Abstract
Coronoid process fractures of the ulna are difficult to treat, and are associated with stiffness, recurrent instability, and pain. Hence, treatment of coronoid process fractures are challenging for surgeons. The purpose of this study was to report the clinical outcomes of an anterior surgical approach associated with plate fixation for Regan and Morrey type II or type III fractures of the coronoid process.
We evaluated 16 consecutive patients who underwent surgical treatment for fracture of the coronoid process of the ulna from March 2012 to July 2016. Ten patients had a type II fracture, and 6 patients had a type III fracture. All patients underwent surgical treatment for coronoid process fracture through an anterior approach. While preserving the neurovascular structure, all fractures were treated with buttress plate fixation, maintaining the gap between brachial artery and median nerve. Each patient was treated with concentric reduction of both the ulnotrochlear and the radiocapitellar articulations, without any evidence of elbow instability, except 1 case, who showed some medial instability.
At the final follow-up, solid osseous union was confirmed for all coronoid fractures. The average time to radiologic union was 16.3 weeks. The mean flexion–extension arc was 124.25 ± 12.12 degree, with a mean flexion contracture of 8.25 ± 4.36 degree, and further flexion of 132.5 ± 9.31 degree. The mean forearm rotation arc was 167.81 ± 10.49 degree. Fifteen patients achieved a functional arc of motion. The mean Mayo elbow performance score was 92.1 points, with 12 excellent cases and 4 good cases.
Coronoid process fractures of the ulna can be treated successfully with plate fixation through an anterior surgical approach, which allows for accurate reduction and rigid internal fixation and early functional exercise, resulting in a reasonable outcome.
Keywords: anterior approach, coronoid process, fracture, plate fixation, the terrible triad of the elbow, treatment
1. Introduction
Coronoid process fractures of the ulna are relatively uncommon injuries, occurring in 2% to 10% of patients with elbow dislocations. Generally associated with relatively high-energy injuries, coronoid process fractures occur rarely in isolation, and are most often associated with other bony and soft tissue injuries around the elbow.[1,2] There are 3 types of coronoid process fracture, delineated by Regan and Morrey classification[3] according to the amount of process detachment from the ulna: type I (fracture of the tip), type II (up to 50% of the coronoid process detached), and type III (more than 50% detached) fractures. O’Driscoll et al[4] subsequently modified the Regan and Morrey classification based on the fracture location determined using CT scanning: type I (transverse fracture of the tip), type II (fracture of the anteromedial facet), and type III (fracture of the base) fractures.
It is well known that the larger the fragment of the coronoid process, the greater the resultant joint instability, and thus the more likely the need for surgical stabilization.[1] The incidence of elbow dislocation and poor outcome is proportional to the size of the coronoid fragment. It is generally accepted that a Regan and Morrey type I coronoid process fracture in isolation should be treated conservatively. However, for type II and type III fractures, conservative treatment may lead to a considerable risk of loss of motion or recurrent instability, and therefore, in most cases, these types II and III fractures should be treated with open reduction and internal fixation to restore elbow stability and minimize stiffness.[3]
Under optimal circumstances, a good surgical approach to the coronoid process should provide adequate extensile exposure and preservation of the neurovascular structures while permitting anatomic reduction of the intra-articular injury and early mobilization of a stable joint. Coronoid fractures can be fixed through several approaches, including lateral, medial, and anterior approaches.[1,3,5,6] The purpose of this study was to report the clinical outcomes of internal plate fixation through an anterior approach for Regan and Morrey type II and type III fractures of the coronoid process of the ulna, which we believe could be useful for these types of fractures.
2. Materials and methods
2.1. Ethical statement
This study was approved by the Ethics Committee of Hong Hui Hospital, Xi’an Jiaotong University. The patients provided written informed consent for the publication of individual clinical details and images. In addition, this study was performed in line with the international ethical guidelines for studies involving human subjects according to the Declaration of Helsinki.
