Abstract
Introduction:
Acupoint embedment, a modified acupuncture technique, is gaining its popularity in weight control in adult obesity or overweight nowadays. The objective of this study was to investigate the clinical efficacy of acupoint embedment in weight control of adult obesity or overweight by systematically assess available randomized controlled trials (RCTs) and analyze the integrated findings. A total of 529 literatures were initially searched from the databases. Five RCTs in assessing the effect of acupoint embedment versus sham control group were identified.
Results:
A total of 219 subjects in the intervention group and 206 subjects in the control group from 5 eligible studies were eventually included in this meta-analysis. Mean body mass index (BMI) decreased 0.94 kg/m2 (95% confidence interval [CI]: −1.56 to −0.32, P = .003) more in acupoint embedment group than the sham control group. Meanwhile, subjects received acupoint embedment had 2.97 kg (95% CI: −4.44 to −1.49, P < .0001) decrease in mean body weight more than in sham control group. Both parameters were statistically significant. Adverse events including bruise, soreness and cramp, patchy skin induration, erythema were reported, yet none involved hospitalization or mortality. Interestingly, stomach meridian and spleen meridian involved in all 5 studies.
Conclusion:
This meta-analysis showed that acupoint embedment was more effective in weight control than the sham control group. Together with its convenience and low cost, acupoint embedment may be considered as an alternative treatment in weight control.
Keywords: acupoint, embedment, meridian, obesity, overweight, weight control
1. Introduction
Overweight problem is a pandemic public health issue in the world. Despite the fact that some developing countries are facing a double burden disease of overweight and underweight, the majorities are overwhelmed by overweight and obesity.[1–3] It is well-documented that overweight and obesity are associated with a number of diseases.[4] So far, there is no single universal adopted definition or measurement of overweight/obesity. Body mass index (BMI), percent body fat (F%), weight for height and waist circumference are commonly used in the assessment of overweight or obesity and its impact on human's well-being.[5] Among them, BMI is most widely and frequently adopted. It is an index defined by one's weight in kilogram divided by his height in meter square (kg/m2). Using the World Health Organization (WHO) standard for Asian populations, people were categorized as underweight (BMI < 18.5 kg/m2), normal weight (18.5 kg/m2 ≤ BMI < 23 kg/m2), overweight (23 kg/m2 ≤ BMI < 25 kg/m2), and obese (BMI ≥ 25 kg/m2).[6]
A fact sheet distributed by the WHO in 2016 stated that worldwide obesity has more than doubled since 1980. An effective weight control strategy is an important health concern. A combination of reducing calorie diet and increasing physical activity is recommended in weight reduction with substantial evidence.[7–10] However, the compliance of people with this behavioral therapy is an issue. As a result, alternative therapies are urgently needed. Various pharmacotherapy and surgery have been investigated for their effectiveness and safety in weight control, still clear evidence is lacking. Even though bariatric surgery does show encouraging results in long-term weight control, it should only be considered in patients with BMI > 40 kg/m2.[11,12]
In traditional Chinese medicine (TCM), obesity is believed a sequel of sedentary lifestyle and overconsumption of oily, sweet foods. It seems in accord with the understandings from Western medicine about obesity. It is a problem when calorie input significantly outweighs output.
There are several subtypes of obesity in TCM. It involves dysfunctional organs, including spleen, stomach, liver, kidney or any combination of them. A single or multi-organs dysfunction results in disturbance in Qi, imbalance between Yin and Yang. This leads to an accumulation of pathological by-products, a unique concept in Chinese medicine, which include phlegm, wet, and bruise. To treat obesity, these pathological by-products must be got rid of. TCM practitioners then focus on restoration of organ function and equilibrium of Yin and Yang by prescribing Chinese herb and acupuncture. Both have been practiced from generations to generations. Acupoint embedment, a modified acupuncture technique, on the other hand, is gaining its popularity in weight control since 21st century. Instead of inserting needles for a short period of time into specific acupoints that can regulate Yin Yang and Qi, a short segment of absorbable suture thread is implanted into designated acupoints according to the subtype of obesity. Absorbable thread is burrowed under the skin under aseptic procedure and is then left till it naturally dissolves in situ. The thread takes 1 to 2 weeks to be absorbed. Acupoints chosen are distributed in anterior abdominal wall, thighs and legs for the majority of cases.
Numerous studies were carried out to investigate the efficacy of acupoint embedment in weight control. However, there was still insufficient evidence to draw definitive conclusion as most of the studies were small in sample size or may be carried out with possible methodological deficiencies.[13–15] A few systematic reviews and meta-analysis were published in the past.[16–20] However, they included studies with various control groups, such as auricular acupuncture, moxibustion, oral medication, diet, exercise, and so on. Acupoints chosen for implantation or for simple acupuncture, even in the same study, were merely the same. Readers should interpret the results with caution. This meta-analysis selected high quality RCTs aimed at studying the clinical efficacy of acupoint embedment per se in weight control in adult simple obesity or overweight. The blinding method involves sham will be the control group. Safety and practical use of acupoint embedment also be studied.
2. Materials and methods
2.1. Inclusion and exclusion criteria
2.1.1. Participants
We included only RCTs that assessed the beneficial effects of acupoint embedment in patients with all types of overweight or obesity (BMI ≥ 23 kg/m2 or F% ≥ 35). Studies involve participants with both genders, including all ethnicities.
