Supplemental Digital Content is available in the text.
Abstract
Introduction:
Millennial trainees prefer innovative, multimodal education on topics including the physical exam (PE). Attendings inconsistently meet these needs on family-centered rounds. To enhance PE teaching, a Web site (PEToolkit) was created, but its use was infrequent. We aimed to increase PEToolkit use from 2 to 5 page counts per week in 7 months.
Methods:
This quality improvement project took place at a large academic center in 1 Hospital Medicine team. Key drivers informed interventions, and an annotated run chart tracked progress. We tracked secondary measures, including changes in perception of teaching skill among attendings and resident-observed methods of PE teaching, through survey methodology.
Results:
Median page counts increased to 5 counts per week in 7 months. The most impactful interventions included training senior residents to teach with the PEToolkit Web site and team feedback on Web site usage midweek. Survey responses from 37 attendings showed that those with more exposure to PEToolkit had increased self-perceived skill of PE teaching (P = 0.02). Survey responses from 52 residents showed that those on the intervention team reported more use of video for PE teaching (P < 0.001) and higher frequency of PE teaching (P = 0.02), compared with those on the nonintervention team.
Conclusions:
We increased PEToolkit Web site use during family-centered rounds, thereby emphasizing the importance of PE teaching in this setting in an innovative way. Engagement of learners, frequent feedback, and coaching should be considered when incorporating technology in teaching.
INTRODUCTION
Over the past decade, physician trainees have increasingly utilized online resources and mobile applications to obtain medical information. Devices including smartphones and electronic tablets allow for easy information access that augments patient care and teaching.1–3 Today’s learners also prefer the use of multiple teaching modes (visual, auditory, reading, writing, and kinesthetic) to integrate new knowledge, rather than traditional verbal clinical instruction.4–7 Despite the desire of millennial learners to incorporate technology and multimodal education methods into their learning strategies, their teachers and curricula may lag behind.8
As one avenue for interactive learning, family-centered rounds (FCR) has had an overall positive response from trainees and families in that an integrated team at the bedside allows for effective communication regarding the plan of care.9–12 However, FCR may be time-intensive, potentially leading to missed teaching opportunities.10,13,14 One such potentially overlooked opportunity that learners perceive is the teaching of physical exam (PE) technique at the bedside; FCR provides an opportunity to engage learners by modeling exam skills on patients.15–17
Due to the limited use of multimodal learning as a strategy for teaching PE findings, the study team created a Web site containing PE-related multimedia called the PEToolkit (www.physicalexamtoolkit.com).18 The site, organized by organ system, contains descriptive text, visual aids, audio, and video clips related to PE technique, including normal and abnormal findings. The content of the Web site was garnered from multiple Internet sources to collate publicly available multimedia into a central location that was easily accessible to attending physicians. This content was reviewed and formatted by members of the study team to ensure validity, and the Web site was beta-tested by 12 attendings and fellows before it was made available to learners.
One Hospital Medicine (HM) team was provided a hospital-issued electronic tablet, for ease of access to the PEToolkit Web site. Baseline data were collected for 3 months to assess usage starting in June 2015, and use of the PEToolkit Web site was low, at a median of 2 page counts per week. Our primary aim was to increase PEToolkit Web site use from 2 to 5 page counts per week within 7 months. Our secondary objectives were to evaluate resident perceptions of PE teaching on rounds and attending comfort with teaching PE as well as with teaching using technology.
METHODS
Setting
The study took place at Cincinnati Children’s Hospital Medical Center, a 628-bed pediatric academic medical center, with more than 30,000 admissions annually. The Division of Hospital Medicine includes 45 faculty, 8 staff physicians, and 7 fellows, who provide clinical service on 5 general pediatric inpatient teams. These teams typically consist of an attending, a fellow, 2 senior residents, 3 interns, and 3 medical students. When on FCR, the teams utilize computers-on-wheels to access the electronic health record and other resources.
