Abstract
Background:
Rotator cuff disease can have a progressive natural history of increasing tear size and worsening function. It remains unknown whether rotator cuff repair alters this natural history.
Methods:
A systematic review of the intermediate to long-term (minimum 5-year) results of operative rotator cuff repair and no repair of rotator cuff injuries was performed to compare (1) patient-based outcomes, (2) future surgical intervention, (3) future tear progression or recurrence, and (4) tear size. The no-repair group included both conservative treatment and surgical treatment without repair. After the application of selection criteria, 29 studies with 1,583 patients remained. Meta-regression was conducted to adjust for baseline age, sex, tear size, and duration of follow-up.
Results:
Comparison of the repair and no-repair groups revealed no significant differences in terms of age (p = 0.36), sex (p = 0.88), study level of evidence (p = 0.86), or Coleman methodology score (p = 0.8). The duration of follow-up was significantly longer for the no-repair group (p = 0.004), whereas baseline tear size was significantly larger in the repair group (p = 0.014). The percentage of patients requiring additional surgery was significantly higher in the no-repair group after adjustment for age, sex, duration of follow-up, and tear size (9.5% higher in estimated means between groups [95% confidence interval, 2.1% to 17%]; p = 0.012). The likelihood of a recurrent defect (repair group) or extension of the prior tear (no-repair group) was not different between groups after adjustment for age, sex, duration of follow-up, and tear size (p = 0.4). There were no differences between the repair and no-repair groups in terms of the Constant score after adjustment for age, sex, duration of follow-up, and tear size (p = 0.31). The final tear size was significantly larger in the no-repair group than the repair group (967 mm2 higher in estimated means between groups [95% confidence interval, 771 to 1,164 mm2]; p < 0.001).
Conclusions:
At intermediate to long-term follow-up, rotator cuff repair was associated with decreased final tear size and decreased need for future surgery after adjusting for age, sex, duration of follow-up, and tear size. The likelihood of a recurrent defect after rotator cuff repair did not differ from that of tear extension after nonoperative treatment. Thus, rotator cuff repair may not alter natural history.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Rotator cuff disease can be progressive1-5. Although not all tears increase in size6-8, many partial tears become full-thickness tears1 and many full-thickness tears increase in size1,3,5. Substantial pain and disability, pseudoparalysis9,10, and a characteristic set of chondral degenerative changes called rotator cuff tear arthropathy5,11,12 can develop as a result. As the natural history of rotator cuff disease may not be benign and the clinical results of rotator cuff repair can be good, rotator cuff repair often has been considered to be a reasonable treatment for rotator cuff tears13-16. Indeed, arthroscopic rotator cuff repair is one of the most commonly performed orthopaedic procedures in the United States and continues to increase in incidence17.
However, in the short term, most patients with a full-thickness rotator cuff tear will have excellent results with nonoperative treatment18. In addition, several randomized clinical trials with short-term results have suggested that rotator cuff repair does not provide either a clinically or statistically significant benefit over nonoperative treatment4,19,20. Nonoperative treatment does not reduce tear size or alter the natural history of rotator cuff disease1-5. Rotator cuff repair can result in an intact bone-tendon interface16,21,22, and these results can be maintained in the long term14,23-26. However, it remains unknown whether rotator cuff repair alters the natural history of rotator cuff disease.
The purpose of the present study was to conduct a systematic review of all published clinical studies with a minimum duration of follow-up of 5 years after rotator cuff repair and/or nonoperative treatment of rotator cuff disease in order to compare (1) strength and range of motion, (2) functional and patient-based outcomes, (3) the need for future surgical intervention, (4) the likelihood of future tear progression or recurrence, and (5) tear size. We hypothesized that rotator cuff repair would lead to increased strength and motion, improved outcomes, decreased need for future surgical invention, no change in the likelihood of future tear progression or recurrence, and decreased final tear size when compared with nonoperative therapy.
Materials and Methods
The present study was a systematic review of the literature. A search was performed with use of PubMed, Cochrane, and Embase databases. The search terms included rotator cuff repair, rotator cuff tear, rotator cuff conservative, rotator cuff non-operative, rotator cuff nonoperative, outcomes, long-term, and long term. The search was conducted in November 2016. The exclusion criteria were a minimum duration of follow-up of <5 years, lack of either physical examination findings or clinical data at the time of the latest follow-up, case reports, technique articles, review articles, a sample size of <10, reconstruction with a graft, tendon transfers, arthroplasty studies, and studies published in languages other than English. We manually screened the references of each included study to ensure that no studies were missed. The tables of contents of the last 2 years of The Journal of Bone & Joint Surgery, The American Journal of Sports Medicine, Clinical Orthopaedics and Related Research, Arthroscopy, and Knee Surgery, Sports Traumatology, Arthroscopy were manually searched as well. The librarian at our institution was consulted with regard to the search algorithm. Finally, authors and study data were cross-checked to prevent data duplication, and longer-term data were preferentially included. We adhered to the Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) guidelines25. Studies with levels of evidence ranging from I to IV were included. Studies were divided into those in which a repair of the rotator cuff was performed and those in which no repair was performed. The no-repair group included nonoperative treatments such as physical therapy and steroid injections, surgical subacromial decompression without repair, and surgical debridement with repair. These no-repair treatments were combined as the purpose of the study was to determine whether repair alters natural history. Repair techniques, including open and arthroscopic approaches and single-row and double-row techniques, were combined to allow comparison. Two authors were involved in the decision process regarding the inclusion and exclusion of studies.
