Supplemental Digital Content is available in the text
Keywords: airway management, cardiopulmonary resuscitation, endotracheal intubation, videolaryngoscopy
Abstract
Background:
Endotracheal intubation (ETI) can be challenging, especially in life-threatening situations such as cardiopulmonary resuscitation (CPR). Videolaryngoscopes aim to ease ETI, but effort is still widely discussed. This study intended to investigate 2 different airway devices regarding the success rate of ETI during ongoing chest compressions.
Methods:
This randomized, cross-over, multi-center manikin trial included 85 experienced paramedics actively working in the emergency medicine service. After a standardized training session, all paramedics underwent 3 airway scenarios using both, direct laryngoscopy using a Macintosh blade and videolaryngoscope (the UEScope): normal airway without chest compressions, normal airway with uninterrupted chest compressions, and difficult airway with uninterrupted chest compressions. The primary outcome was successful ETI, defined as successful placement of the endotracheal tube within the manikin's trachea. Secondary outcomes were number of intubation attempts, time to successful ETI, time to best glottis view, best percent of glottic opening, best glottic view score (Cormack and Lehane), occurrence of dental trauma, ease of use, and willing to reuse in real-life situations.
Results:
The UEScope provided a better glottis visualization, and higher first pass intubation success rate compared to direct laryngoscopy in all 3 scenarios. The overall intubation success was higher, and the intubation time was shorter with the UEScope in scenario B and scenario C, but was comparable in scenario A. Dental compression occurred less often using the UEScope and paramedics rated intubation using the UEScope easier compared to direct laryngoscopy in all 3 airway scenarios.
Conclusion:
In simulated CPR scenarios, intubation with the UEScope resulted in a better glottis visualization, a higher intubation success, and a shorter intubation time compared to Macintosh laryngoscope (MAC). Moreover, in situations where the airway is difficult for ETI especially by the paramedic, the UEScope would be a better choice than the MAC. Further studies are needed to confirm these results in real-life patients.
1. Introduction
Cardio pulmonary resuscitation (CPR) is indicated in patient suffering from cardiac arrest and is associated with high mortality, although survival improved over the last few decades. Early start of CPR, rapid defibrillation, and high quality of advanced life support including sufficient airway management are the main cornerstones of current CPR guidelines.[1–3] Ventilation and oxygenation of patients can be life-saving, especially if adequately performed by experienced and skilled CPR providers. Endotracheal intubation (ETI) was considered the gold standard of airway management during CPR to prevent from pulmonary aspiration and provide a constantly protected airway.[4–6] If performed, ETI should not cause any interruption of ongoing chest compressions exceeding 5 seconds, as even a short period of so called “no-flow” or “hands-off” time causes significant decrease of coronary perfusion and is therefore associated with worse outcome.[1] Consequently, ETI during ongoing chest compression is therefore fundamental, but requires high level of personal skills and experience.[4,5,7,8] In addition, airway management in the emergency setting is especially challenging due to facial trauma, pharyngeal obstruction, limited access to the patient and/or airway, and necessity to stabilize the cervical cord.[6,9–12]
Videolaryngoscopy was introduced into the clinical setting in the late 1990s with the ultimate goal to ease ETI, although the benefits are still discussed controversially.[13–17] Several different types and models of video laryngoscopes are currently available, all of them having particular advantages or specific disadvantages.[18] The UEScope (Zhejiang UE Medical Corp, Zhejiang, China; Fig. 1) is a recently introduced videolaryngoscope, and is equipped with a tilt and rotatable 2.5′′ full color display, a high-resolution camera and Macintosh and/or Miller blades in different sizes for the use in patients from neonates to adults.[18–20] The intubation technique with this device is similar to other videolaryngoscopes and is based on insertion along the midline of the mouth without requiring sweeping the tongue.[21]
Figure 1.
UESCope videolaryngoscope.
If the UEScope actually ease ETI during ongoing CPR was not investigated so far. Therefore, the aim of this manikin study was to investigate the clinical impact of the UEScope, when compared to direct laryngoscopy. Specifically, we tested the hypothesis, that the UEScope is associated with a higher rate of successful ETI during ongoing chest compression, compared to direct laryngoscopy.