2.2. Study design and patients
We enrolled 16 consecutive patients (11 males, 5 females; mean age, 34.3 years; range, 16–53 years) who had undergone open reduction and internal fixation (ORIF) in our hospital for the treatment of ulnar coronoid process fractures between March 2012 and July 2016 (Table 1). The right extremity was injured in 7 patients and the left in 9 patients. The primary goal of surgical fixation was to obtain a stable joint that permitted early movement. The inclusion criteria were a Regan and Morrey type II or type III coronoid process fracture without any other elbow fracture that would require additional fixation (i.e., distal humerus condyle fracture, radial head or neck fracture or proximal ulna fracture). Patients with Regan and Morrey type I fractures, or patients with less than 12 months of follow-up were excluded from this study. All 16 patients qualified for the final evaluation.
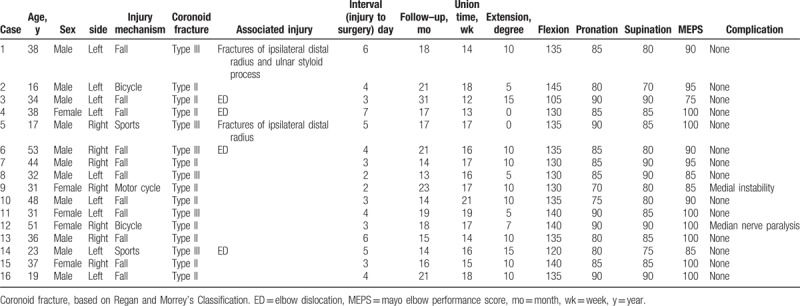
Table 1.
The summary of the cases.
The mechanisms of injury included falling on a flat ground while walking (8 cases), falling from a height (3 cases), bicycle accident (2 cases), sports injury (2 case), and motorcycle accident (1 case). Multiple injuries were present in 3 patients: 1 had a nose injury, 1 had a fracture of the ipsilateral distal radius and styloid process of the ulna, and 1 had a fracture of the ipsilateral distal radius. We used Regan and Morrey classification system to categorize the coronoid fractures.[3,7] According to this classification, 10 patients (63%) had a type II fracture and 6 patients (37%) had a type III fracture. Three of the 6 Regan and Morrey type III fractures and all 10 of the Regan and Morrey type II fractures met the classification of an O’Driscoll type II fracture, whereas the rest were O’Driscoll type III fractures. Four fractures were associated with a dislocation of the elbow joint, and these patients were treated with initial reduction in the emergency room.
All patients had closed injuries without any neurovascular complications. All 16 elbows were treated surgically at a mean of 4 days (range, 2–7 days) after the initial injury. The specific indications for surgical intervention included a displaced intra-articular fracture, and residual instability of the elbow in a functional (30–130 degree) arc of motion after closed reduction.[8]
Preoperatively, radiographic templating was undertaken to identify the exact location of the coronoid process fracture. Computed tomography (CT) and 3D CT were used to obtain additional information on fracture comminution and displacement, which may not be evident on x-rays.
2.3. Surgical technique
After anesthesia, with the patient in the supine position, the operative elbow was extended under tourniquet control. A lazy “S” type incision was created 2-fingers’ breadth proximal to the elbow flexion crease along the medial border of the biceps, and was carried across the elbow crease and distally along the midline of the forearm over the ulna about 3-fingers’ breadth distal to the flexion crease (Fig. 1A). Care was taken to work through any soft tissue disruption created by the trauma, preserving intact soft tissue structures as much as possible. The medial antebrachial cutaneous nerve was identified and protected, and was retracted medially.
Figure 1.