2.1.2. Intervention
We included studies that applied acupoint embedment as an experimental intervention for weight control regardless of suture material used.
2.1.3. Control
Studies applied sham embedment for weight control with the blinding method were included in the control group. Studies involving acupoint embedment for weight control but without control arm were excluded. In addition, studies involving sham embedment for weight control that was not masked from participants in the control group were also excluded.[21]
2.1.4. Outcomes
Primary outcomes were the mean difference in BMI and body weight before and after treatment. Secondary outcomes included adverse events, frequency of acupoints used and the time schedule of acupoint embedment.
2.2. Literature search
Databases searched were PubMed, EMBASE, Cochrane Central Register of Controlled Trials, Allied and Complementary Medicine (AMED), WanFang Data, China Journal Net (CJN), HyRead, and Airiti Library. A literature search was conducted from their respective earliest publications date to April 1, 2018. Language included both English and Chinese. The following keywords in English, including (catgut or thread or suture) and (embed∗ or implant∗ or acup∗) and (obesity or overweight or weight) and (randomized controlled trail or randomized controlled study) were used. Chinese words with meaning acupoint embedment and obesity are used in Chinese databases.
2.3. Data extraction and quality assessment
For each literature, information concerning authors, date of publication, study location, sample size, characteristic of the participants in both intervention and control groups, BMI, body weight before and after treatment, acupoints chosen, duration of treatment, and adverse events was collected. The information was extracted by 2 independent reviewers; the discrepancies were resolved through discussion and came to a conclusion by a third reviewer. No ethical approval is necessary due to its exclusive use of secondary data.
2.4. Literature quality assessment and risk of bias assessment
The quality of the included studies was assessed by the risk of bias assessment tool, which assesses the selecting bias, performance bias, detection bias, attrition bias, reporting bias and other bias in the studies.[22]
2.5. Statistical analysis
The Cochrane Collaboration's software program, RevMan 5.3 for Windows (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark), was used to conduct all statistical analysis. The significance of the heterogeneity among the pooled studies was determined by I2 statistic. If a significant heterogeneity with I2 > 50% was detected, a random-effects model was adopted instead of a fixed-effect model. Risk of publication bias was assessed by a funnel plot. Continuous data were presented as mean difference, with 95% confidence intervals (CIs).
3. Results
3.1. Study selection
A total of 529 literatures were initially searched from the databases. 405 of them were found duplicated or irrelevant. 86 out of 124 potentially eligible studies were excluded for 1 or more than 1 of the following reasons: different age group, different control group, different outcome measurement, not RCT. 43 potential literatures left. However, only 5 literatures carried out sham implantation in the control group, whereas the acupoints applied were exactly the same as the intervention group. All of them were published in Chinese. One was conducted in Taiwan while the rest were from Mainland China. A flow diagram of literature search and process is shown in Figure 1.
Figure 1.
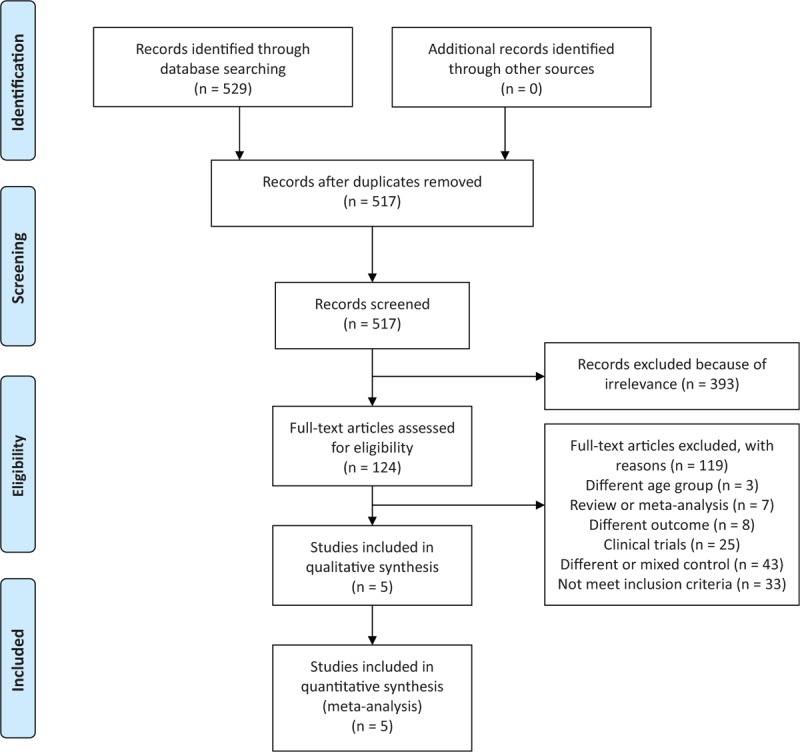
Flow diagram of literature search and process.
