Overview
Introduction
Malfunction of 1 of the 3 major nerves around the hip is a severe surgical complication of periacetabular osteotomy (PAO), and an understanding of the possible impacts of the different steps of the procedure on the nerves in their anatomic vicinity is essential to decrease the risk of these devastating injuries.
Step 1: Make a C-Shaped Skin Incision and Osteotomize the Anterior Superior Iliac Spine (ASIS) to Best Protect the LFCN (Video 1)
Protection of the LFCN depends on the incision and development of the approach.
Step 2: Do Not Transect the Psoas Tendon to Enable an Easier Approach to the Ischium and Pubis as It Protects the Femoral Nerve from Being Overstretched
Sectioning the psoas tendon can result in potentially damaging tensioning of the femoral nerve.
Step 3: Prevent Injury to the Sciatic Nerve While the Osteotomy of the Ischium Is Being Performed from Anterior
We perform the first ischial cut without direct visual control; fluoroscopy can be used to visualize the position of the osteotomy, but it will not completely eliminate the risk of sciatic nerve injury.
Step 4: Protect the Obturator Nerve During Osteotomy of the Pubis
The obturator nerve and vessels cross through the obturator foramen inferior to the superior pubic ramus close to the level of the pubic osteotomy; as the nerve is fixed by a membrane in close vicinity to the undersurface of the pubic bone, it may become injured during pubic osteotomy.
Step 5: Prevent Injury to the Sciatic Nerve During Supra-Acetabular and Posterior Column (Inside-Out Osteotomy) for Complete Ischial Separation
When performing the supra-acetabular osteotomy, the abductors should be tunneled on the lateral aspect of the pelvis, retracted, and protected by a blunt Hohmann retractor.
Step 6: Prevent Femoral Nerve Injuries Resulting from Acetabular Reorientation
Most femoral nerve lesions are caused by kinking and overstretching during large acetabular fragment displacement.
Step 7: Avoid Sciatic Nerve Injury During Fragment Reorientation
Similar to the femoral nerve, the sciatic nerve can potentially be kinked and/or stretched during large displacement of the acetabular fragment; it can also be lanced by a bone spike on the fragment.
Results
Approximately 800 PAOs were performed by the authors over a 9-year period beginning in 2007, when 2 of them started carrying out this procedure on their own (after several supervised operations).
Pitfalls & Challenges
Abstract
The Bernese periacetabular osteotomy (PAO) is a widely used procedure to reorient a dysplastic acetabulum resulting from developmental dysplasia of the hip, retroversion, protrusio, or some deformities with a traumatic etiology. Throughout the execution, the lateral femoral cutaneous nerve (LFCN) as well as the obturator, femoral, and sciatic nerves can be injured. Injury to 1 of the 3 major nerves is a devastating event for the patient followed by an ill-defined period of hope for nerve recovery and fear of lifelong disability. Surgical experience is an essential factor in reducing the prevalence of nerve injury, whereas proof of the value of intraoperative fluoroscopy and nerve monitoring still must be established. Although it is known that, for example, the ischial cuts of the complex osteotomy place the sciatic nerve at risk, the action causing the nerve injury is rarely clear in the individual situation. The literature has been mostly limited to reports of incidence and offers little analytic information.
Through the use of cadaveric dissections, we visualized the possible impacts of the different steps of the procedure on the nerves in their anatomic vicinity, and the present report demonstrates how nerves can be protected with retractor positioning and how lower-limb positioning can lead to nerve relaxation, an important means to avoid mechanical injury. While the frequent injuries of the LFCN are exclusively related to the approach, sciatic nerve injuries are mainly the result of the ischial osteotomy steps and femoral nerve injuries are seen nearly exclusively with the correction of the acetabular fragment. The authors implemented the demonstrated measures for 9 years, during which approximately 800 periacetabular osteotomies resulted in a total of 2 femoral and 2 sciatic nerve lesions—or a nerve injury rate of 0.5%. The nerves injuries resolved within 6 to 9 months in 3 hips, and 1 patient had a definitive foot drop requiring a splint at the time of writing.
Introduction
Malfunction of 1 of the 3 major nerves around the hip is a severe surgical complication of periacetabular osteotomy (PAO), and an understanding of the possible impacts of the different steps of the procedure on the nerves in their anatomic vicinity is essential to decrease the risk of these devastating injuries.
The PAO is a versatile surgical procedure for spatial correction of a number of acetabular and periacetabular deformities. Residual acetabular dysplasia is the main indication. A modified Smith-Petersen approach is preferred, and both the surgical approach and the 5 osteotomy cuts are performed in close vicinity to the lateral femoral cutaneous nerve (LFCN) and the femoral, obturator, and sciatic nerves (Video 1). The rate of injury to the LFCN is reported to be as high as 30%; however, the morbidity associated with such a lesion seems to be low1. The prevalence of major nerve injury has been mentioned to range from 0% to 15%, and this rather large range is assumed to be a result of the learning curve2. Previous reports of nerve injuries during PAO were mainly descriptive with little causative analysis1,3,4.
Video 1.
Performance of PAO.
Appreciation of the mechanisms leading to nerve damage during PAO is the key to reducing the risk of such an event. Therefore, we performed detailed cadaveric dissections to determine how the potential for nerve damage was affected by (1) the surgical approach, (2) the position and direction of the osteotomes as well as the lower-limb positions, and (3) the reorientation maneuver as well as the position of the reoriented fragment. Our dissections demonstrated that LFCN lesions are related to the modified Smith-Petersen approach, lesions of the obturator and sciatic nerves are sequelae of the osteotomy, and femoral nerve damage may occur during reorientation of the acetabular fragment. Precautions to avoid these injuries were tested and are described in the chronological order of the surgical steps of the procedure.
Step 1: Make a C-Shaped Skin Incision and Osteotomize the Anterior Superior Iliac Spine (ASIS) to Best Protect the LFCN (Video 1)
Protection of the LFCN depends on the incision and development of the approach.