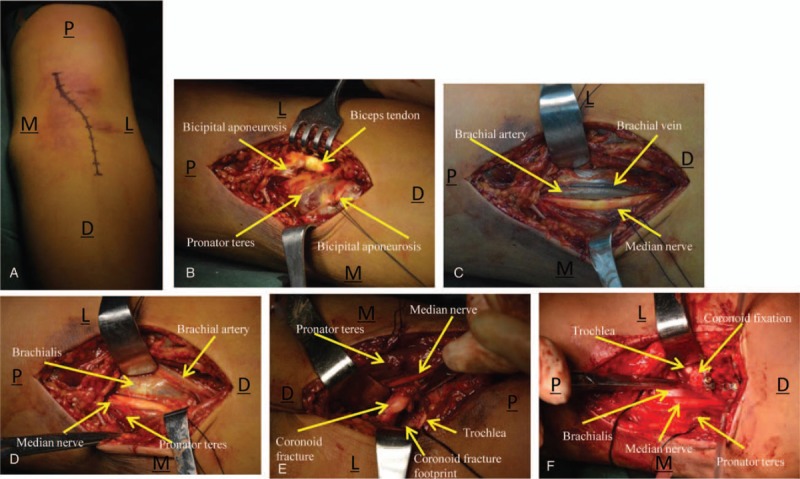
(A) A single “S”-curved incision was made along the medial border of the biceps and extended along the midline of the forearm. (B) Bicipital aponeurosis was exposed and incised. (C) Image depicts the brachial artery, brachial vein, and median nerve. (D) Brachial muscle insertion was exposed through an interval created between the brachial artery and median nerve. (E) After dissection of a small part of the lateral insertion of the brachial muscle, the coronoid fracture fragments are observable. (F) Image shows accurate reduction and rigid fixation of the coronoid process, with an intact brachialis. M = medial, L = lateral, P = proximal, D = distal.
The bicipital aponeurosis was exposed and incised perpendicular to the aponeurotic fibers; the ends were labeled to aid aponeurosis repair after coronoid fixation (Fig. 1B). The brachial fascia was then incised, and the biceps were mobilized, retracting the muscle belly laterally toward the radius where exist its tendon insertion. The pronator teres muscle belly was retracted medially, and the brachial artery and median nerve were identified in the medial side (Fig. 1C). With the elbow slightly flexed and protecting this neurovascular structure, the brachial muscle insertion was exposed through the space between the brachial artery and median nerve (median nerve and pronator teres were retracted medially, brachial artery, brachial vein and biceps were retracted laterally) (Fig. 1D), and a small part of the lateral insertion of the brachial muscle was dissected using an osteotome. This allowed us to access the area of the coronoid fracture.
The joint capsule is usually attached at the tip of the fracture fragment, and, in some cases, we needed to incise the anterior capsule longitudinally in the midline to expose the coronoid fracture. The coronoid fragment was visible with the elbow in full extension (Fig. 1E). After directly identifying the articular surface of the coronoid process by releasing part of the capsule and irrigating the area, accurate reduction of the fragments was performed. Gentle pressure was applied against the coronoid fracture with appropriate surgical tools to get fracture reduction. Before reduction and buttress plating, we ensured that the distal humerus was fully seated in the trochlear notch of the olecranon. In general, 1.5-mm Kirschner wires were used to temporarily fix the fragments in the anteroposterior direction and maintain pressure against the fragment. Then, a 2.0-mm T plate and screws were applied, and, once fixed, the K-wires were removed. The need for additional screw plating at the tip of coronoid process was assessed on a case by case basis. In this study, 5 patients required 1 or 2 screws at the tip of coronoid process (Fig. 1F).
Once bony reconstruction was complete, residual instability was evaluated through direct inspection and radiographic examination of the arm, whereas in varus and valgus, posterior stress was applied to confirm posterior instability. Detachment of the lateral ligament complex from the humerus was then repaired using absorbable sutures or suture anchors through a lateral approach. Mid-substance tears were repaired with number 1 or 2 nonabsorbable sutures. Medial collateral ligament injuries were not routinely repaired unless unacceptable valgus persisted after bony reconstruction; in this case, the medial collateral ligament was exposed and repaired using number 1 or 2 nonabsorbable sutures through a medial approach.[7]
Tourniquet was released before closure and meticulous hemostasis was obtained. The anterior capsule was routinely closed. The wounds were closed in layers.
