Abstract
Background:
Endoscopic placement of multiple plastic stents (MPS) has been the first-line treatment for benign biliary stricture (BBS). Covered self-expanding metal stents (cSEMS) have been used in treatment of BBS; however, the efficacy has not been verified. Therefore, we conducted this meta-analysis according to PRISMA guidelines.
Methods:
PubMed, Embase, and the Cochrane Library were electronically and manually searched for studies published between January 1, 1990 and April 12, 2017. Of 153 studies screened, 90 were excluded because of duplications. After scanning the title or abstract, only 24 studies were eligible for review and 6 were finally included. The investigators selected publications according to inclusion and exclusion criteria, processed the data, and assessed the quality of the selected studies. The primary endpoint outcome was stricture resolution, and the secondary endpoint outcomes included stricture recurrence rate, the number of endoscopic retrograde cholangiopancreatography (ERCP) sessions, and stent migration.
Results:
A total of 6 randomized controlled trials with 330 participants were included in the current meta-analysis. There was no significant difference in stricture resolution between the cSEMS and MPS groups (odds ratio [OR] = 1.05, 95% confidence interval [CI] = 0.53–2.07, I2 = 29%, P = .23, Z = 0.13, P = .90). Similarly, the stricture recurrence rates (OR = 1.39, 95% CI = 0.69–2.81, I2 = 38%, P = .17, Z = 0.91, P = .36) were comparable between cSEMS and MPS groups. Stent migration rates (OR = 1.71, 95% CI = 0.84–3.50, I2 = 4%, P = .241, Z = 1.47, P = .14) were similar between cSEMS and MPS groups. There were fewer ERCP sessions in the cSEMS group than in the MPS group.
Conclusions:
This meta-analysis showed that cSEMS were comparable to MPS in achieving resolution of BBSs with fewer ERCP procedures.
Keywords: benign biliary strictures, covered self-expanding metal stents, endoscopic treatment, multiple plastic stents
1. Introduction
Benign biliary stricture (BBS) is rare and most cases are caused by iatrogenic biliary injury, mainly after open or laparoscopic cholecystectomy, with reported occurrence in 0.1% to 0.5% of open procedures and 0.25% to 1.0% of laparoscopic surgeries.[1,2] The second most common cause is fibrosis at the site of surgical anastomosis after liver transplantation. Other conditions that can lead to benign bile duct obstruction include chronic pancreatitis, sclerosing cholangitis, cholelithiasis, sphincterotomy, and infection of the biliary tract.[3] The clinical symptoms present as obstructive jaundice, chronic cholestasis, and cholangitis, as well as secondary biliary cirrhosis.[4]
Endoscopic treatment rather than percutaneous transhepatic biliary drainage or surgery is considered first-line treatment for BBS. Use of multiple plastic stents (MPS) has been recommended by the European Society of Gastrointestinal Endoscopy for BBS, and uncovered self-expandable metallic stents are not recommended because of removal problems caused by embedding.[3,5] Hence, covered self-expanding metallic stents (cSEMS) are an intriguing option for treatment of BBS due to their removability.
Because they are usually fibrotic and associated with a dilated bile duct, most benign strictures cannot be fully dilated during initial endoscopic retrograde cholangiopancreatography (ERCP). An average of 3 to 4 ERCP procedures are required to dilate, deploy stents, up-size, and ultimately remove all stents once the stricture has resolved. Placement of 10-mm single cSEMS results in radial dilation of a stricture equivalent to that of six or seven 10-Fr plastic stents.[6–9] Some studies have reported that the use of cSEMS could achieve comparable effects with fewer ERCP procedures.[10–12] However, because of small sample sizes, the results were not convincing. Thus, we conducted this meta-analysis to compare the effect of cSEMS with MPS on BBS resolution.
2. Methods
2.1. Search strategy
We searched for relevant articles published between January 1, 1990 and April 12, 2017. Computerized searches in the PubMed, Embase, and Cochrane library electronic databases were performed by using the terms “benign biliary stricture” or “bile duct stenosis” or “biliary anastomotic strictures” and “plastic stent” and “metal stent” or “metallic stent.” Relevant reviews and meta-analyses focusing on BBS treatment were manually examined to identify additional eligible studies.
