Supplemental Digital Content is available in the text
Keywords: pediatric, quality of life, voice, voice handicap index
Abstract
The aim of this study was to investigate differences and correlations between the pediatric Voice Handicap Index (pVHI) and the pediatric Voice-Related Quality-of-life (pVRQOL) questionnaires in children with and without voice disorders. This was a cross-sectional study.
A total of 418 parents with children aged 2 to 14 years participated in this study from May 2016 to July 2017. This included 221 parents of children with voice disorders (dysphonic group) and 197 parents of children without voice disorders (control group). The scores for the pVHI and the pVRQOL were compared, and correlation analysis was performed.
Compared with the control group, the dysphonic group had a significantly higher total score and subscale scores for the pVHI (P < .001), and significantly lower pVRQOL scores (P < .001). The pVHI showed greater differences in subscale scores among the three dysphonic subgroups than the pVRQOL. The Spearman correlation coefficient between the pVHI and pVRQOL was –0.844 (P < .001). The total scores for the pVHI and pVRQOL also correlated significantly for each diagnostic category (P < .001).
Voice-related quality of life was poorer in children with voice disorders than in those without voice disorders. The pVHI and pVRQOL scores were moderately- to strongly correlated. These may be useful tools for assessing the voice-related quality of life in children. The pVHI may provide more useful details about the effects of different types of voice disorders on the voice-related quality of life than the pVRQOL.
1. Introduction
Voice is a vital communication tool for conveying personal thoughts and ideas, and for expressing the individual's identity. There is a strong demand for vocal use but insufficient knowledge about vocal hygiene. The prevalence of voice disorders is 6.2% in adults,[1] and is as high as 54.6% in professional vocal users.[2] Voice disorders are common in children, with prevalence of 6% to 24%.[3,4] The quantification of voice quality and vocal function is difficult. Previous studies have focused on objective assessments, including physical examination, acoustic analysis, laryngoscopy, and measures of aerodynamics.[5] These assessment procedures may be difficult for children, who may have poorer compliance following instructions.
In recent years, the effects of voice disorders on voice-related quality of life have attracted attention.[6–8] The pediatric Voice Handicap Index (pVHI)[9] and the pediatric Voice-Related Quality of Life (pVRQOL)[10] questionnaires are used widely for assessing the voice-related quality of life in children. These pediatric voice-related quality of life questionnaires were modified from the adult versions.[11]
The pVHI is a questionnaire with 23 items, which are divided into 3 subscales: functional, physical, and emotional. Each item is scored from 0 to 4, and a higher score reflects a poorer voice-related quality of life (Appendix A). The pVRQOL comprises 10 items, and is divided into 2 subscales: the social-emotional and physical-functioning. Each item is scored from 0 to 5. The raw scores for the total score and subscale scores are transformed to a scale of 0 to 100, with a lower score reflecting the more severe impairment of voice-related quality of life (Appendix B). As younger children may have difficulties comprehending and answering the questions, the questionaires were designed to be completed by parents.
Recently, the pVHI and pVRQOL have been translated into Chinese and validated.[12,13] Previous studies have confirmed that VHI scores strongly correlated with VRQOL scores in adults.[5] However, to date, no studies have compared the results obtained for the pVHI and the pVRQOL or have analyzed the relationship between these questionnaires in the pediatric dysphonic population. Therefore, the purposes of this study were to compare voice-related quality of life assessed by the pVHI and pVRQOL between children with and without voice disorders, and among children with different types of voice disorders. A further purpose was to analyze the relationships between the pVHI and pVRQOL scores.
2. Methods and Subjects
This was a cross-sectional study. Ethical approval was obtained from the institutional review board of Sichuan University (approval number: 201789). The data were collected at the Department of Otolaryngology, Head & Neck Surgery in the West China Hospital, Sichuan University, and in the Women's & Children's Central Hospital, Chengdu, China, from May 2016 to July 2017.
A total of 418 parents with children aged between 2 and 14 years participated in this study. Among these parents, 221 were parents of children with voice disorders (dysphonic group) and 197 were parents of children without voice disorders (control group). The dysphonic children were diagnosed by videostroboscopic examination (Pentax, LH-150PC, Japan). The children in the control group had no history of voice disorders, or any voice complaints in the present or past. The parents were asked to complete the pVHI and pVRQOL questionnaires by themselves. A consent form was signed by each parent participant before data collection.
3. Statistics
All data were analyzed using IBM SPSS Statistics (version 22.0; IBM Corp., Armonk, NY). The analyses were described as follows:
-
1.
Mean and standard deviation were generated for continuous variables, including age, total scores, and subscale scores. Frequencies were calculated for categorical variables, including sex and vocal abuse habits.
-
2.