2.4. Postoperative Management
A hinged plastic brace was applied after surgery and used for 6 weeks for all patients. The forearm was positioned in pronation or supination in cases of lateral collateral ligament or medial collateral ligament deficiency, respectively. If both the medial and the lateral collateral ligaments had been repaired, the forearm was splinted in neutral rotation. Supervised rehabilitation, including active elbow flexion and extension, was commenced on the second day after surgery, and when pain and swelling had subsided, the frequency of exercises and the range of motion (ROM) were gradually increased. Isometric upper extremity muscle contraction was also encouraged. After radiographic evidence of fracture union at 6 weeks postoperatively, the posterior splint was removed and, at 8 weeks, patients commenced active muscle strengthening exercises of the elbow with increasing loads. In addition, patients were prescribed 25 mg of indomethacin 3 times a day for 3 weeks postoperatively to prevent heterotopic ossification.[9]
2.5. Data collection and analysis
At follow-up, clinical and radiographic examinations were performed by a clinical researcher who did not take part in the treatment. The clinical evaluation consisted of ROM, Mayo Elbow Performance Score (MEPS),[10] and an examination for any detectable surgical complications. Plain radiographs were assessed for fracture union, implant loosening, heterotopic ossification, degenerative changes, and joint congruity. Intra- and postoperative complications were also documented. Confirmation of fracture union was defined as the time that the fracture showed evidence of external bridging of the callus across the fracture lines in 3 cortices on a lateral view of the elbow.[11] Statistical analysis was performed using SPSS version 17.0 software (SPSS Inc., Chicago, IL).
3. Results
All coronoid process fractures were repaired with plate and screws and showed solid osseous union on final follow-up radiographs. The average time to radiologic union was 16.3 weeks (range, 12–21 weeks).
The outcomes are shown in Table 1. The mean duration of follow-up was 18.3 months (range, 13–31 months). At the final follow-up, the mean flexion–extension arc was 124.25 ± 12.12 dgeree, the flexion contracture was 8.25 ± 4.36 degree, and further flexion was 132.5 ± 9.31 degree. The mean pronation arc was 84.06 ± 5.84 degree, supination arc was 83.75 ± 5.92 degree, and forearm rotation arc was 167.81 ± 10.49 degree. The functional arc of motion, as determined according to the criteria of Morrey et al[12] (a flexion–extension arc of 30 to 130 degree and 100 degree of forearm rotation), was achieved in 14 cases. The mean MEPS was 93.1 points (range, 75–100 points), with 12 excellent cases and 4 good cases (Fig. 2).
Figure 2.
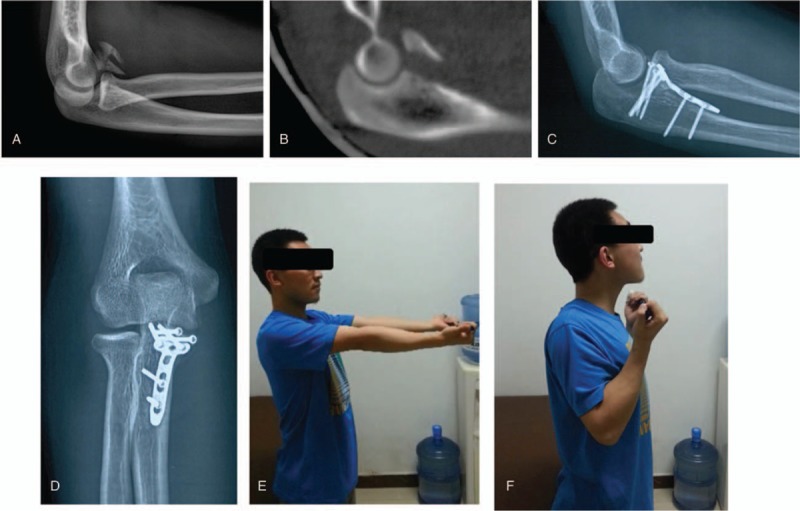
Case example. A 17-year-old boy presented with a Regan and Morrey type III coronoid process fracture and fracture of the ipsilateral distal radius. Preoperative x-ray (A) and computed tomography (B) images show a severe comminuted type III coronoid fracture. Solid union and good outcome were achieved at the 8-month follow-up (C–F).
