Abstract
Purpose of Review
Stroke is the most feared complication of atrial fibrillation. To prevent stroke, left atrial appendage exclusion has been targeted, as it is the prevalent site for formation of heart thrombi during atrial fibrillation.
We review the historic development of methods for exclusion of the left atrial appendage and the evidence to support its amputation during routine cardiac surgery.
Recent Findings
Evidence is not yet sufficient to routinely recommend left atrial exclusion during heart surgery, despite a high prevalence of postoperative atrial fibrillation. Observational studies indicate that electrical isolation of scarring from clip or suture techniques reduces the arrhythmogenic substrate.
Summary
Randomized studies comparing different methods of closure of the left atrial appendage before amputation do not exist. Such studies are therefore warranted, as well as studies that can elucidate whether amputation is superior to leaving the left atrial appendage stump. Potentially, thrombogenic remaining pouch after closure should be addressed.
Keywords: Left atrial appendage, Cardiac surgery, Atrial fibrillation, Thromboembolism, Stroke
Introduction
Does left atrial appendage (LAA) amputation during routine cardiac surgery reduce the risk of stroke and future atrial fibrillation? This question has been posed for more than 150 years [1, 2], since the LAA is recognized as the prevalent site for formation of thrombi during atrial fibrillation (AF) [3–5], with stroke being its most common and potentially devastating thromboembolic complication.
Atrial Fibrillation and Its Relation to Open-heart Surgery
Occurrence of AF following cardiac surgery is common, with a prevalence of 10 to 65% [6–8], and is associated with prolonged hospitalization and higher risk of mortality [7–10].
Paroxysmal AF after cardiac surgery is often self-limiting [11], and up to 40% of patients with AF are asymptomatic during the arrhythmia [12]. Hence, many patients with unrecognized recurrent AF, who do not receive anti-coagulation after surgery, remain at risk for stroke [13]. This is a growing problem since more elderly patients undergo cardiac surgery [14]. Although the risk of complications during surgery is improving, patients continue to have a high risk of stroke if they have AF [15, 16]. Therefore, multiple approaches are targeted to relieve this burden. That is, to prevent the occurrence of AF [17, 18] and its recurrence after surgery [19–21], and, to reduce the thrombogenic substrate, the left atrial appendage (LAA) is excluded [22–24]. Oral anti-coagulation (OAC) is an efficient method for thromboembolism risk reduction [25]. However, the adequate length of OAC after post-operative AF is still unknown [18, 26]. Importantly, between 30 and 50% of patients are not eligible for OAC due to high risk of bleeding or other contraindications [25, 27]. Furthermore, it is estimated that 16–50% of patients in OAC therapy are not sufficiently anti-coagulated [28–30]. In these patients a highly reliable LAA occlusion would be an attractive alternative as it potentially reduces stroke risk by 50% [31].
The Left Atrial Appendage and Thrombus Formation
The LAA is a hook-like diverticulum of the left atrium (LA) consisting of one or more lobes with a trabeculated wall due to parallel-running pectinate muscles [32, 33]. In sinus rhythm, the LAA is highly contractile (contracts from its apex toward the base) and the blood flow within the lumen is sufficient to avoid thrombus formation. Contrarily, during AF, the contractility of the LAA is limited and the blood flow within the lumen is reduced creating a hemodynamic ‘dead-space’ [34, 35]. Furthermore, the highly trabeculated wall of the LAA plays an important role in its high thrombogenicity, and increased thrombus formation occurs with smaller LAA orifice and higher number of lobes [36, 37]. Therefore, the LAA is considered the primary source of cardio-embolic stroke in patients with non-valvular AF [25, 38], although thrombi can develop outside the LAA [3]. Accordingly, transesophageal echocardiography (TEE) is the key examination for diagnosing thrombus formation in the LAA [35, 37, 39], and direct current conversion to sinus rhythm has proved to be safe in the absence of thrombi in the LAA during TEE [33, 34, 40–42].
Historic Perspective on Amputation of the Left Atrial Appendage During Surgery
The first amputations of the LAA in humans [43] were reported almost simultaneously with the results of the procedure in animal experiments [44–46]. After these successful pioneering attempts, they were subsequently performed in addition to mitral commissurotomy, to alleviate the well-known high thrombogenicity in mitral stenosis [38, 47, 48]. Systematic exclusion of the LAA is currently recommended in addition to surgical ablation procedures [21].
Thoracoscopic amputations of the LAA were initially performed by Johnson et al. as a stand-alone procedure in patients with high risk for thromboembolisms, who do not tolerate OAC [25]. Since then, there have been developed minimally invasive approaches to amputate the LAA [19, 49–53]. Nevertheless, the development of safe and effective clip devices for obliteration of the LAA thoracoscopically [54] and intra-operatively [55••, 56], is emerging as a preferred method compared to LAA amputation [57, 58].
Less Arrhythmogenic Substrate After LAA Exclusion
Persistent AF can originate from the LAA [59] and it has been demonstrated that targeting ablation of the LAA can reduce AF [21, 60]. Therefore, exclusion of the LAA can possibly provide an anti-arrhythmogenic effect, in addition to protection against thromboembolisms. Accordingly, a reduction of atrial dispersion has been demonstrated with LAA ligation in patients with AF [61]. Additionally, clip occlusion [62] and epicardial ligation [63] have shown to provide electric appendage isolation. In a recent study, patients randomized to closure or not closure of the LAA during cardiac surgery, closure by epicardial suture seemed to reduce AF during follow-up (Park-Hansen in press). It is conceivable that amputation of the LAA can have a similar anti-arrhythmogenic effect, but such an effect remains to be studied.
