Abstract
Abstract Objective: To measure the effect of computer-based outpatient prescription writing by internal medicine physicians on pharmacist work patterns.
Design: Work sampling at a hospital-based outpatient pharmacy. Data were collected from pharmacists wearing silent, random-signal generators before and after the implementation of computer-based prescribing.
Measurements: The type of work performed by pharmacists (activity), the reason for their work (function), and the people they contacted (contact) were measured.
Results: Total staff hours and prescriptions handled were similar before and after computer-based prescribing. Pharmacists recorded 4,687 observations before and 4,735 observations after implementation of computer-based outpatient prescription writing. After implementation, pharmacists spent 12.9 percent more time correcting prescription problems, had 3.9 percent less idle time, and spent 2.2 percent less time in discussions with others. Pharmacists also spent 34.0 percent less time filling prescriptions, 45.8 percent more time in problem-solving activities involving prescriptions, and 3.4 percent less time providing advice. Over 80 percent of pharmacist time was spent working alone both before and after computer-based outpatient prescription writing.
Conclusion: Computer-based prescribing results in major changes in the type of work done by hospital-based outpatient pharmacists and in the reason for their work and small changes in the people contacted during their work.
Pharmacy has readily accepted computerization, and innovative pharmacy information systems are being developed.1 Pharmacists must carefully process, store, and track a large volume of paper, mainly in the form of prescriptions, maintain an inventory of the most commonly prescribed medications, and routinely make quick linkages between hundreds of prescribers, thousands of patients, and millions of prescriptions. Hence, pharmacists embraced computerization quickly and pervasively to increase their efficiency.
The paper prescription, although historically effective, has always been a somewhat painful prescribing medium for physicians, patients, and pharmacists. The biggest problem with paper prescribing for physicians is the amount of time needed to recall from memory or look up which medication and dosage to prescribe more than 20,000 products. To further complicate matters, physicians increasingly deal with different formularies for sundry insurance schemes. They then must legibly write each prescription. Pharmacists deal with hundreds of prescriptions each day and must legally account for each one, must store them, and must be able to retrieve them for refills. Thus, alternative ways of generating and maintaining prescriptions with computers are often sought.
Computer-based writing of prescriptions by physicians addresses many of the problems posed by the paper prescription.2 Many of the advantages of this form of prescribing are obvious. More advanced systems can provide physicians with the list of medications covered by patients' insurance plans, provide the list of medications obtained in a specific plan's formulary, and enable the pharmacist to easily determine the right medication and even provide a safety check on interactions or dosage. When there are links between the physician's office and patient's pharmacy, the prescription can be sent directly to the pharmacy, be filled while the patient is traveling there from the physician's office, and be ready for pick-up on arrival. Pharmacists would save much time not having to interpret physician's writing and save much space storing prescriptions.3 The time needed for retrieval of prescriptions for refills would be greatly diminished.
There are no studies describing the effect of computer-based outpatient prescription writing by physicians on pharmacist work patterns. We had an ideal opportunity to learn more about this issue as we extended our inpatient physician order-writing workstation into our large primary-care general internal medicine practices. We therefore measured the effects of computer-based outpatient prescription writing by physicians on pharmacist work patterns using multidimensional work sampling. We previously used this methodology to measure pharmacists' work patterns before a randomized health services trial began, to provide a baseline with which future system and process changes could be compared.4 The purpose of this study was to determine the changes in pharmacist work patterns from this baseline after the introduction of computer-based writing of outpatient prescriptions. As such, our hypothesis was stated as the null, namely, implementation of computer-based outpatient prescription writing by physicians would have no effect on pharmacist work patterns.
Methods
Setting
The study was conducted at the general medicine practice (GMP) and the outpatient pharmacy of the Regenstrief Health Center, the primary outpatient facility of Wishard Health Services, Indianapolis, Indiana. In addition to this outpatient facility, Wishard Health Services has a 300-bed urban public teaching hospital and the busiest emergency department in Indiana. The outpatient pharmacy processes 1,000 to 1,500 prescriptions each day, Monday through Friday, as part of the care of more than 50,000 outpatients who make over 400,000 visits annually to the clinics and emergency department. More than 100 internists practice at the GMP during any given week, and they write the largest number of prescriptions for the 11 full-time and 9 part-time pharmacists at the outpatient pharmacy. Pharmacists are assisted by 14 full-time and 4 part-time technicians. Although there are other clinics at the Regenstrief Health Center that are serviced by the pharmacy, the majority of prescriptions derive from the GMP. Our internal studies have revealed that more than 95 percent of patients who receive their care from the GMP fill their prescriptions at the outpatient pharmacy.
