Abstract
Health care in the United States has become an information-intensive industry, yet electronic health records represent patient data inconsistently for lack of clinical data standards. Classifications that have achieved common acceptance, such as the ICD-9-CM or ICD, aggregate heterogeneous patients into broad categories, which preclude their practical use in decision support, development of refined guidelines, or detailed comparison of patient outcomes or benchmarks. This document proposes a framework for the integration and maturation of clinical terminologies that would have practical applications in patient care, process management, outcome analysis, and decision support. Arising from the two working groups within the standards community—the ANSI (American National Standards Institute) Healthcare Informatics Standards Board Working Group and the Computer-based Patient Records Institute Working Group on Codes and Structures—it outlines policies regarding 1) functional characteristics of practical terminologies, 2) terminology models that can broaden their applications and contribute to their sustainability, 3) maintenance attributes that will enable terminologies to keep pace with rapidly changing health care knowledge and process, and 4) administrative issues that would facilitate their accessibility, adoption, and application to improve the quality and efficiency of American health care.
About the process of health care and its understanding, the eminent English epidemiologist William Farr wrote more than 150 years ago that “the nomenclature is of as much importance in this department of inquiry, as weights and measures in the physical sciences, and should be settled without delay.”1
This observation remains true today, although promptness in addressing the challenge is something we cannot claim, and is underscored by a 1993 report of the General Accounting Office2 that emphasizes a need for leadership in developing terminology standards. The analogy to having a system of “weights and measures,” a metric for health care, is persuasive. How can we undertake chemistry or physics without grams, meters, and the periodic table? How can we understand efficient health care and improvement in patient outcomes without corresponding standards? Similarly, how can we compare practice patterns and outcomes without a common “language” or metric?
Finally, how might we efficiently develop practical electronic patient records without each time reinventing the language of their content, to create interchangeable documents rather than electronic repository analogs of Towers of Babel.
Efficient and effective health care delivery has become increasingly dependent on accurate and detailed clinical information. Those with more detailed, reliable, and comparable data for cost and outcome studies, identification of best practices, and management will be more successful in the marketplace. The use of guidelines and other decision support tools to enhance the quality of health care depends on the use of common terms and concepts in patient records and knowledge support resources. The business practices of performance benchmarking, measuring and interpreting outcomes, continuously improving care, and allocating limited resources to optimize quality and effectiveness similarly require comparable data and a standardized approach to information that adequately captures the details of clinical variation. Standardization of information is dependent on standardization of underlying terminologies, which include classifications and nomenclatures.* The quality and resolution of those terminologies dictate the quality of health care information.
Attention to health information standards is now timely. The Health Insurance Portability and Accountability Act of 1996 (PL 104-191) mandates that the National Committee for Vital and Health Statistics recommend to Congress health information standards, including clinical terminologies, for electronic medical records by August 2000. Since this committee was rechartered by the same legislation, they are now engaged in planning and development for this obligation. This document is pertinent to their tasks and addresses practical issues for terminology selection and development.
Why is Terminology Important?
Today, health terminologies are evolving to confront the dynamic challenges of increasingly computerized clinical data and the emergence of practical computerbased patient records. Indeed, the rapidly expanding market and expectations for computer-based patient record (CPR) systems have refocused the attention of the health care community on how we represent the history, findings, management, and outcomes of the patients we treat, in a way that can preserve clinical detail and identify characteristics that make possible improved risk adjustment, common guideline development, aggregate outcomes analyses, and shared decision support rules. These requirements are largely lacking in present day classifications such as ICD-9-CM or the Current Procedural Terminology of the American Medical Association, not only because they are limited for the most part to diagnoses and procedures, but because they and most current clinical classifications cannot represent degrees of severity or other qualifying details.3 The previously unrealistic task of retrieving relevant health risks or pertinent detail across patient histories or physical examination is now a common expectation among CPR information customers. Providers and CPR vendors must each engage in the difficult and expensive task of creating and maintaining clinical terminologies with varying degrees of utility, integrity, and satisfaction.
Were providers and CPR vendors relieved of the need to reinvent and reimplement local terminologies, they would have additional resources available for collaborative contributions to a common terminology and development of decision support applications, thereby improving the quality and efficiency of patient care. Far more important, common terminologies would support the creation of comparable data across health providers in the natural course of care delivery, making possible risk-adjusted benchmarking. Similarly, common guideline development, aggregate outcome analyses, and shared decision support rules could be based on sufficient sample sizes to generate reliable and significant results at a useful degree of clinical specificity. Recognizing the need for standards in clinical terminology, this paper proposes a framework for the development, maintenance, and implementation of integrated systems for American health care terminology.