There were no intraoperative complications. We did not observe anterior heterotopic ossification in any of the patients. There were no wound complications or implantation failure. One patient had mild pain, and 1 patient experienced transient postoperative median nerve paralysis but fully recovered by 10 weeks. All patients have returned to work, and were satisfied with the treatment.
4. Discussion
Elbow stability depends on both bony integrity and soft tissue constraint,[8] and the humeral-ulnar articulation is the most important structure for elbow stability. The ulnar coronoid process acts as an anterior buttress that resists posterior translation of the ulna and angular rotation.[13] It also provides an attachment site for the anterior joint capsule of the elbow, the brachialis muscle, and the medial ulnar collateral ligament.[14] Axial loading is considered to be the main fracture mechanism of the coronoid process, which is especially vulnerable when the elbow is flexed at 80 degree.[15] Coronoid fracture can be either an isolated injury following elbow dislocation or part of a terrible triad of the elbow.[2,16,17] There is a consensus that surgery is optimal for coronoid fracture patients with relatively large fracture fragments and significant dislocation or the presence of an unstable elbow.[1,5,7] However, the operative management of the coronoid fracture is challenging. The purpose of this study was to report the outcomes of plate fixation for the repair of coronoid process fractures of the ulna.
Ulnar coronoid process fractures can be addressed through several approaches. When a coronoid process fracture is associated with a radial head fracture, a lateral approach is very useful for fracture reduction and fixation, repair of the lateral joint capsule and the lateral collateral ligament.[5,9] However, the coronoid process cannot be exposed and fixed directly through this approach.[5] In contrast, the medial approach is recommended for treatment of comminuted and/or anteromedial coronoid fractures[18] and patients with an isolated coronoid fracture.[4] However, this approach needs extensive exposure, and it is difficult to expose the entire anterior portion of the coronoid process. Moreover, it is technically difficult to provide strong vertical compression to the fracture fragment against the base of coronoid process for stronger stability.[6]
An increasing number of studies have published their findings on operative fixation of ulnar coronoid process fractures achieved through an anterior approach.[5,6,19] This approach has several advantages. First, it provides excellent visualization of the entire articular surface of the fractured coronoid process, thereby allowing the surgeon to widely expose the joint and the coronoid process to directly reduce and fix the coronoid process fragment. Second, with the large interval, stable anatomic fixation with compression of coronoid segments can be obtained by placing anterior to posterior screws perpendicular to the fracture line;[20,21] theoretically, the coronoid fragment can be fixed to the main dorsal stock in an easier and firmer way using this approach, and, based on the specific pattern of the fragment, the surgeon can choose what type of instrumentation achieves more stability. Moreover, the surgeon may repair the anterior capsule after implantation, which could increase elbow stability. Fourth, this approach avoids damage to the normal anatomic structure of the elbow joint, such as the medial collateral ligament, the flexor-pronator muscle mass, and the ulnar nerve. And, finally, this approach allows the surgeon to fix the coronoid process through intervals between muscles without requiring wide dissection; this may help reduce the possibility of heterotrophic ossification. In this study, we selected an anterior approach to fix coronoid fractures, and we applied a buttress plate to each case. This led to anatomical restoration and definitive fixation in each patient, and good outcomes at the final follow-up. The results of 16 cases show that an anterior approach leads to good outcomes with minimal surgical and postoperative morbidity.