2.2. Inclusion criteria
Studies meeting the following criteria were included: the enrolled patients had BBS, and strictures resulting from malignant disease were excluded; the study design was a prospective randomized controlled trial (RCT); the study compared the treatment efficacy of plastic stents and cSEMS for BBS, and studies using uncovered SEMS were excluded; and the study should clearly report primary endpoint outcomes, as defined herein.
2.3. Endpoint outcomes defined
The primary endpoint outcome was stricture resolution, and the secondary endpoint outcomes included stricture recurrence, number of ERCP sessions, stent migration, and complications, such as pancreatitis, cholangitis, perforation, hemorrhage, pain, infection, and stent occlusion.
2.4. Data extraction and quality assessment of included studies
Two authors (XZ and XW) independently extracted and recorded data from the studies. The data included the publication year, study period, etiology of stricture, stent design, follow-up time, number of ERCP sessions, success rate, and recurrence rate. Disagreements would be settled through discussion. The risk of bias for RCTs was assessed using the Jadad score.[13]
2.5. Ethics approval
As all analyses were based on previously published studies, no ethics approval or patient consent was required.
2.6. Statistical analysis
Statistical analyses were performed using Stata 14.0 software. For the analysis of stricture resolution rate, stricture recurrence rate, and stent migration rate, pooled odds ratios (ORs) with 95% confidence intervals (CIs) were used (OR > 1 favored the MPS group and OR < 1 favored the cSEMS group). Heterogeneity across studies was evaluated using the I2 statistic, an I2 > 50% was regarded as indicating significant heterogeneity and a random-effects model was used; otherwise, a fixed-effects model was used. Potential publication bias was assessed using Egger linear regression test. A P value < .05 indicated statistical significance.
3. Results
3.1. Characteristic of studies included
Based on the inclusion and exclusion criteria, 6 RCTs with 330 patients were included in the present meta-analysis (Fig. 1).[10–12,14–16] The characteristics of included studies are shown in Table 1. Cochrane bias risk assessment was performed, and the results are shown in Table 2.
Figure 1.
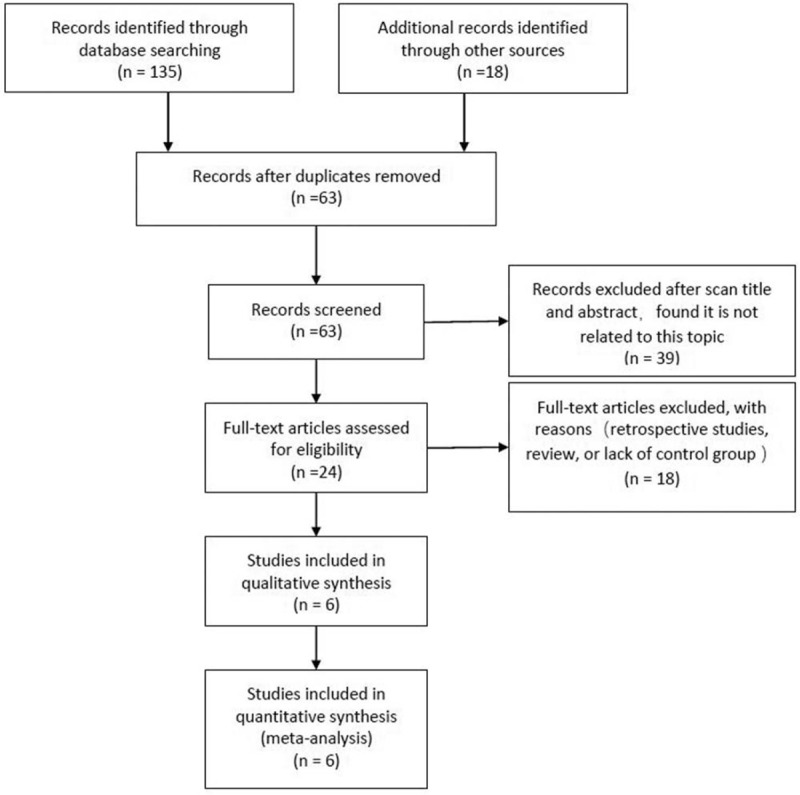
Search process for trials included in this meta-analysis.
