Overview
Introduction
The posterolateral approach for trimalleolar fractures leads to an adequate view of the posterior fragment, allows removal of loose intra-articular fragments, and results in anatomical reduction and sound fixation.
Indications & Contraindications
Step 1: Position and Incision (Figs. 1, 2, and 3 and Video 1)
Perform an incision between the lateral border of the Achilles tendon and the posteromedial border of the fibula.
Step 2: Exposure of the Fibular Fracture (Figs. 4 and 5 and Video 2)
Expose the fibula through an interval lateral to the peroneal muscle.
Step 3: Exposure of the Posterior Fragment (Figs. 6, 7, and 8 and Video 3)
Expose the posterior fragment through an interval medial to the peroneal muscle.
Step 4: Open Reduction and Internal Fixation (ORIF) of the Fibular Fracture (Fig. 9)
Perform ORIF of the fibular fracture.
Step 5: ORIF of the Posterior Fragment (Fig. 10 and Video 4)
Perform ORIF of the posterior fracture.
Step 6: ORIF of the Medial Fracture (Fig. 11)
Perform ORIF of the medial fracture.
Step 7: Final Fluoroscopic Control and Closure (Fig. 12)
Use final fluoroscopic control to confirm anatomical reduction of the fractures, joint congruency, and the correct position of the screws, and close the wounds.
Results
The recently published literature suggests that ORIF of the posterior fragment of trimalleolar fractures through a posterolateral approach is gaining popularity among orthopaedic trauma surgeons1-3.
Pitfalls & Challenges
Background:
Fixation of the posterior fragment in trimalleolar fractures remains a matter of debate. Recent studies have shown that a persistent step-off in the tibiotalar joint is the most important factor in the development of osteoarthritis and therefore the functional outcome. The disadvantages of the regularly performed indirect reduction by ligamentotaxis or percutaneous reduction followed by percutaneous screw fixation of the posterior fragment in an anterior-to-posterior direction are that an anatomical reduction is more difficult to achieve because of the interposition of soft tissue or loose osseous fragments, it is hard to assess reduction satisfactorily using an image intensifier, and fixation of small or comminuted fragments is technically difficult. Therefore, we favor an open, anatomical reduction of the posterior malleolar fragment using a posterolateral approach.
Description:
The patient is prone for the operation. A longitudinal incision is made between the lateral border of the Achilles tendon and the posteromedial border of the fibula. The posterior aspect of the fibula is easily reached through the interval just lateral to the peroneal muscle. After debridement of the fracture, it can be reduced and is fixed with either (1) a buttress plate or (2) lag screw(s) with a neutralizing plate. The belly of the flexor hallucis longus is bluntly dissected off of the interosseous membrane and the lateral side of the tibia through the interval medial to the peroneal muscle. Retracting the muscle belly medially allows the posterior aspect of the tibia to be seen. The periosteum is incised to expose the posterior malleolar fracture. Loose fragments can be removed by levering the posterior fragment distally. Reduction is performed and is held temporarily by Kirschner wires. Fixation is undertaken using either lag screws or a slightly prebent 3-hole buttress plate. Placement of a lag screw through the most distal hole of the plate can help to close any possible gaps. Slight internal rotation of the lower leg allows the medial malleolus to be approached and fixed.
Alternatives:
Percutaneous anterior-to-posterior screw fixation is an alternative, but it frequently leads to a nonanatomical reduction of the fragment.
Rationale:
This technique provides an adequate view of the fracture, an anatomical reduction in most cases, and sound fixation of the posterior malleolar fragment. Other advantages are that small fragments are easier to fix and small intra-articular fragments can be removed from the site of the fracture.
Introductory Statement
The posterolateral approach for trimalleolar fractures leads to an adequate view of the posterior fragment, allows removal of loose intra-articular fragments, and results in anatomical reduction and sound fixation.
Indications & Contraindications
Indications
Trimalleolar fracture.
Isolated posterior malleolar fracture.
Posterior fragment of a tibial pilon fracture.
Contraindications
Very small posterior fragment. Always obtain a computed tomography (CT) scan because radiographs tend to underestimate the size and comminution of the posterior fragment. Fixation of fragments that involve less than 5% to 10% of the articular surface is technically demanding, with the possibility that they will be crushed by the screws or plate.
Patient for whom the prone position is not suitable.
Step 1: Position and Incision (Figs. 1, 2, and 3 and Video 1)
Fig. 1.

Anteroposterior and lateral radiographs showing a trimalleolar fracture. The posterior fragment involves 10% of the articular surface, and there is a loose fragment.
Fig. 2.

A patient in the prone position with the knee slightly flexed and a tourniquet applied.
Fig. 3.