Position the patient supine, and make a c-shaped incision with an average length of 20 cm. The c-shaped incision accounts for the course of the nerve proximal and distal to the ASIS. A bikini incision is cosmetically superior, but it might involve more stretching of the soft tissues, potentially placing the nerve at a higher risk for damage distal to the ASIS.
After sectioning the subcutaneous tissue, identify the fatty tissue band between the sartorius and tensor fasciae latae muscles; it contains the LFCN (Fig. 1).
Incise the fascial layer over the tensor muscle and mobilize the muscle laterally. A proximal branch of the LFCN crosses the tensor muscle, and therefore has to be sectioned, in 3 of 10 hips, a prevalence reflecting the approximately 30% rate of affected LFCN function reported at the time of follow-up after PAO1.
Osteotomize a 1.5-cm-long and 5-mm-deep fragment of the ASIS with the attached origin of the sartorius muscle and mobilize it medially together with the detached obliquus abdominis muscle and the subperiosteally detached iliacus muscle. Mobilize the resulting flap further medially and expose the interspinous ridge (Fig. 2).
Place a Hohmann retractor proximal and/or distal to the ASIS fragment for sufficient medialization of the flap. The LFCN is protected by the soft-tissue barrier consisting of the sartorius and iliacus muscles held together with the ASIS fragment (Fig. 2).
An approach without osteotomy of the ASIS brings the nerve in direct contact with the retractor, increasing the risk of kinking and overstretching (Fig. 3).
Place the extremity on a towel roll in 40° to 60° of hip flexion to reduce the tension on the medial flap (rectus femoris and sartorius muscles).
Fig. 1.
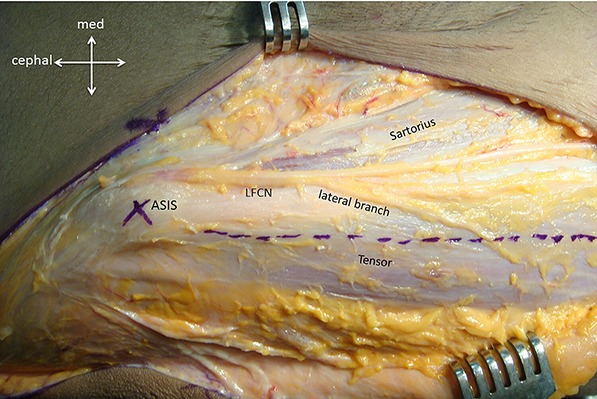
The extrapelvic part of the LFCN runs in a fatty tissue layer between the sartorius and tensor fasciae latae muscles directly under the subcutaneous fascia. It crosses the sartorius origin next to the ASIS. Incising the fascia over the tensor muscle (dotted line) and holding the muscle laterally offer the best protection of the main branch of the LFCN during the deeper approach distal to the ASIS. When present, the lateral branch has to be cut.
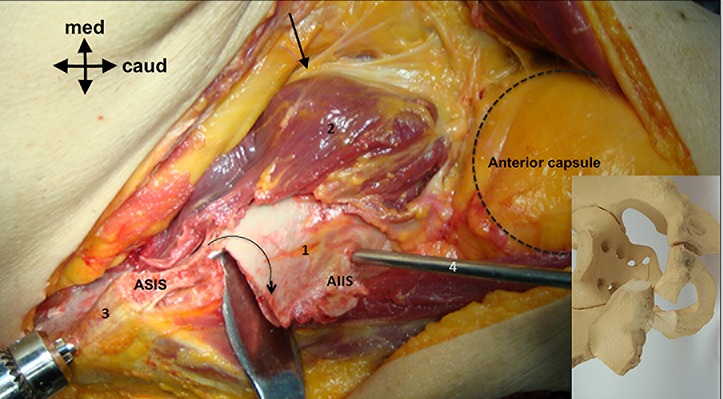
Fig. 2.
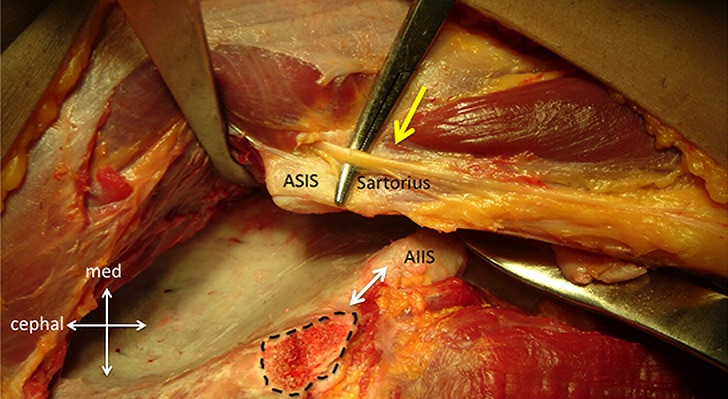
Osteotomy of the ASIS and subperiosteal detachment of the iliacus and obliquus abdominis muscles make it possible to build a strong superficial tissue barrier protecting the LFCN (yellow arrow) from being overstretched during retraction of the medial soft tissues. The dotted line surrounds the cut surface of the ASIS. The interspinous ridge is marked with a white double arrow. AIIS = anterior inferior iliac spine.
Fig. 3.