Table 1.
The characteristics of studies included.
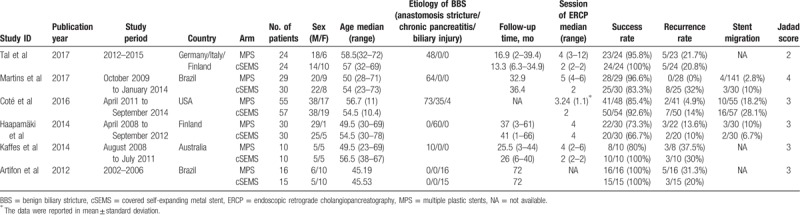
Table 2.
The risk of bias for the studies included.
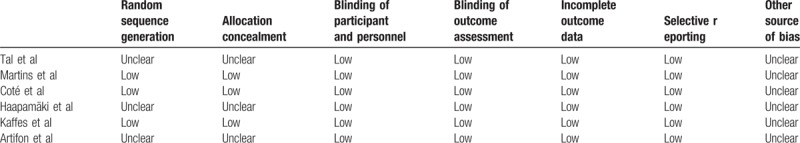
3.2. Stricture resolution
All 6 RCTs reported stricture resolution. As shown in Fig. 2, the stricture resolution rate in the cSEMS and MPS groups was comparable (OR = 1.05, 95% CI = 0.53–2.07, I2 = 29%, P = .23, Z = 0.13, P = .90).
Figure 2.
Meta-analysis of data on stricture resolution in patients with BBS following either cSEMS or MPS treatment. BBS = benign biliary stricture, cSEMS = covered self-expanding metal stent, MPS = multiple plastic stents.
Egger test showed no indication of publication bias (2-sided P = .887) in stricture resolution rates (Fig. 3).
Figure 3.
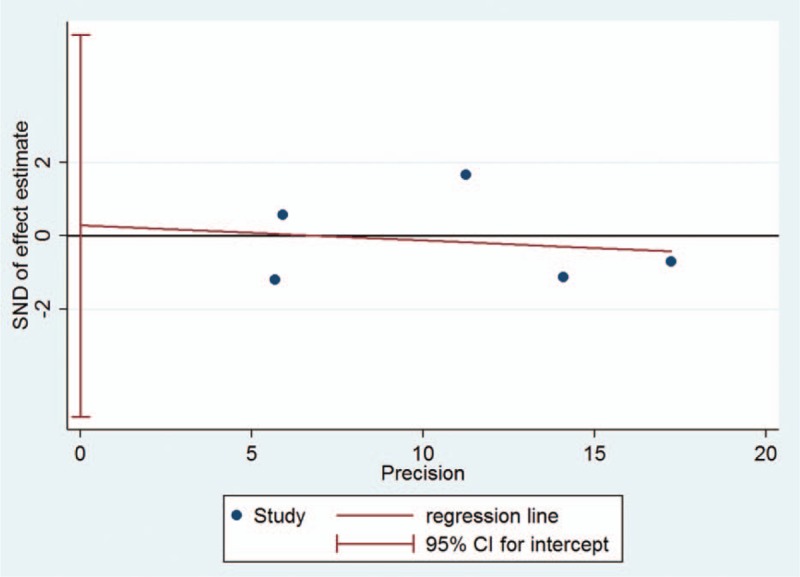
Egger test of publication bias for stricture resolution rates.