Data Collection
The study-related data that were collected included first author, year of publication, journal, level of evidence, number of patients, minimum duration of follow-up, mean duration of follow-up, and treatment technique used (Table I). The demographic data that were collected included the number of patients in whom the dominant side was affected and the duration of symptoms before treatment (Table II). The clinical data that were collected (both preoperatively and at the time of the latest follow-up) included the number of patients who required further surgery, the number of patients with a documented increase in tear size, abduction strength, range of motion; absolute Constant score27, American Shoulder and Elbow Surgeons (ASES) score28, Disabilities of the Arm, Shoulder and Hand (DASH) and QuickDASH (an abbreviated version of the DASH) scores29, visual analogue scale (VAS) score for pain, University of California Los Angeles (UCLA) score30, Simple Shoulder Test (SST) scores31, and Western Ontario Rotator Cuff score32. The radiographic data that were collected included the number of patients at each radiographic Hamada stage12, the number of patients at each Goutallier fatty infiltration stage33, and acromiohumeral distance34. All strength measurements were converted to kilograms from pounds and newtons. The tear sizes before treatment and at the time of the latest follow-up were also collected as reported in each study on the basis of either magnetic resonance imaging (MRI) or ultrasound. All tear sizes were converted to square millimeters. When the length and width rather than the area were stated, these two 1-dimensional measurements were combined to calculate tear size, with the assumption being that the tears were rectangular, and when only a single dimension was stated, it was assumed to represent both the length and the width of a square tear; such calculations were necessary only in 3 of the 23 included repair cohorts. In addition, each cohort was classified as including partial, small, medium, large, or massive tendon tears (according to the authors’ description of the cohorts or the measurements included in the studies) with use of the Cofield system35. Studies that did not describe tear size are classified as “full” and “rotator cuff tear arthropathy” as described by the authors of these studies. When possible, cohorts were split into multiple parts to allow for finer definitions of preoperative tear size; i.e., a study with both small and medium tear cohorts in which outcomes were reported for both cohorts would be split into 2 cohorts (1 containing small tears and 1 containing medium tears) for the purposes of our analysis (Table III). Studies that included patients with tendinosis with no discrete tear at the time of inclusion were excluded. Study quality was graded with use of the Coleman methodology score36.
TABLE I.
Study Characteristics
| Variable | Repair Cohorts (N = 32) | No-Repair Cohorts (N = 13) | P Value | Test |
| Level of evidence (no. of cohorts) | 0.86 | Fisher | ||
| I | 3 (9%) | 2 (15%) | ||
| II | 2 (6%) | 1 (8%) | ||
| III | 9 (28%) | 2 (15%) | ||
| IV | 18 (56%) | 8 (62%) | ||
| Approach (no. of cohorts) | — | — | ||
| Arthroscopic | 16 (50%) | — | ||
| Open | 16 (50%) | — | ||
| Coleman methodology score* (points) | 62.5 ± 11.8 | 61.5 ± 11.3 | 0.80 | T |
The values are given as the mean and the standard deviation.
TABLE II.
Demographics
| Repair |
No Repair |
||||
| Variable | No. of Cohorts* | Value† | No. of Studies* | Value† | P Value |
| Total no. of patients/shoulders | 32 | 1,294 | 13 | 289 | — |
| Age | 30 | 58.6 yr (56.4 to 60.8 yr) | 13 | 56.5 yr (52.7 to 60.4 yr) | 0.36 |
| Male sex | 32 | 66.9% (61.2% to 72.3%) | 13 | 67.6% (60% to 74.8%) | 0.88 |
| Dominant side | 10 | 70.3% (59.8% to 80.8%) | 6 | 67% (49.1% to 85%) | 0.76 |
| Duration of follow-up | 25 | 9.6 yr (8.6 to 10.7 yr) | 12 | 14.9 yr (11.5 to 18.3 yr) | 0.004 |
The values are given as the number of studies in which the value was reported.
The values are reported as the estimated mean, with the 95% CI in parentheses.
TABLE III.
Level of Evidence, Treatment, Sample Size, and Tear Size for Each Cohort
| Study | Level of Evidence | Treatment | Sample Size (no. of patients/shoulders) | Tear Size |
| Bell et al.58 (2013) | IV | Repair | 49 | Large |
| Bidwai et al.59 (2016) | I | No repair | 15 | Medium |
| Bidwai et al.59 (2016) | I | Repair | 18 | Medium |
| Björnsson et al.60 (2010) | III | No repair | 10 | Partial |
| Björnsson et al.60 (2010) | III | No repair | 3 | Full |
| Cuff et al.61 (2016) | III | Repair | 28 | Massive |
| Denard et al.62 (2012) | III | Repair | 62 | Massive |
| Denard et al.62 (2012) | III | Repair | 45 | Massive |
| Dodson et al.63 (2010) | IV | Repair | 15 | Large |
| Galatz et al.64 (2001) | IV | Repair | 33 | Large |
| Goutallier et al.25 (2009) | III | Repair | 30 | Large |
| Gulotta et al.24 (2011) | II | Repair | 106 | Large |
| Inderhaug et al.65 (2017) | IV | Repair | 147 | Massive |
| Jaeger et al.66 (2016) | IV | No repair | 22 | Partial |
| Jaeger et al.66 (2016) | IV | No repair | 17 | Full |
| Jaeger et al.66 (2016) | IV | No repair | 17 | Rotator cuff tear arthropathy |
| Kartus et al.41 (2006) | IV | No repair | 26 | Partial |
| Kijima et al.67 (2012) | II | No repair | 43 | Full |
| Kluger et al.51 (2011) | III | Repair | 72 | Large |
| Kluger et al.51 (2011) | III | Repair | 35 | Large |
| Lucena et al.68 (2015) | III | Repair | 25 | Medium |
| Lucena et al.68 (2015) | III | Repair | 25 | Medium |
| Marrero et al.69 (2011) | IV | Repair | 24 | Medium |
| Miyazaki et al.23 (2015) | III | Repair | 35 | Massive |
| Moosmayer et al.4 (2014) | I | No repair | 39 | Small |
| Moosmayer et al.4 (2014) | I | Repair | 52 | Medium |
| Moosmayer et al.4 (2014) | I | Repair | 12 | Medium |
| Nich et al.70 (2009) | IV | Repair | 33 | Medium |
| Nich et al.70 (2009) | IV | Repair | 4 | Medium |
| Norlin et al.71 (2008) | IV | Repair | 89 | Tendinosis |
| Norlin et al.71 (2008) | IV | Repair | 45 | Partial |
| Norlin et al.71 (2008) | IV | Repair | 5 | Partial |
| Norlin et al.71 (2008) | IV | Repair | 12 | Small |
| Norlin et al.71 (2008) | IV | Repair | 11 | Medium |
| Paxton et al.72 (2013) | IV | Repair | 15 | Massive |
| Porcellini et al.73 (2011) | IV | Repair | 67 | Massive |
| Ranebo et al.42 (2017) | IV | No repair | 24 | Full |
| Ranebo et al.42 (2017) | IV | No repair | 45 | Partial |
| Saraswat et al.14 (2015) | II | Repair | 59 | Medium |
| Sperling et al.74 (2004) | IV | Repair | 29 | Large |
| Stephens et al.75 (1998) | IV | No repair | 11 | Partial |
| Stephens et al.75 (1998) | IV | No repair | 17 | Complete |
| Stuart et al.76 (2013) | IV | Repair | 15 | Partial |
| Zandi et al.77 (2006) | IV | Repair | 74 | Medium |
| Zumstein et al.26 (2008) | IV | Repair | 23 | Massive |
Statistical Analysis
Study characteristics, including level of evidence, surgical approach (arthroscopic or open), and Coleman methodology score were summarized as the count (and percentage) or the mean and the standard deviation and were compared between repair and no-repair cohorts with use of the Fisher exact test or t test as appropriate. Age, male percentage, dominant-side percentage, and number of years of follow-up were pooled across studies with use of a random-effects model with inverse variance weighting. A chi-square Q test for heterogeneity was used to test for differences between repair and no-repair groups. Mixed-effects meta-regression models were used to compare the repair and no-repair groups in terms of the percentage of patients or shoulders requiring further surgery, the percentage with an increase in tear size or recurrence of a defect, and the post-treatment operative Constant score, with adjustment for age, male percentage, number of years of follow-up, and preoperative tear size. Mixed-effects meta-regression also was used to compare the repair and no-repair groups with regard to postoperative ASES, VAS pain score, elevation, elevation strength, and tear size (while controlling for preoperative measures). Meta-analysis and meta-regression were conducted with use of the R package version 3.4 for meta-analysis37. Studies in which results were presented as summaries for different subgroups such as repair status or treatment type were included in the analysis as separate studies. If variance or standard deviation was not given, standard deviation was calculated from the standard error, 95% confidence interval (CI), or range38, as available. The level of significance was set at p < 0.05, and all tests were 2-tailed.