3.2. Characteristics of eligible studies
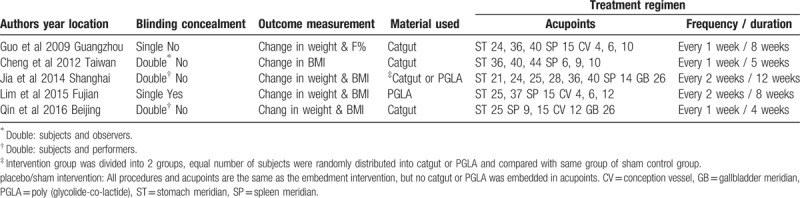
The characteristics of included studies were shown in Table 1. A total of 405 participants were involved with aged 19 to 65.
Table 1.
Characteristic of study methods and treatment regimens.
3.3. Meta-analysis
Heterogeneity in the meta-analysis of mean change in BMI and body weight were high, with I2 = 93% and I2 = 90% respectively as shown in Figures 2 and 3. The random-effects model was adopted. Mean BMI decrease 0.94 kg/m2 (95% CI: −1.56 to −0.32, P = .003) more in acupoint embedment than in the sham group. At the same time, subjects received acupoint embedment had 2.97 kg (95% CI: −4.44 to −1.49, P < .0001) decrease in body weight than in the control group. Both parameters were statically significant. There was no evidence of publication bias in this meta-analysis as funnel plots (data not shown).
Figure 2.
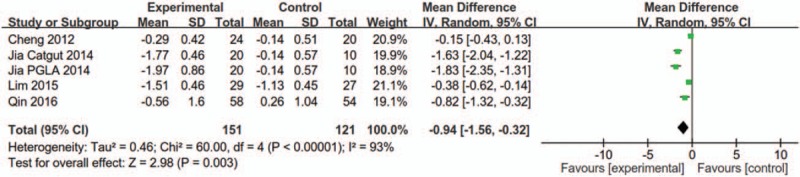
Forest plot for change in mean BMI. BMI = body mass index.
Figure 3.
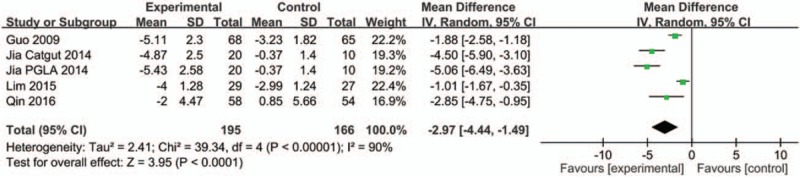
Forest plot for change in mean body weight.
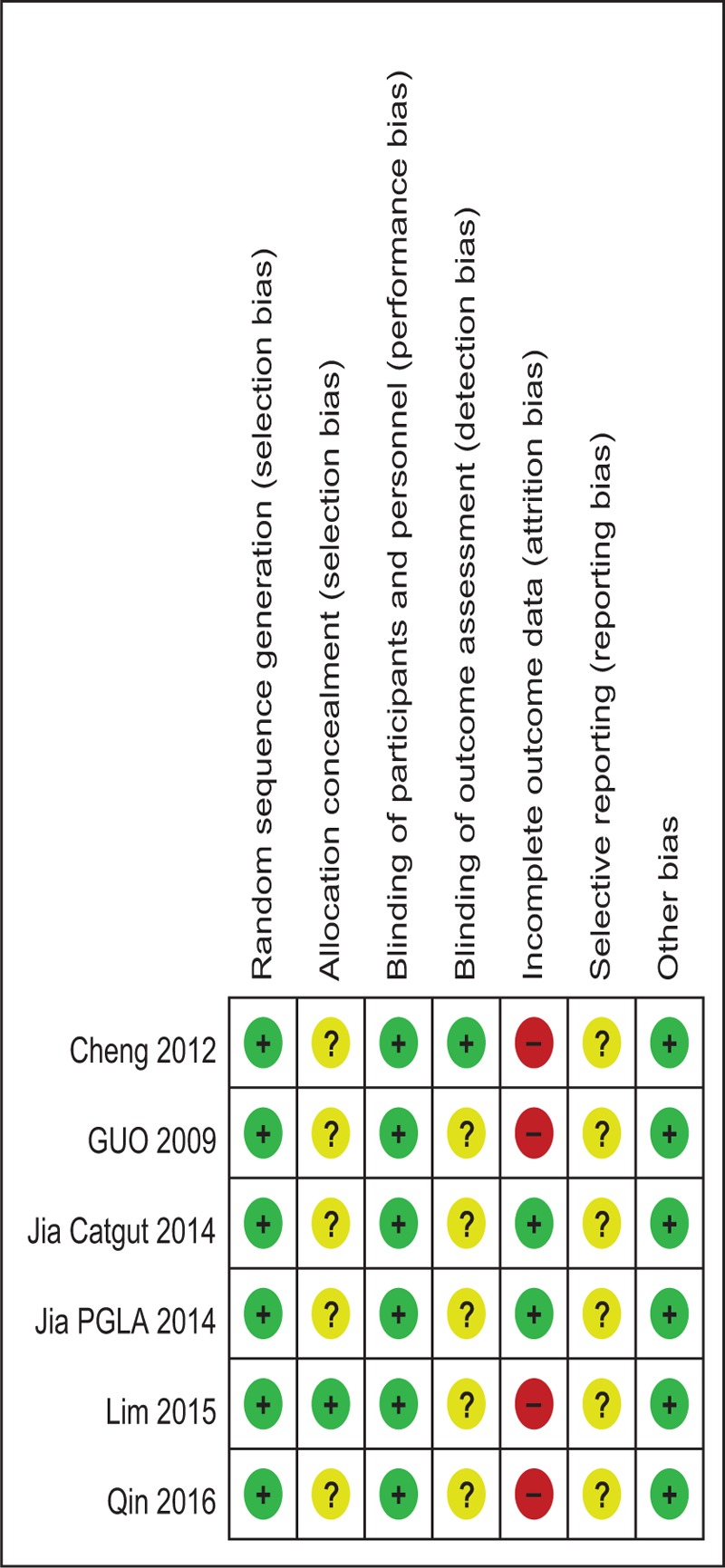
3.4. Risk of bias
Risk bias of studies was assessed using the Cochrane Risk of Bias Assessment Tool in the Cochrane Handbook 5.2.0 (http://handbook.cochrane.org/, Chapter 8). A review of the authors’ judgments about each risk of bias item showed as percentages across all of the included RCTs (Table 2). All studies described a random component in the sequence generation process using a computer for random number generation.[23–27] Allocation concealment was achieved in 1 trial.[26] All studies were assessed as appropriate double blinding of participants and personnel for performance.[23–27] Four studies provided detailed information for double blinding during performance but insufficient information for the blinding of outcome assessment.[23,24,26,27] Four studies were in high risk of bias due to incomplete outcome data.[24–27] Risk of bias was summarized in Table 3.