2. Methods
2.1. Study design and settings
This study was approved by the Institutional Review Board of International Institute of Rescue Research and Education (Approval: 43.10.2017.IRB). Informed consent was obtained from each paramedic prior to the study.
This randomized, cross-over, multi-center trial was performed at 3 different Polish center (Warsaw, Poznan, and Katowice) among participants of the Advanced Cardiovascular Life Support course during 2017 to 2018. Only fully educated paramedics, currently actively working in the emergency medicine service were included in this study. All paramedics are considered at least moderately experienced (defined by more than 50 ETIs) using direct laryngoscopy, but unexperienced in using any videolaryngoscope. This might be surprising, but videolaryngoscopy has not been introduced into Polish out-of-hospital emergency medicine yet. Overall, 84 paramedics met these criteria's and were included into this study on a voluntary basis.
2.2. Training
Each paramedic underwent a standardized 20-minute training session, covering principles of out-of-hospital airway management, and a presentation of the UEScope video laryngoscope, given by the same lecturer in all courses. After the presentation, direct laryngoscopy using a Macintosh blade and UEScope guided intubation was presented and explained in detail in a manikin. Afterwards, all paramedics were allowed to practice and familiarize with both airway devices, using a Laerdal Airway Management Trainer (Laerdal, Stavanger, Norway).
2.3. Simulation scenarios
Cardiac arrest was simulated using the advanced patient simulator SimMan 3G (Laerdal), placed on the floor. The LUCAS3 (Physio-Control, Redmond, WA) was used to generate standardized chest compressions.
The paramedics were asked to perform ETI in 3 different scenarios:
-
1.
Scenario A: Normal airway without chest compression.
-
2.
Scenario B: Normal airway with ongoing chest compression.
-
3.
Scenario C: Difficult airway with uninterrupted chest compression. In this scenario, an ongoing CPR with difficult airway was simulated by inflating the tongue resulting in a Mallampati score class 3.
All intubations were performed with a standard 7.5-mm ID (Mallinckrodt, Covidien, Dublin, Ireland) single lumen tube. The tubes were previously prepared in all intubation attempts with a hockey-stick shaped, lubricated stylet by a highly experienced researcher. Once the manikin's trachea was intubated, the tube cuff was inflated using a 10-mL syringe and the Ambu resuscitator bag (Ambu, Copenhagen, Denmark) was connected and a ventilation breath was given.
All paramedics had to perform ETI with both airway devices (direct laryngoscopy using a Macintosh blade-Macintosh laryngoscope [MAC]-and UEScope) in each scenario, resulting in 6 overall scenarios for each paramedics. Between the scenarios, paramedics were able to rest for at least 10 minutes. The order of the intubation technique and the scenarios were randomized by the Research Randomizer software.[22] Details of the randomization are demonstrated in the Supplementary Figure 1.
2.4. Outcomes
The primary outcome was successful ETI, defined as successful placement of the endotracheal tube within the manikin's trachea.
Secondary outcomes were number of intubation attempts, time to successful ETI, time to best glottis view, best percent of glottic opening (POGO), best glottic view score (Cormack and Lehane), occurrence of dental trauma, ease of use and willing to reuse in real-life situations.
2.5. Measurements
Successful ETI was confirmed by a researcher by the ability to ventilate the manikin lungs with a self-inflating bag. The following criteria were defined for a failed intubation: more than 3 unsuccessful intubation attempts, intubation procedure exceeding 120 seconds or unrecognized esophageal intubation.
During the examination phase, all intubation procedures were recorded by a camcorder (HERO 5; GoPro Inc, San Mateo, CA). Each time variable was precisely identified by reviewing the records. Time to intubation was defined as the time from grabbing the laryngoscope to successful tracheal intubation confirmed by the inflation of the lungs. “Time to best glottis view” was defined as the time from the grabbing the laryngoscope to the stating of the participants “I see the vocal cords.”
The POGO score (0%, 25%, 50%, 75%, and 100%) quantifies the percentage of visualization of the glottis.[23] A POGO score of 100% indicates a visualization of the entire glottis (from the anterior commissure of the vocal cords to the interarytenoid notch), while a POGO score of 0% indicates that no visualization of laryngeal structures was achieved. After each intubation, paramedics were asked to rate the POGO score.
Additionally, the glottic view was documented according to the Cormack–Lehane score.[24]
Dental trauma was recorded by a single independent investigator during each intubation attempt.