In previous studies,[6,19] there was a need to medially retract the median nerve and brachial artery for better visualization of the coronoid fracture, ligating any arteries or venous branches that crossed the site and impeded exposure. Moreover, in these previous studies, the authors needed to protect the lateral antebrachial cutaneous nerve. In most patients, most of the median nerve branches exist medially, and most branches of the brachial artery and vein exist laterally. Therefore, in this study, we created a space between the brachial artery and median nerve to fix the coronoid process fragments,[5] protecting the neurovascular bundle by retracting the median nerve medially and brachial artery and vein laterally; we did not need to ligate the arteries or venous branches, nor did we need to be concerned with the lateral antebrachial cutaneous nerve, unlike in other reports. We also did not split the brachialis: instead, we cut a small piece of its lateral insertion using an osteotome and retracted it laterally; this gave us an excellent visualization and maximally reduced damage to the brachialis. We used a buttress plate in each case: this could shear components and reinforce internal fixation of the coronoid fracture. We surmise that, even for comminuted fractures, the coronoid fragments can be fixed to the main dorsal stock easier and firmer using a plate and, moreover, this definitive fixation permits early functional excise and early joint motion, presumably by recruiting muscle groups that act as dynamic stabilizers of the elbow (Fig. 3).[7]
Figure 3.
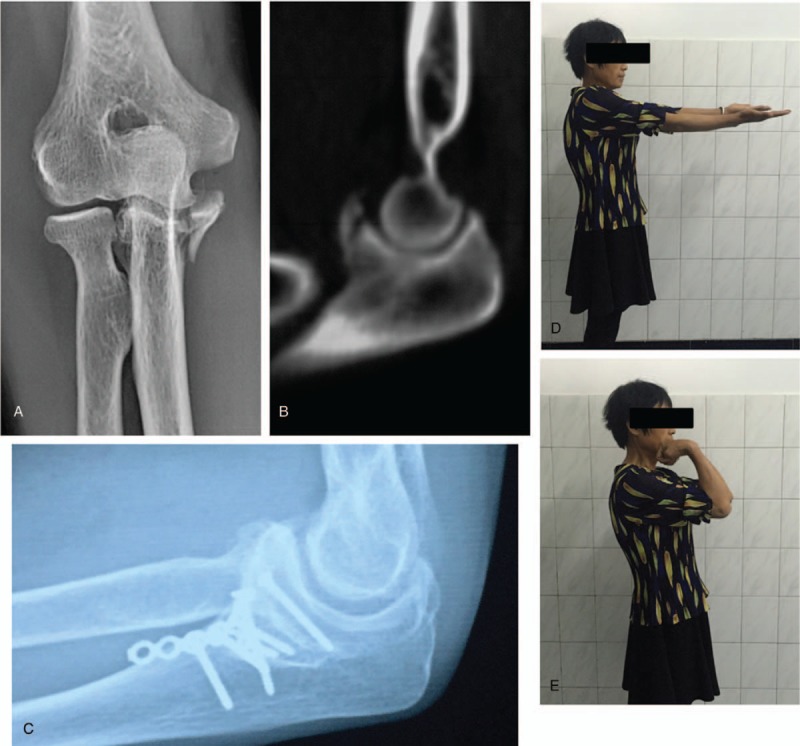
A 51-year-old woman diagnosed with a type Regan and Morrey II coronoid fracture (A, B) experienced transient postoperative median nerve paralysis but fully recovered by 10 weeks. At the final follow-up, plain roentgenograms showed bone union with good function (C). The patient was pain free and has returned to work (D, E).
Despite the advantages, there are some drawbacks of using an anterior approach. First, the brachialis insertion could not be repaired after coronoid fixation, and this might reduce forearm flexion strength. Second, the surgeon might cause damage to the brachial artery or the median nerve. However, this can be avoided by having the joint slightly flexed and with careful protection of the vessels. In this study, only 1 patient experienced transient postoperative median nerve paralysis.
The outcomes of our modified surgical approach are similar to or better than those of other reports. A report by Han et al[6] of the outcomes of 11 isolated Regan and Morrey type III fractures treated by an anterior approach showed an average of 21 months of follow-up, overall flexion arc was 127.3°, average flexion was 130.9 degree, and average pronation and supination were 73.2 and 75.9 degree, MEPS of 92.3 points; these values were very similar to ours (Table 1). Mallard et al,[22] however, reported the results of 5 patients with coronoid process fractures treated by tension band wiring with a minimum of a 1.1-year follow-up. The mean flexion–extension arc of elbow motion was 115.0 ± 9.62 degree, pronation was 86.0 ± 1.87 degree, supination was 85.0 ± 4.47 degree, and MEPS was 81. These values are considerably lower than those achieved in this study.