Results
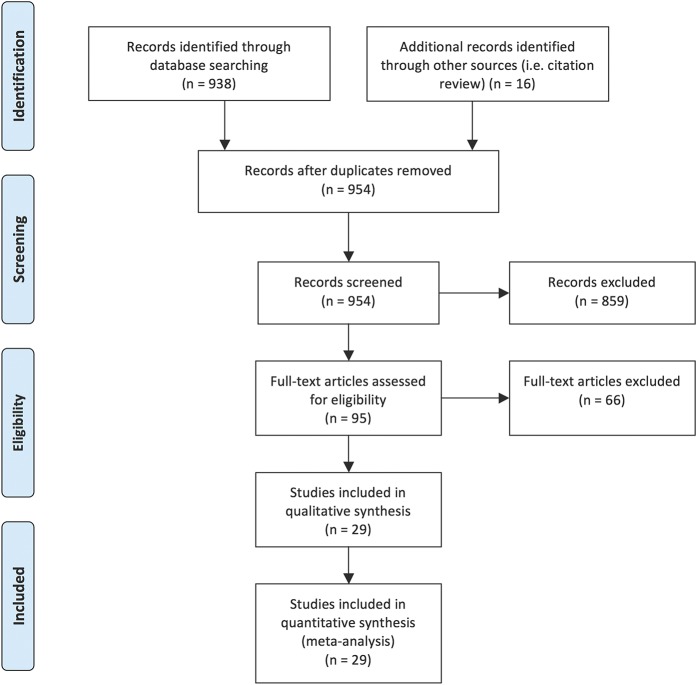
The initial search revealed 938 abstracts. After the application of our study-selection algorithm, 29 studies remained (Fig. 1); of those, 8 evaluated the outcomes of treatment without repair and 23 evaluated the outcomes of repair. The studies included 2 randomized clinical trials, 3 prospective cohort series, 7 retrospective cohort series, and 17 retrospective case series. There were no significant differences in Coleman methodology score between the individual repair cohorts (p = 0.8). The overall repair group that was assessed in the present study included a total of 1,294 patients with a mean duration of follow-up of 9.6 years (95% CI, 8.6 to 10.7 years) (Table II). Of the patients in the repair group, 722 (56%) underwent an arthroscopic repair and 572 (44%) underwent open repair. Of the patients in the repair group, 45 (3.5%) were managed with a double-row technique, 461 (35.6%) were managed with a single-row technique, 505 (39.0%) were managed with a transosseous technique, and 283 (21.9%) were managed with an unspecified technique. The no-repair group included a total of 289 patients with a mean duration of follow-up of 14.9 years (95% CI, 11.5 to 18.3 years). After the studies were split into tear-size and treatment cohorts, there were 32 individual cohorts within the overall repair group and 13 individual cohorts within the overall no-repair group. The repair and no-repair cohorts did not differ with respect to age (p = 0.36), sex (p = 0.88), or the percentage of patients in whom the tear was on the dominant side (p = 0.76) (Table II). The duration of follow-up was significantly longer in the no-repair group (p = 0.004). The baseline tear size was significantly larger in the repair group (p = 0.014) (Table IV). Fewer than 3 repair studies and fewer than 3 no-repair studies evaluated pre-treatment strength, pre-treatment active forward elevation, pre-treatment Constant score, pre-treatment ASES score, pre-treatment VAS score, and radiographic outcomes, and thus no analyses were conducted on these variables.
Fig. 1.
PRISMA diagram showing the result of application of the study algorithm to the number of studies included, with the number of studies removed with application of each exclusion criterion displayed.
TABLE IV.
Distribution of Pre-Treatment Tear Types in No-Repair and Repair Cohorts
| Tear Type | No-Repair Cohort (N = 289) | Repair Cohort (N = 1,294) |
| Partial | 114 (39%) | 154 (12%) |
| Small | 39 (13%) | 12 (1%) |
| Medium | 15 (5%) | 337 (26%) |
| Large | 0 (0%) | 369 (29%) |
| Massive | 0 (0%) | 422 (33%) |
| Full | 104 (36%) | 0 (0%) |
| Rotator cuff tear arthropathy | 17 (6%) | 0 (0%) |
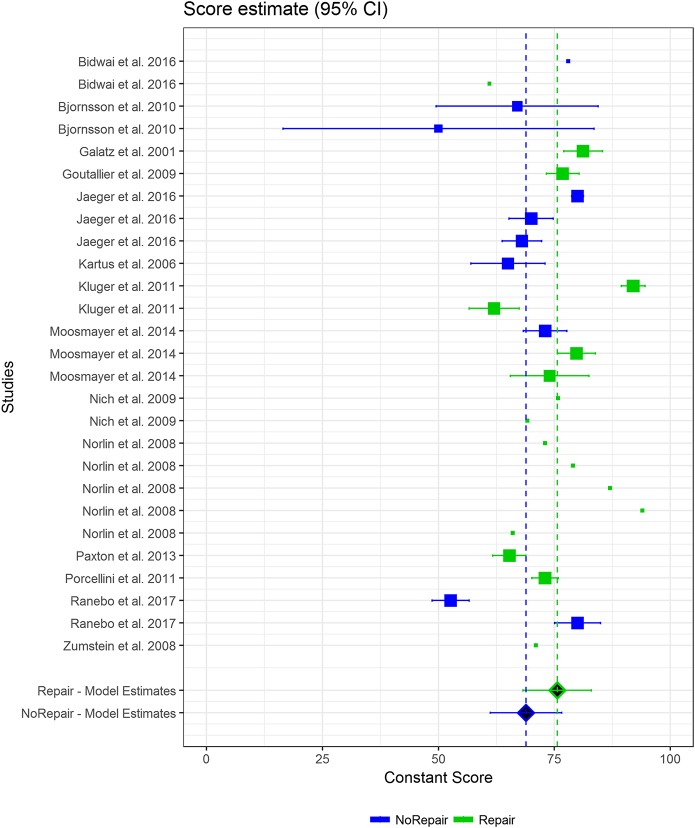
There were no differences between the groups in terms of physical examination findings or strength at the time of the latest follow-up. Specifically, there were no differences in terms of elevation range of motion (p = 0.4) or elevation strength (p = 0.72) (Table V). There also were no differences between the groups in terms of functional and patient-based outcomes, including the ASES score (p = 0.86) or VAS pain score (p = 0.94) at the time of the latest follow up (Table VI). In addition, the final Constant score did not differ between the groups after adjusting for age, sex, duration of follow-up, and tear size (p = 0.31) (Fig. 2 and Table VI).