The Regenstrief Medical Record System
For 25 years the GMP and outpatient pharmacy have been served by the Regenstrief Medical Record System (RMRS).5 The components of the RMRS that are relevant to this study are a VAX-based pharmacy computer module used by the pharmacists in the pharmacy to process all prescriptions (paper and electronic) and a network of comprehensive microcomputer workstations used by physicians in the GMP. The pharmacy module is the primary information system enabling the pharmacy to fill prescriptions. Sixty-four percent of prescriptions derived from GMP physicians during this study. Before computer-based outpatient prescription writing by physicians became available at the GMP, physicians wrote paper prescriptions. The patient hand-carried these paper prescriptions from the GMP to the outpatient pharmacy, where they were then interpreted by pharmacists and technicians who entered the prescription information into the RMRS at one of the five VAX terminals throughout the pharmacy. The RMRS stored all prescription data for ready retrieval and then generated a label for the pharmacist to apply to the medication's container.
Computer-based Prescribing
Online prescription entry created major changes in the process of handling prescriptions by physicians and pharmacists. First, GMP physicians entered their prescriptions directly into microcomputer workstations located throughout the GMP.5 After a patient's hospital number is entered, a menu of actions is displayed on the monitor. Among selections on the menu is one for prescription medications. When the prescription order selection is chosen, all active prescription medications for the patient are shown. The physician can renew or modify an existing medication that has been previously stored or order a new medication.
Prescription renewal is as simple as highlighting the medication, reviewing the fields corresponding to the medication's dosage, sig, and quantity to dispense. To prescribe a new medication, the physician can quickly summon a specific order by typing in a few letters of the medication's name or can peruse a specific formulary class of drugs to look for alternative treatments. This process can improve practice by removing some of the practical ambiguities physicians have in writing prescriptions (which drug, strength, dosage, how supplied, and costs) and by reminding physicians how to effectively monitor patients' drug therapy and avoid important drug interactions.
After the physician enters all medications, an electronic copy of the patient's prescription is sent to the pharmacy and a paper copy is printed for the patient. The paper copy given to the patient serves two purposes. First, pharmacies in Indiana are required by law to store a paper copy of the prescription. Second, the paper copy brought to the pharmacy by the patient serves to notify the pharmacist that the patient is at the pharmacy and their prescriptions have already been written and stored. To display the patient's prescriptions, the pharmacist enters a prescription access code specific to the patient, physician, and date. All the patient's prescriptions are then displayed for the pharmacist to accept, modify, or reject. The paper copy is filed later in the evening after the majority of patients have been served during the day.
Multidimensional Work Sampling
The method used to measure the work patterns of pharmacists has been described previously.4 We briefly describe the methods here. We used multidimensional work sampling to determine the proportion of pharmacists' time spent in a variety of predefined work activities (activity), the reason for each activity (function), and the people contacted by the pharmacists to do their work (contact). Recording the appropriate combination of items from each of these three dimensions permitted any work-related task to be accurately described. The Appendix contains the definitions measured. Although we collected data on a variety of specific activities and functions, we condensed into a single dimension several specific activities and functions that were closely related, to facilitate graphic interpretation.
We measured the work patterns of pharmacists before and after the implementation of computer-based outpatient prescription writing by GMP physicians. Online entry of prescriptions by physicians at the GMP began on Feb 28, 1994. Therefore, the first work sampling period was from Dec 13, 1993 through Feb 11, 1994, and the second sampling period was from Mar 2 through Apr 15, 1994. We scheduled the after-phase of work sampling soon after computer prescribing began, to avoid confounding our results with other interventions being planned, such as pharmacy renovation.