Table 2.
Risk of bias graph.
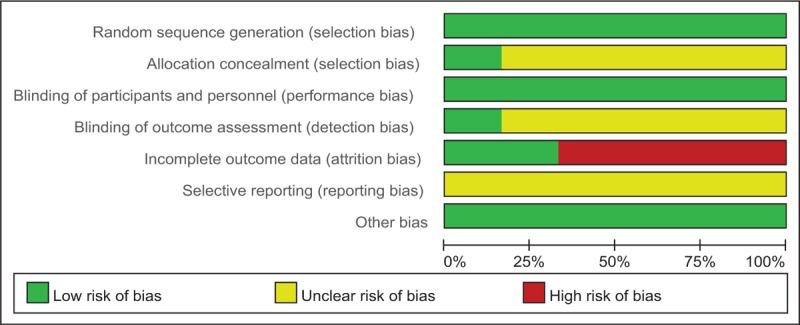
Table 3.
Risk of bias summary.
3.5. Practical procedure
Stomach meridian (ST) and spleen meridian (SP) involved in all 5 studies. Conception vessel (CV) and gallbladder meridian (GB) were the second most involved meridians. However, the acupoints chosen were not identical even for same meridian. ST40 appeared most frequently. It was employed in 80% of the studies. 60% of the studies had a thread implanted at ST25, ST36, and SP15. ST24, SP9, CV4, CV6, CV12, and GB26 appeared in more than 1 study. 1 up to 2 cm long thread was implanted in each acupoint in the intervention groups. All subjects received treatment once every 1 or 2 weeks. Duration of treatment lasted from 5 to 12 weeks, with an average of 8.2 ± 3.4 weeks. The overall dropout was low in both intervention and control group. A total of 16 subjects and 21 subjects dropped out before treatment completed in the intervention and sham control groups respectively. The average dropout rate in the intervention and sham control groups was 5.8 ± 6.6% and 9.9 ± 10.3%. Among these 5 studies, none of the subjects was dropped out in Jia et al.[23]
3.6. Adverse events
Soreness, cramp, bruise, patchy skin induration, erythema, decrease appetite, increase bowel movement were encountered by some subjects, mainly in the intervention group. All except 1 completed treatment despite the above adverse effect. None of the subjects involved hospitalization or mortality.
4. Discussion
Statistically significant decreases in both BMI and body weight significantly decreased after acupoint embedment. Mean BMI decreased 0.95 kg/m2 (95% CI: 0.3–1.61, P = .004) more in the acupoint embedment group than the sham control group. Meanwhile, subjects received acupoint embedment had 3 kg (95% CI: 1.47–4.52, P = .0001) decrease in mean body weight more than in the sham control group. Individual studies were described as below.
Guo et al recruited 150 subjects with F% > 35 from a hospital in Guangzhou. Software PEMS 3.1 was adopted to generate the random allocation sequence.[24] 2 groups of 6 specific acupoints were implanted in the alternate week for 8 weeks. Blinding applied to all subjects, but not performer nor observer. There was a 0.15 kg (95% CI: 0.13–0.43) decrease in the mean body weight in the intervention group than in the sham group.
Cheng et al recruited 20 to 40 years old female subjects from a hospital in Taiwan with BMI 24 to 33 kg/m2.[25] 57 subjects were allocated randomly to the intervention or sham group with the help of a random-number table. Blinding applied to all subjects and observers. Short fragment of catgut was implanted into 2 different sets of acupoints in an alternate week basis for 5 weeks. A decrease of the mean BMI (0.29 ± 0.42 kg/m2, P = .005) was shown between the intervention and control groups. However, the mean difference in body weight did not show any statistical significance.