Hemodynamic Consequences of LAA Amputation
Natriuretic hormones can be secreted from all myocytes but, in normal healthy conditions they are primarily produced in the LAA [64–67]. Levels of natriuretic hormones are elevated in permanent AF [68] and, specially, levels of B-type natriuretic peptide reveal paroxysms after ablation [69–73].
The first successful LAA amputations on healthy dogs in the 1940s [1] were followed by concerns on possible impairment of mechanisms to compensate fluid overload, due to the loss of atrium natriuretic peptides and a reduced stroke volume of the left atrium [44–46]. Despite these concerns, experimental observations in animals do not seem to have clinical importance in humans [74].
Recently, it has been raised concern by the observation that, along with a decrease on the left atrium volume that follows successful AF ablation, there is an increase in the LAA volume, assessed with magnetic resonance scanning [75]. This is a matter of concern, since larger LAA volume increases the risk of stroke in patients with comparable thromboembolic risk profile [76, 77].
In a recent study, no hemodynamic changes have been observed immediately after percutaneous LAA closure [78]. Nevertheless, it seems to be important whether the LAA is closed from the endocardial or from the epicardial site, since comparing the two approaches, only the epicardial closure proved beneficial hemodynamic changes [79].
According to these observations, an epicardial closure, with or without subsequent amputation, should be the preferred approach.
Thrombogenicity After Amputation of the LAA
The thrombogenicity of the LAA during AF is, in part, attributable to loss of contractility of the LAA. In a retrospective study of patients who underwent occlusion of the LAA, those with preserved LAA had a better contractility estimated with echocardiography, compared with a group where the LAA was amputated; however, this difference did not preclude differences on stroke nor occurrence of AF [80].
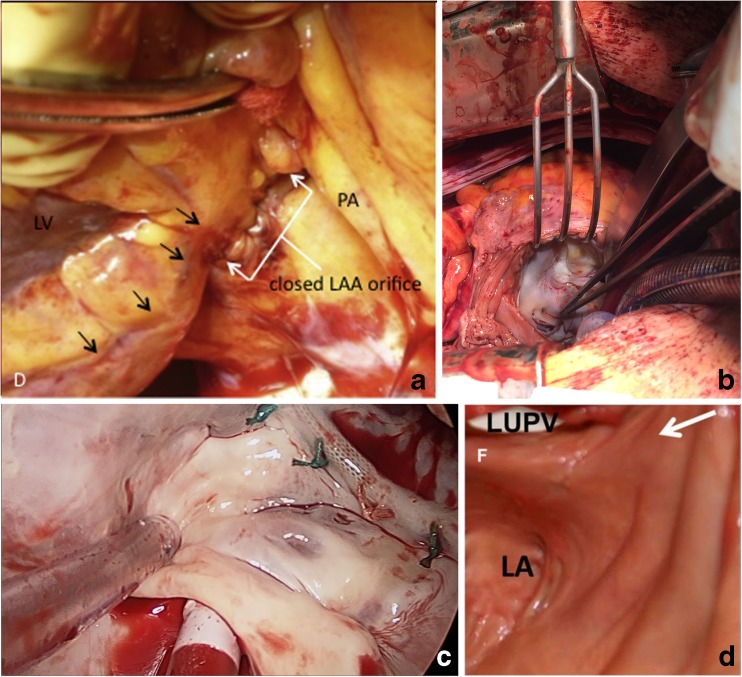
Regardless of the LAA exclusion method, the potential thrombogenicity of the remaining appendage pouch is a matter of major concern [31, 81••, 82]. In a previous non-randomized study that compared efficacy of several methods of LAA closure, TEE reveled a remnant LAA in 26% of patients. Importantly, 12% of these patients had suffered strokes in the lapse from the operation to the time when TEE was performed, despite none having clots in the remnant LAA [83]. In early studies on excision of the LAA after stapling, additional sutures were necessary to repair tears [84, 85], and similar complications with tears needing repair have also been reported more recently in the LAAOS-II trial [86]. Furthermore, intuitively, an irregular endocardial surface after suture (Fig. 1a) may be more thrombogenic than a smoother surface observable after epicardial stapling (Fig. 1b) and after epicardial clips (Fig. 1c) or snaring (Fig. 1d). Assuming the size of the remaining pouch is important for its thrombogenicity, perioperative TEE could serve for assessing its size, and perioperatively, limit the size of the pouch for example to less than 1 cm, by performing an additional suture or stapler line, or placing an additional clip when needed.
Fig. 1.
View of the endocardial surface of the left atrium, after LAA exclusion with: suture marked with white arrows, the black arrows show the circumflex coronary artery a, epicardial stapling (b), clips (c), or epicardial snoring, with a black arrow showing the endocardial surface (d). LAA left atrium appendage. (Figure 1a is reproduced from Aoyagi S. et al. Heart, Lung and Circulation, 2017.26:413–15, with permission from Elsevier; [87].) (Figure 1c is kindly provided by AtriCure Inc.) (Figure 1d is reproduced from Bartus K et al. Circ Arrhythm Electrophysiol. 2014;7:764–767, with permission; [88])
Conclusion
Several studies support a beneficial effect of LAA closure during surgery, but evidence is not yet sufficient to support closure of the LAA systematically in addition to heart surgery, to protect against thromboembolisms related to AF. Hence, there is a need for randomized studies to provide the evidence of stroke protection and, furthermore, comparing different methods for closure of the LAA in terms of arrhythmogenic impact. Such studies should address how to manage the potential thromboembolic problem of a remaining pouch after LAA closure, to elucidate what is the optimal management of the LAA during surgery.