In this study, elbow dislocation occurred in 4 patients, and lateral collateral ligament complex repair was required for 5 cases using a lateral approach (2 with anchors and 3 with nonabsorbable sutures). We did not routinely repair the medial collateral ligament unless unacceptable valgus persisted after the coronoid process was fixed and the lateral collateral ligamentous complex was repaired:[7,23] medial collateral ligament repair with nonabsorbable sutures was required in 1 case. At the final follow-up, 1 patient showed medial instability of <10 degree, but, because the patient showed good elbow function, no further intervention was required.
There were a few shortcomings in this study. Although patients were identified from a prospectively gathered fracture database, the study was essentially retrospective, and there was no control group for comparison. Furthermore, there were only 16 valid cases in the final evaluation, with only 5 female patients. However, there is a low incidence of coronoid process fracture in our institution. The age range was large (16–53 years) and our mean duration of follow-up was only 18.3 months. It is therefore possible that there might be some biases inherent in this study. However, given our successful outcomes, with a larger sample size and a longer follow-up, future studies may provide more convincing findings. Future work may also explore an anterior approach and plate fixation for coronoid process fractures in terrible triad elbow injuries.
5. Conclusion
In this study, we found that coronoid process fractures can be treated successfully through an anterior approach using buttress plate fixation, which allows for accurate reduction and rigid internal fixation even for small bony fragments. Furthermore, buttress plate fixation through an anterior approach facilitates early functional exercise and a reasonable outcome. However, an anterior approach calls for a well-trained surgeon to avoid damage to the neurovascular structures.
Acknowledgments
The authors thank Dr. Michael McKee (St. Michael's Hospital and the University of Toronto, Toronto, Ontario, Canada) for his assistance with the manuscript.
Author contributions
Conceptualization: Jun Zhang.
Data curation: Dongxu Feng, Hao Wang.
Formal analysis: Dongxu Feng, Yangjun Zhu, Hao Wang, Jun Zhang.
Investigation: Xin Zhang.
Methodology: Xin Zhang, Yonghong Jiang.
Resources: Dongxu Feng, Yonghong Jiang, Yangjun Zhu, Shufang Wu, Kun Zhang, Zhan Wang, Jun Zhang.
Software: Dongxu Feng, Xin Zhang, Yonghong Jiang, Yangjun Zhu, Shufang Wu.
Supervision: Kun Zhang, Zhan Wang, Jun Zhang.
Validation: Hao Wang, Shufang Wu, Kun Zhang.
Writing – original draft: Dongxu Feng.
Footnotes
Abbreviations: CT = computed tomography, MEPS = Mayo Elbow Performance Score, ROM = range of motion.
D.F. and X.Z. contributed equally to this work.
The authors report no conflicts of interest.