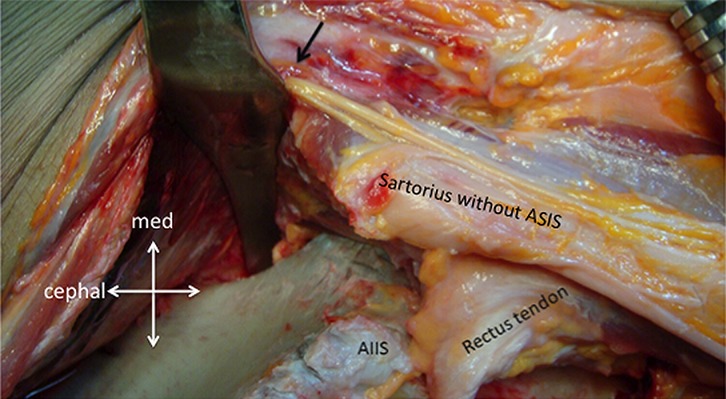
Without osteotomy of the ASIS the nerve is directly exposed to the edge of the retractor (black arrow) and may be overstretched. AIIS = anterior inferior iliac spine.
Step 2: Do Not Transect the Psoas Tendon to Enable an Easier Approach to the Ischium and Pubis as It Protects the Femoral Nerve from Being Overstretched
Sectioning the psoas tendon can result in potentially damaging tensioning of the femoral nerve.
To approach the ischium and expose the lateral part of the pubis, insert a sharp Hohmann retractor under the medial soft-tissue flap and impact it into the pubic bone about 2 to 2.5 cm medial to the iliopectineal eminence. This keeps the soft-tissue flap, including the psoas tendon, medially.
To place the spiked Hohmann retractor into the pubis, flex the hip to release tension from the medial soft tissues. Abduction and extension of the hip would increase the tension, while flexion, neutral rotation, and adduction will reduce it (Video 2).
Do not section the psoas tendon to facilitate the exposure. Although one might be tempted to do so, especially when the tendon is rather tight due to a Legg-Calvé-Perthes hip morphology, sectioning the psoas tendon can result in potentially damaging tensioning of the femoral nerve.
In a rectus-origin-sparing approach, there may be a risk of the most proximal branch of the femoral nerve being overstretched (Fig. 4). Surgeons using this approach should be aware of the vicinity to the first branch of the femoral nerve and avoid overstretching by maintaining constant hip flexion while also keeping in mind that hip flexion increases the tension of the sciatic nerve and therefore the risk of its injury during the first ischial cut.
Fig. 4.
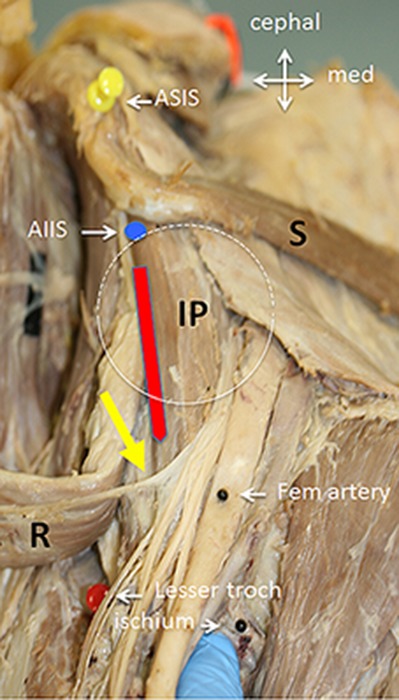
Topography of the rectus-origin-sparing approach (red line) between the iliopsoas (IP) and rectus femoris (R). The first branch of the femoral nerve (yellow arrow) reaches the undersurface of the rectus muscle at the level of the lesser trochanter (Less troch). S = sartorius muscle, ASIS (yellow pin) = anterior superior iliac spine, and AIIS (blue dot) = origin of the direct rectus tendon on the anterior inferior iliac spine. The white circle indicates the position of the joint. (Courtesy of Karl Grob, MD, HCARE KSSG St. Gallen, Switzerland.)
Video 2.
Retractors placed for exposure of the anteromedial pelvic surface and lateral pubic bone increase the tension of the femoral nerve when the hip is in full extension; flexion of the hip decreases the tension. Abduction of the flexed hip also produces nerve tension whereas adduction reduces it.
Step 3: Prevent Injury to the Sciatic Nerve While the Osteotomy of the Ischium Is Being Performed from Anterior
We perform the first ischial cut without direct visual control; fluoroscopy can be used to visualize the position of the osteotomy, but it will not completely eliminate the risk of sciatic nerve injury.
Direct the osteotome toward the contralateral shoulder to help avoid lateral perforation (Fig. 5). While the distance from the osteotomy to the inferior lip of the joint (Fig. 6) can be controlled by palpating the infracotyloid groove and inferior acetabular lip with instruments or fluoroscopy, it is more difficult to control the medial-lateral insertion. Lateral perforation with the osteotome must be avoided to prevent injury to the sciatic nerve (Fig. 7).
Use an osteotome with double rounded tips, which somewhat protects against direct catching and violation of the sciatic nerve (Figs. 8 and 9).
Keep the hip in flexion when placing the osteotome for the lateral part of the ischial osteotomy.
Before starting the osteotomy of the lateral aspect of the ischium, it is important to move the hip into full extension; this results in the least tension of the sciatic nerve, whereas any hip flexion will immediately increase nerve tension (Video 3). When the hip cannot be fully extended, nerve relaxation can be increased with additional knee flexion and further increased with additional hip abduction (Video 3). However, when full extension of the hip is possible it results in optimal relaxation of the nerve and additional flexion of the knee does little to increase nerve relaxation (Video 4).
Flexion of the hip also moves the sciatic nerve closer to the ischial osteotomy site, while the distance increases somewhat with hip abduction (Video 5).
Maintain the extended position with an assistant’s hand around the forefoot. This allows recognition of movement of the foot, which indicates a neuromuscular reaction.