Abbreviations
- AF
Atrial fibrillation
- LA
Left atrium
- LAA
Left atrial appendage
- OAC
Oral anti-coagulants
- TEE
Trans-esophageal echocardiography
Conflict of Interest
Helena Domínguez, Christoffer Valdorff Madsen, Oliver Nøhr Hjorth Westh, Peter Appel Pallesen, Christian Lildal Carrranza, Akhmadjon Irmukhamedov, and Jesper Park-Hansen declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Invasive Electrophysiology and Pacing
Contributor Information
Helena Domínguez, Phone: +45 38166068, Email: mdom0002@regionh.dk.
Christoffer Valdorff Madsen, Email: Christoffer.valdorff.madsen@regionh.dk.
Oliver Nøhr Hjorth Westh, Email: hts772@alumni.ku.dk.
Peter Appel Pallesen, Email: peter.pallesen@rsyd.dk.
Christian Lildal Carrranza, Email: christian.lildal.carranza@regionh.dk.
Akhmadjon Irmukhamedov, Email: akhmadjon.irmukhamedov@rsyd.dk.
Jesper Park-Hansen, Email: Jesper.park.hansen@regionh.dk.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major Importance
- 1.Hellerstein HK, Sinaiko E, Dolgin M. Amputation of the canine atrial appendages. Proc Soc Exp Biol Med. 1947;66(2):337. doi: 10.3181/00379727-66-16084P. [DOI] [PubMed] [Google Scholar]
- 2.Castella M. The new 2016 European Society of Cardiology/European Association for Cardio-Thoracic Surgery Guidelines: enough guidance? enough evidence? Eur J Cardiothorac Surg. 2018;53(suppl_1):i9–i13. doi: 10.1093/ejcts/ezx495. [DOI] [PubMed] [Google Scholar]
- 3.Mahajan R, Brooks AG, Sullivan T, Lim HS, Alasady M, Abed HS, Ganesan AN, Nayyar S, Lau DH, Roberts-Thomson KC, Kalman JM, Sanders P. Importance of the underlying substrate in determining thrombus location in atrial fibrillation: implications for left atrial appendage closure. Heart. 2012;98(15):1120–1126. doi: 10.1136/heartjnl-2012-301799. [DOI] [PubMed] [Google Scholar]
- 4.Aberg H. Atrial fibrillation. II. A study of fibrillatory wave size on the regular scalar electrocardiogram. Acta Med Scand. 1969;185(5):381–5. [PubMed] [Google Scholar]
- 5.Tsai LM, Lin LJ, Teng JK, Chen JH. Prevalence and clinical significance of left atrial thrombus in nonrheumatic atrial fibrillation. Int J Cardiol. 1997;58(2):163–169. doi: 10.1016/S0167-5273(96)02862-8. [DOI] [PubMed] [Google Scholar]
- 6.Rho RW. The management of atrial fibrillation after cardiac surgery. Heart. 2009;95(5):422–429. doi: 10.1136/hrt.2007.132795. [DOI] [PubMed] [Google Scholar]
- 7.Mathew JP, Fontes ML, Tudor IC, Ramsay J, Duke P, Mazer CD, Barash PG, Hsu PH, Mangano DT, Investigators of the Ischemia Research and Education Foundation. Multicenter Study of Perioperative Ischemia Research Group A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291(14):1720–1729. doi: 10.1001/jama.291.14.1720. [DOI] [PubMed] [Google Scholar]
- 8.Maesen B, Nijs J, Maessen J, Allessie M, Schotten U. Post-operative atrial fibrillation: a maze of mechanisms. Europace. 2012;14(2):159–174. doi: 10.1093/europace/eur208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahlsson A, Fengsrud E, Bodin L, Englund A. Postoperative atrial fibrillation in patients undergoing aortocoronary bypass surgery carries an eightfold risk of future atrial fibrillation and a doubled cardiovascular mortality. Eur J Cardiothorac Surg. 2010;37(6):1353–1359. doi: 10.1016/j.ejcts.2009.12.033. [DOI] [PubMed] [Google Scholar]
- 10.Saxena A, Dinh D, Dimitriou J, Reid C, Smith J, Shardey G, Newcomb A. Preoperative atrial fibrillation is an independent risk factor for mid-term mortality after concomitant aortic valve replacement and coronary artery bypass graft surgery. Interact Cardiovasc Thorac Surg. 2013;16(4):488–494. doi: 10.1093/icvts/ivs538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kowey PR, et al. Clinical outcome of patients who develop PAF after CABG surgery. Pacing Clin Electrophysiol. 2001;24(2):191–193. doi: 10.1046/j.1460-9592.2001.00191.x. [DOI] [PubMed] [Google Scholar]
- 12.Healey JS, Connolly SJ, Gold MR, Israel CW, van Gelder I, Capucci A, Lau CP, Fain E, Yang S, Bailleul C, Morillo CA, Carlson M, Themeles E, Kaufman ES, Hohnloser SH, ASSERT Investigators Subclinical atrial fibrillation and the risk of stroke. N Engl J Med. 2012;366(2):120–129. doi: 10.1056/NEJMoa1105575. [DOI] [PubMed] [Google Scholar]
- 13.Almahameed ST, et al. Left atrial appendage exclusion and the risk of thromboembolic events following mitral valve surgery. J Cardiovasc Electrophysiol. 2007;18(4):364–366. doi: 10.1111/j.1540-8167.2006.00755.x. [DOI] [PubMed] [Google Scholar]