Multidimensional work sampling requires that pharmacists record a large number of instantaneous observations taken at random intervals.6,7,8,9,10 Because pharmacists work inside and outside the pharmacy, we conducted the study using self-reported work sampling (as opposed to direct observation methods) with a random-signal generator that pharmacists took with them wherever they went during their work day.4, 11 Each day pharmacists were provided with a pager-sized device (JD-7, Divilbliss Electronics, Champaign, Illinois) that randomly buzzed pharmacists at the rate of four to eight signals per hour, prompting them to record their activity, function, and contact on a form that exact instant the pager buzzed. For example, imagine that at 10:15 A.M. a pharmacist was checking a prescription previously filled by a technician, when she felt the pager buzz. She stopped what she was doing, pulled the recording sheet out of her pocket, and wrote 2-1-1 under the 10-to-11 time block on the sheet. This notation, when decoded (see Appendix) indicates the no. 2 activity, “Check/Prescription,” the no. 1 function, “Fill Prescription,” and the no. 1 contact, “Self.” In other words, at the instant the pharmacist was interrupted, she was checking a prescription to dispense it by herself.
At the end of the day, pharmacists returned their pagers and the completed forms. Because their work was not characteristic of the other pharmacists, pharmacist supervisors did not participate in the study. Furthermore, measurement of work performed by technicians also was not an objective of this study. Technical support remained constant in both the type of work performed and the numbers of full-time and part-time technicians performing the work. However, the distribution of the type of work done, the reason for that work, and the contacts were likely to shift in response to the changes in pharmacists' work.
We trained pharmacists on work documentation procedures and pretested them on the sampling method. Pharmacists getting 90 percent or more of test questions correct were able to participate after being given explanations of any errors they made. Pharmacists scoring less than 90 percent (n=2) were provided with additional lessons and further time to study the dimensions being measured. Afterwards, these pharmacists received scores of 100 percent. We conducted a run-in phase of one week to allow pharmacists to become acquainted with the work-recording process. Run-in data were discarded.
Validation Study
Multidimensional work sampling has been shown to be an accurate, indirect method of work measurement.8, 12, 13 To validate our sampling methodology, we directly observed pharmacists recording their work and determined percentage agreement with their work-measurement recording. A research assistant, trained in the assessment of pharmacist work patterns, was introduced to all the pharmacists in the study, and the purpose of the validation study was explained to the pharmacists. At random times, Monday through Friday, 8:00 A.M. to 7:00 P.M. (the study sampling time frame), the research assistant visited the pharmacy and observed the pharmacists while they worked. During these visits, the research assistant stopped the pharmacist during a variety of activities and asked him or her to describe in detail the activity, function, and contact at that instant. For 103 interruptions, 309 coded entries were assessed by the research assistant and then by one of us. Of the activities measured, the percentage agreement among pharmacists, the research assistant, and the investigator was 95 percent (95 percent confidence interval: 89-98 percent), and of the functions and contacts, the percentage agreements were both 99 percent (95 percent confidence interval: 95-100 percent). We believe these results validate our data recording method and are in agreement with the findings of other investigators.13
Statistical Analysis
Using our baseline data, we performed sample size estimates,14 which indicated that 4,500 observations would provide us with sufficient power to detect a 0.7 percent absolute change in the advising function (counseling patients and consulting with physicians). For estimation, the baseline advising function (function 7) accounts for 5.9 percent of all functions. Based on this sample proportion, 4,500 observations allows us to control the margin of error to less than 0.7 percent with 95 percent confidence. For more general estimates (any activities, contacts, functions), this margin of error is no more than 1.5 percent.
For tests of significance comparing two proportions, the sample size depends on the significance level of the test as well as the allocation of sample sizes. At 0.05 significance level, assuming the two samples have equal sizes of 4,500, the test has the power to detect a 1 percent change in advising function. For more general tests, two samples—each with a size of 4,500—allow for the detection of changes greater than 2 percent.
