December 10, 2015.
- 31.Linam WM, Honeycutt MD, Gilliam CH, et al. Successful development of a direct observation program to measure health care worker hand hygiene using multiple trained volunteers. Am J Infect Control. 2016;44:544–547.. [DOI] [PubMed] [Google Scholar]
- 32.Perla RJ, Provost LP, Murray SK. The run chart: a simple analytical tool for learning from variation in healthcare processes. BMJ Qual Saf. 2011;20:46–51.. [DOI] [PubMed] [Google Scholar]
- 33.Luria JW, Muething SE, Schoettker PJ, et al. Reliability science and patient safety. Pediatr Clin North Am. 2006;53:1121–1133.. [DOI] [PubMed] [Google Scholar]
- 34.Nolan T, Resar R, Haraden C, Griffin FA. Improving the Reliability of Health Care. IHI Innovation Series white paper. Boston, MA: Institute for Healthcare Improvement; 2004. Available at: http://www.IHI.org. Accessed November 3, 2010. [Google Scholar]
- 35.Jenner EA, Fletcher BC, Watson P, et al. Discrepancy between self-reported and observed hand hygiene behaviour in healthcare professionals. J Hosp Infect. 2006;63:418–422.. [DOI] [PubMed] [Google Scholar]
- 36.Haas JP, Larson EL. Measurement of compliance with hand hygiene. J Hosp Infect. 2007;66:6–14.. [DOI] [PubMed] [Google Scholar]
- 37.Mackie G, Moneti F, Shakya H, Denny E. What are social norms? How are they measured? 2015. Available at https://www.unicef.org/protection/files/4_09_30_Whole_What_are_Social_Norms.pdf. Accessed November 28 2016.
- 38.Eckmanns T, Bessert J, Behnke M, et al. Compliance with antiseptic hand rub use in intensive care units: the Hawthorne effect. Infect Control Hosp Epidemiol. 2006;27:931–934.. [DOI] [PubMed] [Google Scholar]