- 14.Tarakji KG, Sabik JF, 3rd, Bhudia SK, Batizy LH, Blackstone EH. Temporal onset, risk factors, and outcomes associated with stroke after coronary artery bypass grafting. JAMA. 2011;305(4):381–390. doi: 10.1001/jama.2011.37. [DOI] [PubMed] [Google Scholar]
- 15.Zoni-Berisso M, Lercari F, Carazza T, Domenicucci S. Epidemiology of atrial fibrillation: European perspective. Clin Epidemiol. 2014;6:213–220. doi: 10.2147/CLEP.S47385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, McAnulty JH, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA, Ezzati M, Murray CJL. Worldwide epidemiology of atrial fibrillation: a global burden of disease 2010 study. Circulation. 2014;129(8):837–847. doi: 10.1161/CIRCULATIONAHA.113.005119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burgess DC, Kilborn MJ, Keech AC. Interventions for prevention of post-operative atrial fibrillation and its complications after cardiac surgery: a meta-analysis. Eur Heart J. 2006;27(23):2846–2857. doi: 10.1093/eurheartj/ehl272. [DOI] [PubMed] [Google Scholar]
- 18.Frendl G, Sodickson AC, Chung MK, Waldo AL, Gersh BJ, Tisdale JE, Calkins H, Aranki S, Kaneko T, Cassivi S, Smith SC Jr, Darbar D, Wee JO, Waddell TK, Amar D, Adler D, American Association for Thoracic Surgery 2014 AATS guidelines for the prevention and management of perioperative atrial fibrillation and flutter for thoracic surgical procedures. J Thorac Cardiovasc Surg. 2014;148(3):e153–e193. doi: 10.1016/j.jtcvs.2014.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gillinov AM. Advances in surgical treatment of atrial fibrillation. Stroke. 2007;38(2 Suppl):618–623. doi: 10.1161/01.STR.0000247934.04848.79. [DOI] [PubMed] [Google Scholar]
- 20.Saltman AE, Gillinov AM. Surgical approaches for atrial fibrillation. Cardiol Clin. 2009;27(1):179–188. doi: 10.1016/j.ccl.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 21.Badhwar V, Rankin JS, Damiano RJ, Jr, Gillinov AM, Bakaeen FG, Edgerton JR, Philpott JM, McCarthy PM, Bolling SF, Roberts HG, Thourani VH, Suri RM, Shemin RJ, Firestone S, Ad N. The Society of Thoracic Surgeons 2017 clinical practice guidelines for the surgical treatment of atrial fibrillation. Ann Thorac Surg. 2017;103(1):329–341. doi: 10.1016/j.athoracsur.2016.10.076. [DOI] [PubMed] [Google Scholar]
- 22.Onalan O, Crystal E. Left atrial appendage exclusion for stroke prevention in patients with nonrheumatic atrial fibrillation. Stroke. 2007;38(2 Suppl):624–630. doi: 10.1161/01.STR.0000250166.06949.95. [DOI] [PubMed] [Google Scholar]
- 23.Caliskan, E., et al. Epicardial left atrial appendage AtriClip occlusion reduces the incidence of stroke in patients with atrial fibrillation undergoing cardiac surgery. Europace. 2017. [DOI] [PubMed]
- 24.Melduni RM, Schaff HV, Lee HC, Gersh BJ, Noseworthy PA, Bailey KR, Ammash NM, Cha SS, Fatema K, Wysokinski WE, Seward JB, Packer DL, Rihal CS, Asirvatham SJ. Impact of left atrial appendage closure during cardiac surgery on the occurrence of early postoperative atrial fibrillation, stroke, and mortality: a propensity score-matched analysis of 10 633 patients. Circulation. 2017;135(4):366–378. doi: 10.1161/CIRCULATIONAHA.116.021952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson WD, Ganjoo AK, Stone CD, Srivyas RC, Howard M. The left atrial appendage: our most lethal human attachment! Surgical implications. Eur J Cardiothorac Surg. 2000;17(6):718–722. doi: 10.1016/S1010-7940(00)00419-X. [DOI] [PubMed] [Google Scholar]
- 26.Kirchhof P, et al. 2016 ESC Guidelines for the Management of Atrial Fibrillation Developed in Collaboration With EACTS. Rev Esp Cardiol (Engl Ed) 2017;70(1):50. doi: 10.1016/j.rec.2016.11.033. [DOI] [PubMed] [Google Scholar]
- 27.Kirchhof P, Ammentorp B, Darius H, de Caterina R, le Heuzey JY, Schilling RJ, Schmitt J, Zamorano JL. Management of atrial fibrillation in seven European countries after the publication of the 2010 ESC guidelines on atrial fibrillation: primary results of the PREvention oF thromboemolic events--European registry in atrial fibrillation (PREFER in AF) Europace. 2014;16(1):6–14. doi: 10.1093/europace/eut263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Waldo AL, Becker RC, Tapson VF, Colgan KJ, NABOR Steering Committee Hospitalized patients with atrial fibrillation and a high risk of stroke are not being provided with adequate anticoagulation. J Am Coll Cardiol. 2005;46(9):1729–1736. doi: 10.1016/j.jacc.2005.06.077. [DOI] [PubMed] [Google Scholar]