Outline of a longitudinal incision midway between the Achilles tendon and the posteromedial border of the fibula.
Perform an incision between the lateral border of the Achilles tendon and the posteromedial border of the fibula.
Position the patient prone for the operation.
Place the distal part of the lower leg on a foam cushion with the knee slightly flexed to allow maximal dorsiflexion of the ankle during reduction.
Apply a tourniquet to the thigh (if that is your preference).
Identify the Achilles tendon, the fibula, and the level of the fibular fracture.
Outline a longitudinal incision midway between the Achilles tendon and the posteromedial border of the fibula, from approximately the distal tip of the fibula to 1 in (2.5 cm) proximal to the fibular fracture.
Cut the skin with a scalpel.
Video 1.
Patient positioning and skin incision.
Step 2: Exposure of the Fibular Fracture (Figs. 4 and 5 and Video 2)
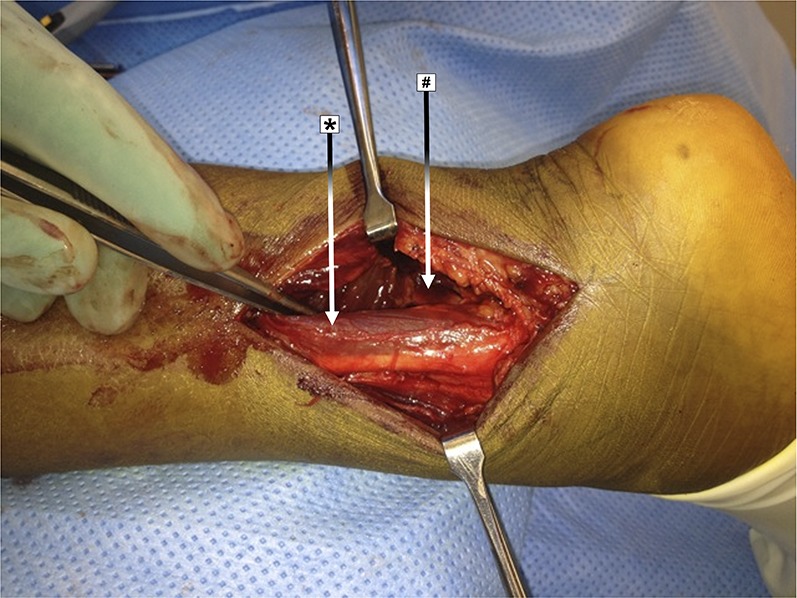
Fig. 4.

Incision of the skin and subcutaneous tissue, exposing the peroneal muscle (*).
Fig. 5.

Exposure of the fibular fracture (#). * = peroneal muscle.
Expose the fibula through an interval lateral to the peroneal muscle.
Perform a blunt subcutaneous dissection onto the peroneal muscle, taking care to avoid injury to the sural nerve.
Reach the posterior aspect of the fibula through the interval just lateral to the peroneal muscle.
For more distal fibular fractures it is occasionally necessary to incise the proximal part of the superior peroneal retinaculum for optimal placement of a (buttress) plate. Do not dissect the retinaculum completely to avoid peroneal muscle subluxation.
Expose and debride the fibular fracture.
Video 2.
Exposure of the fibular fracture.
Step 3: Exposure of the Posterior Fragment (Figs. 6, 7, and 8 and Video 3)
Fig. 6.
Development of the interval medial to the peroneal muscle (*). # = flexor hallucis longus muscle belly.
Fig. 7.

Exposure of the posterior fragment (+). * = peroneal muscle and # = flexor hallucis longus muscle belly.
Fig. 8.

Lifting of the posterior fragment (+) with a dental pick and removal of loose fragments (^). * = peroneal muscle and # = flexor hallucis longus muscle belly.
Expose the posterior fragment through an interval medial to the peroneal muscle.
Open the interval medial to the peroneal muscle.
Bluntly dissect the belly of the flexor hallucis longus off of the interosseous membrane and the lateral side of the tibia, taking particular care to avoid injury to the peroneal artery and its smaller branches.
Visualize the posterior aspect of the tibia by retracting the muscle belly medially with use of Langenbeck or Hohmann retractors.
Incise the periosteum to expose the posterior malleolar fracture. It is important not to damage the posterior inferior tibiofibular ligament at this stage.
Video 3.
Exposure of the posterior fragment.
Step 4: Open Reduction and Internal Fixation (ORIF) of the Fibular Fracture (Fig. 9)
Fig. 9.