Planning the Intervention
The quality improvement (QI) team consisted of an HM fellow leader, 4 HM attending physicians, an HM nurse practitioner, a clinical research coordinator, and a pediatric resident, who participated in a 7-month local QI collaborative course. The model for improvement was used as a framework to guide study design.19 The team mapped the rounding process and conducted a failure mode and effects analysis (see Figure, Supplemental Digital Content 1, http://links.lww.com/PQ9/A13). The team noted multiple barriers to teaching on rounds using technology, such as access to a device and comfort with navigating the Web site. These informed key drivers to plan and prioritize interventions, including awareness of millennial learning preferences, comfort with technology, familiarity with Web site content, and attending physician and learner engagement (Fig. 1). Our primary measure was to increase PEToolkit use from 2 to 5 page counts per week between August 2015 and February 2016. As PE may compete with other valuable teaching topics, we chose a goal of 5 to provide attendings flexibility to teach a variety of subjects while on service. Our secondary measures were change in resident perception of, and attending perceived skill level with, teaching PE at the bedside and use of technology during FCR pre- to postintervention.
Fig. 1.
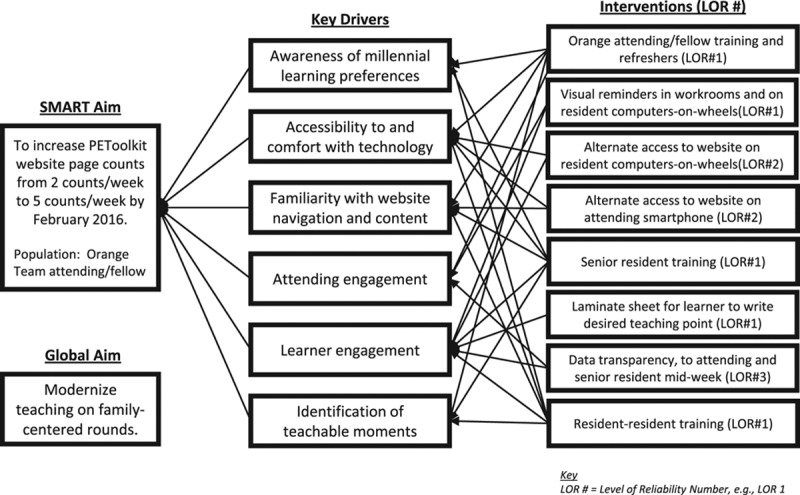
Key driver diagram. LOR, level of reliability.
Improvement Activities
As the team planned each PDSA cycle of intervention, we continually elicited formative feedback from residents and attendings on the intervention team to guide the next ramp of improvement. We assigned levels of reliability to each intervention, with level 1 for awareness and training, level 2 for built-in redundancies in the system, and level 3 for identification and prevention of failures.19
Education and Training.
In June 2015, the QI team leader conducted a 1-hour workshop with the HM attendings and fellows scheduled for service on the intervention team. This session included an explanation of the project, how to use the electronic tablet, how to access the PEToolkit Web site, and a small group exercise to practice how to use the Web site for teaching. If there were several weeks to months between initial training and a week of service, the QI team leader conducted training refreshers with the intervention team attending before his/her week of service.
Initial Reminders and Feedback.
Attendings were e-mailed a daily calendar invite before the start of rounds, as a reminder to bring the electronic tablet. At the end of the week of service, the attending and/or fellow was asked to provide feedback on the Web site, the electronic tablet, and any reasons for failure of use. This information was collected each week by the study team, along with the daily Web site page counts.
Visual Reminders.
The team created visual reminders to place in clinical work areas, to ensure both attendings and trainees were aware of the PEToolkit Web site. A poster containing information about the Web site content and directions for access was posted in both resident and attending workrooms. In addition, colorful laminated cards containing the logo and Web site address were placed on the corners of workroom computer monitors.
Alternate Points of Access.
Upon discovering that attendings occasionally forgot to bring the electronic tablet to rounds, the study team added alternate points of access to the Web site to the resident computers-on-wheels and the attending smartphones. These included adding the Web site to the “favorites” area of Web browsers, as well as loading shortcuts to the main screens.