- 29.Ogilvie IM, Newton N, Welner SA, Cowell W, Lip GYH. Underuse of oral anticoagulants in atrial fibrillation: a systematic review. Am J Med. 2010;123(7):638–645 e4. doi: 10.1016/j.amjmed.2009.11.025. [DOI] [PubMed] [Google Scholar]
- 30.Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–314. doi: 10.4065/mcp.2010.0575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chatterjee S, Alexander JC, Pearson PJ, Feldman T. Left atrial appendage occlusion: lessons learned from surgical and transcatheter experiences. Ann Thorac Surg. 2011;92(6):2283–2292. doi: 10.1016/j.athoracsur.2011.08.044. [DOI] [PubMed] [Google Scholar]
- 32.Kerut EK. Anatomy of the left atrial appendage. Echocardiography. 2008;25(6):669–673. doi: 10.1111/j.1540-8175.2008.00637.x. [DOI] [PubMed] [Google Scholar]
- 33.Barbero U, Ho SY. Anatomy of the atria: a road map to the left atrial appendage. Herzschrittmacherther Elektrophysiol. 2017;28(4):347–354. doi: 10.1007/s00399-017-0535-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pollick C, Taylor D. Assessment of left atrial appendage function by transesophageal echocardiography. Implications for the development of thrombus. Circulation. 1991;84(1):223–231. doi: 10.1161/01.CIR.84.1.223. [DOI] [PubMed] [Google Scholar]
- 35.Beigel R, Wunderlich NC, Ho SY, Arsanjani R, Siegel RJ. The left atrial appendage: anatomy, function, and noninvasive evaluation. J Am Coll Cardiol Img. 2014;7(12):1251–1265. doi: 10.1016/j.jcmg.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 36.Di Biase L, et al. Does the left atrial appendage morphology correlate with the risk of stroke in patients with atrial fibrillation? Results from a multicenter study. J Am Coll Cardiol. 2012;60(6):531–538. doi: 10.1016/j.jacc.2012.04.032. [DOI] [PubMed] [Google Scholar]
- 37.Khurram IM, Dewire J, Mager M, Maqbool F, Zimmerman SL, Zipunnikov V, Beinart R, E. Marine J, Spragg DD, Berger RD, Ashikaga H, Nazarian S, Calkins H. Relationship between left atrial appendage morphology and stroke in patients with atrial fibrillation. Heart Rhythm. 2013;10(12):1843–1849. doi: 10.1016/j.hrthm.2013.09.065. [DOI] [PubMed] [Google Scholar]
- 38.Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996;61(2):755–759. doi: 10.1016/0003-4975(95)00887-X. [DOI] [PubMed] [Google Scholar]
- 39.Malik SB, Kwan D, Shah AB, Hsu JY. The right atrium: gateway to the heart--anatomic and pathologic imaging findings. Radiographics. 2015;35(1):14–31. doi: 10.1148/rg.351130010. [DOI] [PubMed] [Google Scholar]
- 40.Grimm RA, Stewart WJ, Black IW, Thomas JD, Klein AL. Should all patients undergo transesophageal echocardiography before electrical cardioversion of atrial fibrillation? J Am Coll Cardiol. 1994;23(2):533–541. doi: 10.1016/0735-1097(94)90443-X. [DOI] [PubMed] [Google Scholar]
- 41.Shen X, Li H, Rovang K, Hee T, Holmberg MJ, Mooss AN, Mohiuddin SM. Transesophageal echocardiography before cardioversion of recurrent atrial fibrillation: does absence of previous atrial thrombi preclude the need of a repeat test? Am Heart J. 2003;146(4):741–745. doi: 10.1016/S0002-8703(03)00390-9. [DOI] [PubMed] [Google Scholar]
- 42.Smith SA, Binkley PF, Foraker RE, Nagaraja HN, Orsinelli DA. The role of repeat transesophageal echocardiography in patients without atrial thrombus prior to cardioversion or ablation. J Am Soc Echocardiogr. 2012;25(10):1106–1112. doi: 10.1016/j.echo.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Madden JL. Resection of the left auricular appendix; a prophylaxis for recurrent arterial emboli. J Am Med Assoc. 1949;140(9):769–772. doi: 10.1001/jama.1949.02900440011003. [DOI] [PubMed] [Google Scholar]
- 44.Stewart JM, Dean R, Brown M, Diasparra D, Zeballos GA, Schustek M, Gewitz MH, Thompson CI, Hintze TH. Bilateral atrial appendectomy abolishes increased plasma atrial natriuretic peptide release and blunts sodium and water excretion during volume loading in conscious dogs. Circ Res. 1992;70(4):724–732. doi: 10.1161/01.RES.70.4.724. [DOI] [PubMed] [Google Scholar]