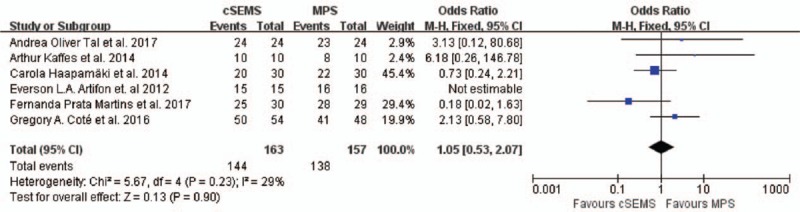
3.3. Recurrence rate
All 6 RCTs reported stricture recurrence. The recurrence rate was similar in cSEMS and MPS groups (OR = 1.39, 95% CI = 0.69–2.81, I2 = 38%, P = .17, Z = 0.91, P = .36) (Fig. 4).
Figure 4.
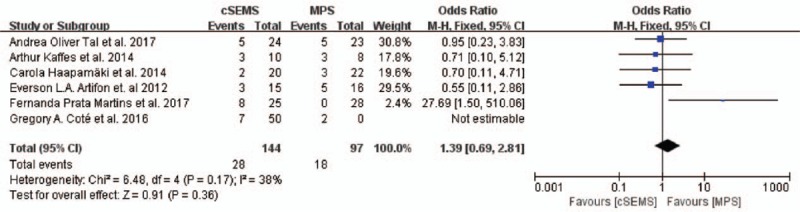
Meta-analysis of data on stricture recurrence rates in patients with BBS following either cSEMS or MPS treatment. BBS = benign biliary stricture, cSEMS = covered self-expanding metal stent, MPS = multiple plastic stents.
3.4. ERCP session
As shown in Table 1, there were significantly fewer ERCP sessions in the cSEMS group than in the MPS group. In a study by Martins et al, patients receiving MPS treatment underwent an average of 5 (4–6) ERCP procedures, whereas the cSEMS group underwent an average of 2 sessions until anastomotic biliary stricture resolution (P < .001). Similarly, in a study by Tal et al, the MPS group underwent an average of 4 (3–12) ERCP sessions, while the cSEMS group underwent an average of 2 (P < .001). In a study by Coté et al, fewer ERCP sessions were required to achieve resolution in the cSEMS (2.14) versus MPS group (3.24; mean difference, 1.10; 95% CI = 0.74–1.46; P < .001). A study by Kaffes et al showed similar results (MPS vs cSEMS, 4 [2–6] vs 2 [2–2], P = .001). Thus, the use of cSEMS can decrease the number of ERCP procedures.
3.5. Stent migration
Three studies reported the complication of stent migration. Migration was more common in the cSEMS group than in the MPS group. (OR = 1.71, 95% CI = 0.84–3.50, I2 = 4%, P = .241, Z = 1.47, P = .14) (Fig. 5).
Figure 5.
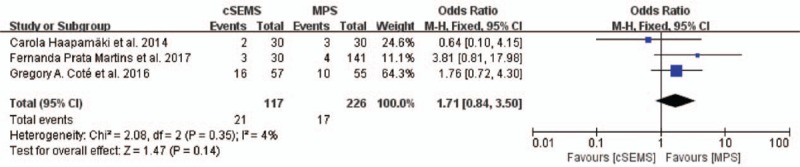
Meta-analysis of data on stent migration in patients with BBS following either cSEMS or MPS treatment. BBS = benign biliary stricture, cSEMS = covered self-expanding metal stent, MPS = multiple plastic stents.
4. Discussion
Numerous studies have evaluated cSEMS as salvage and first-line treatment for BBS. It has been reported that cSEMS were comparable to MPS when used for initial treatment, but achieved resolution with significantly fewer ERCP procedures.[10–12,17] This meta-analysis further confirms the treatment benefit of cSEMS for BBS.
Stricture recurrence after endoscopic treatment occurs in about 10% to 30% of cases.[18–21] However, it has been unclear as to which type of stent could decrease the recurrence rate. This meta-analysis showed that the recurrence rate was similar between cSEMS and MPS groups.
Stent migration remains an important limitation of currently available cSEMS.[22,23] However, this study found that the stent migration rate was similar in cSEMS and MPS groups. This is most likely attributable to the improvement of cSEMS with antimigration features. There remains a need to develop novel, expandable stents that can be used in smaller-diameter ducts, without the need for routine follow-up ERCP for retrieval. Similarly, stent migration is also an issue with MPS, because of the sphincterotomy procedure used to facilitate side-by-side stent placement.
