Abstract
Introduction:
Herlyn–Werner–Wunderlich syndrome (HWWS) is a rare congenital abnormality of the urogenital tract characterized by uterus didelphys, obstructed hemivagina, and ipsilateral renal agenesis. It is usually diagnosed after menarche, with a clinical presentation of dysmenorrhea, recurrent abdominal pain, and irregular menses. However, it is rare to diagnose it during pregnancy, subsequently resulting in spontaneous abortion.
Case presentation:
A 22-year-old Chinese woman with HWWS whose left uterine pregnancy underwent spontaneous abortion presented with a right perforated obstructed hemivagina and right renal agenesis. The right vaginal septum was resected and the hematocolpos was drained, thereby relieving lower abdominal pain and preserving future fertility.
Conclusion:
Co-presentation of unilateral renal agenesis and uterus didelphys should encourage clinicians to rule out HWWS. Early diagnosis and subsequent treatment can avoid possible serious complications.
Keywords: abortion, Herlyn–Werner–Wunderlich syndrome, pregnancy, renal agenesis, uterus didelphys
1. Introduction
Herlyn–Werner–Wunderlich syndrome (HWWS) is a rare congenital abnormality of the urogenital tract. The precise etiology and pathogenesis of HWWS are still unknown.[1] HWWS is caused by the anomalous development of Müllerian and Wolffian ducts,[2] and its estimated occurrence is between 0.1% and 3.8%.[3] Patients with HWWS usually have uterus didelphys and obstructed hemivagina paired with ipsilateral renal agenesis. Clinical presentation is usually described with dysmenorrhea, abdominal pain, pelvic mass, and foul mucopurulent discharge (purulent vaginal discharge). It is usually misdiagnosed and mistreated owing to rare and variant clinical manifestations, understandably resulting in severe complications. We report here a case of HWWS in a young Chinese woman with a right, perforated obstructed hemivagina whose left uterine pregnancy was spontaneously aborted. The unique feature of this case is that the diagnosis was made during the pregnancy, which eventually ended in spontaneous abortion.
2. Case report
A 22-year-old primigravida Chinese woman presented to the department of obstetrics and gynecology of our hospital, with complains of lower abdominal pain accompanied by vaginal bleeding for duration of 2 days at 80 days gestation. Her white blood cell count was 12.59 × 109/L and beta-human chorionic gonadotropin levels were 315.90 mIU/mL. She underwent menarche at 13 years of age, and her menses were regular with 10 period days and 30-day interval with mild dysmenorrhea. She revealed that she was aware of an absent right kidney and double cervix, as diagnosed by another clinical institute 3 years ago. After 41 days of menopause, ultrasound (US) examination confirmed the presence of a double uterus, with the pregnancy sac in the left uterus. A pelvic ultrasound revealed uterus didelphys, normal-sized uteri, 1.4-cm-thick endometrium, and normal adnexal region (Fig. 1A); an echogenic structure measuring 6.5 × 5.5 cm within strong echo was observed in the vagina (Fig. 1B). Subsequently, an abdominal computed tomography (CT) was performed to better characterize the pelvic anatomy (Fig. 1C and D) and confirm the absence of the right kidney (Fig. 1E). The external genitalia appeared normal; however, a strong suspicion of HWWS was presented. Pelvic examination with the patient under anesthesia found swelling on the right vaginal wall measuring 7.0 cm × 6.0 cm × 6.0 cm.
Figure 1.