- 45.Benjamin BA, Metzler CH, Peterson TV. Chronic atrial appendectomy alters sodium excretion in conscious monkeys. Am J Phys. 1988;254(4 Pt 2):R699–R705. doi: 10.1152/ajpregu.1988.254.4.R699. [DOI] [PubMed] [Google Scholar]
- 46.Massoudy P, Beblo S, Raschke P, Zahler S, Becker BF. Influence of intact left atrial appendage on hemodynamic parameters of isolated Guinea pig heart. Eur J Med Res. 1998;3(10):470–474. [PubMed] [Google Scholar]
- 47.Bailey CP, et al. Commissurotomy for mitral stenosis; technique for prevention of cerebral complications. J Am Med Assoc. 1952;149(12):1085–1091. doi: 10.1001/jama.1952.02930290007002. [DOI] [PubMed] [Google Scholar]
- 48.Belcher JR, Somerville W. Systemic embolism and left auricular thrombosis in relation to mitral valvotomy. Br Med J. 1955;2(4946):1000–1003. doi: 10.1136/bmj.2.4946.1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Matsutani N, Takase B, Ozeki Y, Maehara T, Lee R. Minimally invasive cardiothoracic surgery for atrial fibrillation: a combined Japan-US experience. Circ J. 2008;72(3):434–436. doi: 10.1253/circj.72.434. [DOI] [PubMed] [Google Scholar]
- 50.Syed TM, Halperin JL. Left atrial appendage closure for stroke prevention in atrial fibrillation: state of the art and current challenges. Nat Clin Pract Cardiovasc Med. 2007;4(8):428–435. doi: 10.1038/ncpcardio0933. [DOI] [PubMed] [Google Scholar]
- 51.Yilmaz A, Geuzebroek GSC, van Putte BP, Boersma LVA, Sonker U, de Bakker JMT, van Boven WJ. Completely thoracoscopic pulmonary vein isolation with ganglionic plexus ablation and left atrial appendage amputation for treatment of atrial fibrillation. Eur J Cardiothorac Surg. 2010;38(3):356–360. doi: 10.1016/j.ejcts.2010.01.058. [DOI] [PubMed] [Google Scholar]
- 52.Yilmaz A, Van Putte BP, Van Boven WJ. Completely thoracoscopic bilateral pulmonary vein isolation and left atrial appendage exclusion for atrial fibrillation. J Thorac Cardiovasc Surg. 2008;136(2):521–2. doi: 10.1016/j.jtcvs.2008.01.035. [DOI] [PubMed] [Google Scholar]
- 53.Inoue T, Suematsu Y. Left atrial appendage resection can be performed minimally invasively with good clinical and echocardiographic outcomes without any severe risk. Eur J Cardiothorac Surg. 2018;54:78–83. doi: 10.1093/ejcts/ezx506. [DOI] [PubMed] [Google Scholar]
- 54.Suwalski P, Witkowska A. Totally thoracoscopic left atrial occlusion concomitant to endoscopic atraumatic coronary artery bypass grafting (EACAB). Multimed Man Cardiothorac Surg. 2018;2018. [DOI] [PubMed]
- 55.Lee R, et al. A randomized, prospective pilot comparison of 3 atrial appendage elimination techniques: Internal ligation, stapled excision, and surgical excision. J Thorac Cardiovasc Surg. 2016;152(4):1075–1080. doi: 10.1016/j.jtcvs.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 56.Ailawadi G, et al. Exclusion of the left atrial appendage with a novel device: early results of a multicenter trial. J Thorac Cardiovasc Surg. 2011;142(5):1002–1009. doi: 10.1016/j.jtcvs.2011.07.052. [DOI] [PubMed] [Google Scholar]
- 57.Emmert MY, Puippe G, Baumüller S, Alkadhi H, Landmesser U, Plass A, Bettex D, Scherman J, Grünenfelder J, Genoni M, Falk V, Salzberg SP. Safe, effective and durable epicardial left atrial appendage clip occlusion in patients with atrial fibrillation undergoing cardiac surgery: first long-term results from a prospective device trial. Eur J Cardiothorac Surg. 2014;45(1):126–131. doi: 10.1093/ejcts/ezt204. [DOI] [PubMed] [Google Scholar]
- 58.Khan HR, Kralj-Hans I, Haldar S, Bahrami T, Clague J, de Souza A, Francis D, Hussain W, Jarman J, Jones DG, Mediratta N, Mohiaddin R, Salukhe T, Jones S, Lord J, Murphy C, Kelly J, Markides V, Gupta D, Wong T. Catheter ablation versus thoracoscopic surgical ablation in long standing persistent atrial fibrillation (CASA-AF): study protocol for a randomised controlled trial. Trials. 2018;19(1):117. doi: 10.1186/s13063-018-2487-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Di Biase L, Santangeli P, Natale A. How to ablate long-standing persistent atrial fibrillation? Curr Opin Cardiol. 2013;28(1):26–35. doi: 10.1097/HCO.0b013e32835b59bb. [DOI] [PubMed] [Google Scholar]
- 60.Di Biase L, et al. Left atrial appendage isolation in patients with longstanding persistent AF undergoing catheter ablation: BELIEF trial. J Am Coll Cardiol. 2016;68(18):1929–1940. doi: 10.1016/j.jacc.2016.07.770. [DOI] [PubMed] [Google Scholar]