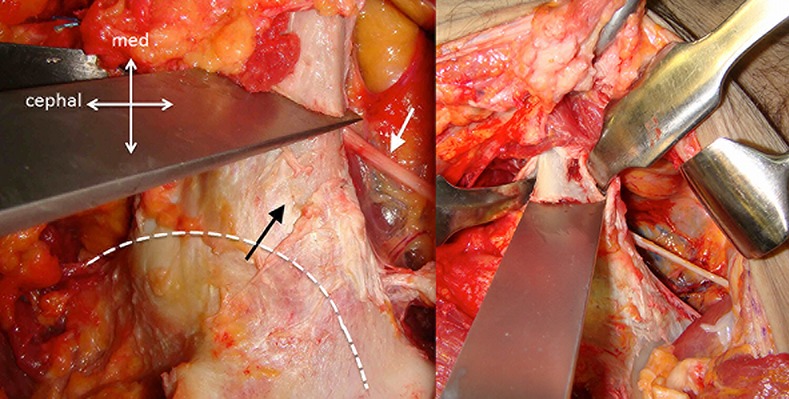
Fig. 5.
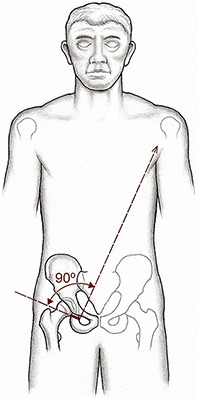
Orientation of the osteotome for the first, incomplete osteotomy of the ischium from anterior. It should be aligned toward the opposite shoulder of the patient to avoid penetration of the outer cortex and a risk of sciatic nerve violation.
Fig. 6.

The osteotome is inserted following the inferior aspect of the capsule and is placed distal to the osseous lip of the acetabulum at the infracotyloid groove, a topography that can be palpated with an instrument and/or verified with fluoroscopy. The first cut is made in the middle of the ischium and is followed by a more medial and a more lateral position.
Fig. 7.
Simulation of an osteotome position (black arrow) perforating the lateral (retroacetabular outer) cortex. With the hip in flexion, the sciatic nerve would be under tension and could be injured with further advancement of the osteotome. The dotted line indicates the position of the hip joint.
Fig. 8.

PAO osteotomes. 1 = 20-mm large osteotome with a 30° curve and no handle. It is used for the starting cut of the retroacetabular osteotomy at its supra-acetabular part. The same device without a curve can also be used. 2 = 20-mm large osteotome that is angulated 30° and has a handle and square shoulders. It was once applied for the first and last ischial cuts but is no longer in use. 3 = 20-mm large double-tipped osteotome with blunt edges that is angulated 30° at 40 mm from the cutting edge and has sloping shoulders. It is used for the inside-out cut of the retroacetabular osteotomy. 4 = 15-mm large double-tipped osteotome with blunt edges, a 30° curve, and no shoulders. The complete absence of shoulders prevents tethering. The osteotome is primarily used for the first ischial cut.
Fig. 9.
With the hip in extension, the relaxed sciatic nerve may escape an inaccurately aligned osteotome while the rounded edges of the osteotome may help further to prevent nerve injury.
Video 3.
An immediate and important increase in sciatic nerve tension occurs with hip flexion, modest relaxation of the nerve occurs with flexion of the knee while the hip is in a flexed position, and slightly more relaxation occurs with additional hip abduction.
Video 4.
Flexion of the knee while the hip is fully extended does not visibly increase sciatic nerve relaxation.
Video 5.
Flexion of the hip not only places the sciatic nerve under tension but also displaces it anteriorly and closer to the osteotomy level. Simultaneous rotation has little additional effect. The relaxing effect with abduction, as seen in Video 3, is overridden by the retractor holding away the nerve at the moment of abduction.
Step 4: Protect the Obturator Nerve During Osteotomy of the Pubis
The obturator nerve and vessels cross through the obturator foramen inferior to the superior pubic ramus close to the level of the pubic osteotomy; as the nerve is fixed by a membrane in close vicinity to the undersurface of the pubic bone, it may become injured during pubic osteotomy.
Bring the hip back into the flexed position. Place 2 curved, blunt Hohmann retractors subperiosteally around the pubis just medial to the iliopectineal eminence. Orient the retractors so that the obturator nerve and vessels are protected against the penetrating osteotome when cutting the contralateral cortex of the pubic bone. Use these retractors even when performing the osteotomy with an oscillating or Gigli saw (Fig. 10).
Perform a wedge cut of the ipsilateral cortex with an osteotome or oscillating saw to avoid unintended cracks when deepening the insertion of bulky osteotomes (Fig. 10).
Keep the instrument inclined 45° from anterolateral to posteromedial to ensure that the posterior pubic penetration is medial to the joint (Fig. 11, Video 6).
During the osteotomy, maintain constant observation to ensure that the retractors are placed exactly where the osteotome penetrates the contralateral cortex. Although it has not yet been reported as a complication of PAO in a published study (but has been occasionally seen after acetabular fracture fixation), an obturator nerve lesion can be a substantial problem that impairs active hip adduction.
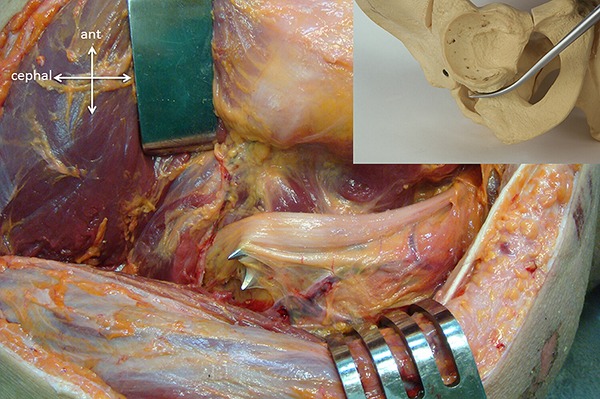
Fig. 10.
Protection of the neurovascular obturator bundle is ensured with 2 strictly subperiosteally placed blunt retractors. The white arrow points to the nerve, and the black arrow points to the vascular bundle. The dotted double line indicates the wedge cut of the ipsilateral cortex executed with an oscillating saw. This cut allows penetration of the osteotome without initiating fissures of the surrounding bone.