Fig. 2.
Forest plot showing the final follow-up Constant scores for the repair (green) and no-repair (blue) cohorts. The horizontal bars show the 95% CIs for individual cohorts. The vertical dashed lines show the grand means.
TABLE V.
Effect of Repair (Versus No Repair) on Primary Outcomes with Adjustment for Covariates*
| Outcome | No. of Cohorts | Coefficient (95% CI)† | P Value |
| Percent requiring additional surgery | 34 | −0.095 (−0.17 to −0.021) | 0.012 |
| Percent with subsequent increase in tear size | 22 | 0.529 (−0.693 to 1.751) | 0.4 |
| Constant score at latest follow-up | 14 | 21.197 (−20.01 to 62.403) | 0.31 |
Age, sex, duration of follow-up, and pre-treatment tear size.
Coefficients can be interpreted as estimated mean differences between groups after adjustment for covariates.
TABLE VI.
Effect of Repair (Versus No Repair) on Secondary Outcomes
| Outcome at Latest Follow-up | No. of Cohorts | Coefficient* (95% CI) | P Value |
| ASES score | 10 | 1.67 (−17.21 to 20.55) | 0.86 |
| VAS pain score | 8 | 1 (−25.23 to 27.23) | 0.94 |
| Elevation | 9 | −14.87° (−49.31° to 19.57°) | 0.4 |
| Elevation strength | 6 | 1.13 kg (−5.17 to 7.43 kg) | 0.72 |
| Tear size | 6 | −967.37 mm2 (−1,163.89 to −770.84 mm2) | <0.001 |
Coefficients can be interpreted as estimated mean differences between groups after adjustment for covariates.
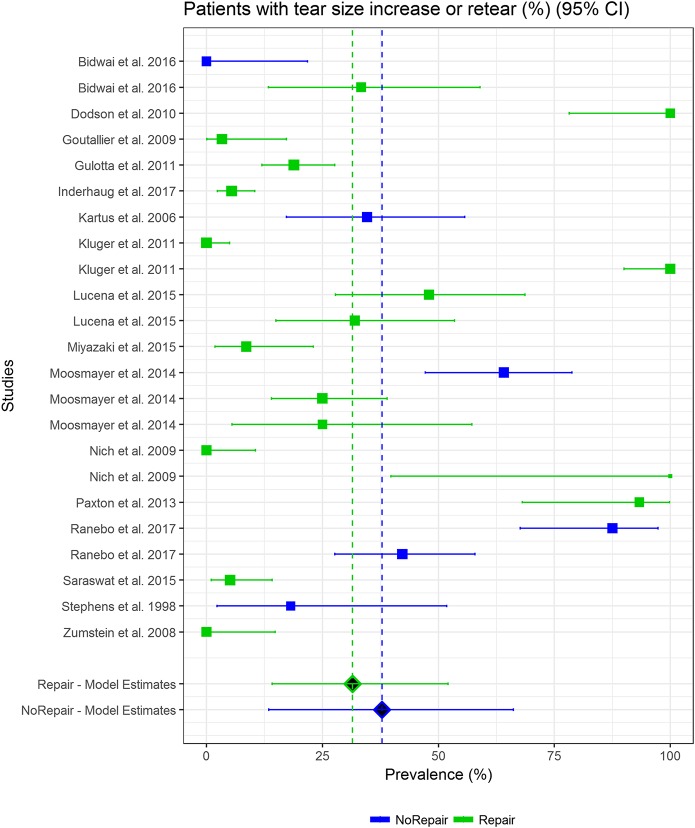
The percentage of patients requiring additional surgery was significantly higher in the no-repair group after adjustment for age, sex, duration of follow-up, and tear size (9.5% higher in estimated means between groups [95% CI, 2.1% to 17%]; p = 0.012) (Fig. 3 and Table VI). The percentage of patients with a recurrent defect in the repair group did not differ from the percentage of patients with an increase in tear size in the no-repair group after adjusting for age, sex, duration of follow-up, and tear size (p = 0.4) (Fig. 4 and Table V). The final tear size was significantly larger in the no-repair group than the repair group (967 mm2 greater [95% CI, 771 to 1,164 mm2 greater], p < 0.001) (Table VI).
Fig. 3.
Forest plot showing the mean percentage of patients requiring additional surgery for the repair (green) and no-repair (blue) cohorts. The horizontal bars show the 95% CIs for individual cohorts. The vertical dashed lines show the grand means.
Fig. 4.
Forest plot showing the percentage of patients sustaining either a recurrent defect or an enlargement or the tear from pre-treatment to the latest follow-up for the repair (green) and no-repair (blue) cohorts. The horizontal bars show the 95% CIs for individual cohorts. The vertical dashed lines show the grand means.
Discussion
Rotator cuff tears may increase in size and can lead to pain, disability, and ultimately pseudoparalysis and rotator cuff tear arthropathy1-5,9-12. Because rotator cuff repair can result in a continuous bone-tendon interface in the long term14,16,21-26, rotator cuff repair may be able to forestall this natural history. The purpose of the present study was to conduct a systematic review of all published clinical studies with a minimum duration of follow-up of 5 years after rotator cuff repair and/or nonoperative treatment of rotator cuff disease in order to evaluate (1) strength and range of motion on physical examination, (2) functional and patient-based outcomes, (3) the need for future surgical intervention, (4) the likelihood of future tear progression or recurrence, and (5) final tear size.