Source
The American National Standards Institute (ANSI) convened a Health Information Standards Planning Panel in 1991 to coordinate the development of health care information standards in the United States and to participate in emerging global efforts.† A subcommittee of this panel, on clinical vocabulary, has worked to define a framework for understanding health care terminology needs and development priorities. This team has collaborated with the Working Group on Codes and Structures of the Institute of Medicine study4-inspired Computer-based Patient Records Institute (CPRI). The CPRI Working Group had undertaken a preliminary evaluation of content coverage for the major coding systems in use today,3 concluding that most classifications capture clinical detail poorly.
The joint Working Group on Codes and Structures of the CPRI and the Vocabulary Working Group of the ANSI Health Informatics Standards Board have developed this framework for the development and evolution of health terminologies. This white paper can also advise those selecting health care terminologies for use in their information systems and by their health care policy makers, although it is recognized that no current or imminent terminology possesses all the noted criteria.
Functional Characteristics
We propose that terminologies that can meet the important needs of health care in the near future must have, or evolve toward having, the following characteristics:
-
General. Basic characteristics of a terminology influence its utility and appropriateness in clinical applications.
- 1.1. Completeness.5 Each segment of the health care process must have explicit in-depth coverage and not rely on broad summary categories that lump specific clinical concepts together. For example, it is often important to distinguish specific diagnoses from categories currently labeled Not Elsewhere Classified or to differentiate disease severity, such as indolent prostate cancer from widely metastatic disease.
-
1.2. Comprehensiveness.6 All segments of the health care process must be addressed for all related disciplines—such as physical findings, risk factors, and functional status—across medicine, surgery, nursing, and dentistry. This criterion applies because decision support, risk adjustment, outcome research, and useful guidelines require more than diagnoses and procedures. Examples include existing AHCPR (Agency for Health Care Policy and Research) guidelines and the HCFA (Health care Financing Administration) mortality model discussed below.What practical alternatives for terminology development exist to achieve comprehensiveness? An obvious choice is a single, large terminology that is complete, comprehensive, and centrally administered. Alternatively, a system of integrated terminologies could evolve from established developers collaborating within a common framework such as the one we are proposing.
-
1.3. Characteristics of integration.7 Integrated terminologies would support unique term representation. Each terminology could be independently maintained to ensure relevance to the people using these systems. Comprehensiveness and completeness would therefore be more tractable, since they need apply only over the aggregate of integrated terminologies.
- 1.3.1. Nonoverlapping: Specialized terminologies should be nonredundant and should interrelate with existing systems by extension. This requirement eliminates the problem of an unknowable number of possible terms with identical meaning that might be chosen, making retrieval and aggregation tedious or impossible.
- 1.3.2. Integrated: To avoid overlapping concepts as these systems evolve, the number of cross-references by extension should grow and become interdependent. This process will require increasing coordination of content, as changes will ripple throughout these cross-dependencies. For example, it would be desirable if all terminologies reference a common anatomic hierarchy. Terminology sets will benefit from an integrated coordination of their development by reference to authoritative components, simplified development, and reduced maintenance.
- 1.4. Nonredundant. Terminologies must be internally consistent and have one and only one preferred way of representing a concept or idea. Nonoverlapping classifications are not possible if they are internally inconsistent. This does not exclude synonymy (§2.3); rather, it requires that synonymy be explicitly represented.
- 1.5. Mapping.8 Government and payers mandate the form and classification schema for much clinical data exchange. Thus, comprehensive and detailed representations of patient data in computer-based patient records need to be mapped to those systems, such as ICD-9-CM. Since detailed patient data and broader classification exist along a continuum, these mappings should be algorithmic and derive from mapping tables or hierarchies within the classification or should be created commonly (e.g., the Metathesaurus of the UMLS).
-
Structure of the terminology model. Terminology structures determine the ease with which practical and easy-to-use interfaces—for term navigation, entry, or retrieval—can be supported.
- 2.1. Atomic base.9 Concepts should be separable into their constituent components, to the extent practicable. These should form the root basis of all concepts. For example, a category for “hysterectomy with and without oophorectomy” does not permit the aggregation or study of oophorectomy.