Learner Engagement.
The study team assessed current interventions and determined that greater learner engagement was needed. We thus began training senior residents on how to use the electronic tablet and access the PEToolkit Web site. A visual prompt, in the form of a laminated placard on resident computers-on-wheels, was also created to obtain medical student teaching requests.
Data Transparency.
Both the attending and senior residents received midweek feedback regarding their usage of the Web site.
Secondary Measures
The attendings were surveyed during the study period to assess change in perception of teaching on FCR. Eligible participants were those who provided clinical service on the 5 general pediatric inpatient teams during this time. The surveys included (1) a prestudy survey distributed to eligible HM attendings and fellows, inquiring about years of experience, training in teaching, comfort level in teaching about the PE at the bedside, and comfort with use of technology to teach, (2) a poststudy survey distributed at the end of the QI project, to assess change in comfort level. Residents from 2 groups, intervention (1 HM team) and nonintervention (2 HM teams), were also surveyed at 2 time points (1) at the start of each 4-week HM rotation inquiring about year of training, comfort with PE skills, teaching on rounds, preferred learning styles, and use of technology in medical education and (2) at the end of the month, to assess differences in observed teaching methods between teams. If a resident was scheduled for the rotation more than once during the study period, only the first survey response was included for analysis. Nonintervention teams were teams whose attendings had knowledge of the project and access to the PEToolkit Web site but were not provided with training or an electronic tablet.
Planning the Study of the Intervention
A run chart was used to follow weekly usage data from the PEToolkit Web site. As the Web site is capable of recording unique page counts per day, the team was able to discern frequency of daily use by the intervention team, as well as other teams and guest users. The total number of page counts for the intervention team attending were plotted each week. Special cause variation was identified on the run chart using accepted rules, with 8 consecutive points above or below the centerline, indicating a shift in the median.20
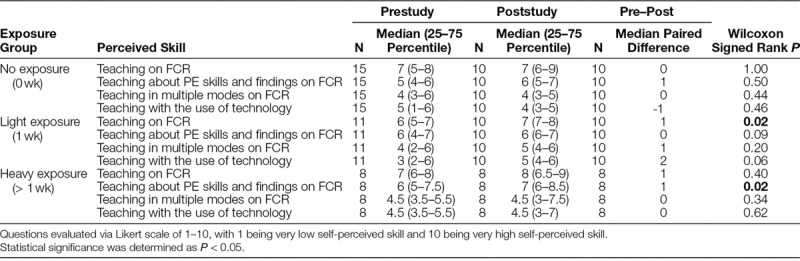
Survey Analysis.
We divided HM attendings into groups of no exposure, light exposure (1 week of service on intervention team), and heavy exposure (> 1 week of service on intervention team) at the end of the study period. Descriptive statistics, medians, and interquartile ranges for Likert-scale variables were generated by exposure group and by study time point: pre- and poststudy period. Paired pre–post results for the exposure groups were compared using Wilcoxon signed rank test.
We divided residents into groups of intervention and nonintervention teams. Similar descriptive statistics were generated by intervention group and by study time point: pre- and postrotation. Baseline and postrotation measures were compared between intervention and nonintervention groups using Wilcoxon rank sum test for ordinal variables and Fisher’s exact for binary variables. Statistical significance was determined as P < 0.05.
Ethical Considerations
The study was approved as an exempted review, with waiver of written consent, by the Cincinnati Children’s Hospital Medical Center Institutional Review Board. All eligible participants were given the option to opt out of completing the electronic surveys, and the results were deidentified during analysis.
RESULTS
Over an initial 7-month period with 28 attending and fellow participants, PEToolkit page counts increased from 2 to 5 counts per week (Fig. 2). The most impactful interventions were training of the senior residents and midweek feedback to the intervention team regarding their use of the Web site. In February 2016, when in-person reminders were discontinued to automate the process, we noted a trend toward decreased attending use of the PEToolkit Web site. To mitigate this concern, the team leader resumed in-person trainings and refreshers with the intervention team attendings, and PEToolkit Web site usage subsequently stabilized.