The present study demonstrated no differences between rotator cuff repair and no repair with respect to strength and range of motion. This finding is in concordance with the 3 randomized clinical trials that have been performed to date, each of which demonstrated no differences between rotator cuff repair and no repair with respect to strength and range of motion4,19,20. Following rotator cuff repair, shoulders in which an intact tendon is achieved have greater strength than those in which an intact tendon is not achieved39. In addition, strength has been correlated with tear size5,40. Given our finding that final tear size was larger in the no-repair group as compared with the repair group, improved strength would be expected in the repair group, but this effect may have been obscured by heterogeneity in strength measurement between studies.
We found that, compared with no repair, rotator cuff repair did not improve outcomes as measured with the Constant score even after adjustment for age, sex, duration of follow-up, and tear size. These findings are roughly congruent with those of the 3 randomized clinical trials that have been conducted to date4,19,20. One of those studies demonstrated no clinically or statistically significant differences between groups19, 1 demonstrated a statistically but not clinically significantly better outcome in terms of the Constant score for rotator cuff repair resulting in an intact tendon4, and 1 demonstrated both a clinically and statistically significantly better outcome in terms of the Constant score for rotator cuff repair resulting in an intact tendon20.
Our study demonstrated that rotator cuff repair appears to protect the shoulder from the need for future operative intervention after adjusting for age, sex, duration of follow-up, and tear size. As tear size increases following nonoperative treatment, some patients may become increasingly symptomatic and may be considered for arthroscopic debridement, subacromial decompression, biceps tenotomy or tenodesis, rotator cuff repair, tendon transfer, or ultimately reverse total shoulder arthroplasty. In addition, tear size4,41,42, age, and muscular atrophy33,42 all continue to increase following nonoperative treatment, thereby decreasing the likelihood of achieving an intact tendon21,22,33,38,43-55. As a result, nonoperative treatment both increases the likelihood of future surgery and may decrease the likelihood of success if that surgery is a repair.
The present study indicates that rotator cuff repair does not decrease the likelihood of sustaining a future tear after adjusting for age, sex, duration of follow-up, and tear size but does decrease final tear size. Rotator cuff repair does not alter the underlying tendon biology that causes rotator cuff tearing, and therefore the likelihood of a recurrent defect after rotator cuff repair may be similar to the likelihood of tear progression with nonoperative treatment. A “recurrent defect” after rotator cuff repair thus may be understood not as a surgical failure but instead as a continuation of the underlying, unaltered, biological degeneration that leads to rotator cuff pathology. However, our study demonstrated that final tear size was significantly smaller after rotator cuff repair than after treatment without repair.
Our study has several limitations. First, the data were drawn from studies with different designs, and thus heterogeneity between studies limits the conclusions that can be drawn. In addition, surgical repairs and postoperative rehabilitation have changed between the publication of the first study in 2001 and that of the most recent study in 2017. Second, as with any meta-analysis, the quality of the conclusions that can be drawn is limited by the quality of the original data, which are drawn from studies of varying levels of evidence. Third, the included studies were limited to those published in English, which may introduce bias. However, each of these limitations affect both the repair and no-repair cohorts, which may mitigate their influence on our results. Fourth, a variety of repair and no-repair treatment methods were included. There is continuing debate as to whether single-row or double-row repair provides superior outcomes or a higher likelihood of an intact tendon56. Fifth, there are certainly other variables that would have been valuable to compare, such as radiographic progression toward rotator cuff tear arthropathy as indicated by Hamada stage, muscular atrophy or tendon quality at baseline and at the latest follow-up, and which specific subsequent procedures were necessary. Unfortunately, these details were not available in the included studies and thus we could not analyze them. Sixth, tear size was measured on both MRI and ultrasound scans. Finally, although no difference existed in baseline demographic data between the repair and no-repair cohorts, unmeasured residual bias likely existed between the cohorts. For instance, the baseline tear size was larger in the repair group. To mitigate this effect, we controlled for tear size in our analyses of the primary outcomes. However, for many other variables (strength, motion, Constant score, etc.), insufficient evidence existed within the pre-treatment data to allow comparison. We were able to control for age, sex, and tear size, which are the 3 variables that have been shown to most strongly correlate with outcome57. Only a randomized controlled trial will be able to overcome this limitation.
In conclusion, at intermediate to long-term follow-up, rotator cuff repair was associated with decreased final tear size and decreased need for future surgery but was not associated with higher final standardized outcomes after adjusting for age, sex, duration of follow-up, and tear size. The likelihood of a recurrent defect after rotator cuff repair did not differ from the likelihood of tear extension with nonoperative treatment, and thus rotator cuff repair may not alter natural history.
Disclosure of Potential Conflicts of Interest
Footnotes
Investigation performed at the University of Utah, Salt Lake City, Utah
Disclosure: This study was supported in part by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 5UL1TR001067-02 (formerly 8UL1TR000105 and UL1RR025764). On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work and “yes” to indicate that the author had a patent and/or copyright, planned, pending, or issued, broadly relevant to this work (http://links.lww.com/JBJSOA/A29).