- 2.2. Compositional. Atomic concepts must be able to be combined to create composite concepts.10 For example “colon cancer” comprises Carcinoma and Large Bowel as atomic components. These composite phrases are humanly intuitive and comfortable, as indeed the inconvenience of using exclusively atomic components for documenting care would preclude their adoption.
- 2.3. Synonyms. Alternative words and shorthand terms for composite concepts must be supported and consistently mapped. This functionality is critical to define explicitly equivalent meaning and to accommodate personal, regional, and discipline-specific preferences. These include abbreviations, but their implementation requires care to avoid ambiguity. In addition, the incorporation of non-English terms as synonyms can provide a simple form of multilingual support.
-
2.4. Attributes.11 Terminologies must support a logical structure that can modify or qualify meaning and support temporal duration and trend. Attributes must be themselves elements of a terminology and fit into a practical model that extends a terminology. For example, cancers may be described by stage and histology, by the specific time they have been symptomatic, and by their progression over an interval. Attributes are required to capture important data features for structured data entry and pertinence to secondary data uses such as aggregation and retrieval. Although nonoverlapping terms are an explicit goal (§1.3.1), they are not likely to be achieved for some time. Nevertheless, for a given concept that appears in multiple terminologies, attributes must be consistent to avoid incomparability.
- 2.4.1. Inheritance12: The default attributes of a term should vary among hierarchies. In many hierarchies the important attributes are well established—e.g., stage, grade, and histology are important features of tumors. Templates can be created to suggest attributes to clinicians in structured data entry. Inheritance simply recognizes that these templates will vary as a function of the primary diagnosis or procedure but will be similar across closely related concepts.
-
2.5. Multiple hierarchies.13 Concepts should be accessible through all reasonable hierarchic paths (i.e., they should have multiple semantic parents). For example, stomach cancer can be viewed as a neoplasm or as a gastrointestinal disease. This feature assumes obvious advantages for natural navigation of terms, as a concept of interest can be found by following intuitive paths. Users should not have to guess where a particular concept was put.
- 2.5.1. Consistency of view14: A concept in multiple hierarchies must be the same concept in each case. Our example of stomach cancer must not have changes in nuance or structure when arrived at via the cancer hierarchy as opposed to the gastrointestinal disease hierarchy. Inconsistent views could have catastrophic consequences for retrieval and decision support by inadvertently introducing variations in meaning of uncertain degree.
- 2.6. Explicit uncertainty. Notions of probable, suspected, and actual (diagnosed) conditions and differential possibilities must be supported. The impact of certain versus very uncertain information has obvious impact on decision support and other secondary data uses. Similarly, incomplete syndromes should identify the partial criteria.
- 2.7. Lexical rules. Terminologies should support software to accept typed input and filter valid words.15 It is often stated that every terminology system should have built-in spelling checkers. Mechanisms to support spelling integrity include valid word lists or a lexicon, optionally with a list of commonly misspelled entries. Similarly, a terminology should accommodate syntactic variants, inflections, and common word endings to facilitate recognition.
- 2.8. Representation. Computer coding of concepts must not have arbitrary restrictions, such as numbers of digits, attributes, or composite elements. These restrictions subvert meaning and content to the limitations of format, which often results in the assignment of concepts to the wrong location because they might no longer “fit” where they belong in a hierarchy. These reshufflings confuse people and machines alike, as intelligent navigation agents are led astray for arbitrary reasons. Because machines will process these identifiers, human perceptions of their length, appearance, or complexity are of little concern. The long, sequential alphanumeric tags used as concept identifiers in the UMLS (Unified Medical Language System) exemplify this principle (§3.1).
-
Maintenance. Technical choices can effect the capacity of a terminology to evolve, change, and remain usable over time.
-
3.1. Context-free identifiers.16 Unique codes attached to concepts must not be tied to hierarchic position or other contexts; they must not carry meaning. Because medical knowledge is being constantly updated, how we categorize medical concepts is likely to change. (For example, AIDS is now understood to be an infectious disease, but this was not always so.) For this reason, the “code” assigned to a concept must not be linked to a hierarchy, so that we need not change the code as we update our understanding. Changing the code may make historical patient data confusing or erroneous.Techniques that manage multiple hierarchies (§2.5) are widely available17 and will permit term or concept identifiers to be independent of context. As a practical matter, these hierarchic “tags,” or aliases, can be used as coding surrogates but must not replace unique codes.
- 3.2. Unique identifiers. Codes must not be reused after a term becomes obsolete or is superseded. Consistency of patient description over time is not possible when concepts change codes; the problem is worse when codes can change meaning. This practice not only disrupts historical analyses of aggregate data but can be dangerous in the care of individual patients whose data might be subsequently misinterpreted.