Fig. 2.
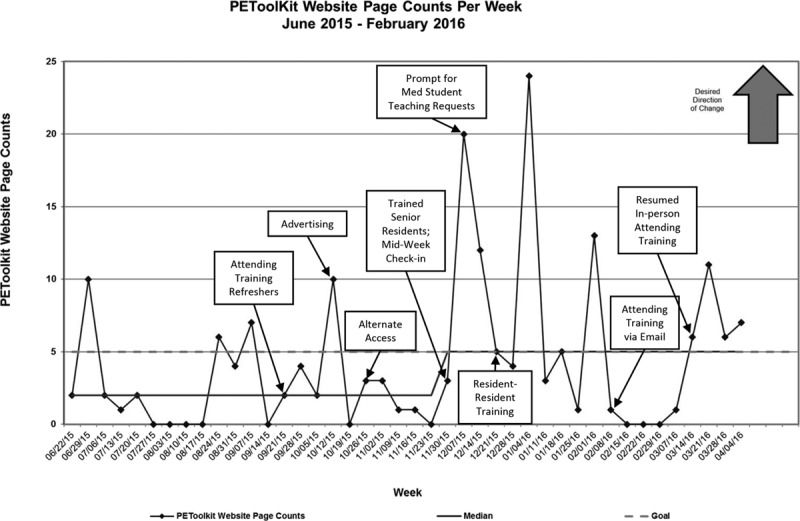
Run chart. Line with points, PEToolkit Web site page counts; solid horizontal line, median; dashed line, goal.
Daily census data on the intervention team were collected from September 2015 through February 2016. The median census was 12 patients, and the average daily census was 11.3 patients.
For our secondary measures, 37 of 44 eligible attendings completed the presurvey (84%), and 28 of 34 eligible attendings completed the postsurvey 1 year later (82%), resulting in 28 paired pre- to poststudy responses (Table 1). Ten survey respondents had no exposure, and 9 had light exposure. Eight attendings had heavy exposure, with a median of 2 weeks (interquartile ratio, 2–3). There was no difference between the attending groups regarding years of experience or previous training in teaching. Surveys were also sent to 101 residents over the 8-month study period; 52 completed the postsurvey (51%), with 23 in the intervention group and 29 in the nonintervention group. The attending and resident survey results had several notable findings. The heavy exposure group had a significant increase in comfort with PE teaching on FCR (P = 0.02); however, none of the 3 exposure groups had significant change in comfort of teaching with technology over the past year (Table 2).
Table 1.
Attending Exposure Groups
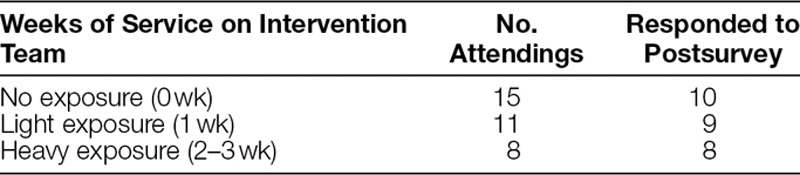
Table 2.