- 61.Kawamura M, Scheinman MM, Lee RJ, Badhwar N. Left atrial appendage ligation in patients with atrial fibrillation leads to a decrease in atrial dispersion. J Am Heart Assoc. 2015;4(5). [DOI] [PMC free article] [PubMed]
- 62.Starck CT, Steffel J, Emmert MY, Plass A, Mahapatra S, Falk V, Salzberg SP. Epicardial left atrial appendage clip occlusion also provides the electrical isolation of the left atrial appendage. Interact Cardiovasc Thorac Surg. 2012;15(3):416–418. doi: 10.1093/icvts/ivs136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Afzal MR, Kanmanthareddy A, Earnest M, Reddy M, Atkins D, Bommana S, Bartus K, Rasekh A, Han F, Badhwar N, Cheng J, Dibiase L, Ellis CR, Dawn B, Natale A, Lee RJ, Lakkireddy D. Impact of left atrial appendage exclusion using an epicardial ligation system (LARIAT) on atrial fibrillation burden in patients with cardiac implantable electronic devices. Heart Rhythm. 2015;12(1):52–59. doi: 10.1016/j.hrthm.2014.09.053. [DOI] [PubMed] [Google Scholar]
- 64.Tabata T, Oki T, Yamada H, Abe M, Onose Y, Thomas JD. Relationship between left atrial appendage function and plasma concentration of atrial natriuretic peptide. Eur J Echocardiogr. 2000;1(2):130–137. doi: 10.1053/euje.2000.0019. [DOI] [PubMed] [Google Scholar]
- 65.Goetze JP, Friis-Hansen L, Rehfeld JF, Nilsson B, Svendsen JH. Atrial secretion of B-type natriuretic peptide. Eur Heart J. 2006;27(14):1648–1650. doi: 10.1093/eurheartj/ehl109. [DOI] [PubMed] [Google Scholar]
- 66.Hamid Q, Wharton J, Terenghi G, Hassall CJ, Aimi J, Taylor KM, Nakazato H, Dixon JE, Burnstock G, Polak JM. Localization of atrial natriuretic peptide mRNA and immunoreactivity in the rat heart and human atrial appendage. Proc Natl Acad Sci U S A. 1987;84(19):6760–6764. doi: 10.1073/pnas.84.19.6760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Leinonen JV, Emanuelov AK, Platt Y, Helman Y, Feinberg Y, Lotan C, Beeri R. Left atrial appendages from adult hearts contain a reservoir of diverse cardiac progenitor cells. PLoS One. 2013;8(3):e59228. doi: 10.1371/journal.pone.0059228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rossi A, Enriquez-Sarano M, Burnett JC, Jr, Lerman A, Abel MD, Seward JB. Natriuretic peptide levels in atrial fibrillation: a prospective hormonal and Doppler-echocardiographic study. J Am Coll Cardiol. 2000;35(5):1256–1262. doi: 10.1016/S0735-1097(00)00515-5. [DOI] [PubMed] [Google Scholar]
- 69.Hussein AA, Saliba WI, Martin DO, Shadman M, Kanj M, Bhargava M, Dresing T, Chung M, Callahan T, Baranowski B, Tchou P, Lindsay BD, Natale A, Wazni OM. Plasma B-type natriuretic peptide levels and recurrent arrhythmia after successful ablation of lone atrial fibrillation. Circulation. 2011;123(19):2077–2082. doi: 10.1161/CIRCULATIONAHA.110.007252. [DOI] [PubMed] [Google Scholar]
- 70.Giannopoulos G, Kossyvakis C, Angelidis C, Efremidis M, Panagopoulou V, Letsas K, Bouras G, Vassilikos VP, Goudevenos J, Tousoulis D, Lekakis J, Deftereos S. Amino-terminal B-natriuretic peptide levels and postablation recurrence in hypertensive patients with paroxysmal atrial fibrillation. Heart Rhythm. 2015;12(7):1470–1475. doi: 10.1016/j.hrthm.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 71.Degener S, Pattberg SV, Feuersenger H, Bansmann PM, Shin DI, Krummenauer F, Horlitz M. Predictive value of B-type natriuretic peptide levels in patients with paroxysmal and persistent atrial fibrillation undergoing pulmonary vein isolation. J Interv Card Electrophysiol. 2011;30(3):217–225. doi: 10.1007/s10840-010-9540-2. [DOI] [PubMed] [Google Scholar]
- 72.Yamada T, Murakami Y, Okada T, Okamoto M, Shimizu T, Toyama J, Yoshida Y, Tsuboi N, Ito T, Muto M, Kondo T, Inden Y, Hirai M, Murohara T. Plasma atrial natriuretic peptide and brain natriuretic peptide levels after radiofrequency catheter ablation of atrial fibrillation. Am J Cardiol. 2006;97(12):1741–1744. doi: 10.1016/j.amjcard.2005.12.071. [DOI] [PubMed] [Google Scholar]
- 73.Ma XX, Zhang YL, Hu B, Jiang WJ, Wang M, Zheng DY, Zhu MR, Xue XP. Association between left atrial appendage emptying velocity, N-terminal plasma brain natriuretic peptide levels, and recurrence of atrial fibrillation after catheter ablation. J Interv Card Electrophysiol. 2017;48(3):343–350. doi: 10.1007/s10840-016-0216-4. [DOI] [PubMed] [Google Scholar]