After each intubation, the participants were asked to describe the difficulty of the intubation on a rating scale graded from 1 (very easy) to 10 (very difficult), as well as the willingness to reuse the device in a real-life situation reaching from 1 (would never use it again) to 10 (would like to use it).
2.6. Statistical analysis
Sample size calculation was performed using G∗Power 3.1 with a 2-tailed t test (Cohen d: 0.8, alpha error: 0.05, power: 0.95). According to the calculation a minimum of 54 participants were necessary. We ended up included 84 paramedics, as we included every eligible participants of the Advanced Cardia Arrest Courses.
Normal distribution was assessed using the Kolmogorov–Smirnov test. Categorical data are reported as frequency (n) and percent (%) and numerical data as median and interquartile range (IQR). Fisher exact test was used to compare categorical data. Numerical data were analyzed using the Mann–Whitney U test and/or the Kruskal–Wallis test. Statistical significance was set as a 2-tailed P-value of <.05. All statistical analyses were performed with the statistical package Statistica v.12EN (StatSoft, Tulusa, OK).
3. Results
Eighty-five paramedics (63 males and 22 females) with a mean age of 36 ± 6 years, and a mean work experience of 11 ± 5 years were included into this study. All 85 paramedics, performed all 6 scenarios each, resulting in an overall of 692 intubation procedures.
3.1. Scenario A: normal airway without chest compressions
Intubation success at the first attempt was higher using the UEScope compared to MAC (100% vs 87%, P < .001). For both devices, the overall intubation success was 100%. Using the UEScope a significantly better glottis visualization was achieved regarding the Cormack–Lehane grade and the POGO score (Fig. 2). Time to best glottis view (Fig. 3), and intubation time (Fig. 4) were comparable for both devices. Dental compression indicating dental trauma occurred more often using the MAC. Participants assessed the intubation with the UEScope as easier compared to MAC reflecting in the higher willingness to reuse the UEScope (Table 1).
Figure 2.
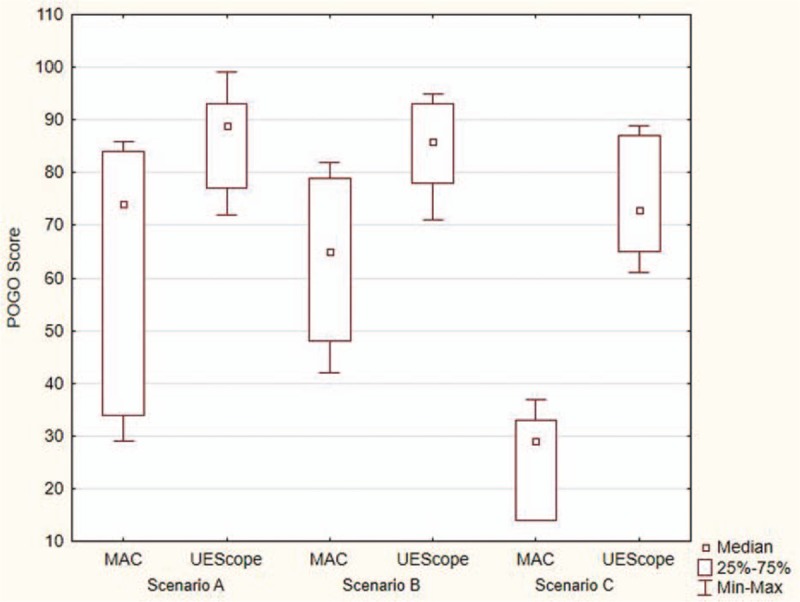
Percentage of glottis opening (POGO) score depending on intubation scenario.
Figure 3.