Attending Pre–Post Survey Findings
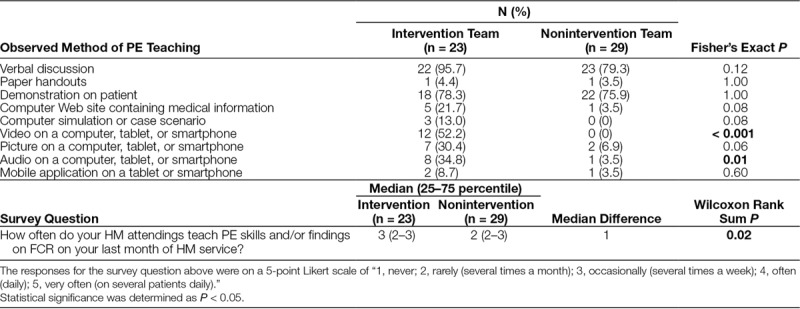
For residents, respondents on the intervention team had greater preference for teaching in the patient rooms (72.2% versus 35%; P = 0.03) before their HM rotation. Respondents in both groups had a strong desire for multimodal teaching and teaching with technology. At the end of their HM rotation, residents on the intervention team noted more PE teaching on FCR (P = 0.02), with a perceived PE teaching frequency of several times a week on the intervention team, compared with several times a month on the nonintervention team (Table 3). Residents on the intervention team also noted more use of video (P < 0.001) and audio clips from PEToolkit (P = 0.01) to teach on FCR, compared with residents on the nonintervention team.
Table 3.
Resident Postsurvey Findings
DISCUSSION
We successfully incorporated an innovative method of PE teaching in the clinical setting and increased the number of PEToolkit page counts from 2 to 5 counts per week over 7 months through interventions focused on in-person training, inclusion and training of additional resident users, and feedback with data transparency to attending and resident teachers. Additionally, our surveys revealed an increase in attending comfort with PE teaching on FCR in the heavy exposure group. We identified no change in comfort with technology pre- to postintervention period for any of the groups. Residents on the intervention team also noted an increase in PE teaching and use of video to teach on FCR, compared with residents on the nonintervention team; the increase in use of video signified the successful uptake of the educational intervention.
In reviewing the interventions that led to our success, engagement of the senior residents was valuable in achieving our goal. Many senior residents at our institution are part of the millennial generation, which may account for their ability to quickly integrate technology into their self-directed learning and transfer it into their teaching on FCR. Trainees who are born after 1982 are now the most populous generation and the emerging workforce in the medical field.21,22 Many institutions have developed resident-as-teacher curricula to develop their skills as educational leaders.23,24 Residents have significant face-time with their peers and medical students, thus educational efforts focused on residents becoming effective teachers are especially important.25 Senior residents on inpatient teams balance both supervision and instruction with the attendings. Parallel faculty and resident instruction in modern teaching methods allows the residents to role-model multimodal teaching techniques demonstrated by attendings.26 Ideally, the patient serves as a real-life example, while the Web site provides multimedia as a complement to demonstrate the spectrum of illness.18
Sustainability of QI work is important, and automated processes are the most reliable intervention.19 We noted a declining trend on our run chart when we attempted to remove the person-driven reminder to the attendings regarding site usage. This suggests that using a resource like the PEToolkit Web site to teach is not yet a natural method of teaching incorporated into our educators’ repertoire of techniques. Indeed, our attending survey indicates that, even in those with heavy exposure to the PEToolkit Web site, comfort with technology did not increase from pre- to poststudy. Over time, as more technology is available to our teachers and the millennial generation becomes the primary group of medical educators, use of Web sites to teach may be a more preferred method. Using a bundle that includes adequate training of attending physicians, access to equipment for ease of use, incorporating trainees in the teaching process, and frequent feedback on usage may allow for greater success in teaching with technology.
In considering modes of teaching, use of video was noted to increase with the help of the PEToolkit. Providing easily accessible visual aids engages the audience and can facilitate the concise summarization of teaching points.27 Videos can also portray complex concepts that may be difficult to explain in words.27 Furthermore, incorporation of images into the educational process increases learning retention, as learning that involves multiple modes, is more powerful, and long-lasting.28,29 Adults are self-directed active learners who value integration of learning into their workflow. In an era where resident duty hours are restricted and there may be less time for teaching, incorporating more efficient and effective methods are both useful and necessary.30
Limitations
There were several limitations to this study. First, the study was conducted at a single institution on the HM service; therefore, the results may not be generalizable. However, the interest of millennial learners in technology and multiple learning modalities are likely similar at other institutions. Second, in considering the application of QI methods to increase multimodal teaching, data collection and measurement were challenging. Page counts are an imperfect measure for quantifying multimodal teaching with technology on rounds. The site statistics were only able to quantify how often a page was reached but not the duration or specific media utilized. Attendings may prefer using hands-on patient demonstrations or other technology resources on the electronic tablet that were not captured. To account for the importance of inclusion of other valuable teaching topics in addition to PE education, we aimed to modestly increase the Web site usage to 5 page counts per week, which represented a realistic yet notable improvement. Third, attending variation had an impact on our study, given that a new attending physician came on service each week, making it difficult to carry over and capitalize on interventions from week to week. Fourth, it is challenging to base an intervention on a teaching habit that is not a required process. Teaching is one of several priorities to balance when on clinical service. Furthermore, attendings vary in their comfort, investment, and strategies for teaching, which may affect their motivation to incorporate a novel educational technique.