Jia et al recruited 60 subjects in Shanghai with their BMI ≥ 23 kg/m2.[23] 20 of them were randomly allocated to catgut implantation, another 20 subjects for poly (glycolide-co-lactide) (PGLA) implantation. The rest of 20 subjects were randomly distributed to sham as the control group to both the catgut and PGLA groups. 2 cm long absorbable suture thread, catgut or PGLA, was implanted to 8 different acupoints every 2 weeks in the intervention groups for 12 weeks. Both subjects and performers were not aware of which group they belonged to. There were 1.63 kg/m2 (95% CI: 1.31–1.95) and 1.83 kg/m2 (95% CI: 1.38–2.28) decrease in the mean BMI of the catgut and PGLA groups than in the sham group. A significant weight decrease of 4.5 kg (95% CI: 3.24–5.76) and 5.06 kg (95% CI: 3.77–6.35) were found in the catgut implantation and PGLA implantation groups than in the sham group.
Lim et al recruited 60 subjects, 30 subjects in each group, with BMI ≥ 24 kg/m2 from a hospital in Fujian.[26] Two cm long PGLA were implanted into 7 acupoints in the intervention group every 2 weeks for 8 weeks. The difference in mean BMI and weight reduction between the intervention and sham groups were 0.38 kg/m2 (95% CI: 0.14–0.62) and 1.01 kg (95% CI: 0.35–1.67), respectively.
Qin et al recruited 120 subjects with BMI ≥ 25 kg/m2 from a hospital in Beijing. 61 subjects were allocated to the intervention group and 59 subjects to the sham group by a random table.[27] One cm long PGLA were implanted into 6 acupoints every 1 week for 4 times. All participants were blinded to which group they were allocated, so as the performers. Mean BMI significantly decreased 0.82 kg/m2 (95% CI: 0.32–1.32) in the intervention group than in the sham group. A significant decrease of 2.85 kg (95% CI: 0.95–4.75) in mean body weight was shown in the intervention group than in the sham group.
Three studies used catgut and 1 opted for PGLA for implantation material. On the other hand, Jia et al applied catgut and PGLA separately for acupoint embedment as 2 independent intervention groups and compared the results with the same control group.[23] All control groups were sham implantation, they underwent the same procedure as intervention groups except that catgut or PGLA implantation was actually not implanted. All participants were randomly distributed into either intervention or control group and all of them were blinded about the procedures. In the studies of Jia et al and Qin et al, even the performers, that is, the acupuncturists had no idea if absorbable thread was implanted.[23,27] They were given an empty insertion needle in blind. On the other hand, Cheng et al had their observer blinded in outcome measurement.[25]
All the included studies were RCTs. They all clearly described how random sequences were generated. A stringent randomization method allowed each individual had the same chance of allocation to either group. Possible confounders were thus equally distributed in the intervention and sham groups. The observed difference between the 2 groups could then be interpreted more confidently. It was more desirable if allocation concealment was adequately carried out as in Lim et al, in order to minimize selection bias.[26] All studies did make comparisons in the main characteristics of subjects including their weight or BMI between the intervention and sham groups. Results showed no statistically significant difference. Comparability of 2 groups in each study was assured. Blinding is a measure to reduce ascertainment bias. All studies adopted at least single blinded approach to subjects. Three of them were double blinded RCTs. Cheng et al had blinding implemented to observers while Jia et al and Qin et al had performers blinded instead.[23,25,27] Observation bias and performer bias were minimized accordingly. Measurement of outcome was unified in Cheng et al and Lim et al, this again helped to reduce observation bias.[25,26]
Apart from Lim et al, none explained how they achieved or intended to achieve allocation concealment.[26] Inadequate allocation concealment was subjected to selection bias. The highest dropout rate was detected in Cheng et al, up to 28%.[25] Although the other 4 studies had a dropout rate ranged from 0% to 13%, none of them gave details of missing data. There was no comparison between the dropout group and the completion group. Intention to treat for outcome analysis was not performed in any single study. More efforts needed to prevent possible attrition bias.
Apart from Guo et al, all studies defined overweight and obesity by BMI. Their BMI readings were at least 23 kg/m2.[24] Definition of obesity or overweight differed in each study. 4 of them recruited subjects with BMI ≥ 23 kg/m2, which was classified as overweight in the Asian population, and 1 with F% ≥ 35. Both criteria were widely adopted in assessing overweight or obesity. All subjects involved in the 5 studies were volunteers. Only Cheng et al explicitly indicated the number and reason of withdrawal in the eligible population before allocation, though a baseline characteristics comparison between these 2 groups was not done.[25] Volunteer bias was not addressed in all studies. Adverse events, a secondary outcome of this meta-analysis, related to acupoint embedment or sham should be clearly documented. Sore, bruises were most frequently encountered. Cheng et al reported 1 case failed to complete the intervention course because of severe pain at the implantation site.[25] However, the exact number of subjects who had experienced adverse events was not clear, no matter in the intervention or control groups.
Acupoints chosen consistently followed the line of thought in treating obesity in Chinese Medicine's perspective. ST and SP were employed in every treatment regimen among the included studies. These 2 meridians worked closely with each other in the absorption and transport of nutrients. CV and GB were involved in 3 out of 5 treatment regimens. They were compatible with the concept of Qi regulation in treating obesity.