To assess whether the computer-based outpatient prescription writing by GMP physicians changed the distributions of the activity, functions, and contacts of pharmacists' operation, we used chi-squared tests to test the hypothesis that the distributions of the activities (or functions or contacts) are independent.15 To identify the specific activities, functions, and contacts that have changed significantly after computer-based outpatient prescription writing, we compared the probabilities of each individual category before and after proportions. Since we considered only one particular activity at a time (for example, “discuss” versus all others) a binomial model was appropriate. A commonly used test for comparing two proportions is the t-test.16 In large sample situations, the distribution of the test statistic T can be approximated by the standard normal distribution. The conclusion from the t-test was confirmed with tests based on generalized estimation equation models, which take into account the potential intercorrelation among the observations of the same subject (pharmacist) in the analysis.17
Results
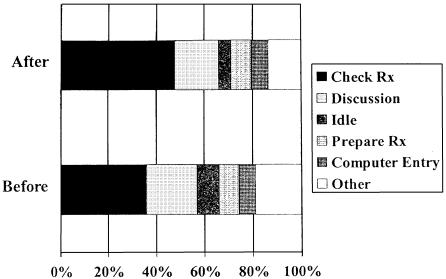
Before and after computer-based prescribing, total staff hours and numbers of prescriptions were similar. During both periods, pharmacists and technicians worked 475 and 660 hours per week, respectively. The total numbers of prescriptions handled before and after computer-based prescribing were 926 and 1007 prescriptions per day, respectively. Pharmacists recorded a total of 9,422 observations during the study. Before computer-based outpatient prescription writing began, 4,687 observations were recorded, and afterward pharmacists recorded 4,735 observations. ▶ shows the proportion of time spent on the various activities, functions, and contacts. The overall distributions before and after computer-based outpatient prescription writing differed significantly for activities, functions, and contacts (P < 0.001). This indicates that computer-based outpatient prescription writing significantly affected the type of work pharmacists performed, why they did the work, and who they came in contact with while they worked. ▶ shows the before and after distributions of work activities. After computer-based outpatient prescription writing, pharmacists spent 12.9 percent more time checking prescriptions. These are activities that might be expected to increase as pharmacists became more vigilant with regard to physician's electronic orders. Pharmacists spent 3.9 percent less time waiting for work to do, and 2.2 percent less time meeting.
Table 1.
Comparison of Pharmacist Work Patterns (Percentage of Time) Before and After Online Entry of Prescriptions by Physicians
| Work Characteristic | Before (%) | After (%) | Difference | P-Value |
|---|---|---|---|---|
| Activity | ||||
| Check prescription | 36.16 | 49.05 | +12.89 | 0.001 |
| Discussion | 20.72 | 18.48 | -2.24 | 0.006 |
| Prepare prescription | 8.19 | 8.41 | -0.22 | 0.700 |
| Idle | 9.15 | 5.24 | -3.91 | 0.001 |
| Computer entry | 6.76 | 7.31 | +0.55 | 0.299 |
| Other | 19.01 | 13.69 | -5.32 | 0.001 |
| Function | ||||
| Fill prescription | 51.27 | 17.3 | -33.97 | 0.001 |
| Advise/inform | 13.36 | 10.04 | -3.32 | 0.001 |
| Problem-solve | 5.06 | 50.87 | +45.81 | 0.001 |
| Other | 30.32 | 21.75 | -8.57 | 0.001 |
| Contact | ||||
| Self | 80.01 | 84.01 | +4.0 | 0.001 |
| Patient | 11.46 | 10.53 | -0.93 | 0.152 |
| Pharmacy staff | 4.25 | 2.17 | -2.08 | 0.001 |
| MD/RN | 1.73 | 2.06 | +0.33 | 0.242 |
|
Other
|
2.56
|
1.18
|
-1.38
|
0.001
|
| Note: The activities, functions, and contacts listed here are defined in the Appendix. | ||||
Figure 1.
Pharmacist work activities before and after computer-based outpatient prescription writing by physicians. The activities are defined in the Appendix. Rx indicates prescription.
Interestingly, pharmacists spent about the same amount of time entering information into the computer after computer-based outpatient prescription writing as they did before (P = 0.299), although this fraction of their activities is small. Before online entry pharmacists (or technicians) had to hand-enter all the prescription data from the paper copy. After computer prescribing began, most of the pharmacists' computer time involved the electronic review of previously entered prescription data, which involves moving through the fields (sig, dosage form, quantity to dispense) to accept or edit the data entered by physicians. Although this would reduce the amount of time, pharmacists spent more computer time editing the previously entered physician orders (vide infra).