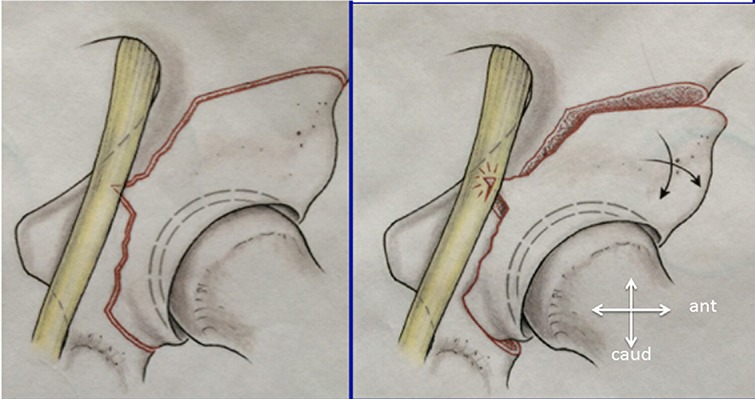
Fig. 11.
The starting point of the osteotomy is slightly medial to the iliopectineal eminence (black arrow). Vertical orientation of the osteotome (left image) may create a risk of articular penetration. Inclining the osteotome 45° (right image) allows avoidance of the joint and ends medial to the obturator nerve (white arrow in left image). The dotted line (left image) indicates the acetabular border.
Video 6.
Protection of the obturator neurovascular bundle during pubic osteotomy with the osteotome inclined 45° from anterolateral to posteromedial. Additional protection is provided with 2 subperiosteally placed Hohmann retractors with rounded tips.
Step 5: Prevent Injury to the Sciatic Nerve During Supra-Acetabular and Posterior Column (Inside-Out Osteotomy) for Complete Ischial Separation
When performing the supra-acetabular osteotomy, the abductors should be tunneled on the lateral aspect of the pelvis, retracted, and protected by a blunt Hohmann retractor.
Elevate the soft tissues from the ilium for the dissection of the abductors with the hip extended and abducted to avoid damage to the sciatic nerve. After the supra-acetabular osteotomy, which is usually performed with an oscillating saw with the blunt Hohmann retractor protecting the soft tissues, the inside-out completion of the ischial separation is executed without visual control; therefore, there is a risk of sciatic nerve injury.
Keep the hip flexed for placement of the osteotome. Fluoroscopy can help to control the starting point and direction of the cut but is less reliable for controlling advancement in the bone and perforation of the outer cortex.
Relax the nerve again as described in Step 3 (Videos 3, 4, and 5).
A change in the sound of the hammer blows advancing the curved osteotome indicates when the lateral cortex has been perforated and advancement of the osteotome must stop; the point when the advancement must stop can vary according to bone quality. The area at risk for the sciatic nerve is around the gemellus inferior (Fig. 12). Therefore, gentle advancement of the osteotome through the rather narrow bone of the posterior column is recommended.
Use an osteotome with double rounded tips to further reduce the risk of catching the nerve (Fig. 13).
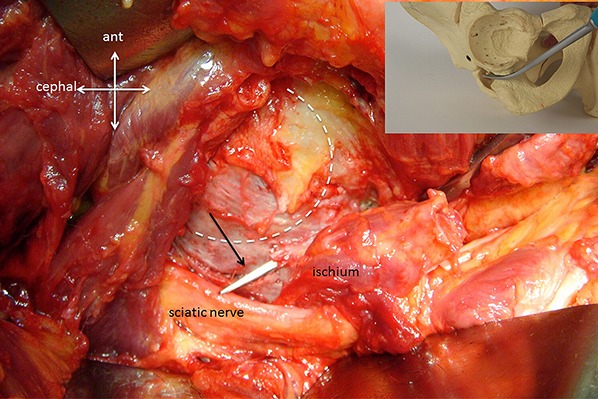
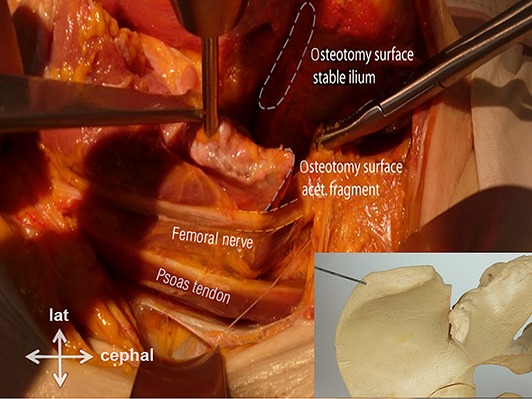
Fig. 12.
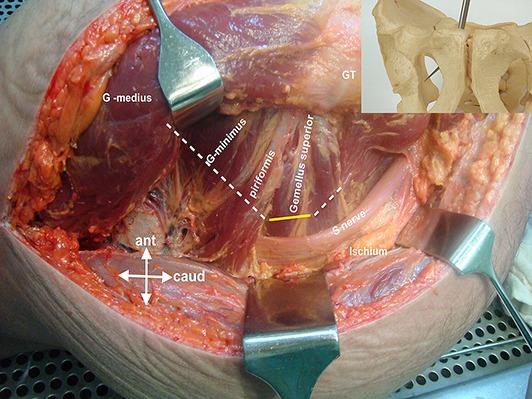
The yellow line indicates the area of retroacetabular bone to be separated with an inside-out osteotomy. It combines the retroacetabular cut with the first incomplete ischial cut (dotted lines). The distance of the bone to be cut is rather short, and the diameter at this level is rather small. A change in the sound of the hammer blows indicates lateral perforation by the osteotome. GT = greater trochanter.
Fig. 13.