References
- [1].Adams JE, Hoskin TL, Morrey BF, et al. Management and outcome of 103 acute fractures of the coronoid process of the ulna. J Bone Joint Surg Br 2009;91:632–5. [DOI] [PubMed] [Google Scholar]
- [2].Hotchkiss RN. Rockwood CA, Green DP, Bucholz RW, Heckman JD. Fractures and dislocations of the elbow. Rockwood and Green's Fractures in Adults, vol. 1 4th ed.Philadelphia: Lippincott-Raven; 1996. 929–1024. [Google Scholar]
- [3].Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am 1989;71:1348–54. [PubMed] [Google Scholar]
- [4].O’Driscoll SW, Jupiter JB, Cohen MS, et al. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect 2003;52:113–34. [PubMed] [Google Scholar]
- [5].Yang X, Chang W, Chen W, et al. A novel anterior approach for the fixation of ulnar coronoid process fractures. Orthop Traumatol Surg Res 2017;103:899–904. [DOI] [PubMed] [Google Scholar]
- [6].Han SH, Yoon HK, Rhee SY, et al. Anterior approach for fixation of isolated type III coronoid process fracture. Eur J Orthop Surg Traumatol 2013;23:395–405. [DOI] [PubMed] [Google Scholar]
- [7].Regan W, Morrey BF. Classification and treatment of coronoid process fractures. Orthopedics 1992;15:845–8. [DOI] [PubMed] [Google Scholar]
- [8].Pugh DM, Wild LM, Schemitsch EH, et al. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am 2004;86-A:1122–30. [DOI] [PubMed] [Google Scholar]
- [9].Zhang C, Zhong B, Luo CF. Treatment strategy of terrible triad of the elbow: experience in Shanghai 6th People's Hospital. Injury 2014;45:942–8. [DOI] [PubMed] [Google Scholar]
- [10].Morrey BF, An K-N. Morrey BF, Sanchez-Sotelo J. Functional evalution of the elbow. The Elbow and its Disorders 4th ednPhiladelphie: Saunders Elsevier; 2009. 80–91. [Google Scholar]
- [11].Kristiansen TK, Ryaby JP, McCabe J, et al. Accelerated healing of distal radial fractures with the use of specific, low-intensity ultrasound. A multicenter, prospective, randomized, double-blind, placebo-controlled study. J Bone Joint Surg Am 1997;79:961–73. [DOI] [PubMed] [Google Scholar]
- [12].Morrey BF, Askew LJ, An KN, et al. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am 1981;63:872–7. [PubMed] [Google Scholar]
- [13].Matzon JL, Widmer BJ, Draganich LF, et al. Anatomy of the coronoid process. J Hand Surg Am 2006;31:1272–8. [DOI] [PubMed] [Google Scholar]
- [14].Cage DJ, Abrams Ra, Callahan JJ, et al. Soft tissue attachments of the ulnar coronoid process: an anatomic study with radiographic correlation. Clin Orthop Relat Res 1995;320:154–8. [PubMed] [Google Scholar]
- [15].Closkey RF, Goode JR, Kirschenbaum D, et al. The role of the coronoid process in elbow stability: a biomechanical analysis of axial loading. J Bone Joint Surg Am 2000;82-A:1749–53. [DOI] [PubMed] [Google Scholar]
- [16].Shen L, Yu X, Zhong B, et al. A figure-eight suture loop with Kirschner wires for fixation of anteromedial coronoid process fractures: a case series. Int J Surg Case Rep 2017;33:130–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Wang P, Zhuang Y, Li Z, et al. Lasso plate—an original implant for fixation of type I and II Regan-Morrey coronoid fractures. Orthop Traumatol Surg Res 2017;103:447–51. [DOI] [PubMed] [Google Scholar]
- [18].Ring D, Doornberg JN. Fracture of the anteromedial facet of the coronoid process surgical technique. J Bone Joint Surg Am 2007;89(suppl 2 pt 2):267–83. [DOI] [PubMed] [Google Scholar]
- [19].Reichel LM, Milam GS, Reitman CA. Anterior approach for operative fixation of coronoid fractures in complex elbow instability. Tech Hand Up Extrem Surg 2012;16:98–104. [DOI] [PubMed] [Google Scholar]
- [20].Moon JG, Zobitz ME, An KN, et al. Optimal screw orientation for fixation of coronoid fractures. J Orthop Trauma 2009;23:277–80. [DOI] [PubMed] [Google Scholar]
- [21].Ring D, Jupiter JB. Surgical exposure of coronoid fractures. Tech Shoulder Elbow Surg 2002;3:48–56. [Google Scholar]
- [22].Mallard F, Hubert L, Steiger V, et al. An original internal fixation technique by tension band wiring with steel wire in fractures of the coronoid process. Orthop Traumatol Surg Res 2015;101(4 suppl):S211–5. [DOI] [PubMed] [Google Scholar]
- [23].Gupta A, Barei D, Khwaja A, et al. Single-staged treatment using a standardized protocol results in functional motion in the majority of patients with a terrible triad elbow injury. Clin Orthop Relat Res 2014;472:2075–83. [DOI] [PMC free article] [PubMed] [Google Scholar]