-
3.3. Version control.18 Updates and modifications must be referable to consistent version identifiers. Usage in patient records should carry this version information. Because the interpretation of coded patient data is a function of terminologies that exist at a point in time19 (e.g., AIDS patients were coded inconsistently before the introduction of the term AIDS), terminology representations should specify the state of the terminology system at the time a term is used. Version information most easily accomplishes this and may be hidden from ordinary review.
- 3.3.1. Dated: New terms, concepts, and synonyms must have their date of entry or effect in the system. Previous ways of representing a new entry should be recorded for historical retrieval purposes.
- 3.3.2. Obsolete marking: Superseded entries should be so marked, together with their preferred successor. Because data may still exist in historical patient records using obsolete terms, their future interpretation and aggregation are dependent on that term being carried and cross-referenced to subsequent terms.
- 3.4. Definitions. Each term must have an explicit definition. A common authority is important for the consistent interpretation of terms by providers and aggregate data analysts. At the present time, the definitions of terms differ among medical dictionaries and vary substantially among users in clinical practice.
- 3.5. Language independence. Non-English synonyms should be supported. As medicine confronts the global economy and multi-ethnic practice environments, routine terminology maintenance must incorporate multilingual support. While substantially lacking the power and utility of machine translation linguistics, this simplistic addition will enhance understanding and use in non-English speaking areas.
- 3.6. Responsiveness. The frequency of updates, or subversions, should be sufficiently short to accommodate new codes and repairs quickly, ideally within weeks. A coordinating authority for vocabulary maintenance would simplify the updating process.
-
-
Administration. Policies on the administration of vocabulary development and distribution will affect accessibility and broad adoption.
- 4.1. Coordination. In the absence of a single, all-embracing health care terminology, the coordination of and organizing support for interrelated terminologies should be undertaken by centralized nonprofit entities.
- 4.2. Access. The distribution and pricing of terminologies should not impose a barrier to wide access. Ideally, subsidized terminologies would be freely available on the Internet (as are ICD-9-CM and ICD-10-PCS), while others could be obtained or updated on demand for a nominal cost.
- 4.3. Funding. Funding for the coordination of terminology efforts should derive from public and private sectors. Support sources for the development and maintenance of component terminologies will vary, but they should balance adequate funding for these tasks with reasonable pricing to foster access and adoption. Developers might pursue revenue by the marketing of value-added functions, such as term look-up or maintenance tools, application software, terminology browsers, mappers, interfaces, or user education and support.
Finally, given equal rigor in the development and implementation of equivalent classifications and terminologies, those that have broad acceptance and usage, preferably in an international context, should receive preference.
Discussion
Ancient Hippocratic views of medicine dominated the classification of disease until the mid-17th century. The 16th century London Bills of Mortality20 gave rise to the notion of statistical causes of death, whose heritage persists in the International Classification of Disease (ICD).21,22 Despite the laudable effort to “clinically modify” the ICD in the United States,23 the Government Accounting Office issued a report on electronic medical records2 that targeted clinical vocabulary as being among the most strategic but least developed of the underlying information technologies.
The modern reality of the health care industry will not permit us an additional 150 years to respond to Farr's challenge.1 Computer-based patient record systems are being designed, constructed, purchased, and installed today. And hoc terminologies are being incorporated in this explosive market to address urgent practical needs. As these terminologies mature for use in automated systems, it is important that they evolve in a common direction toward standard data representation. Failure to achieve common goals and standards will preclude efficient comparison of practice patterns and outcomes, and we will therefore have great difficulty identifying best practices and sharing these findings among institutions or nations. Nor would we be able to consistently implement identified best practices across institutions, as health care deliverers begin to develop decision support resources in parallel throughout our nation and internationally.