Although the pathogenesis of obesity in TCM is different from that in Western medicine, the mechanism of acupuncture in weight control has been studied in a scientific way. A large number of experiments were carried out in animal models in weight control by different acupuncture techniques, including auricular acupuncture, electroacupuncture (EA) or manual acupuncture. The mechanism of catgut implantation for weight control may be associated with rebalancing peripheral and hypothamic leptin in obesity and enhancing insulin sensitivity, in turn, increasing the glucose metabolism.[28,29] Gao et al found that EA and acupoint catgut-embedding could regulate the lipid metabolic disorders in rats with obesity through enhancing the expression of peroxisome proliferator-activated receptor (PPAR)-γ mRNA in adipose tissues, activating the activities of lipoprotein lipase and hepatic lipase, as well as decreasing the levels of total cholesterol and low-density lipoprotein cholesterol in serum.[30] Further study reported that EA stimulation of ST36 and SP6 could reduce body weight in rats with simple obesity, EA intervention could downregulate the suppressor of cytokine signaling 3 and PPAR-γ mRNA expression in epididymis adipose tissue.[31] On the other hand, a beneficial neuro-hormonal changes were demonstrated which influenced the body's homeostatic mechanisms, suggesting a decrease in appetite might account for weight reduction mediated by the neuro-hormonal pathway.[32–35]
Promising results were also shown in human studies. Acupuncture was proven to be associated with a decrease in leptin, a hormone produced physiologically to regulate energy balance by inhibiting hunger.[36–40] Chen et al also reported that both acupoint catgut-embedding and acupuncture had a definite therapeutic effect in the treatment of simple obesity, which is closely associated with the decline of serum insulin, glucose and TNF-α levels, as well as the decrease of insulin resistance.[41] These reports were compatible with the clinical findings in this meta-analysis.
To our knowledge, it was the first meta-analysis showing that acupoint embedment was effective in weight reduction with a statistically significant decrease in mean BMI and mean body weight when compared to the sham control group. We conducted an extensive literature search. Apart from literature published in English, databases in Chinese were searched meticulously. One important strength of this meta-analysis focused in high quality RCTs. Cautious implementation of randomization and blinding in these 5 studies helped to eliminate or reduce the confounder and placebo effect. It made interpretation of the observed result more reliable. The locations of the included studies were dispersedly distributed in China. They involved cities with moist subtropical climate such as Guangzhou, as well as places with dry and cold climate such as Beijing. Results derived from subjects from different geographic regions led to a better external validity to the general population. Catgut might be an option for acupoint embedment years ago. PGLA was found more frequently used in the past few years. This meta-analysis included both absorbable materials for comparison with sham. It allowed generalization of results to target population in the long run.
On the other hand, there were few limitations of this study. Though with much effort in literature search, it is obvious that those unpublished studies and publications not in English and Chinese language were not included. Besides, it is possible that the published studies were different from unpublished studies. Inadequacy in concealment of treatment allocation and failure in the management of missing data are some concerns. Acupoint embedment procedure, such as the length of absorbable thread used and the depth of implantation, were not properly mentioned and should be standardized. The random-effects model was used during data analysis for a high heterogeneity in the meta-analysis. It was difficult to perform subgroup analysis due to the small number of subjects in this study. The longest treatment received was 12 weeks and no further follow-up data was collected. Persistency of the beneficial effect was not certain. The long term effect of acupoint embedment in weight reduction in adult obesity or overweight should be further studied. Recording risk or adverse effects of acupoint embedment, apart from mortality and hospitalization, was incomplete. Practical advice in performing acupoint embedment could not be concluded as there was no standardized procedure (such as length of thread or depth of implantation).
4.1. Challenges
It is well recognized that the prevalence of obesity and overweight is rapidly increasing. It becomes a leading health problem worldwide. This problem affects patient's own quality of life, and also exerts a great financial burden to public health system.[42,43] The patients’ compliance on diet and physical exercise will affect much on the effectiveness of weight control. Pharmacotherapies and bariatric surgery for weight loss, on the other hand, are still controversial for their effectiveness and safety.
Acupoint embedment is considered as an alternative approach regarding its less attendance to care providers when compared to other forms of acupuncture. A cost-benefit analysis showed that catgut-embedding had lower cost and fine economics benefit, yet its effectiveness was comparable to EA in treating obesity.[44] Catgut was once the only material used in acupoint embedment. PGLA, a synthetic absorbable suture material, is going to replace catgut for its comparably same efficacy and less side effect caused.[45] Regardless of the suture material being used, it intends to exert a continuous, long-lasting and more intensive stimulation at acupoints when comparing to simple acupuncture. It takes 1 to 2 weeks for the suture thread to be absorbed in situ.
5. Conclusion
Both the mean BMI and mean body weight in adult overweight or obesity significantly decreased when comparing the acupoint embedment group with the sham control group in this meta-analysis. ST and SP are most commonly used meridians in the studies; CV and GB were the second most involved meridians. However, it is not easy to draw a definitive conclusion on the clinical efficacy of acupoint embedment in the weight control of adult overweight and obesity due to the limitations of the small sample sizes in the studies. Well-designed multi-center large scale RCT is warranted to settle the controversies in weight control by acupoint embedment.