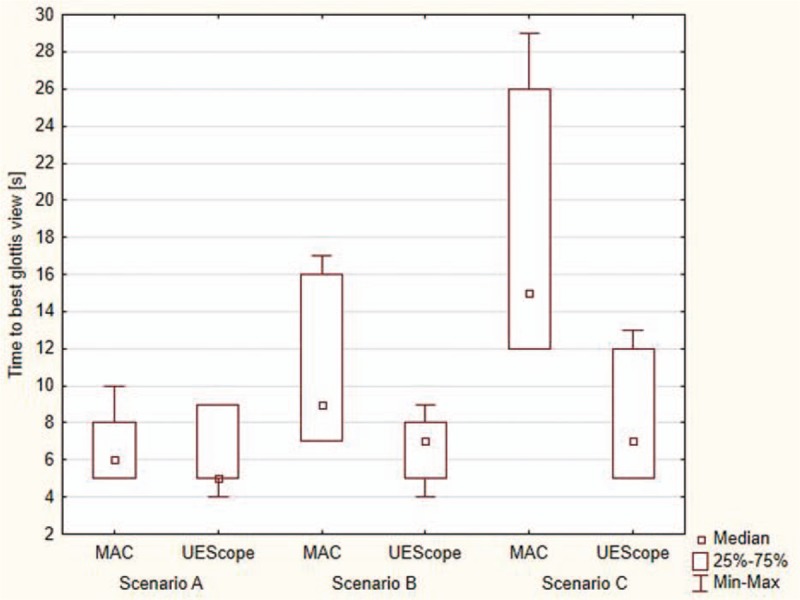
Time to best glottis view during different study scenarios.
Figure 4.
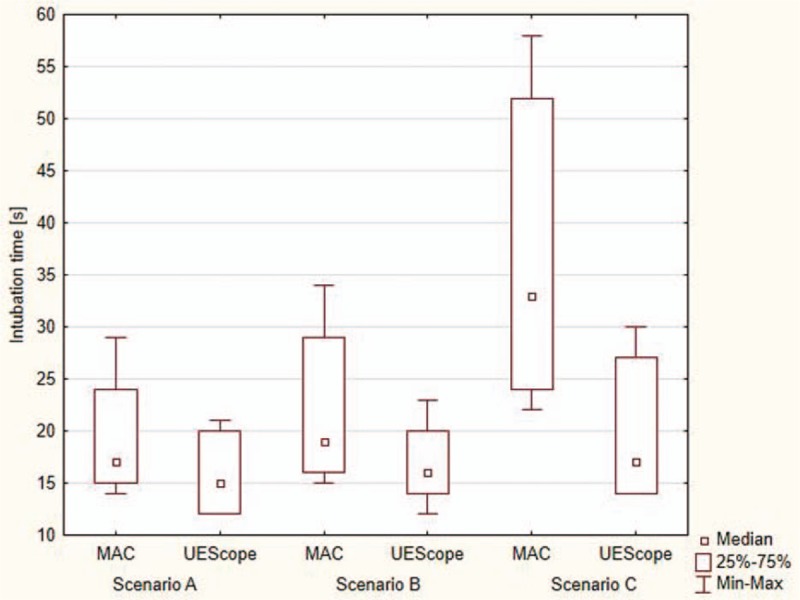
Intubation time during different study scenarios.
Table 1.
Endotracheal intubation parameters in scenario A – normal airway without chest compressions.

3.2. Scenario B: normal airway with uninterrupted chest compressions
In simulated CPR situations with normal airways, intubation success at the first attempt as well as the overall intubation success was significantly higher using the UEScope compared to MAC (94% vs 53%, P = .001; 100% vs 91%, P = .031, respectively). A significantly better glottis visualization was achieved with the UEScope (Fig. 2). Time to best glottis view and intubation time were significantly shorter for the UEScope (Figs. 3 and 4). Dental compression indicating dental trauma occurred more often using the MAC. Participants assessed the intubation with the UEScope as much easier compared to the MAC reflecting also in the higher willingness to reuse the UEScope (Table 2).
Table 2.
Endotracheal intubation parameters in scenario B: normal airway with uninterrupted chest compressions.

3.3. Scenario C: difficult airway with uninterrupted chest compressions
In simulated CPR with a difficult airway, the UEScope was superior to the MAC in all analyzed parameters (Table 3): Intubation success at the first attempt as well as the overall intubation success was significantly higher using the UEScope compared to MAC (93% vs 17%, P < .001; 100% vs 75%, P < .001, respectively). Using the UEScope a significantly better glottis visualization was achieved (Fig. 2). Time to best glottis view and intubation time were significantly shorter for the UEScope (Figs. 3 and 4). Dental compression indicating dental trauma occurred more often using the MAC. Participants assessed the intubation with the UEScope as much easier compared to the MAC reflecting also in the higher willingness to reuse the UEScope (Table 3).