Finally, our survey sample sizes were small. The attending responses were subjective and may have been affected by social desirability bias of wanting to use newer forms of teaching. There was only a 51% response rate among the residents, which may affect generalizability. Although the surveys measured changes in perception, they did not assess changes in patient care or resident knowledge outcomes, which are the ultimate goals of medical education. Next steps of the project will include assessment of change in trainee knowledge and/or skills.
CONCLUSIONS
To engage millennial learners and enhance PE teaching on FCR, the study team developed the multimedia PE Web site PEToolkit (free of charge and publicly accessible at www.physicalexamtoolkit.com) and increased its use during FCR over a 7-month period. As millennial learners continue to evolve their methods of self-directed learning, hospitalists also seek to develop more extensive approaches in innovating teaching in the inpatient setting. Engagement of learners, frequent feedback, and educational coaching are all useful methods for incorporating technology in teaching and may be first steps in meeting the needs of modern learners.
ACKNOWLEDGMENTS
Assistance with the study: The study team would like to thank the HM attendings and fellows, chief residents, and pediatric residents for their participation in this study. The team would also like to thank the Hospital Medicine leadership for supporting the team’s Quality Improvement efforts through the Rapid Cycle Improvement Collaborative course at Cincinnati Children’s Hospital Medical Center.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Presented at Pediatric Academic Societies Meeting, May 2016, Baltimore, Md., and at Pediatric Hospital Medicine Annual Conference, July 2016, Chicago, Ill.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Sclafani J, Tirrell TF, Franko OI. Mobile tablet use among academic physicians and trainees. J Med Syst. 2013;37:9903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robin BR, McNeil SG, Cook DA, et al. Preparing for the changing role of instructional technologies in medical education. Acad Med. 2011;86:435–439.. [DOI] [PubMed] [Google Scholar]
- 3.Short SS, Lin AC, Merianos DJ, et al. Smartphones, trainees, and mobile education: implications for graduate medical education. J Grad Med Educ. 2014;6:199–202.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sousa DA. How the Brain Learns. 2011Thousand Oaks, CA: Corwin Press. [Google Scholar]
- 5.Turner DA, Narayan AP, Whicker SA, et al. Do pediatric residents prefer interactive learning? Educational challenges in the duty hours era. Med Teach. 2011;33:494–496.. [DOI] [PubMed] [Google Scholar]
- 6.Kharb P, Samanta PP, Jindal M, et al. The learning styles and the preferred teaching-learning strategies of first year medical students. J Clin Diagn Res. 2013;7:1089–1092.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim RH, Gilbert T, Ristig K, et al. Surgical resident learning styles: faculty and resident accuracy at identification of preferences and impact on ABSITE scores. J Surg Res. 2013;184:31–36.. [DOI] [PubMed] [Google Scholar]
- 8.Armstrong AD, Jarvis-Selinger S. I feel disconnected: learning technologies in resident education. Instr Course Lect. 2013;62:577–585.. [PubMed] [Google Scholar]
- 9.Mittal V. Family-centered rounds: a decade of growth. Hosp Pediatr. 2014;4:6–8.. [DOI] [PubMed] [Google Scholar]