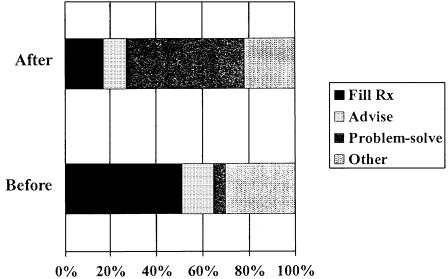
▶ shows the distributions of work functions or the reason for their work. After computer-based outpatient prescription writing, pharmacists spent 45.8 percent more of their time problem-solving physician's orders. This undoubtedly had much to do with physicians' learning more about the various medications stored in the pharmacy inventory and the need for pharmacists to help them deal with a variety of prescribing issues that were new to them.
Figure 2.
Pharmacist work functions before and after computer-based outpatient prescription writing by physicians. The functions are defined in the Appendix. Rx indicates prescription.
Most of these problems involved the pharmacists' editing or double-entering work, on each individual prescription, already entered by physicians. Pharmacists were required to inspect each field and accept or correct data entered by the physician. Before computer-based prescribing, pharmacists were required to conform to a firm syntax when entering the prescription sig such as “1 tab PO TID.” To make entry of prescriptions easy for the physicians, the system was designed to allow them to enter the sig as free-form text, which then had to be translated back by pharmacists into the appropriate syntax.
Because physicians' lack familiarity with the strengths and dosage forms available in the pharmacy, pharmacists needed to edit these entries. For example, a physician may enter a prescription as “Take one 100-mg tablet TID” when the pharmacy has 50-mg capsules. The pharmacist would need to change this to read “Take two 50-mg capsules TID.” Physicians also have no way of telling when a drug or dosage has been depleted from the pharmacy inventory. When it has, the pharmacist may need to change the patient's dosage regimen (e.g., from one 100-mg tablet to two 50-mg tablets) to fill the prescription quickly. Moreover, physicians were not aware that some medications were available in ready-to-dispense packaging, which was encouraged to reduce counting of individual tablets and capsules for commonly used medications. Owing largely to this time spent problem solving, the time spent filling prescriptions decreased by 34 percent. The time pharmacists spent advising physicians about other aspects of patients' treatments and advising patients decreased by 3.3 percent, a considerably smaller effect than that seen with problem solving and prescription filling.
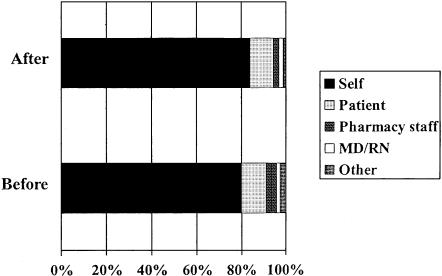
▶ shows the distribution of pharmacist contacts during their work. Both before and after computer-based outpatient prescription writing by physicians, pharmacists spent more than 80 percent of their time working alone. There was a small increase (4 percent) in the amount of solo work by pharmacists after computer-based outpatient prescription writing and a complementary small decrease in the amount of time pharmacists spent in direct contact with other pharmacists. Differences in effects on the amount of time spent with physicians and nurses and with patients were small and not statistically significant.
Figure 3.
Pharmacist work contacts before and after computer-based outpatient prescription writing by physicians. The contacts are defined in the Appendix.
Discussion
Our results indicate that the overall effect of computer-based outpatient prescription writing by physicians on pharmacist work patterns was to increase the percentage of pharmacists' time spent checking prescriptions entered by physicians and sorting out problems that occurred. Pharmacists were able to perform this work without directly increasing interactions with physicians and without increasing the number of staff required to handle the workload. In our previous study of pharmacist work patterns before computer-based outpatient prescription writing, we found that pharmacists spent most of their time working alone.4 We had some hopes that changes in prescription processing resulting from computer-based outpatient prescription writing would reduce the time pharmacists spent processing prescriptions and provide more time for communicating with patients and health professionals. That did not occur.
Assessment of the proportion of pharmacist time spent in work activities, functions, and contacts during this study provided us with an improved understanding of shifts in pharmacist work with prescription and information processing changes. This becomes especially relevant when state Boards of Pharmacy permit paperless (electronic) prescribing. As pharmacy progresses in its delivery of pharmaceutic care in this era of managed care, such systems could become more common. If so, understanding their influence on pharmacist work patterns will be pivotal.