References
- 1.Keener JD, Galatz LM, Teefey SA, Middleton WD, Steger-May K, Stobbs-Cucchi G, Patton R, Yamaguchi K. A prospective evaluation of survivorship of asymptomatic degenerative rotator cuff tears. J Bone Joint Surg Am. 2015. January 21;97(2):89-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keener JD, Wei AS, Kim HM, Steger-May K, Yamaguchi K. Proximal humeral migration in shoulders with symptomatic and asymptomatic rotator cuff tears. J Bone Joint Surg Am. 2009. June;91(6):1405-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moosmayer S, Tariq R, Stiris M, Smith HJ. The natural history of asymptomatic rotator cuff tears: a three-year follow-up of fifty cases. J Bone Joint Surg Am. 2013. July 17;95(14):1249-55. [DOI] [PubMed] [Google Scholar]
- 4.Moosmayer S, Lund G, Seljom US, Haldorsen B, Svege IC, Hennig T, Pripp AH, Smith HJ. Tendon repair compared with physiotherapy in the treatment of rotator cuff tears: a randomized controlled study in 103 cases with a five-year follow-up. J Bone Joint Surg Am. 2014. September 17;96(18):1504-14. [DOI] [PubMed] [Google Scholar]
- 5.Moosmayer S, Gärtner AV, Tariq R. The natural course of nonoperatively treated rotator cuff tears: an 8.8-year follow-up of tear anatomy and clinical outcome in 49 patients. J Shoulder Elbow Surg. 2017. April;26(4):627-34. Epub 2017 Jan 12. [DOI] [PubMed] [Google Scholar]
- 6.Jost B, Zumstein M, Pfirrmann CWA, Gerber C. Long-term outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2006. March;88(3):472-9. [DOI] [PubMed] [Google Scholar]
- 7.Zingg PO, Jost B, Sukthankar A, Buhler M, Pfirrmann CWA, Gerber C. Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Joint Surg Am. 2007. September;89(9):1928-34. [DOI] [PubMed] [Google Scholar]
- 8.Fucentese SF, von Roll AL, Pfirrmann CW, Gerber C, Jost B. Evolution of nonoperatively treated symptomatic isolated full-thickness supraspinatus tears. J Bone Joint Surg Am. 2012. May 02;94(9):801-8. [DOI] [PubMed] [Google Scholar]
- 9.Boileau P, Chuinard C, Roussanne Y, Bicknell RT, Rochet N, Trojani C. Reverse shoulder arthroplasty combined with a modified latissimus dorsi and teres major tendon transfer for shoulder pseudoparalysis associated with dropping arm. Clin Orthop Relat Res. 2008. March;466(3):584-93. Epub 2008 Jan 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Denard PJ, Lädermann A, Brady PC, Narbona P, Adams CR, Arrigoni P, Huberty D, Zlatkin MB, Sanders TG, Burkhart SS. Pseudoparalysis from a massive rotator cuff tear is reliably reversed with an arthroscopic rotator cuff repair in patients without preoperative glenohumeral arthritis. Am J Sports Med. 2015. October;43(10):2373-8. Epub 2015 Aug 21. [DOI] [PubMed] [Google Scholar]
- 11.Chalmers PN, Salazar DH, Steger-May K, Chamberlain AM, Stobbs-Cucchi G, Yamaguchi K, Keener JD. Radiographic progression of arthritic changes in shoulders with degenerative rotator cuff tears. J Shoulder Elbow Surg. 2016. November;25(11):1749-55. Epub 2016 Aug 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990. May;(254):92-6. [PubMed] [Google Scholar]
- 13.Robinson HA, Lam PH, Walton JR, Murrell GAC. The effect of rotator cuff repair on early overhead shoulder function: a study in 1600 consecutive rotator cuff repairs. J Shoulder Elbow Surg. 2017. January;26(1):20-9. Epub 2016 Aug 9. [DOI] [PubMed] [Google Scholar]
- 14.Saraswat MK, Styles-Tripp F, Beaupre LA, Luciak-Corea C, Otto D, Lalani A, Balyk RA. Functional outcomes and health-related quality of life after surgical repair of full-thickness rotator cuff tears using a mini-open technique: a concise 10-year follow-up of a previous report. Am J Sports Med. 2015. November;43(11):2794-9. Epub 2015 Sep 22. [DOI] [PubMed] [Google Scholar]
- 15.Moraiti C, Valle P, Maqdes A, Boughebri O, Dib C, Giakas G, Kany J, Elkholti K, Garret J, Katz D, Leclère FM, Valenti P. Comparison of functional gains after arthroscopic rotator cuff repair in patients over 70 years of age versus patients under 50 years of age: a prospective multicenter study. Arthroscopy. 2015. February;31(2):184-90. Epub 2014 Nov 11. [DOI] [PubMed] [Google Scholar]
- 16.Keener JD, Galatz LM, Stobbs-Cucchi G, Patton R, Yamaguchi K. Rehabilitation following arthroscopic rotator cuff repair: a prospective randomized trial of immobilization compared with early motion. J Bone Joint Surg Am. 2014. January 01;96(1):11-9. [DOI] [PubMed] [Google Scholar]
- 17.Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012. February 01;94(3):227-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dunn WR, Kuhn JE, Sanders R, An Q, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Harrell F, Holloway BG, Jones GL, Ma CB, Marx RG, McCarty EC, Poddar SK, Smith MV, Spencer EE, Vidal AF, Wolf BR, Wright RW; MOON Shoulder Group. 2013 Neer Award: predictors of failure of nonoperative treatment of chronic, symptomatic, full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2016. August;25(8):1303-11. [DOI] [PubMed] [Google Scholar]
- 19.Kukkonen J, Joukainen A, Lehtinen J, Mattila KT, Tuominen EK, Kauko T, Aärimaa V. Treatment of non-traumatic rotator cuff tears: A randomised controlled trial with one-year clinical results. Bone Joint J. 2014. January;96-B(1):75-81. [DOI] [PubMed] [Google Scholar]
- 20.Lambers Heerspink FO, van Raay JJAM, Koorevaar RCT, van Eerden PJ, Westerbeek RE, van ’t Riet E, van den Akker-Scheek I, Diercks RL. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: a randomized controlled trial. J Shoulder Elbow Surg. 2015. August;24(8):1274-81. [DOI] [PubMed] [Google Scholar]
- 21.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005. June;87(6):1229-40. [DOI] [PubMed] [Google Scholar]
- 22.Le BTN, Wu XL, Lam PH, Murrell GAC. Factors predicting rotator cuff retears: an analysis of 1000 consecutive rotator cuff repairs. Am J Sports Med. 2014. May;42(5):1134-42. Epub 2014 Apr 18. [DOI] [PubMed] [Google Scholar]