Lag screw fixation of the fibular fracture.
Perform ORIF of the fibular fracture.
Debride the fibular fracture.
Perform an open reduction with a clamp.
Fix the fracture with either (1) a buttress plate or (2) lag screw(s) with a neutralizing plate. Occasionally, in selected young patients with a simple spiral fracture, the fixation is performed with 2 lag screws alone.
Step 5: ORIF of the Posterior Fragment (Fig. 10 and Video 4)
Fig. 10.

Reduction of the posterior fragment with temporary Kirschner wire fixation, followed by insertion of a buttress plate and a lag screw through the plate.
Perform ORIF of the posterior fracture.
Lift the posterior fragment with an elevator.
Remove loose fragments that are intra-articular or blocking adequate reduction.
After maximal dorsiflexion of the ankle, the fragment will reduce by ligamentotaxis. More reduction can be achieved by pushing with a bone tamp or using a dental pick.
Place temporary Kirschner wires to hold the reduction.
Confirm anatomical reduction with image intensification in 2 planes.
Fix the posterior fragment using either lag screws or a slightly prebent 3-hole buttress plate. Placement of a lag screw through the most distal hole of the plate can help to close any possible gaps. A plate is biomechanically superior to lag screws alone because it serves as a strong buttress. Moreover, screws have the tendency to countersink in the soft metaphyseal cortex. Disadvantages of plate fixation are protrusion of the very distal part of the plate if it is not prebent anatomically and postoperative adhesions of the flexor hallucis longus muscle belly. Therefore, it is preferable to use only lag screws with washers, but if there is any doubt about the strength of this fixation use a plate. If loose fragments are removed, it is important not to overcompress the fracture, which may occur if you completely close the resultant “gap.”
Video 4.
Fixation of the posterior fragment.
Step 6: ORIF of the Medial Fracture (Fig. 11)
Fig. 11.

Exposure of the medial fracture.
Perform ORIF of the medial fracture.
Slightly internally rotate the lower leg.
Perform a regular approach to the medial malleolus.
Perform ORIF of the medial fracture.
Step 7: Final Fluoroscopic Control and Closure (Fig. 12)
Fig. 12.