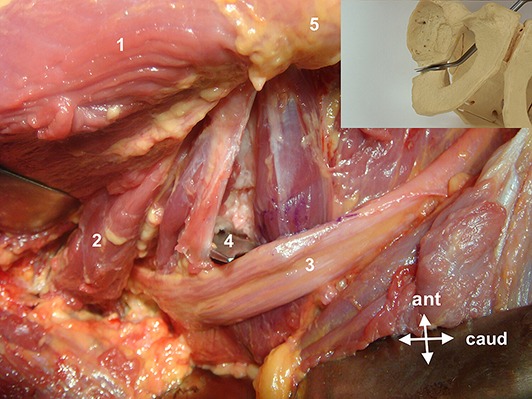
Further advancement of the osteotome after lateral perforation should be strictly avoided. Protection of the nerve by the external rotators is minimal. The best protection is relaxation of the sciatic nerve with full hip extension and some abduction. The rounded edges of the osteotome help to avoid lancing of the nerve. 1 = gluteus medius, 2 = piriformis, 3 = sciatic nerve, 4 = bifid osteotome, and 5 = greater trochanter.
Step 6: Prevent Femoral Nerve Injuries Resulting from Acetabular Reorientation
Most femoral nerve lesions are caused by kinking and overstretching during large acetabular fragment displacement.
Nerve injuries are due to large corrections achieving fragment anteversion.
The injury may have a delayed presentation after a short symptom-free interval.
The large corrections causing these injuries are needed in a deep socket with a negative roof angle and in extremely retroverted hips (iatrogenic) or lateralized hips (posttraumatic dysplasia) (Figs. 14 and 15)5.
If hinge-free fragment mobilization cannot be achieved despite careful osteotomies, the superior edge of the fragment may be resected to reduce the tension of the nerve.
Do not transect the psoas tendon, as it protects the femoral nerve by reducing the bulging of the iliacus muscle (Video 2), which is seen especially with anterior fragment rotation—for example, to correct an extreme, mainly iatrogenic retroversion (Fig. 16).
Large medial displacement of the acetabular fragment as required for extremely retroverted hips (iatrogenic) or lateralized hips (posttraumatic dysplasia)6,7 can also lead to stretching of the femoral nerve. Keep the hip in a flexed position during the initial postoperative period. Allowing only gradual extension might be helpful in the initial postoperative period.
Watch for a large gap at the pubic osteotomy site, in which the psoas tendon and even the femoral nerve can be trapped (Fig. 17). Check for such a gap before wound closure and, if found, fill it with a solid bone graft from the iliac crest.
Fig. 14.
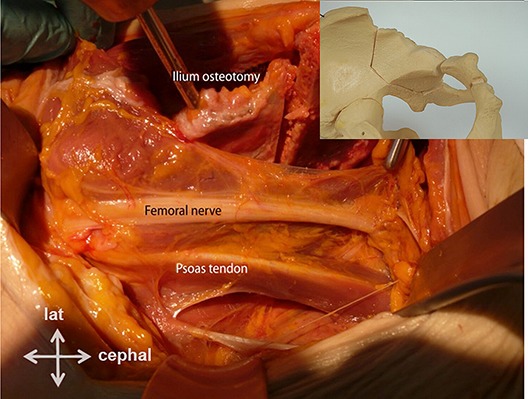
View of the inside of the iliopsoas muscle with the femoral nerve in a left hip. All osteotomies have been executed, but the acetabular fragment has not yet been corrected.
Fig. 15.
Same specimen as in Figure 14. Large medial displacement at the proximal fragment end can result from a hinge near the infracotyloid groove. It may lead to kinking of the femoral nerve at the fragment edge, which will be increased with full extension of the hip.
Fig. 16.
With large anterior (and, to a lesser degree, posterior) rotation of the acetabulum (curved arrow), the rising pubic end of the fragment leads to a ventral lift of the femoral nerve (straight arrow), especially when additional lateral coverage has to be performed. Full hip extension may lead to intolerable stretching of the nerve. Massive medial fragment displacement as necessary in posttraumatic dysplasia may be followed by a similar adverse translation of the nerve. 1 = acetabular fragment, 2 = iliacus muscle, 3 = iliac crest, 4 = Schanz screw, and AIIS = anterior inferior iliac spine.
Fig. 17.
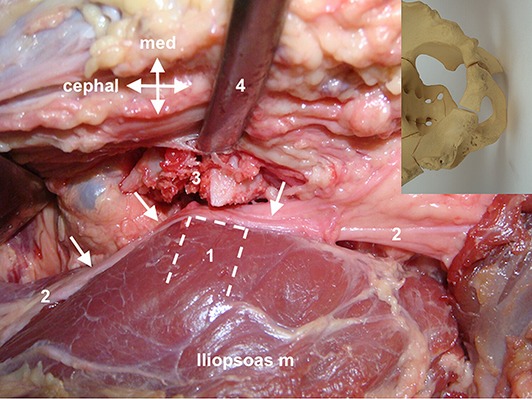
Large diastasis or fragmentation at the pubic osteotomy site may allow not only the psoas tendon but also the femoral nerve to get caught. 1 (dotted line) = pubic end of the acetabulum, 2 (arrows) = femoral nerve, 3 = fragmentation of the medial pubis near the osteotomy site due to avulsion by the spiked Hohmann retractor, and 4 = instrument retracting the medial soft tissue.
Step 7: Avoid Sciatic Nerve Injury During Fragment Reorientation
Similar to the femoral nerve, the sciatic nerve can potentially be kinked and/or stretched during large displacement of the acetabular fragment; it can also be lanced by a bone spike on the fragment.
Control whether the legs of the supra-acetabular and retroacetabular osteotomies meet at the lateral cortex. During fragment mobilization, a remaining osseous bridge due to an incomplete osteotomy may create a spike on the acetabular fragment; during repositioning maneuvers, it may tent and eventually lance the sciatic nerve (Fig. 18). This complication has been reported8.