Pharmaceutic care fosters increased involvement in the process of drug therapy evaluation, problem solving, monitoring and, when necessary, intervention to increase the beneficial effects of drugs and reduce their adverse effects.18, 19 The emphasis of managed care on efficient use of resources and time in the delivery of services makes changes in prescription management critical.20 Such a focus will increasingly require pharmacists to transfer some aspects of their prescription management to computers and dispensing activities to technicians. It is hoped that this would increase the amount of time pharmacists had available to advise patients and interact with physicians. However, we did not find this expected work shift. Instead, more time was required for solving prescribing problems. Others have reported similar shifts from one type of dispensing work to another (without an increase in interaction with patients or physicians) after an outpatient pharmacy had been computerized.13, 21
There are four limitations to this study. First, it would have been helpful to learn how computer-based outpatient prescription writing affected the amount of time physicians spent doing their work. Unfortunately, we were unable to conduct such a study of physicians' work patterns. Second, multidimensional work sampling has its own inherent deficiencies, which have been recently delineated.8, 10 Nonetheless, agreement was excellent in our direct-observation validation study. Third, our work sampling might have begun too soon after computer-based outpatient prescription writing was introduced and so might differ from a stable estimate made several months later. To address this possibility, we further examined the effect of time using our data. We split our before and after measurement periods to compare the results of the early part of the before period (Dec 13, 1993, to Jan 2, 1994; n = 2,286 observations) to the latter part of the after period (Mar 24 to Apr 15, 1994; n = 2,461 observations). We then compared distributions of activities, functions, and contacts. We found that the distributions of activities, functions, and contacts are similar to the original distributions, and the tests of significance lead us to the same fundamental conclusions as our original data. Obviously, it would have been preferable to have collected data at a later time. However, impending renovations to the pharmacy precluded a later measurement phase. Finally, our electronic medical record system is unique. Its capabilities are more advanced than those of most other health care systems, yet those advancements, by their very nature, are more crude than can be expected when more mature systems became widely adapted.
We conclude that computer-based outpatient prescription writing by physicians has a profound effect on the type of pharmacist work and reasons for it but little overall effect on the amount of time pharmacists spend with patients and physicians. This information would be beneficial to managers and planners who are considering the implementation of computer-based prescribing. We are exploring how other process changes to the delivery of information affect physicians and pharmacists as they work. It is possible that collectively these process changes will improve the ability of pharmacists to deliver pharmaceutic care, especially if the electronic medical record can target high-risk patients for pharmacist interventions. Finally, we believe that work sampling is a valuable tool for measuring the effect of longitudinal changes within a pharmacy on pharmacist work patterns.
Acknowledgments
The authors acknowledge the patience and support of the participating pharmacists and physicians. They thank Ms. Holly Borgers and Ms. Debby Garey for their time and patience entering the work observations made by pharmacists in this study.
Appendix
Definitions of Work Dimensions*
Activities
Discussion: Any interactions with one or more people, including telephone conversations.
Check Prescription: Checking a prescription that has been prepared.
Prepare Prescription: Retrieving a drug from the shelf, counting tablets or capsules, putting the medications into the container, and labeling the container.
Idle: Includes traveling from one place to another or waiting for the next activity.
Computer Entry: Any time spent entering information into the computer through the computer keyboard. (Other data input devices were unavailable.)
Other: Includes indexing and filing prescriptions, writing notes, and running errands, taking a break or eating lunch, and miscellaneous activities.
Functions
Fill Prescription: Preparing the prescription to dispense it to the patient.
Advise/Inform: Includes giving or taking information about the patient, including any professional consultation or advice given to a patient, patient representative, physician, or nurse concerning medication use.
Problem-solve: Detecting and correcting problems associated with prescription duplication and other prescription problems, such as no signature, no strength provided or unavailable strength, nonformulary drug, or a drug interaction.
Other: Includes recording financial information, stocking medications, continuing education, work measurement, and miscellaneous other functions.
Contacts
Self: Includes time when pharmacists are not interacting with anyone.
Patient: Includes interactions with all patients and the people who are with them.
Pharmacy Personnel: Includes interactions with outpatient, inpatient, and administrative pharmacy personnel.
MD/RN: Includes all physicians, residents, and dentists, whether or not they work at the institution, and licensed registered and practical nurses.
Other: Includes interactions with someone not listed above.
This work was supported by Pharmaceutical Outcomes Grant R01-HS07763 from the Agency for Health Care Policy and Research.