Author contributions
Conceptualization: William C. Cho.
Formal analysis: Ching Li, Hai-Yong Chen.
Methodology: Ching Li, Hai-Yong Chen.
Validation: William C. Cho, Hai-Yong Chen.
Writing – original draft: Ching Li, William C. Cho.
Writing – review & editing: William C. Cho, Hai-Yong Chen.
Footnotes
Abbreviations: BMI = body mass index, CV = conception vessel, EA = electroacupuncture, F% = percent body fat, GB = gallbladder meridian, PGLA = poly (glycolide-co-lactide), PPAR = peroxisome proliferator-activated receptor, RCT = randomized controlled trial, SP = spleen meridian, ST = stomach meridian, TCM = traditional Chinese medicine, WHO = world heath organization.
The authors have no conflicts of interest to disclose.
References
- [1].Haslam DW, James WPT. Obesity. Lancet 2005;366:1197–209. [DOI] [PubMed] [Google Scholar]
- [2].Razak F, Corsi DJ, Slutsky AS, et al. Prevalence of body mass index lower than 16 among women in low- and middle-income countries. JAMA 2015;314:2164–71. [DOI] [PubMed] [Google Scholar]
- [3].Vos T, Barber RM, Bell B, et al. Global, regional and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet 2015;386:743–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Malnick SD, Knobler H. The medical complications of obesity. QJM: Int J Med 2006;99:565–79. [DOI] [PubMed] [Google Scholar]
- [5].Hubbard VS. Defining overweight and obesity: what are the issue. Am J Clin Nutr 2000;72:1067–8. [DOI] [PubMed] [Google Scholar]
- [6].International Obesity TaskForce. The Asia-Pacific perspective: Redefining obesity and its treatment. IASO International Association for the Study of Obesity 2000, p. 18. [Google Scholar]
- [7].Andersen RE, Wadden TA, Bartlett SJ, et al. Effects of lifestyle activity vs structured aerobic exercise in obese women: a randomized trial. JAMA 1999;281:335–40. [DOI] [PubMed] [Google Scholar]
- [8].Cho WC, Yue KK, Leung AW. An outline of obesity and its therapy by Chinese and western medicine. Chin J Tradit West Med 2004;24:3073–5. [Google Scholar]
- [9].Murphy MH, Blair SN, Murtagh EM. Accumulated versus continuous exercise for health benefit: a review of empirical studies. Sport Med 2009;39:29–43. [DOI] [PubMed] [Google Scholar]
- [10].Wadden TA, Webb VL, Moran DH, et al. Lifestyle modification for obesity: new development in diet, physical activity, and behavior therapy. Circulation 2012;125:1157–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kasama K, Mui W, Lee WJ, et al. IFSO-APC consensus statement 2011. Obes Surg 2012;22:677–84. [DOI] [PubMed] [Google Scholar]
- [12].Stegenga H, Haines A, Jones K, et al. Identification, assessment and management of overweight and obesity: summary of updated NICE guidance. BMJ 2014;349:g6608. [DOI] [PubMed] [Google Scholar]
- [13].Yang F. Clinical study on acupoint catgut embedding for treatment of simple obesity. Zhongguo Zhen Jiu 2005;25:237–9. [PubMed] [Google Scholar]
- [14].Shi Y, Zhang L, Zhao C, et al. Comparison of therapeutic effects of acupuncture-cupping plus acupoint catgut embedding and electroacupuncture on simple obesity of stomach and intestine excess-heat type. Zhongguo Zhen Jiu 2006;26:547–50. [PubMed] [Google Scholar]
- [15].Yan RH, Liu XM, Bai J, et al. Clinical efficacy of simple obesity treated by catgut implantation at acupoints. Chin J Integr Med 2015;21:594–600. [DOI] [PubMed] [Google Scholar]
- [16].Lim L, Tan Y. Acupoint embedding in treating obesity: a meta-analysis. Chin Manip Rehabil Med 2011;62:56–7. [Google Scholar]
- [17].Zhang XP, Jia CS, Wang JL, et al. Systematic review on the effectiveness of embedding catgut therapy for simple obesity. World J Acupunct-Moxib 2013;23:53–8. [Google Scholar]
- [18].Cheng L, Dong Q, Tang QQ. Catgut implantation at acupoint for treatment of simple obesity cases-quantitative analysis and study of its clinical application. J Liaoning Univ TCM 2014;16:1673–842. [Google Scholar]
- [19].Guo T, Ren Y, Kou J, et al. Acupoint catgut embedding for obesity: systematic review and meta-analysis. Evid based Complement Alternat Med 2015;2015:40191420 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Liu MY, Xu GG. Systematic review of acupoint embedding in treating obesity. China Prac Med 2016;11:278–9. [Google Scholar]
- [21].Boutron I, Estellat C, Guittet L, et al. Methods of blinding in reports of randomized controlled trials assessing pharmacologic treatments: a systematic review. PLoS Med 2006;3:e425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org. Accessed on 13 August, 2018. [Google Scholar]