- 23.Miyazaki AN, Santos PD, da Silva LA, do Val Sella G, Checchia SL, Yonamine AM. Are the good functional results from arthroscopic repair of massive rotator cuff injuries maintained over the long term? Rev Bras Ortop. 2015. December 30;51(1):40-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gulotta LV, Nho SJ, Dodson CC, Adler RS, Altchek DW, MacGillivray JD; HSS Arthroscopic Rotator Cuff Registry. Prospective evaluation of arthroscopic rotator cuff repairs at 5 years: part I—functional outcomes and radiographic healing rates. J Shoulder Elbow Surg. 2011. September;20(6):934-40. Epub 2011 Jun 29. [DOI] [PubMed] [Google Scholar]
- 25.Goutallier D, Postel JM, Radier C, Bernageau J, Zilber S. Long-term functional and structural outcome in patients with intact repairs 1 year after open transosseous rotator cuff repair. J Shoulder Elbow Surg. 2009. Jul-Aug;18(4):521-8. Epub 2009 Feb 11. [DOI] [PubMed] [Google Scholar]
- 26.Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2008. November;90(11):2423-31. [DOI] [PubMed] [Google Scholar]
- 27.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987. January;(214):160-4. [PubMed] [Google Scholar]
- 28.L’Insalata JC, Warren RF, Cohen SB, Altchek DW, Peterson MG. A self-administered questionnaire for assessment of symptoms and function of the shoulder. J Bone Joint Surg Am. 1997. May;79(5):738-48. [PubMed] [Google Scholar]
- 29.Davis AM, Beaton DE, Hudak P, Amadio P, Bombardier C, Cole D, Hawker G, Katz JN, Makela M, Marx RG, Punnett L, Wright JG. Measuring disability of the upper extremity: a rationale supporting the use of a regional outcome measure. J Hand Ther. 1999. Oct-Dec;12(4):269-74. [DOI] [PubMed] [Google Scholar]
- 30.Amstutz HC, Sew Hoy AL, Clarke IC. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981. Mar-Apr;(155):7-20. [PubMed] [Google Scholar]
- 31.Matsen FA, 3rd, Tang A, Russ SM, Hsu JE. Relationship between patient-reported assessment of shoulder function and objective range-of-motion measurements. J Bone Joint Surg Am. 2017. March 01;99(5):417-26. [DOI] [PubMed] [Google Scholar]
- 32.Kirkley A, Alvarez C, Griffin S. The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: The Western Ontario Rotator Cuff Index. Clin J Sport Med. 2003. March;13(2):84-92. [DOI] [PubMed] [Google Scholar]
- 33.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994. July;(304):78-83. [PubMed] [Google Scholar]
- 34.McCreesh KM, Crotty JM, Lewis JS. Acromiohumeral distance measurement in rotator cuff tendinopathy: is there a reliable, clinically applicable method? A systematic review. Br J Sports Med. 2015. March;49(5):298-305. Epub 2013 Jul 2. [DOI] [PubMed] [Google Scholar]
- 35.Cofield RH. Subscapular muscle transposition for repair of chronic rotator cuff tears. Surg Gynecol Obstet. 1982. May;154(5):667-72. [PubMed] [Google Scholar]
- 36.Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD; Victorian Institute of Sport Tendon Study Group. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Scand J Med Sci Sports. 2000. February;10(1):2-11. [DOI] [PubMed] [Google Scholar]
- 37.Schwarzer G. Meta: an R package for meta-analysis. R News. 2007. [Google Scholar]
- 38.Mihata T, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, Fujiwara K, Kinoshita M. Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am J Sports Med. 2011. October;39(10):2091-8. Epub 2011 Jul 22. [DOI] [PubMed] [Google Scholar]
- 39.Yang J, Jr, Robbins M, Reilly J, Maerz T, Anderson K. The clinical effect of a rotator cuff retear: a meta-analysis of arthroscopic single-row and double-row repairs. Am J Sports Med. 2017. March;45(3):733-41. Epub 2016 Jul 21. [DOI] [PubMed] [Google Scholar]
- 40.Kim HM, Teefey SA, Zelig A, Galatz LM, Keener JD, Yamaguchi K. Shoulder strength in asymptomatic individuals with intact compared with torn rotator cuffs. J Bone Joint Surg Am. 2009. February;91(2):289-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kartus J, Kartus C, Rostgård-Christensen L, Sernert N, Read J, Perko M. Long-term clinical and ultrasound evaluation after arthroscopic acromioplasty in patients with partial rotator cuff tears. Arthroscopy. 2006. January;22(1):44-9. [DOI] [PubMed] [Google Scholar]
- 42.Ranebo MC, Björnsson Hallgren HC, Norlin R, Adolfsson LE. Clinical and structural outcome 22 years after acromioplasty without tendon repair in patients with subacromial pain and cuff tears. J Shoulder Elbow Surg. 2017. July;26(7):1262-70. Epub 2017 Jan 25. [DOI] [PubMed] [Google Scholar]
- 43.Cho NS, Lee BG, Rhee YG. Arthroscopic rotator cuff repair using a suture bridge technique: is the repair integrity actually maintained? Am J Sports Med. 2011. October;39(10):2108-16. Epub 2011 Feb 24. [DOI] [PubMed] [Google Scholar]
- 44.Chung SW, Oh JH, Gong HS, Kim JY, Kim SH. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med. 2011. October;39(10):2099-107. Epub 2011 Aug 3. [DOI] [PubMed] [Google Scholar]
- 45.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000. April;82(4):505-15. [DOI] [PubMed] [Google Scholar]
- 46.Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997. November;(344):275-83. [PubMed] [Google Scholar]
- 47.Gladstone JN, Bishop JY, Lo IKY, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007. May;35(5):719-28. Epub 2007 Mar 2. [DOI] [PubMed] [Google Scholar]
- 48.Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006. May-Jun;15(3):290-9. [DOI] [PubMed] [Google Scholar]
- 49.Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994. July;(304):43-53. [PubMed] [Google Scholar]
- 50.Huijsmans PE, Pritchard MP, Berghs BM, van Rooyen KS, Wallace AL, de Beer JF. Arthroscopic rotator cuff repair with double-row fixation. J Bone Joint Surg Am. 2007. June;89(6):1248-57. [DOI] [PubMed] [Google Scholar]
- 51.Kluger R, Bock P, Mittlböck M, Krampla W, Engel A. Long-term survivorship of rotator cuff repairs using ultrasound and magnetic resonance imaging analysis. Am J Sports Med. 2011. October;39(10):2071-81. Epub 2011 May 24. [DOI] [PubMed] [Google Scholar]
- 52.Nho SJ, Shindle MK, Adler RS, Warren RF, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: subgroup analysis. J Shoulder Elbow Surg. 2009. Sep-Oct;18(5):697-704. Epub 2009 Mar 9. [DOI] [PubMed] [Google Scholar]
- 53.Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2007. May;89(5):953-60. [DOI] [PubMed] [Google Scholar]