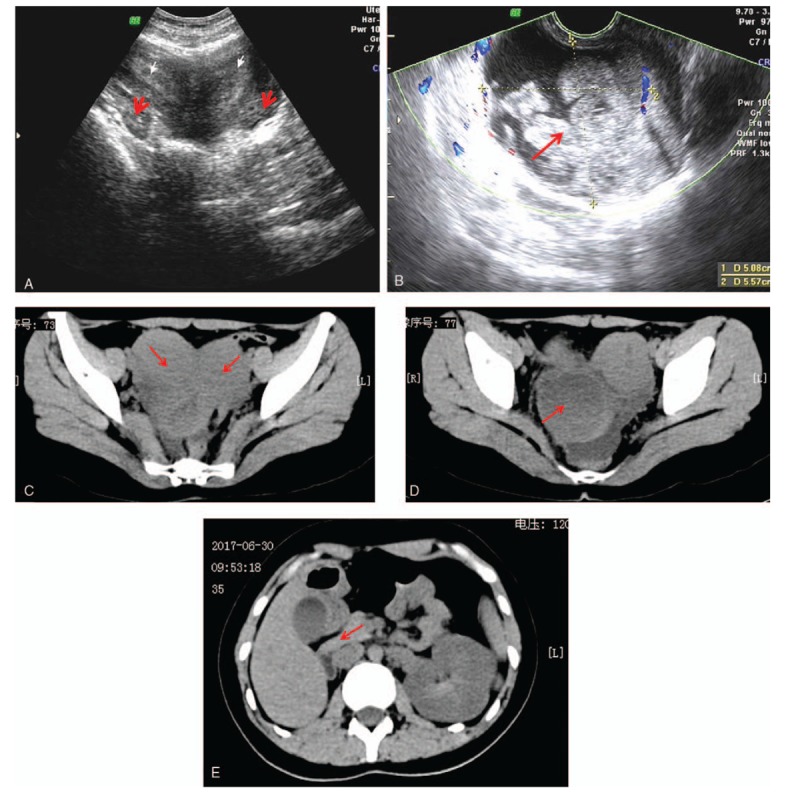
(A) Transabdominal US showing uterus didephys (white arrow) and normal adnexal region (red arrow). (B) Transvaginal US showing hematocolpos mixed echogenicity (red arrow). (C) CT finding of uterus didelphys (red arrow). (D) CT finding of hematocolpos (red arrow). (E) CT finding of the right kidney is absent (red arrow). CT = computed tomography, US = ultrasound.
A small amount of dark red blood was observed to leak out of a microperforation measuring 0.2 cm in diameter above the right vaginal wall and along the left cervix an annular cut was made to the oblique vaginal septum through a small hole, and the cutting range was 2.5 cm wide; thereafter, a large amount of decidual tissue and blood flowed out of the right hemivagina. The resection margin was lock-stitch sutured and extended up to the oblique septum to explore the small cervix. Under ultrasound guidance, the right uterine cavity showed a depth of 9 cm. At the same time, the left uterus was given a curettage, and the contents of the scraped uterus and the right uterine cavity effluent were sent for pathological examination. The pathological findings showed secretory failure in the endometrium (Fig. 2A), and the mesenchyme clearly had endometrial stroma (Fig. 2B) with no villus component. Therefore, it was assumed that the patient underwent a spontaneous abortion. No complications were found at 1 and 3 months after surgery. The patient was asymptomatic and having regular menses at the most recent follow-up.
Figure 2.
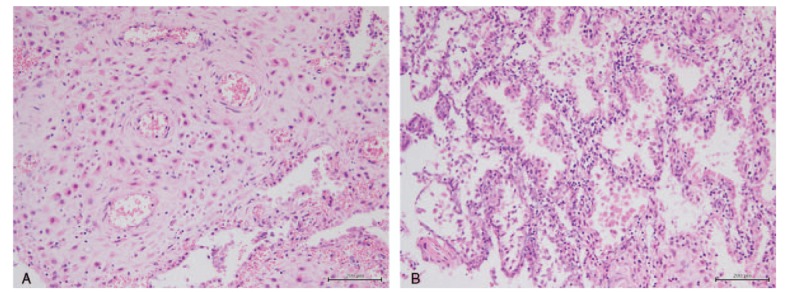
(A) The endometrium showing secretion failure. (B) The mesenchyme clearly showing endometrial stroma.
3. Discussion
HWWS is a rare congenital unparallel malformation of the genital tract first reported by Purslow in 1922. In 1971, the association of renal agenesis with ipsilateral blind hemivagina was reported as Herlyn–Werner syndrome. In 1976, Wunderlich described it as an association of right renal aplasia with a bicornuate uterus and simple vagina in the presence of an isolated hematocervix. Clinical presentation is usually with abdominal pain, dysmenorrhea, urinary retention, hematosalpinx, endometriosis, and rupture of a tubo-ovarian abscess.
The exact etiology and pathogenesis of HWWS is still unclear. It has been considered to represent the anomalous development of paramesonephric (Müllerian) and mesonephric (Wolffian) ducts. The mesonephric ducts, besides giving origin to the kidneys, are also inductor elements for adequate Müllerian duct fusion. Therefore, a developmental anomaly of the caudal portion of one of the mesonephric ducts may be the cause of unilateral renal agenesis associated with imperforate hemivagina.[4] On the side where the mesonephric duct is absent, the Müllerian duct is displaced laterally and cannot fuse with the contralateral duct, resulting in a didelphic uterus. The contralateral Müllerian duct gives rise to the vagina, whereas the displaced Müllerian duct that cannot come into contact with the urogenital sinus centrally forms a blind sac, leading to an imperforate or obstructed hemivagina. Renal agenesis is the most common associated nongenital anomaly and is always seen on the side with the obstructed hemivagina.