Routinely check the outer edge of the fragment before reorientation and, if there is a spike, resect it. Visual control of the edges of the osteotomy site at the meeting point of the supra-acetabular and retroacetabular osteotomies and of the proximal part of the retroacetabular osteotomy is possible by widening either gap using a lamina spreader. With abduction of the extended lower limb, the acetabular fragment can be manipulated using an inserted Schanz screw. With a blunt retractor placed along the outer osteotomy border and the use of a periosteal elevator, the osteotomy site can be examined distally almost to the level of the infracotyloid groove. Sharp-edged bone spikes are most likely on the acetabular fragment and should be resected using a small but sharp osteotome; fragments should be retrieved, avoiding blind poking within the soft tissues.
As the nerve follows the osteotomized fragment, large medial displacement of the acetabular fragment might cause it to be kinked over the posterosuperior edge of the stable ilium (Fig. 19), although so far this has only been observed during cadaver dissections9. Control the tension of the abductor musculature, which might be increased (especially with adduction of the lower limb). Keep the lower limb in abduction for several days postoperatively.
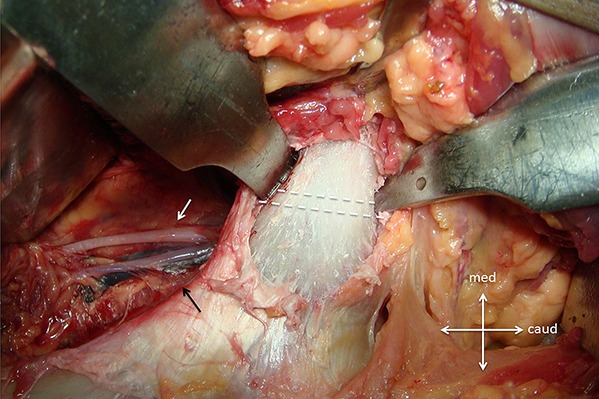
Fig. 18.
A lateral bone spike on the acetabular fragment may pierce the sciatic nerve during corrective manipulations.
Fig. 19.
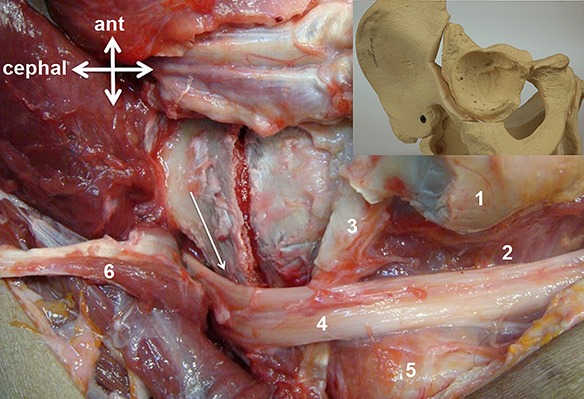
Showing kinking of the sciatic nerve over the edge of the stable ilium (arrow) with substantial medial shifting of the acetabular fragment. 1 = greater trochanter, 2 = quadratus femoris, 3 = obturator externus, 4 = sciatic nerve, 5 = ischium, and 6 = reflected piriformis.
Results
Approximately 800 PAOs were performed by the authors over a 9-year period beginning in 2007, when 2 of them started carrying out this procedure on their own (after several supervised operations). These procedures led to a total of 2 lesions of the sciatic nerve and 2 of the femoral nerve, corresponding to a nerve injury rate of 0.5%. In 3 hips, nerve function was fully recovered within 6 to 9 months. One patient had a definitive foot drop requiring a splint at the time of writing.
The senior author was actively involved in about 40 PAOs per year since 1984, about one-third of which were complex surgical procedures combining femoral and acetabular corrections or revisions. His last case with a sciatic nerve lesion dates back to 2003 and occurred in a hip that had undergone several prior operations, including a pelvic triple osteotomy. Unfortunately, the nerve did not recover substantially over time. His last case with femoral nerve injury occurred 2 years later in a hip with a deep socket and a marked negative roof angle; major medial displacement of the proximal part of the acetabular fragment was established to achieve a neutral roof angle. The nerve injury fully resolved within 9 months. This case prompted cadaver dissections to study the pathomorphological correlations (Figs. 14 and 15). The insights were applied to the surgery on the contralateral hip, resulting in a better correction without damage of the femoral nerve.
Pitfalls & Challenges
Appreciate size differences, particularly for small or large pelvic anatomies. The resulting dimensional changes necessitate spatial adaptation of the surgical activities.
Appreciate femoral offset changes as found in both coxa valga and coxa vara. In coxa valga, the first ischial cut must be performed from an anteromedial to posterolateral direction to circumvent the medially protruding calcar, and this direction is dangerous for the sciatic nerve. Abduct the lower limb to move the calcar more laterally; this maneuver also creates some additional nerve relaxation. On the other hand, increased offset in coxa vara might allow the osteotome to be directed lateral to the ischium, a direction that is also dangerous to the sciatic nerve.
When the PAO is combined with a femoral correction, start with the femoral surgery with the patient in lateral decubitus and perform the first ischial cut through the lateral approach with the possibility of visual control of the sciatic nerve10. Identification and mobilization of the sciatic nerve are technically easier when the ischial osteotomy is done immediately after the trochanteric flip and before working on the femur. Draping can be done in such a way that moving the patient into a supine position is possible without redraping.
When a repeat PAO is being done, carefully evaluate the previous surgery including the approach. Magnetic resonance imaging (MRI) might be advisable to identify substantial scarring of the surrounding soft tissue. If there is scarring at the posterior column, a revision of the sciatic nerve with the patient in lateral decubitus and performance of the ischial osteotomy through a lateral approach should be considered. The remaining osteotomies can be performed through the Smith-Petersen approach.
Revision of a sciatic nerve that has been previously damaged is almost mandatory. The nerve might be trapped in the scar and therefore less mobile and either directly damaged or stretched during the procedure.