Footnotes
References
- 1.Nold EG. Trends in health information systems. Am J Health Syst Pharm. 1997;54: 269-74. [DOI] [PubMed] [Google Scholar]
- 2.Sittig DF, STead WW. Computer-based physician order entry: The state of the art. J Am Med Inform Assoc. 1994;1: 108-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tierney WM, Miller, ME, Overhage JM, McDonald CJ. Physician inpatient order writing on microcomputer workstations: effects on resource utilization. JAMA. 1993;269: 379-83. [PubMed] [Google Scholar]
- 4.Murray MD, Rupp MT, Overhage JM, Ebbeler DE, Main JW, Tierney WM. Multidimensional work sampling in an outpatient pharmacy. Pharm Pract Manage Q. 1995;15: 44-56. [PubMed] [Google Scholar]
- 5.McDonald CJ, Tierney WM, Overhage JM, Martin DK, Wilson GA. The Regenstrief Medical Record System: 20 years of experience in hospitals, clinics, and neighborhood health centers. MD Comput. 1992;9: 206-17. [PubMed] [Google Scholar]
- 6.Roberts M, Kvalseth TO, Jermstad RL. Work measurement in hospital pharmacy. Top Hosp Pharm Manage. 1982;2: 1-17. [PubMed] [Google Scholar]
- 7.Robertsen JA. Multidimensional work sampling: a new tool for pharmacy management. Top Hosp Pharm Manage. 1982;2: 1824. [PubMed] [Google Scholar]
- 8.Hadsall RS, Gourley DR, Haggerty, JA, Yih P, Windle MJ, Ohri L. Work sampling in contemporary pharmacy practice: a multidimensional approach. Top Hosp Pharm Manage. 1982;2(Nov): 15-26. [PubMed] [Google Scholar]
- 9.Rascati KL, Kimberlin CL, McCormick. Work measurement in pharmacy research. Am J Hosp Pharm. 1986;43: 2445-52. [PubMed] [Google Scholar]
- 10.Nickman NA, Guerrero RM, Bair JN. Self-reported work-sampling methods for evaluating pharmaceutical services. Am J Hosp Pharm. 1990;47: 1611-7. [PubMed] [Google Scholar]
- 11.Guerrero RM, Nickman NA, Bair JN. Work activities of pharmacy teams with drug distribution and clinical responsibilities. Am J Health Syst Pharm. 1995;52: 614-20. [DOI] [PubMed] [Google Scholar]
- 12.Nickman NA, Schneider JK, Knick KA. Work activities at an ambulatory care pharmacy with an integrated model of pharmacy practice. Am J Health Syst Pharm. 1996;53: 397-402. [DOI] [PubMed] [Google Scholar]
- 13.Rascati KL, Kimberlin CL, Foley PT, Williams RB. Multidimensional work sampling to evaluate the effects of computerization in an outpatient pharmacy. Am J Hosp Pharm. 1987;44: 2060-7. [PubMed] [Google Scholar]
- 14.Hepler CD. Work analysis and time study. In: Smith MC, Brown TR (eds). Handbook of Institutional Pharmacy Practice. Baltimore, Md.: Williams & Wilkins, 1979: 84-8.
- 15.Agresti A. Categorical Data Analysis. New York: John Wiley, 1990.
- 16.Santner, TJ, Duffy DE. The Statistical Analysis of Discrete Data. New York: Springer-Verlag, 1989: 217.
- 17.Miller ME. (1996) Some techniques for the analysis of work sampling data. Stat Med. 1996;15: 607-18. [DOI] [PubMed] [Google Scholar]
- 18.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am Hosp Pharm. 1990;47: 533-43. [PubMed] [Google Scholar]
- 19.Penna RP. Pharmaceutical care: pharmacy's mission for the 1990s. Am J Hosp Pharm. 1990;47: 543-9. [PubMed] [Google Scholar]
- 20.Iglehart JK. Managed care. N Engl J Med. 1992;327: 742-7. [DOI] [PubMed] [Google Scholar]
- 21.Kohout TW, Broekemeier RL, Daniels CE. Work-sampling evaluation of an upgraded outpatient pharmacy computer system. Am J Hosp Pharm. 1983;40: 606-8. [PubMed] [Google Scholar]