Table 3.
Endotracheal intubation parameters in scenario C: difficult airway with uninterrupted chest compressions.

4. Discussion
The aim of this study was to compare the rate of successful intubations during ongoing chest compression with two different airway devices in a manikin setting. The main findings of our study are that ETI using a videolaryngoscope resulted in higher first intubation attempt, better glottis visualization, shorter intubation time, and less dental trauma compared to direct laryngoscopy throughout all 3 airway scenarios tested in our study.
Interruptions of chest compressions should be limited as much as possible, as any interruption is associated with decrease of coronary perfusion and consequently with poor outcome.[25] According to current CPR guidelines, chest compressions should only paused for a maximum of 5 seconds, and only if considered necessary by the intubating healthcare provider.[26]
Several studies investigated the impact on airway management and the associated interruption of chest compressions so far.[4,5,27,28] One of the few studies investigating interruptions of chest compression and airway management, if performed by paramedics was published by Wang et al.[29] The authors observed a median time to intubation of 46 seconds and the associated interruption of chest compressions was 109 seconds. Consequently, ETI contributed for nearly 23% of all interruptions of chest compressions, a rate which is considered unacceptable. Successful ETI requires high level of skills and experience, and it was reported several times, that highly experienced airway experts as anesthesiologists are able to intubate more or less during ongoing chest compressions.[27] However, paramedics are much less experienced and prolonged interruption of chest compressions seems reasonable.
Several studies from a wide range of different clinical settings and different providers, reported, that videolaryngoscopes provide better glottis visualization.[13–18] If better glottis visualization leads to minimized interruptions, especially if performed by less to moderate experienced airway providers like paramedics remains currently unclear.
The mismatch between better glottis visualization and rate of intubation success might be attributed to the different shapes of currently available video laryngoscopes. Each video laryngoscope requires a modification from the intubation technique used with the direct laryngoscope. The angulated blade design of UEscope is significantly different from those of sharply angulated video laryngoscopes such as Glidescope (Verathon Medical, Bothell, WA), McGrath (Aircraft Medical, Edinburgh, Scotland), and Storz D-Blade (KARL STORZ Endoscopy, Tuttlingen, Germany). A recent review reported that the UEScope may provide more benefits than other video laryngoscopes in patients with normal and difficult airways.[19]
The UEScope was previously investigated in 3 RCT, including more than 600 patients. The UEScope consistently provided better laryngeal view, a shorter time to laryngeal visualization and intubation compared to direct laryngoscopy.[19] In contrast to these results in real-life patients our manikin study showed comparable results in overall intubation success and time to glottis visualization and intubation in airway scenario A.
Results of our study clearly support previous findings that use of the videolaryngoscope improves better glottis visualization. Our data also support that using the videolaryngoscope was associated with higher success rate with the initial intubation attempt, and also in overall intubation success rate. The major strength of this study is that all intubation attempts were performed during ongoing chest compressions, and consequently any intubation attempt was associated with any interruption of chest compressions.
In accordance to our result showing less dental trauma with the UEScope, videolaryngoscopy was shown to be less associated with traumatic complications compared to direct laryngoscopy.[13]
Our study has several limitations. First, this study was performed in manikins, which may not reflect actual real-world CPR conditions. Due to ethical consideration, this study is not feasible in real patients having CPR. Furthermore, manikins study allows standardization, which would never be possible in real CPR settings. However, results obtained in manikin studies have to be confirmed in real patients.
5. Conclusion
As a conclusion, the videolaryngoscope used in this study provided much better glottis visualization, a higher overall, and first-pass intubation success and a shorter intubation time compared to direct laryngoscopy. The results of this study are limited by the fact, that it was performed in manikins instead of real patients. However, this study supports the assessment, that videolaryngoscopy might be an attractive alternative to direct laryngoscopy during ongoing chest compressions. Moreover, in situations where the airway is difficult for ETI especially by the paramedic, the UEScope would be a better choice than the MAC.
Author contributions
Conceptualization: Lukasz Szarpak, Agnieszka Madziala, Kurt Ruetzler.
Data curation: Lukasz Szarpak.
Formal analysis: Lukasz Szarpak, Alexander Kaserer.