When there is a postoperative neurological deficit, advanced imaging should be done as early as possible. Either MRI or computed tomography (CT) can identify soft-tissue and osseous alteration. A hematoma or bone spike around the nerve may require immediate revision surgery.
Proceed in a similar fashion whenever there is a neurological deficit, even if it became evident after a preliminary postoperative period of normal function8.
Clinical Comments
Major nerve injuries with PAO are apparently not rare during the early phase of the learning curve, whereas the prevalence drops to about 2% among experienced surgeons2. However, retrospective data collection may result in the underreporting of nerve injuries during PAO. More accurate data are to be expected with prospective collection using a specifically designed form, which should be eventually expanded with an algorithm for evaluation and treatment of such complications. For affected patients, such a nerve injury is a terrifying experience with uncertainty about whether they will have full, partial, or no recovery. Efforts to further reduce the prevalence of such injuries are required, particularly as this procedure becomes increasingly popular. Modifications in the approach and assisting techniques may have an influence on how to implement such efforts. In contrast to others, we do not use fluoroscopy on a regular basis throughout the procedure. For the first ischial cut, we rely on instrument palpation of the bone and use a 15-mm large double-tipped osteotome, starting in the middle of the transverse diameter; a second, coequal cut separates the strong medial cortex whereas a third, more lateral cut incises only the surface of the bone. We also do not use intraoperative nerve monitoring, the predictive value of which is questionable. The number of nerve lesions caused by acetabular fracture treatment has been reported to be similar regardless of whether monitoring was used11. Neuromonitoring during PAO could record the moment when and the maneuver during which nerve injury occurred, but it was ineffective as a preventive measure in a previous study12. However, it might help surgeons to avoid stretching-induced nerve damage during fragment reorientation, especially when large corrections are necessary and during revision PAO. Finally, we do not use epidural anesthesia for postoperative pain management, as doing so could mask an eventual nerve deficit and delay its treatment.
In conclusion, cadaveric dissections allow a better understanding of the topography and pathomechanisms of nerve injuries during PAO as well as the opportunity to test options for prophylaxis. Videos can show how lower-limb positions can relax or tighten a nerve and how retractors can protect nerves, helping to reduce the risk of injury. It is especially important to protect the sciatic nerve, as it is the most frequently injured. Better knowledge will have a positive effect on the learning curve, although it needs to be stated that a dissected cadaveric nerve is probably more mobile than a nerve in a living patient. Moreover, simulation involves simplifying and cannot cover all possible variants of risk during the approach and technical execution of the procedure. Providing a hip position that results in the greatest nerve relaxation during execution of the osteotomy step is efficient prophylaxis against nerve damage.
Footnotes
Published outcomes of this procedure can be found at: Bone Joint J. 2015 May;97-B(5):636-41.
Disclosure: The authors indicated that no external funding was received for any aspect of this work. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJSEST/A194).
References
- 1. Hussell JG, Rodriguez JA, Ganz R. Technical complications of the Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999. June;(363):81-92. [PubMed] [Google Scholar]
- 2. Sierra RJ, Beaule P, Zaltz I, Millis MB, Clohisy JC, Trousdale RT; ANCHOR group. Prevention of nerve injury after periacetabular osteotomy. Clin Orthop Relat Res. 2012. August;470(8):2209-19. Epub 2012 Jun 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Davey JP, Santore RF. Complications of periacetabular osteotomy. Clin Orthop Relat Res. 1999. June;(363):33-7. [PubMed] [Google Scholar]
- 4. Thawrani D, Sucato DJ, Podeszwa DA, DeLaRocha A. Complications associated with the Bernese periacetabular osteotomy for hip dysplasia in adolescents. J Bone Joint Surg Am. 2010. July 21;92(8):1707-14. [DOI] [PubMed] [Google Scholar]
- 5. Leunig M, Nho SJ, Turchetto L, Ganz R. Protrusio acetabuli: new insights and experience with joint preservation. Clin Orthop Relat Res. 2009. September;467(9):2241-50. Epub 2009 May 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dora C, Zurbach J, Hersche O, Ganz R. Pathomorphologic characteristics of posttraumatic acetabular dysplasia. J Orthop Trauma. 2000. Sep-Oct;14(7):483-9. [DOI] [PubMed] [Google Scholar]
- 7. Dora C, Ganz R. Correction of posttraumatic acetabular dysplasia. In: Marti RK, van Heerwarden RJ, editors. Osteotomies for posttraumatic deformities. Switzerland: AO Publishing; 2008. p. 261-7. [Google Scholar]
- 8. Leunig M, Vigdorchik JM, Pour AE, Willi-Dähn S, Ganz R. Delayed-onset sciatic nerve palsy after periacetabular osteotomy: a case report. JBJS Case Connect. 2017. Jan-Mar;7(1):e9. [DOI] [PubMed] [Google Scholar]
- 9. Kalhor M, Gharehdaghi J, Schoeniger R, Ganz R. Reducing the risk of nerve injury during Bernese periacetabular osteotomy: a cadaveric study. Bone Joint J. 2015. May;97-B(5):636-41. [DOI] [PubMed] [Google Scholar]
- 10. Ganz R, Huff TW, Leunig M. Extended retinacular soft-tissue flap for intra-articular hip surgery: surgical technique, indications, and results of application. Instr Course Lect. 2009;58:241-55. [PubMed] [Google Scholar]
- 11. Haidukewych GJ, Scaduto J, Herscovici D, Jr, Sanders RW, DiPasquale T. Iatrogenic nerve injury in acetabular fracture surgery: a comparison of monitored and unmonitored procedures. J Orthop Trauma. 2002. May;16(5):297-301. [DOI] [PubMed] [Google Scholar]
- 12. Pring ME, Trousdale RT, Cabanela ME, Harper CM. Intraoperative electromyographic monitoring during periacetabular osteotomy. Clin Orthop Relat Res. 2002. July;(400):158-64. [DOI] [PubMed] [Google Scholar]