Final fluoroscopic control before closure.
Use final fluoroscopic control to confirm anatomical reduction of the fractures, joint congruency, and the correct position of the screws, and close the wounds.
Use fluoroscopic control to confirm anatomical reduction of the fractures, joint congruency, and the correct position of the screws (especially no penetration of the joint).
For fibular fractures proximal to the syndesmoses, accurate intraoperative testing of syndesmotic stability is necessary to prevent widening of the ankle joint postoperatively. If there is any doubt, place a syndesmotic screw.
Close all wounds. Handle the skin in a delicate manner to reduce the risk of wound complications.
Apply a bandage or splint, according to your preference.
Results
The recently published literature suggests that ORIF of the posterior fragment of trimalleolar fractures through a posterolateral approach is gaining popularity among orthopaedic trauma surgeons1-3. Although I am not aware of any study comparing anterior-to-posterior percutaneous screw placement with ORIF through a posterolateral approach, the advantages of the latter seem clear because persistent step-off occurred in 23% to 42% of patients after percutaneous fixation4,5. Whether it is better to fix the fracture fragment with screws or a buttress plate has not been determined, and the outcomes do not appear to differ significantly in the sparse literature6.
Several authors described their experience in terms of complications and outcomes with ORIF through a posterolateral approach for trimalleolar fractures1-3. Forberger et al. used the AAOS (American Academy of Orthopaedic Surgeons) Foot and Ankle Questionnaire and postoperative radiographs to review the cases of 45 patients in whom a trimalleolar fracture had been treated with ORIF through a posterolateral approach3. The indication to fix the posterior fragment was involvement of >25% of the articular surface or involvement of >10% in combination with persistent subluxation in patients younger than 50 years old. Postoperative skin problems occurred in 5 patients (11%), and 2 patients (4%) developed complex regional pain syndrome3. In the largest study of which I am aware, Little et al. reviewed the results of the posterolateral approach to 112 ankle fractures, 71 of which were treated with posterior malleolar fixation and 41 (without a posterior malleolar fracture) of which underwent fixation of the fibular fracture2. Postoperative wound infection developed in 5 patients, 2 of whom required implant removal after the fracture had healed, and 1 superficial peroneal nerve injury was documented. In the most recent study, Verhage et al. described a series of 52 patients who underwent ORIF of the posterior fragment through a posterolateral approach1. The mean posterior fragment size was 27% of the articular surface. A buttress plate was used in 40 patients, and only lag screws were employed in 12. Reduction was anatomical in all patients, with a residual step-off at the articular surface of ≤1 mm. Complications comprised a wound infection in 1 patient and temporary numbness of the superficial peroneal cutaneous nerve area in 2.
Gardner et al. described the advantages of syndesmotic stabilization through the fixation of the posterior malleolar fragment in AO 44-C fractures7. Verhage et al. reported that, in 9 of 11 AO 44-C fractures in their study, the syndesmosis was stable after fixation of the posterior fragment and a syndesmosis screw was not needed1. Similarly, Miller et al. found that the functional outcomes of fixation of the posterior malleolus alone were at least equivalent to the outcomes of fixation with syndesmotic positioning screws in a prospectively followed series of 31 AO 44-C fractures, including 17 posterior fractures8.
Pitfalls & Challenges
Fixation of the fibular fracture before fixation of the posterior malleolar fracture has advantages and disadvantages. Fixing the fibula first will, in some cases, facilitate an adequate reduction of the posterior malleolar fracture, but sometimes it will limit the movement of the posterior malleolar fracture and therefore interfere with reduction. In my opinion, the best strategy is to dissect and perform careful anatomical reduction of both fractures, with the choice of which fracture to fix first made on a case-by-case basis.
Fixation of the fibular fracture before addressing the posterior fragment may make it difficult to confirm adequate reduction of the posterior fragment on lateral fluoroscopic imaging because of the radiopaque plate.
Exposure of the medial malleolus with the patient in the prone position may be more challenging than performing such an exposure with the patient in the supine position.
ORIF of fragments on the anterior side (Tillaux or Wagstaffe fractures) is very difficult in a prone patient. In selected cases, it is advisable to first perform an ORIF of the fibular fracture and posterior fragment with the patient prone and follow this with a percutaneous or open reduction of the ventral avulsion fragments with the patient supine.
In fibular fractures proximal to the syndesmoses (pronation-external rotation fractures), fixation of the posterior fragment frequently stabilizes the syndesmosis without placement of syndesmotic positioning screws. However, accurate intraoperative testing of syndesmotic stability is necessary to prevent widening of the ankle joint after the operation. If there is doubt, syndesmotic screws should be placed.
Footnotes
Published outcomes of this procedure can be found at: Bone Joint J. 2016 Jun;98-B(6):812-7.
Disclosure: The author indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest form is provided with the online version of the article (http://links.lww.com/JBJSEST/A191).
References
- 1. Verhage SM, Boot F, Schipper IB, Hoogendoorn JM. Open reduction and internal fixation of posterior malleolar fractures using the posterolateral approach. Bone Joint J. 2016. June;98-B(6):812-7. [DOI] [PubMed] [Google Scholar]
- 2. Little MT, Berkes MB, Lazaro LE, Sculco PK, Helfet DL, Lorich DG. Complications following treatment of supination external rotation ankle fractures through the posterolateral approach. Foot Ankle Int. 2013. April;34(4):523-9. Epub 2013 Feb 27. [DOI] [PubMed] [Google Scholar]
- 3. Forberger J, Sabandal PV, Dietrich M, Gralla J, Lattmann T, Platz A. Posterolateral approach to the displaced posterior malleolus: functional outcome and local morbidity. Foot Ankle Int. 2009. April;30(4):309-14. [DOI] [PubMed] [Google Scholar]
- 4. Drijfhout van Hooff CC, Verhage SM, Hoogendoorn JM. Influence of fragment size and postoperative joint congruency on long-term outcome of posterior malleolar fractures. Foot Ankle Int. 2015. June;36(6):673-8. Epub 2015 Feb 11. [DOI] [PubMed] [Google Scholar]
- 5. Xu HL, Li X, Zhang DY, Fu ZG, Wang TB, Zhang PX, Jiang BG, Shen HL, Wang G, Wang GL, Wu XB. A retrospective study of posterior malleolus fractures. Int Orthop. 2012. September;36(9):1929-36. Epub 2012 Jul 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Erdem MN, Erken HY, Burc H, Saka G, Korkmaz MF, Aydogan M. Comparison of lag screw versus buttress plate fixation of posterior malleolar fractures. Foot Ankle Int. 2014. October;35(10):1022-30. Epub 2014 Jun 24. [DOI] [PubMed] [Google Scholar]
- 7. Gardner MJ, Brodsky A, Briggs SM, Nielson JH, Lorich DG. Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clin Orthop Relat Res. 2006. June;447:165-71. [DOI] [PubMed] [Google Scholar]
- 8. Miller AN, Carroll EA, Parker RJ, Helfet DL, Lorich DG. Posterior malleolar stabilization of syndesmotic injuries is equivalent to screw fixation. Clin Orthop Relat Res. 2010. April;468(4):1129-35. Epub 2009 Oct 2. [DOI] [PMC free article] [PubMed] [Google Scholar]