- 74.Al-Saady NM, Obel OA, Camm AJ. Left atrial appendage: structure, function, and role in thromboembolism. Heart. 1999;82(5):547–554. doi: 10.1136/hrt.82.5.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kim YG, Shim J, Oh SK, Park HS, Lee KN, Hwang SH, Choi JI, Kim YH. Different responses of left atrium and left atrial appendage to radiofrequency catheter ablation of atrial fibrillation: a follow up MRI study. Sci Rep. 2018;8(1):7871. doi: 10.1038/s41598-018-26212-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lee JM, Kim JB, Uhm JS, Pak HN, Lee MH, Joung B. Additional value of left atrial appendage geometry and hemodynamics when considering anticoagulation strategy in patients with atrial fibrillation with low CHA2DS2-VASc scores. Heart Rhythm. 2017;14(9):1297–1301. doi: 10.1016/j.hrthm.2017.05.034. [DOI] [PubMed] [Google Scholar]
- 77.Chen Z, Bai W, Li C, Wang H, Tang H, Qin Y, Rao L. Left atrial appendage parameters assessed by real-time three-dimensional transesophageal echocardiography predict thromboembolic risk in patients with nonvalvular atrial fibrillation. J Ultrasound Med. 2017;36(6):1119–1128. doi: 10.7863/ultra.16.05070. [DOI] [PubMed] [Google Scholar]
- 78.Asmarats Lluis, Bernier Mathieu, O’Hara Gilles, Paradis Jean-Michel, O’Connor Kim, Beaudoin Jonathan, Bilodeau Sylvie, Cavalcanti Rafael, Champagne Jean, Rodés-Cabau Josep. Hemodynamic impact of percutaneous left atrial appendage closure in patients with paroxysmal atrial fibrillation. Journal of Interventional Cardiac Electrophysiology. 2018;53(2):151–157. doi: 10.1007/s10840-018-0387-2. [DOI] [PubMed] [Google Scholar]
- 79.Lakkireddy D, Turagam M, Afzal MR, Rajasingh J, Atkins D, Dawn B, di Biase L, Bartus K, Kar S, Natale A, Holmes DJ., Jr Left atrial appendage closure and systemic Homeostasis: the LAA HOMEOSTASIS study. J Am Coll Cardiol. 2018;71(2):135–144. doi: 10.1016/j.jacc.2017.10.092. [DOI] [PubMed] [Google Scholar]
- 80.Lee CH, Kim JB, Jung SH, Choo SJ, Chung CH, Lee JW. Left atrial appendage resection versus preservation during the surgical ablation of atrial fibrillation. Ann Thorac Surg. 2014;97(1):124–132. doi: 10.1016/j.athoracsur.2013.07.073. [DOI] [PubMed] [Google Scholar]
- 81.Aryana A, et al. Association between incomplete surgical ligation of left atrial appendage and stroke and systemic embolization. Heart Rhythm. 2015;12(7):1431–1437. doi: 10.1016/j.hrthm.2015.03.028. [DOI] [PubMed] [Google Scholar]
- 82.Ventosa-Fernandez G, Quintana E, Castellá M, Pereda D. Exclusion of the left atrial appendage with the TigerPaw II system: a word of caution. Interact Cardiovasc Thorac Surg. 2015;21(6):803–804. doi: 10.1093/icvts/ivv256. [DOI] [PubMed] [Google Scholar]
- 83.Kanderian AS, Gillinov AM, Pettersson GB, Blackstone E, Klein AL. Success of surgical left atrial appendage closure: assessment by transesophageal echocardiography. J Am Coll Cardiol. 2008;52(11):924–929. doi: 10.1016/j.jacc.2008.03.067. [DOI] [PubMed] [Google Scholar]
- 84.Gillinov AM, Pettersson G, Cosgrove DM. Stapled excision of the left atrial appendage. J Thorac Cardiovasc Surg. 2005;129(3):679–680. doi: 10.1016/j.jtcvs.2004.07.039. [DOI] [PubMed] [Google Scholar]
- 85.Healey JS, Crystal E, Lamy A, Teoh K, Semelhago L, Hohnloser SH, Cybulsky I, Abouzahr L, Sawchuck C, Carroll S, Morillo C, Kleine P, Chu V, Lonn E, Connolly SJ. Left atrial appendage occlusion study (LAAOS): results of a randomized controlled pilot study of left atrial appendage occlusion during coronary bypass surgery in patients at risk for stroke. Am Heart J. 2005;150(2):288–293. doi: 10.1016/j.ahj.2004.09.054. [DOI] [PubMed] [Google Scholar]
- 86.Whitlock RP, Vincent J, Blackall MH, Hirsh J, Fremes S, Novick R, Devereaux PJ, Teoh K, Lamy A, Connolly SJ, Yusuf S, Carrier M, Healey JS. Left atrial appendage occlusion study II (LAAOS II) Can J Cardiol. 2013;29(11):1443–1447. doi: 10.1016/j.cjca.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 87.Aoyagi S, Tayama E, Oda T, Kosuga T, Yasunaga H. Intra-atrial excision of the left atrial appendage: a simple and easy technique. Heart Lung Circ. 2017;26(4):413–115. doi: 10.1016/j.hlc.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 88.Bartus K, Morelli RL, Szczepanski W, Kapelak B, Sadowski J, Lee RJ. Anatomic analysis of the left atrial appendage after closure with the LARIAT device. Circ Arrhythm Electrophysiol. 2014;7(4):764–767. doi: 10.1161/CIRCEP.113.001084. [DOI] [PubMed] [Google Scholar]