- [23].Jia YF, Mao HJ, Guo CZ, et al. Double-blinded randomized control trial in treating obesity by acupoint implantation. Liaoning J Tradit Chin Med 2014;41:72–4. [Google Scholar]
- [24].Guo SW, Tong YF, Chen L, et al. Clinical trial of acupoint embedding in treating simple obesity. Chin Manip Qi Gong Ther 2009;25:11–3. [Google Scholar]
- [25].Cheng SC, Lee FW, Cheung WH, et al. Single blinded randomized control trial of acupoint embedment in simple obesity female. J Chin Med 2012;23:223–33. [Google Scholar]
- [26].Lim SM. Acupoint Catgut Embedding and Sham Acupoint Catgut Embedding in Treating Simple Obesity [unpublished dissertation]. Fujian University of Traditional Chinese Medicine; 2015. [Google Scholar]
- [27].Qin WL, Wang ZX, Yang WX, et al. Clinical study on abdominal type of simple obesity treated with acupoint catgut embedding therapy. Beijing J Tradit Chin Med 2016;35:207–10. [Google Scholar]
- [28].Yan R, Liu X, Bai J, et al. Influence of catgut implantation at acupoints on leptin and insulin resistance in simple obesity rats. J Tradit Chin Med 2012;32:477–81. [DOI] [PubMed] [Google Scholar]
- [29].Chang SL, Lin KJ, Lin RT, et al. Enhanced insulin sensitivity using electroacupuncture on bilateral Zusanli acupoints (ST 36) in rats. Life Sci 2006;79:967–71. [DOI] [PubMed] [Google Scholar]
- [30].Gao L, Kong XJ, Shi X. Effects of electroacupuncture and acupoint catgut-embedding on mRNA expression of lipid metabolism gene PPAR-gamma and related lipase of rats with simple obesity. Zhongguo Zhen Jiu 2011;31:535–8. [PubMed] [Google Scholar]
- [31].Gao J, Tang CL, Liu RJ, et al. Effect of different intensities of electroacupuncture stimulation on expression of SOCS-3 and PPAR-gamma mRNA in adipose tissues of obesity rats. Zhen Ci Yan Jiu 2013;38:31–4. [PubMed] [Google Scholar]
- [32].Lui Z, Sun F, Su J, et al. Study on action of acupuncture on ventromedial nucleus of hypothalamus in obese rats. J Tradit Chin Med 2001;21:220–4. [PubMed] [Google Scholar]
- [33].Wei Q, Cai H, Liu Z, et al. Study of acupunctures effect on the function of the raphe nuclei of fat rats. Int J Clin Acupunct 2005;14:267–72. [Google Scholar]
- [34].Cabioglu MT, Gundogan N. The efficacy of electroacupuncture for weight loss changes plasma lipoprotein A, apolipoprotein A and apolipoprotein B levels in obese women. Am J Chin Med 2008;36:1029–39. [DOI] [PubMed] [Google Scholar]
- [35].Wen CK, Lee TY. Electroacupuncture decreases the leukocyte infiltration to white adipose tissue and attenuates inflammatory response in high fat diet-induced obesity rats. Evid Based Complement Alternat Med 2014;2014:47397811 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Baocun Y, Caixia Z, Jing Y, et al. Observation and mechanism exploration of acupuncture on body weight reduction. J Tradit Chin Med 2006;26:250–3. [Google Scholar]
- [37].Darbandi M, Darbandi S, Mobarhan MG. Effects of auricular acupressure combined with low-calorie diet on the leptin hormone in obese and overweight Iranian individuals. Acupunct Med 2012;30:208–13. [DOI] [PubMed] [Google Scholar]
- [38].Darbandi S, Darbandi M, Mokarram P. Effects of electroacupuncture on plasma leptin concentrations in obese and overweight people in Iran: a randomized controlled trial. Alternat Ther Health Med 2013;19:24–31. [PubMed] [Google Scholar]
- [39].Belivani M, Dimitroula C, Katsiki N, et al. Acupuncture in the treatment of obesity: a narrative review of the literature. Acupunct Med 2013;31:88–97. [DOI] [PubMed] [Google Scholar]
- [40].Sui Y, Zhao HL, Wong VC, et al. A systematic review on use of Chinese medicine and acupuncture for treatment of obesity. Obes Rev 2012;13:409–30. [DOI] [PubMed] [Google Scholar]
- [41].Chen F, Wu S, Zhang Y. Effect of acupoint catgut embedding on TNF-alpha and insulin resistance in simple obesity patients. Zhen Ci Yan Jiu 2007;32:49–52. [PubMed] [Google Scholar]
- [42].Ko GT. The cost of obesity in Hong Kong. Obes Rev 2008;9:74–7. [DOI] [PubMed] [Google Scholar]
- [43].Huang LC, Pan WY. Comparison of effect and cost-benefit analysis between acupoint catgut-embedding and electroacupuncture on simple obesity. Zhongguo Zhen Jiu 2011;31:883–6. [PubMed] [Google Scholar]
- [44].Cho WC, Yue KK, Leung AW. An outline of obesity and its therapy by Chinese and Western medicine. Chin J Tradit West Med 2004;5:3073–5. [Google Scholar]
- [45].He YN. A review of PGLA model of medical materials in clinical catgut embedding application. Adv Mater Res 2014;1096:224–7. [Google Scholar]