Because of lacking of RCTs, the previous meta-analysis was focusing on 1 method (MPS alone or cSEMS alone) in the management of BBS,[24,25] leading to less convincible result. In this meta-analysis, the including studies was all RCTs, resulting in the result more credible.
This meta-analysis had some limitations. First, few RCTs focused on the treatment of BBS using either cSEMS or MPS, limiting the robustness of the meta-analysis. Second, as the etiology of BBS was mixed, subgroup analysis was difficult. Third, the pooled results for stent migration were less valid because of high heterogeneity.
cSEMS were comparable to MPS in achieving stricture resolution in patients with BBS, using fewer ERCP procedures. Further randomized studies are required to improve the treatment of BBS.
Author contributions
Conceptualization: Xinjing Zhang, Jiahong Dong.
Data curation: Xuedong Wang.
Formal analysis: Xinjing Zhang.
Funding acquisition: Jiahong Dong.
Investigation: Xinjing Zhang.
Methodology: Xinjing Zhang.
Software: Xinjing Zhang, Xuedong Wang, Rui Tang.
Supervision: Jiahong Dong.
Validation: Liang Wang.
Writing – original draft: Xinjing Zhang, Rui Tang.
Writing – review & editing: Jiahong Dong.
Footnotes
Abbreviations: BBS = benign biliary stricture, CI = confidence interval, cSEMS = covered self-expanding metal stent, ERCP = endoscopic retrograde cholangiopancreatography, MPS = multiple plastic stents, OR = odds ratio, RCT = randomized controlled trial.
This study was supported by the Beijing Municipal Administration of Hospital Clinical medicine Development of special funding support (code: ZYLX201712).
The authors have no conflicts of interest to disclose.
References
- [1].Tocchi A, Mazzoni G, Liotta G, et al. Management of benign biliary strictures: biliary enteric anastomosis vs endoscopic stenting. Arch Surg 2000;135:153–7. [DOI] [PubMed] [Google Scholar]
- [2].Laasch HU, Martin DF. Management of benign biliary strictures. Cardiovasc Intervent Radiol 2002;25:457–66. [DOI] [PubMed] [Google Scholar]
- [3].van Boeckel PG, Vleggaar FP, Siersema PD. Plastic or metal stents for benign extrahepatic biliary strictures: a systematic review. BMC Gastroenterol 2009;9:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Warshaw AL, Schapiro RH, Ferrucci JT, Jr, et al. Persistent obstructive jaundice, cholangitis, and biliary cirrhosis due to common bile duct stenosis in chronic pancreatitis. Gastroenterology 1976;70:562–7. [PubMed] [Google Scholar]
- [5].Siriwardana HP, Siriwardena AK. Systematic appraisal of the role of metallic endobiliary stents in the treatment of benign bile duct stricture. Ann Surg 2005;242:10–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Judah JR, Draganov PV. Endoscopic therapy of benign biliary strictures. World J Gastroenterol 2007;13:3531–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kahaleh M, Behm B, Clarke BW, et al. Temporary placement of covered self-expandable metal stents in benign biliary strictures: a new paradigm? (With video). Gastrointest Endosc 2008;67:446–54. [DOI] [PubMed] [Google Scholar]
- [8].Behm B, Brock A, Clarke BW, et al. Partially covered self-expandable metallic stents for benign biliary strictures due to chronic pancreatitis. Endoscopy 2009;41:547–51. [DOI] [PubMed] [Google Scholar]
- [9].Irani S, Baron TH, Akbar A, et al. Endoscopic treatment of benign biliary strictures using covered self-expandable metal stents (CSEMS). Dig Dis Sci 2014;59:152–60. [DOI] [PubMed] [Google Scholar]