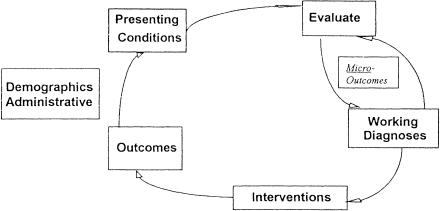
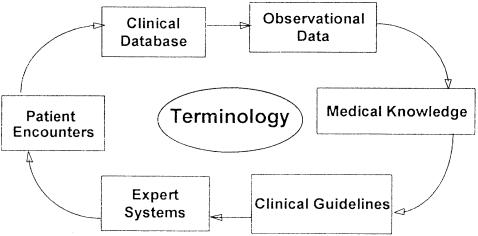
The inclusion of outcomes in a common framework is perhaps the single most critical feature of a useful clinical classification. Outcomes may be regarded in the circle of longitudinal care as analogous to the presenting conditions of a subsequent episode, including outcomes manifest as a resolution of diseases or syndromes (▶). Furthermore, in the course of clinical care, micro-outcomes are generated (labeled “Working Diagnoses” in ▶), which in turn influence ongoing diagnostic studies, evaluation, and appropriate intervention. Understanding and managing the health care process would be greatly enhanced by a composite representational system that unifies these views. Failure to connect terminologies for presenting conditions, final diagnoses, interventions, and outcomes not only perpetuates artificial divisions but compromises the capacity of medical knowledge to enhance and be enhanced by patient care experience (▶).
Figure 1.
Cycle of longitudinal care, illustrating that outcomes can be regarded as presenting conditions for a subsequent episode.
Figure 2.
Cycle of patient data generating medical knowledge and improved care. Terminology is the conceptual glue that links the processes and resources.
This concern is not academic. The HCFA mortality analyses24 have been used as a quality proxy for U.S. hospitals. Calculated from Medicare reporting data, they rely on ICD-9-CM discharge diagnoses to approximate case mix and co-morbid conditions. For illustration, we employed the model on a Mayo cohort of lung and colon cancer patients and repeated the analysis by adding severity of illness as measured by cancer stage,25 which ICD-9-CM does not capture. We demonstrated the profound bias in HCFA mortality models based only on the ICD-9-CM-derived representations among hospitals where the distribution of cancer stage differs appreciably. Quality and policy decisions may be suspect if they rest on data that do not adequately capture patient conditions and pertinent qualifiers.
There is a natural harmony between the clinical application of terminologies and the administrative needs for reimbursement grouping, practice management, and statistical reporting. In simple terms, administrative information can always be derived from clinical detail, but the converse is rarely true. Integrated clinical classifications help ensure this practical reality. The GAO report asserts that there is an absence of leadership, but it may be that to achieve the goals of comprehensive, integrated terminologies we have too many leaders, all moving independently. Despite this sobering observation, strong precedents for integrated terminologies do exist, most successfully in the sharing of histopathology terms and codes among MONTAC,26, SNOMED, and ICD-O.22
Proposed Activities
We must articulate the need for common support for the coordinated integration of terminology sets and work toward creating it by securing funding from providers, system vendors, payers, and the government.
Developers of clinical classifications must consider ways they can develop their systems to become part of an integrated set of terminology systems.
Providers, system vendors, payers, and the government must endorse these requirements and become partners in their development.
A national conference should be convened to explore new partnerships in terminology development and maintenance, to strengthen existing collaborations, and to address ways an integrated system of terminologies can evolve. Conclusions should define the nature and role of a coordinating body for terminology integration.
An entity serving the public interest should be selected or created to coordinate health care terminology content in the spirit proposed by this document and modified by the national conference.
Attention and resources must be focused on the iterative evaluation and practical improvement of integrated terminology sets as these evolve in realworld applications.
From these beginnings, the evolution and growth of health care terminologies that satisfy the needs of providers, payers, managers, and researchers and, most important, contribute to more efficient and effective care of patients can proceed. The absence of a detailed clinical terminology that enjoys wide use will only continue to hinder practical measurement and improvements in health care delivery.
Footnotes
In the document we consider nomenclature and classification to be on a continuum to which we refer as terminology. Aggregating “classifications” should derive from more finely grained “nomenclatures.” See ISO 1087-1 Terminology Work—Vocabulary—Part 1: Theory and Application for formal definitions of their nuances.
The Planning Panel was converted to the Healthcare Informatics Standards Board in December 1995.
References
- 1.Farr W. First Annual Report of the Registrar-General of Births, Deaths, and Marriages in England. London, England, 1839, p. 99.
- 2.General Accounting Office. Medical ADP Systems: Automated Medical Records: Leadership Needed to Expedite Standards Development. Washington, D.C.: GAO, 1993. Publication no. GAO-IMTEC-93-17.