At present, the classification standards adopted by Rock and Jones in 1980 are widely used internationally, including complete locking and incomplete locking.[5] In 2018, Chinese gynecology and obstetrics specialists headed by Peking Union Medical College Hospital divided HWWS into 3 types.[6]
Type I, with blind hemivagina: in this classification, the hemivagina is completely obstructed; the uterus behind the septum is completely isolated from the contralateral uterus, and no communication is present between the duplicated uterus and vagina (Fig. 3A). Type II, partial reabsorption of the vaginal septum: a small communication exists between the 2 vaginas, which make the vaginal cavity behind the septum incompletely obstructed. The uterus behind the septum is completely isolated from the contralateral uterus. Menstrual blood can outflow through the small communication, but the drainage is impeded (Fig. 3B). Type III, with communicating uteri: in this classification, the hemivagina is completely obstructed, and a small communication exists between the duplicated cervices. Menstrual blood from the uterus behind the septum can outflow through the communication to the offside contralateral cervix. However, because the communication is small, the drainage is still impeded (Fig. 3C). The patient in our report showed uterus didelphys and a microperforation measuring 0.2 cm in diameter on the right obstructed hemivagina associated with right renal agenesis, thereby classified as Type II.
Figure 3.
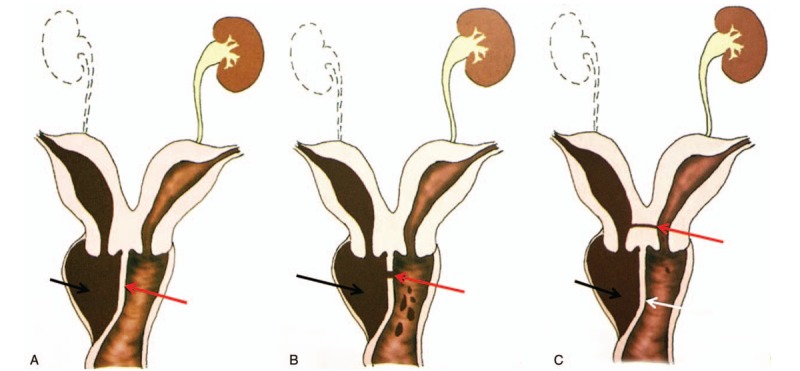
(A) Type 1, the vaginal cavity behind the septum (black arrow) and blind hemivagina (red arrow). (B) Type 2, the vaginal cavity behind the septum (black arrow) and perforating septa (red arrow). (C) Type 3, the vaginal cavity behind the septum (black arrow) with blind hemivagina (white arrow) and communicating uteri (red arrow). (Courtesy: Ref.[6]).
The clinical manifestation of HWWS is various, but characteristically presents with a pelvic mass after menarche, cyclic lower abdominal pain, intermenstrual bleeding, and foul mucopurulent discharge. The menstrual cycles of our patient were regular, but menstrual drainage was difficult and even retrograde owing to obstructed hemivagina, which could result in dysmenorrhea. The vagina is a rather distensible organ, allowing it to accommodate a large amount of blood. Part of the blood is absorbed between the periods and therefore patients with HWWS can go unrecognized from a few months to several years after the onset of menstruation. Long-term continual reverse menstrual flow may result in hematocolpos, hematometra, and hematosalpinx, leading to long-term complications such as pelvic adhesions, endometriosis, infertility, and increased risk of abortion.[4] Women with uterus didelphys have a high likelihood of becoming pregnant, with approximately 80% of patients being able to conceive, but with considerably high rates of premature delivery (22%) and abortion (74%).[7] Consistent with literature, our patient experienced a spontaneous abortion. Patients usually complain of acute abdominal disease, resulting in delayed diagnosis. A differential diagnosis from other pelvic disorders such as endometriosis, pelvic inflammatory disease, complicated ovarian cysts, and tubo-ovarian abscess.[8]
Ultrasound imaging—sometimes as transabdominal US and/or transvaginal US—is commonly employed as the initial imaging procedure to diagnose HWWS. US evaluates uterine morphology and detects the level of characteristic fluid contents in the proximal vagina and uterine cervices. US examination of our patient revealed uterus didelphys associated with complicated fluid echoes at the level of the proximal vagina or cervices. The US imaging features of the hemorrhage may vary from a pure cystic, mixed echogenicity, or even gas echoes, associated with infection. CT and MRI are both beneficial tools for diagnosing HWWS [9,10] In this case, abnormalities related to uterine malformations were confirmed by CT. This case is unique in that it presented and was diagnosed late with coexisting abortion. The probable reason for the delayed presentation was the partial resorption of blood between periods and distensibility of the vagina. However, over time, the generation of large amounts of blood and decidual tissue could not be absorbed as efficiently, resulting in hematocolpos.