- [10].Cote GA, Slivka A, Tarnasky P, et al. Effect of covered metallic stents compared with plastic stents on benign biliary stricture resolution: a randomized clinical trial. JAMA 2016;315:1250–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Tal AO, Finkelmeier F, Filmann N, et al. Multiple plastic stents versus covered metal stent for treatment of anastomotic biliary strictures after liver transplantation: a prospective, randomized, multicenter trial. Gastrointest Endosc 2017;86:1038–45. [DOI] [PubMed] [Google Scholar]
- [12].Kaffes A, Griffin S, Vaughan R, et al. A randomized trial of a fully covered self-expandable metallic stent versus plastic stents in anastomotic biliary strictures after liver transplantation. Therap Adv Gastroenterol 2014;7:64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].McCormick F, Cvetanovich GL, Kim JM, et al. An assessment of the quality of rotator cuff randomized controlled trials: utilizing the Jadad score and CONSORT criteria. J Shoulder Elbow Surg 2013;22:1180–5. [DOI] [PubMed] [Google Scholar]
- [14].Haapamaki C, Kylanpaa L, Udd M, et al. Randomized multicenter study of multiple plastic stents vs. covered self-expandable metallic stent in the treatment of biliary stricture in chronic pancreatitis. Endoscopy 2015;47:605–10. [DOI] [PubMed] [Google Scholar]
- [15].Martins FP, De Paulo GA, Contini MLC, et al. Metal versus plastic stents for anastomotic biliary strictures after liver transplantation: a randomized controlled trial. Gastrointest Endosc 2018;87:131.e1–3. [DOI] [PubMed] [Google Scholar]
- [16].Artifon EL, Coelho F, Frazao M, et al. A prospective randomized study comparing partially covered metal stent versus plastic multistent in the endoscopic management of patients with postoperative benign bile duct strictures: a follow-up above 5 years. Rev Gastroenterol Peru 2012;32:26–31. [PubMed] [Google Scholar]
- [17].Saxena P, Diehl DL, Kumbhari V, et al. A US multicenter study of safety and efficacy of fully covered self-expandable metallic stents in benign extrahepatic biliary strictures. Dig Dis Sci 2015;60:3442–8. [DOI] [PubMed] [Google Scholar]
- [18].Deviere J, Nageshwar Reddy D, Puspok A, et al. Successful management of benign biliary strictures with fully covered self-expanding metal stents. Gastroenterology 2014;147:385–95. [DOI] [PubMed] [Google Scholar]
- [19].Costamagna G, Boskoski I. Current treatment of benign biliary strictures. Ann Gastroenterol 2013;26:37–40. [PMC free article] [PubMed] [Google Scholar]
- [20].Parlak E, Disibeyaz S, Odemis B, et al. Endoscopic treatment of patients with bile duct stricture after cholecystectomy: factors predicting recurrence in the long term. Dig Dis Sci 2015;60:1778–86. [DOI] [PubMed] [Google Scholar]
- [21].de Reuver PR, Rauws EA, Vermeulen M, et al. Endoscopic treatment of post-surgical bile duct injuries: long term outcome and predictors of success. Gut 2007;56:1599–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Walter D, Laleman W, Jansen JM, et al. A fully covered self-expandable metal stent with antimigration features for benign biliary strictures: a prospective, multicenter cohort study. Gastrointest Endosc 2015;81:1197–203. [DOI] [PubMed] [Google Scholar]
- [23].Tarantino I, Mangiavillano B, Di Mitri R, et al. Fully covered self-expandable metallic stents in benign biliary strictures: a multicenter study on efficacy and safety. Endoscopy 2012;44:923–7. [DOI] [PubMed] [Google Scholar]
- [24].Siiki A, Helminen M, Sand J, et al. Covered self-expanding metal stents may be preferable to plastic stents in the treatment of chronic pancreatitis-related biliary strictures: a systematic review comparing 2 methods of stent therapy in benign biliary strictures. J Clin Gastroenterol 2014;48:635–43. [DOI] [PubMed] [Google Scholar]
- [25].Huszar O, Kokas B, Matrai P, et al. Meta-analysis of the long term success rate of different interventions in benign biliary strictures. PLoS ONE 2017;12:e0169618. [DOI] [PMC free article] [PubMed] [Google Scholar]