- 3.Chute CG, Cohn SP, Campbell KE, Oliver DE, Campbell JR. The content coverage of clinical classifications. J Am Med Inform Assoc. 1996;3(3): 224-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dick RS, Steen EB. The Computer-Based Record: An Essential Technology for Health Care. Washington, D.C.: National Academy Press, 1991. [PubMed]
- 5.Cimino JJ. Desiderata for controlled medical vocabularies in the twenty-first century. Methods Inf Med. 1998, in press. [PMC free article] [PubMed]
- 6.Côté RA, Rothwell DJ. The classification-nomenclature issues in medicine: a return to natural language. Medical Inform. 1989;14(1): 25-41. [DOI] [PubMed] [Google Scholar]
- 7.Friedman C, Huff SM, Hersh WR, Pattison-Gordon E, Cimino JJ. The Canon Group's effort: working toward a merged model. J Am Med Inform Assoc. 1995;2(1): 4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rocha RA, Rocha BH, Huff SM. Automated translation between medical vocabularies using a frame-based interlingua. Proc 17th Annu Symp Comput Appl Med Care. 1993: 690-4. [PMC free article] [PubMed]
- 9.Evans DA, Cimino JJ, Hersh WR, Huff SM, Bell DS, for the CANON Group. Position statement: toward a medical concept representation language. J Am Med Inform Assoc. 1994;1: 207-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bernauer J, Franz M, Schoop D, Schoop M, Pretschner DP. The compositional approach for representing medical concept systems. Medinfo. 1995;8(Pt 1): 70-4. [PubMed] [Google Scholar]
- 11.Blois MS. Information and Medicine. The Nature of Medical Descriptions. Berkeley, Calif.: University of California Press, 1984.
- 12.Rector AL, Nowlan WA, Glowinski A. Goals for concept representation in the GALEN project. Proc 17th Annu Symp Comput Appl Med Care. 1993: 414-8. [PMC free article] [PubMed]
- 13.Campbell KE, Musen MA. Representation of clinical data using SNOMED III and conceptual graphs. Proc 16th Annu Symp Comput Appl Med Care. 1992: 354-8. [PMC free article] [PubMed]
- 14.Rossi Mori A, Galeazzi E, Gangemi A, Pisanelli DM, Thornton AM. Semantic standards for the representation of medical records. Med Decis Making. 1991;4(suppl): S76-80. [PubMed] [Google Scholar]
- 15.McCray AT, Srinivasan S, Browne AC. Lexical methods for managing variation in biomedical terminologies. Proc 18th Annu Symp Comput Appl Med Care. 1994: 235-9. [PMC free article] [PubMed]
- 16.Tuttle MS, Olson NE, Campbell KE, Sherertz DD, Nelson SJ, Cole WG. Formal properties of the Metathesaurus. Proc 18th Annu Symp Comput Appl Med Care. 1994: 145-9. [PMC free article] [PubMed]
- 17.Cimino JJ, Clayton PD, Hripcsak G, Johnson SB. Knowledge-based approaches to the maintenance of a large controlled medical terminology. J Am Med Inform Assoc. 1994; 1(1): 35-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Campbell KE, Cohn SP, Chute CG, Rennels G, Shortliffe EH. Galapagos: computer-based support for evolution of a convergent medical terminology. J Am Med Inform Assoc. 1996; SympSuppl: 269-73. [PMC free article] [PubMed]
- 19.Cimino JJ. Formal descriptions and adaptive mechanisms for changes in controlled medical vocabularies. Methods Inf Med. 1996;35(3): 211-17. [PubMed] [Google Scholar]
- 20.Graunt J. Natural and Political Observations Made Upon the Bills of Mortality. London Bills, 1662. Republished by The Johns Hopkins Press, Baltimore, Md., 1939.
- 21.Greenwood M. Medical statistics from Graunt to Farr, parts I-V. Biometrika. 1942;32: 101-27, 203-25; 1943;33:1-24. [Google Scholar]
- 22.World Health Organization. International Classification of Diseases for Oncology (ICD-O), Geneva, Switzerland: WHO, 1976.
- 23.World Health Organization. International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM). Vols 1-3. Ann Arbor, Mich.: Commission on Professional and Hospital Activities, 1977.
- 24.Appendix 6. Medicare Hospital Information, 1988-1990. Washington, D.C.: U.S. Government Printing Office, 1992.
- 25.Beahrs OH, Henson DE, Hutter RVP, Myers MH (eds). Manual for Staging of Cancer. 3rd ed. Chicago, Ill.: American Joint Committee on Cancer, 1988.
- 26.American Cancer Society Statistics Committee. Manual of Tumor Nomenclature and Coding (MONTAC). Chicago, Ill.: ACS, 1951.