Resection of as much of the obstructing vaginal septum as possible is the most effective treatment, which can rapidly relieve symptoms and prevent complications in a timely manner, leading to good prognosis. If the malformation and lesions are promptly corrected, the reproductive outcome is better and both uteri can sustain normal pregnancy and subsequent delivery; however, the oblique-septum contralateral uterine pregnancy is more common.[6] Although fertility is not impaired and the fetal survival rate is high, premature rupture of fetal membranes and delayed fetal development are still causes for concern.[11] Therefore, when unilateral renal agenesis and uterus didelphys coexist, the first thing to consider and rule out is the presence of a blind vagina.
Author contributions
Supervision: Lifeng Cui, Yan Wen.
Validation: Fengyan Gong.
Writing – original draft: Guifeng Jia.
Writing – review & editing: Wei Chai, Miao Cui.
Footnotes
Abbreviations: CT = computed tomography, HWWS = Herlyn–Werner–Wunderlich syndrome, MRI = magnetic resonance imaging, US = ultrasound.
Ethical approval: Ethical approval is not needed in our case report.
Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. Copy of the written consent is available for review by the editor of this journal.
The authors have no funding and no conflicts of interest to disclose.
References
- [1].Wang J, Zhu L, Lang J, et al. Clinical characteristics and treatment of Herlyn–Werner–Wunderlich syndrome. Arch Gynecol Obstet 2014;290:947–50. [DOI] [PubMed] [Google Scholar]
- [2].Zurawin RK, Dietrich JE, Heard MJ, et al. Didelphic uterus and obstructed hemivagina with renal agenesis: case report and review of the literature. J Pediatr Adolesc Gynecol 2004;17:137–41. [DOI] [PubMed] [Google Scholar]
- [3].Burgis J. Obstructive müllerian anomalies: case report, diagnosis, and management. Am J Obstet Gynecol 2001;185:338–44. [DOI] [PubMed] [Google Scholar]
- [4].Orazi C, Lucchetti MC, Schingo PMS, et al. Herlyn- Werner-Wunderlich syndrome: uterus didelphys, blind hemivagina and ipsilateral renal agenesis. Sonographic and MR findings in 11 cases. Pediatr Radiol 2007;37:657–65. [DOI] [PubMed] [Google Scholar]
- [5].Tzialidou-Palermo I, von Kaisenberg CS, Garcia-Rocha GJ, et al. Diagnostic challenges of hemihematocolpos and dysmenorrhea in adolescents: obstructed hemivagina, didelphys or bicornuate uterus and renal aplasia is a rare female genital malformation. Arch Gynecol Obstet 2012;286:785–91. [DOI] [PubMed] [Google Scholar]
- [6].Zhu L, Lang J, Song L, et al. Chinese expert consensus on the diagnosis and treatment of Herlyn–Werner–Wunderlich syndrome, Mayer–Rokitansky–Kuster–Hauser syndrome and vaginal atresia. Chin J Obstet Gynecol 2018;53:35–42. [DOI] [PubMed] [Google Scholar]
- [7].Piccinini PS, Doski J. Herlyn–Werner–Wunderlinch syndrome: a case report. Rev Bras Ginecol Obsetet 2015;37:192–6. [DOI] [PubMed] [Google Scholar]
- [8].Alpaslan Y, Aydin B, Mertihan K, et al. Herlyn–Werner–Wunderlich syndrome: merits of sonographic and magnetic resonance imaging for accurate diagnosis and patient management in 13 cases. J Pediatr Adolesc Gynecol 2015;28:47–52. [DOI] [PubMed] [Google Scholar]
- [9].Fields SI, Katz S, Beyth Y. Computed tomography of unilateral hematometrocolpos. J Comput Assist Tomogr 1988;12:530. [DOI] [PubMed] [Google Scholar]
- [10].Marten K, Vosshenrich R, Funke M, et al. MRI in the evaluation of mullerian duct anomalies. Clin Imaging 2003;27:346. [DOI] [PubMed] [Google Scholar]
- [11].Cozzolino M, Corioni S, Magro Malosso ER, et al. Two successful pregnancies in Herlyn–Werner–Wunderlich syndrome. Obstet Case Rep 2014;91:48–58. [DOI] [PubMed] [Google Scholar]