- 10.Sandhu AK, Amin HJ, McLaughlin K, et al. Leading educationally effective family-centered bedside rounds. J Grad Med Educ. 2013;5:594–599.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mittal V, Krieger E, Lee BC, et al. Pediatrics residents’ perspectives on family-centered rounds: a qualitative study at 2 children’s hospitals. J Grad Med Educ. 2013;5:81–87.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muething SE, Kotagal UR, Schoettker PJ, et al. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119:829–832.. [DOI] [PubMed] [Google Scholar]
- 13.Wenrich MD, Jackson MB, Ajam KS, et al. Teachers as learners: the effect of bedside teaching on the clinical skills of clinician-teachers. Acad Med. 2011;86:846–852.. [DOI] [PubMed] [Google Scholar]
- 14.Williams KN, Ramani S, Fraser B, et al. Improving bedside teaching: findings from a focus group study of learners. Acad Med. 2008;83:257–264.. [DOI] [PubMed] [Google Scholar]
- 15.Crumlish CM, Yialamas MA, McMahon GT. Quantification of bedside teaching by an academic hospitalist group. J Hosp Med. 2009;4:304–307.. [DOI] [PubMed] [Google Scholar]
- 16.Janjigian MP, Charap M, Kalet A. Development of a hospitalist-led-and-directed physical examination curriculum. J Hosp Med. 2012;7:640–643.. [DOI] [PubMed] [Google Scholar]
- 17.Mookherjee S, Pheatt L, Ranji SR, et al. Physical examination education in graduate medical education—a systematic review of the literature. J Gen Intern Med. 2013;28:1090–1099.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel A, Unaka N, Sobolewski B, et al. Five steps for success in building your own educational Web site. Acad Pediatr. 2017;17:345–348.. [DOI] [PubMed] [Google Scholar]
- 19.Langley GJ, Moen R, Nolan KM, et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2009San Francisco, CA: John Wiley & Sons. [Google Scholar]
- 20.Provost LP, Murray S. The Health Care Data Guide: Learning from Data for Improvement. 2011Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- 21.Eckleberry-Hunt J, Tucciarone J. The challenges and opportunities of teaching “generation y”. J Grad Med Educ. 2011;3:458–461.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fry R. Millennials overtake Baby Boomers as America’s largest generation. 2016. Available at http://www.pewresearch.org/fact-tank/2016/04/25/millennials-overtake-baby-boomers/. Accessed May 6, 2016.
- 23.Morrison EH, Hafler JP. Yesterday a learner, today a teacher too: residents as teachers in 2000. Pediatrics. 2000;105(1 Pt 3):238–241.. [PubMed] [Google Scholar]
- 24.Bree KK, Whicker SA, Fromme HB, et al. Residents-as-teachers publications: what can programs learn from the literature when starting a new or refining an established curriculum? J Grad Med Educ. 2014;6:237–248.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karani R, Fromme HB, Cayea D, et al. How medical students learn from residents in the workplace: a qualitative study. Acad Med. 2014;89:490–496.. [DOI] [PubMed] [Google Scholar]
- 26.Balmer DF, Giardino AP, Richards BF. The dance between attending physicians and senior residents as teachers and supervisors. Pediatrics. 2012;129:910–915.. [DOI] [PubMed] [Google Scholar]
- 27.Hurtubise L, Martin B, Gilliland A, et al. To play or not to play: leveraging video in medical education. J Grad Med Educ. 2013;5:13–18.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Merriam SB, Caffarella RS, Baumgartner LM. Learning in Adulthood: A Comprehensive Guide. 2012Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- 29.Mahan JD, Stein DS. Teaching adults-best practices that leverage the emerging understanding of the neurobiology of learning. Curr Probl Pediatr Adolesc Health Care. 2014;44:141–149.. [DOI] [PubMed] [Google Scholar]
- 30.Stanski N, Patel A. Improving trainee education during family-centered rounds: a resident’s perspective. Pediatrics. 2016;137:e20153679. [DOI] [PubMed] [Google Scholar]