Investigation: Lukasz Szarpak, Agnieszka Madziala, Marek Dabrowski, Marcin Madziala.
Methodology: Lukasz Szarpak, Ruslan Yakubtsevich, Kurt Ruetzler.
Project administration: Lukasz Szarpak.
Resources: Lukasz Szarpak, Agnieszka Madziala.
Software: Lukasz Szarpak.
Supervision: Lukasz Szarpak, Jerzy Robert Ladny.
Validation: Lukasz Szarpak, Jacek Smereka, Alexander Kaserer, Kurt Ruetzler.
Visualization: Lukasz Szarpak, Michael Czekajlo.
Writing – original draft: Lukasz Szarpak, Agnieszka Madziala, Jacek Smereka, Alexander Kaserer, Marcin Madziala, Ruslan Yakubtsevich, Jerzy Robert Ladny.
Writing – review & editing: Lukasz Szarpak, Agnieszka Madziala, Michael Czekajlo, Jacek Smereka, Alexander Kaserer, Marek Dabrowski, Kurt Ruetzler.
Supplementary Material
Footnotes
Abbreviations: CPR = cardiopulmonary resuscitation, ETI = endotracheal intubation, ID = internal diameter, IQR = interquartile range, MAC = Macintosh laryngoscope, POGO = percentage of glottis opening.
Approval was granted by the Institutional Review Board of International Institute of Rescue Research and Education (Approval: 43.10.2017.IRB).
Informed consent was obtained from all individual participants included in the study.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: adult advanced cardiovascular life support: 2015 American Heart Association Guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015;132:S444–64. [DOI] [PubMed] [Google Scholar]
- [2].Ong MEH, Perkins GD, Cariou A. Out-of-hospital cardiac arrest: prehospital management. Lancet 2018;391:980–8. [DOI] [PubMed] [Google Scholar]
- [3].Szarpak Ł, Czyżewski Ł, Kurowski A, et al. Comparison of the TruView PCD video laryngoscope and macintosh laryngoscope for pediatric tracheal intubation by novice paramedics: a randomized crossover simulation trial. Eur J Pediatr 2015;174:1325–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Ruetzler K, Gruber C, Nabecker S, et al. Hands-off time during insertion of six airway devices during cardiopulmonary resuscitation: a randomised manikin trial. Resuscitation 2011;82:1060–3. [DOI] [PubMed] [Google Scholar]
- [5].Gruber C, Nabecker S, Wohlfarth P, et al. Evaluation of airway management associated hands-off time during cardiopulmonary resuscitation: a randomised manikin follow-up study. Scand J Trauma Resusc Emerg Med 2013;21:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Piegeler T, Neth P, Schlaepfer M, et al. Advanced airway management in an anaesthesiologist-staffed Helicopter Emergency Medical Service (HEMS): a retrospective analysis of 1047 out-of-hospital intubations. Resuscitation 2016;105:66–9. [DOI] [PubMed] [Google Scholar]
- [7].Goliasch G, Ruetzler A, Fischer H, et al. Evaluation of advanced airway management in absolutely inexperienced hands: a randomized manikin trial. Eur J Emerg Med 2013;20:310–4. [DOI] [PubMed] [Google Scholar]
- [8].Szarpak L, Truszewski Z, Czyzewski L, et al. A comparison of the McGrath-MAC and Macintosh laryngoscopes for child tracheal intubation during resuscitation by paramedics. A randomized, crossover, manikin study. Am J Emerg Med 2016;34:1338–41. [DOI] [PubMed] [Google Scholar]
- [9].Thoeni N, Piegeler T, Brueesch M, et al. Incidence of difficult airway situations during prehospital airway management by emergency physicians - a retrospective analysis of 692 consecutive patients. Resuscitation 2015;90:42–5. [DOI] [PubMed] [Google Scholar]
- [10].Smereka J, Ladny JR, Naylor A, et al. C-MAC compared with direct laryngoscopy for intubation in patients with cervical spine immobilization: a manikin trial. Am J Emerg Med 2017;35:1142–6. [DOI] [PubMed] [Google Scholar]
- [11].Bielski K, Smereka J, Ladny JR, et al. A comparison of the Macintosh laryngoscope and blind intubation via I-gel in intubating an entrapped patient: a randomized crossover manikin study. Am J Emerg Med 2017;35:787–9. [DOI] [PubMed] [Google Scholar]