- 54.Lapner PLC, Sabri E, Rakhra K, McRae S, Leiter J, Bell K, Macdonald P. A multicenter randomized controlled trial comparing single-row with double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2012. July 18;94(14):1249-57. [DOI] [PubMed] [Google Scholar]
- 55.Tashjian RZ, Hollins AM, Kim HM, Teefey SA, Middleton WD, Steger-May K, Galatz LM, Yamaguchi K. Factors affecting healing rates after arthroscopic double-row rotator cuff repair. Am J Sports Med. 2010. December;38(12):2435-42. Epub 2010 Oct 28. [DOI] [PubMed] [Google Scholar]
- 56.Mascarenhas R, Chalmers PN, Sayegh ET, Bhandari M, Verma NN, Cole BJ, Romeo AA. Is double-row rotator cuff repair clinically superior to single-row rotator cuff repair: a systematic review of overlapping meta-analyses. Arthroscopy. 2014. September;30(9):1156-65. Epub 2014 May 10. [DOI] [PubMed] [Google Scholar]
- 57.Diebold G, Lam P, Walton J, Murrell GAC. Relationship between age and rotator cuff retear: a study of 1,600 consecutive rotator cuff repairs. J Bone Joint Surg Am. 2017. July 19;99(14):1198-205. [DOI] [PubMed] [Google Scholar]
- 58.Bell S, Lim YJ, Coghlan J. Long-term longitudinal follow-up of mini-open rotator cuff repair. J Bone Joint Surg Am. 2013. January 16;95(2):151-7. [DOI] [PubMed] [Google Scholar]
- 59.Bidwai ASC, Birch A, Temperley D, Odak S, Walton MJ, Haines JF, Trail I. Medium- to long-term results of a randomized controlled trial to assess the efficacy of arthoscopic-subacromial decompression versus mini-open repair for the treatment of medium-sized rotator cuff tears. Shoulder Elbow. 2016. April;8(2):101-5. Epub 2015 Dec 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Björnsson H, Norlin R, Knutsson A, Adolfsson L. Fewer rotator cuff tears fifteen years after arthroscopic subacromial decompression. J Shoulder Elbow Surg. 2010. January;19(1):111-5. [DOI] [PubMed] [Google Scholar]
- 61.Cuff DJ, Pupello DR, Santoni BG. Partial rotator cuff repair and biceps tenotomy for the treatment of patients with massive cuff tears and retained overhead elevation: midterm outcomes with a minimum 5 years of follow-up. J Shoulder Elbow Surg. 2016. November;25(11):1803-9. Epub 2016 Jun 6. [DOI] [PubMed] [Google Scholar]
- 62.Denard PJ, Jiwani AZ, Lädermann A, Burkhart SS. Long-term outcome of arthroscopic massive rotator cuff repair: the importance of double-row fixation. Arthroscopy. 2012. July;28(7):909-15. Epub 2012 Feb 24. [DOI] [PubMed] [Google Scholar]
- 63.Dodson CC, Kitay A, Verma NN, Adler RS, Nguyen J, Cordasco FA, Altchek DW. The long-term outcome of recurrent defects after rotator cuff repair. Am J Sports Med. 2010. January;38(1):35-9. Epub 2009 Sep 14. [DOI] [PubMed] [Google Scholar]
- 64.Galatz LM, Griggs S, Cameron BD, Iannotti JP. Prospective longitudinal analysis of postoperative shoulder function : a ten-year follow-up study of full-thickness rotator cuff tears. J Bone Joint Surg Am. 2001. July;83(7):1052-6. [PubMed] [Google Scholar]
- 65.Inderhaug E, Kollevold KH, Kalsvik M, Hegna J, Solheim E. Preoperative NSAIDs, non-acute onset and long-standing symptoms predict inferior outcome at long-term follow-up after rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2017. July;25(7):2067-72. Epub 2015 Oct 31. [DOI] [PubMed] [Google Scholar]
- 66.Jaeger M, Berndt T, Rühmann O, Lerch S. Patients with impingement syndrome with and without rotator cuff tears do well 20 years after arthroscopic subacromial decompression. Arthroscopy. 2016. March;32(3):409-15. Epub 2015 Oct 24. [DOI] [PubMed] [Google Scholar]
- 67.Kijima H, Minagawa H, Nishi T, Kikuchi K, Shimada Y. Long-term follow-up of cases of rotator cuff tear treated conservatively. J Shoulder Elbow Surg. 2012. April;21(4):491-4. Epub 2012 Jan 21. [DOI] [PubMed] [Google Scholar]
- 68.Lucena TR, Lam PH, Millar NL, Murrell GA. The temporal outcomes of open versus arthroscopic knotted and knotless rotator cuff repair over 5 years. Shoulder Elbow. 2015. October;7(4):244-55. Epub 2015 Apr 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Marrero LG, Nelman KR, Nottage WM. Long-term follow-up of arthroscopic rotator cuff repair. Arthroscopy. 2011. July;27(7):885-8. Epub 2011 May 28. [DOI] [PubMed] [Google Scholar]
- 70.Nich C, Mütschler C, Vandenbussche E, Augereau B. Long-term clinical and MRI results of open repair of the supraspinatus tendon. Clin Orthop Relat Res. 2009. October;467(10):2613-22. Epub 2009 Jun 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Norlin R, Adolfsson L. Small full-thickness tears do well ten to thirteen years after arthroscopic subacromial decompression. J Shoulder Elbow Surg. 2008. Jan-Feb;17(1)(Suppl):12S-6S. [DOI] [PubMed] [Google Scholar]
- 72.Paxton ES, Teefey SA, Dahiya N, Keener JD, Yamaguchi K, Galatz LM. Clinical and radiographic outcomes of failed repairs of large or massive rotator cuff tears: minimum ten-year follow-up. J Bone Joint Surg Am. 2013. April 03;95(7):627-32. [DOI] [PubMed] [Google Scholar]
- 73.Porcellini G, Castagna A, Cesari E, Merolla G, Pellegrini A, Paladini P. Partial repair of irreparable supraspinatus tendon tears: clinical and radiographic evaluations at long-term follow-up. J Shoulder Elbow Surg. 2011. October;20(7):1170-7. Epub 2011 Feb 1. [DOI] [PubMed] [Google Scholar]
- 74.Sperling JW, Cofield RH, Schleck C. Rotator cuff repair in patients fifty years of age and younger. J Bone Joint Surg Am. 2004. October;86(10):2212-5. [DOI] [PubMed] [Google Scholar]
- 75.Stephens SR, Warren RF, Payne LZ, Wickiewicz TL, Altchek DW. Arthroscopic acromioplasty: a 6- to 10-year follow-up. Arthroscopy. 1998. May-Jun;14(4):382-8. [DOI] [PubMed] [Google Scholar]
- 76.Stuart KD, Karzel RP, Ganjianpour M, Snyder SJ. Long-term outcome for arthroscopic repair of partial articular-sided supraspinatus tendon avulsion. Arthroscopy. 2013. May;29(5):818-23. Epub 2013 Apr 2. [DOI] [PubMed] [Google Scholar]
- 77.Zandi H, Coghlan JA, Bell SN. Mini-incision rotator cuff repair: a longitudinal assessment with no deterioration of result up to nine years. J Shoulder Elbow Surg. 2006. Mar-Apr;15(2):135-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.