- [12].Ladny JR, Smereka J, Szarpak L. Comparison of the Trachway video intubating stylet and Macintosh laryngoscope for endotracheal intubation. Preliminary data. Am J Emerg Med 2017;35:574–5. [DOI] [PubMed] [Google Scholar]
- [13].Pieters BMA, Maas EHA, Knape JTA, et al. Videolaryngoscopy vs. direct laryngoscopy use by experienced anaesthetists in patients with known difficult airways: a systematic review and meta-analysis. Anaesthesia 2017;72:1532–41. [DOI] [PubMed] [Google Scholar]
- [14].Lewis SR, Butler AR, Parker J, et al. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation: a Cochrane Systematic Review. Br J Anaesth 2017;119:369–83. [DOI] [PubMed] [Google Scholar]
- [15].Sulser S, Ubmann D, Schlaepfer M, et al. C-MAC videolaryngoscope compared with direct laryngoscopy for rapid sequence intubation in an emergency department: a randomised clinical trial. Eur J Anaesthesiol 2016;33:943–8. [DOI] [PubMed] [Google Scholar]
- [16].Jiang J, Ma D, Li B, et al. Videolaryngoscopy does not improve the intubation outcomes in emergency and critical patients - a systematic review and meta-analysis of randomized controlled trials. Crit Care 2017;21:288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lascarrou JB, Boisrame-Helms J, Bailly A, et al. Videolaryngoscopy vs direct laryngoscopy on successful first-pass orotracheal intubation among ICU patients: a randomized clinical trial. JAMA 2017;317:483–93. [DOI] [PubMed] [Google Scholar]
- [18].Ruetzler K, Imach S, Weiss M, et al. Comparison of five video laryngoscopes and conventional direct laryngoscopy: investigations on simple and simulated difficult airways on the intubation trainer. Anaesthesist 2015;64:513–9. [DOI] [PubMed] [Google Scholar]
- [19].Xue FS, Yang BQ, Liu YY, et al. Current evidences for the use of UEscope in airway management. Chin Med J (Engl) 2017;130:1867–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].UE Medical Devices I. Available at http://www.uescope.com/product.html. Accessed March 3, 2018. [Google Scholar]
- [21].Alter SM, Haim ED, Sullivan AH, et al. Intubation of prehospital patients with curved laryngoscope blade is more successful than with straight blade. Am J Emerg Med 2018;S0735-6757. [DOI] [PubMed] [Google Scholar]
- [22].Urbaniak GC. PS: Research Randomizer (Version 4.0) [Computer software]. Retrieved on June 22, 2013. Available at http://www.randomizer.org/. [Google Scholar]
- [23].Biro P, Ruetzler K. The reflective intubation manoeuvre increases success rate in moderately difficult direct laryngoscopy: a prospective case-control study. Eur J Anaesthesiol 2015;32:406–10. [DOI] [PubMed] [Google Scholar]
- [24].Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984;39:1105–11. [PubMed] [Google Scholar]
- [25].Yeung J, Chilwan M, Field R, et al. The impact of airway management on quality of cardiopulmonary resuscitation: an observational study in patients during cardiac arrest. Resuscitation 2014;85:898–904. [DOI] [PubMed] [Google Scholar]
- [26].Soar J, Nolan JP, Bottiger BW, et al. Adult advanced life support section C: European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation 2015;95:100–47. [DOI] [PubMed] [Google Scholar]
- [27].Schuerner P, Grande B, Piegeler T, et al. Hands-off time for endotracheal intubation during CPR is not altered by the use of the C-MAC video-laryngoscope compared to conventional direct laryngoscopy. A randomized crossover manikin study. PLoS One 2016;11:e0155997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Wiese CH, Bahr J, Popov AF, et al. Influence of airway management strategy on “no-flow-time” in a standardized single rescuer manikin scenario (a comparison between LTS-D and I-gel). Resuscitation 2009;80:100–3. [DOI] [PubMed] [Google Scholar]
- [29].Wang HE, Simeone SJ, Weaver MD, et al. Interruptions in cardiopulmonary resuscitation from paramedic endotracheal intubation. Ann Emerg Med 2009;54:645–52. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