The total score and subscale scores were compared between the dysphonic group and control group using the nonparametric Mann–Whitney U test. The total score and subscales scores were compared between 3 subgroups within the dysphonic group and the control group using the Kruskal-Wallis test. Post hoc analysis was conducted using the least significance difference test.
-
3.
Correlations between the scores for the 2 questionnaires were calculated using Spearman rank analysis. For all test, P < .05 was considered to be significant.
4. Results
4.1. Demographic characteristics and diagnosis of voice disorders
All participants completed 2 questionnaires within 10 minutes.
In the dysphonic group, 221 parents of a child with voice disorders completed the questionnaires. The mean age of children was 5.31 years. There were 148 boys and 73 girls (boy: girl = 2.03: 1) in this group. The types of voice disorders included vocal fold nodules (n = 165, 74.7%), chronic laryngitis (n = 43, 19.5%), and vocal fold polyps (n = 13, 5.9%). In the control group, 197 parents with a child with normal vocal health completed the questionnaires. The mean age of children was 4.97 years. There were 107 boys and 90 girls (boy: girl = 1.19: 1) in this group. There were significantly more boys than girls in the dysphonic group (P < .05). However, age did not differ significantly between the 2 groups (P = .15).
4.2. Vocal abuse habits
The frequency of vocal abuse habits was significantly higher in the dysphonic group than the control group (P < .05) (Fig. 1). In the dysphonic group, the highest frequency of vocal abuse habit was shouting loudly (n = 198), followed by speaking for a long time (n = 171), then crying loudly (n = 113), laughing loudly (n = 105), and speaking fast (n = 72). In this group, significantly more girls than boys reported the “crying loudly” vocal abuse habit (67 vs. 46, P = .013), but there were no significant differences for other vocal abuse habits (P > .05).
Figure 1.
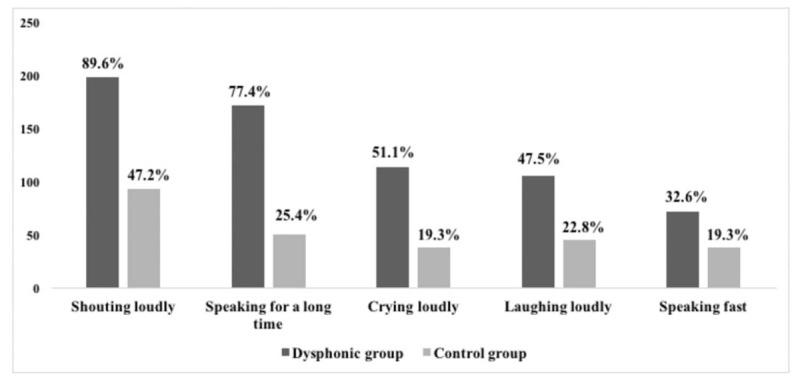
Comparison of vocal abuse habits between the dysphonic group and control group.
4.3. Comparisons of the total score and subscale scores in the pVHI and the pVRQOL between the dysphonic and control groups
As expected, the total pVHI score (26.63 ± 14.69 vs. 5.05 ± 5.98, P < .001) and the subscale scores of the pVHI were significantly higher in the dysphonic group than in the control group. The total score (79.12 ± 16.41 vs. 96.99 ± 7.07, P < .001) and the subscales scores of the pVRQOL were significantly lower in the dysphonic group than in the control group (P < .001). In the pVHI of the dysphonic group, the highest subscale score was the physical domain, and the lowest subscale score was the emotional domain. In the pVRQOL of the dysphonic group, the score for the physical functioning domain was lower than for the social-emotional domain. All subscale scores in the pVHI and pVRQOL differed significantly between the three dysphonic patient subgroups and the control group (P < .001). The vocal fold nodules and vocal fold polyps groups had higher scores in the pVHI and lower scores in the pVRQOL when compared with the chronic laryngitis (Table 1).
Table 1.
Demographic characteristics in the dysphonic group and the control group.

For the pVHI, post hoc analysis revealed that the control group had significantly lower physical subscale scores than the three dysphonic subgroups (P < .001). Among the 3 dysphonic subgroups, the vocal fold nodules group had significantly higher subscales (physical, functional, and emotional) scores than the chronic laryngitis group (P < .001). The vocal fold nodules group had significantly higher functional (P = .026) and emotional (P = .038) subscale scores than the vocal fold polyps group. The pVHI physical domain score did not differ significantly between the vocal fold nodules group and the other 2 groups (P = .067 for comparison with the vocal fold polyps group and P = .168 for the comparison with the chronic laryngitis group). The vocal fold polyps and chronic laryngitis groups did not differ significantly on the scores in the functional domain (P = .959) and emotional domain (P = .780) (Fig. 2 A–C).
Figure 2.
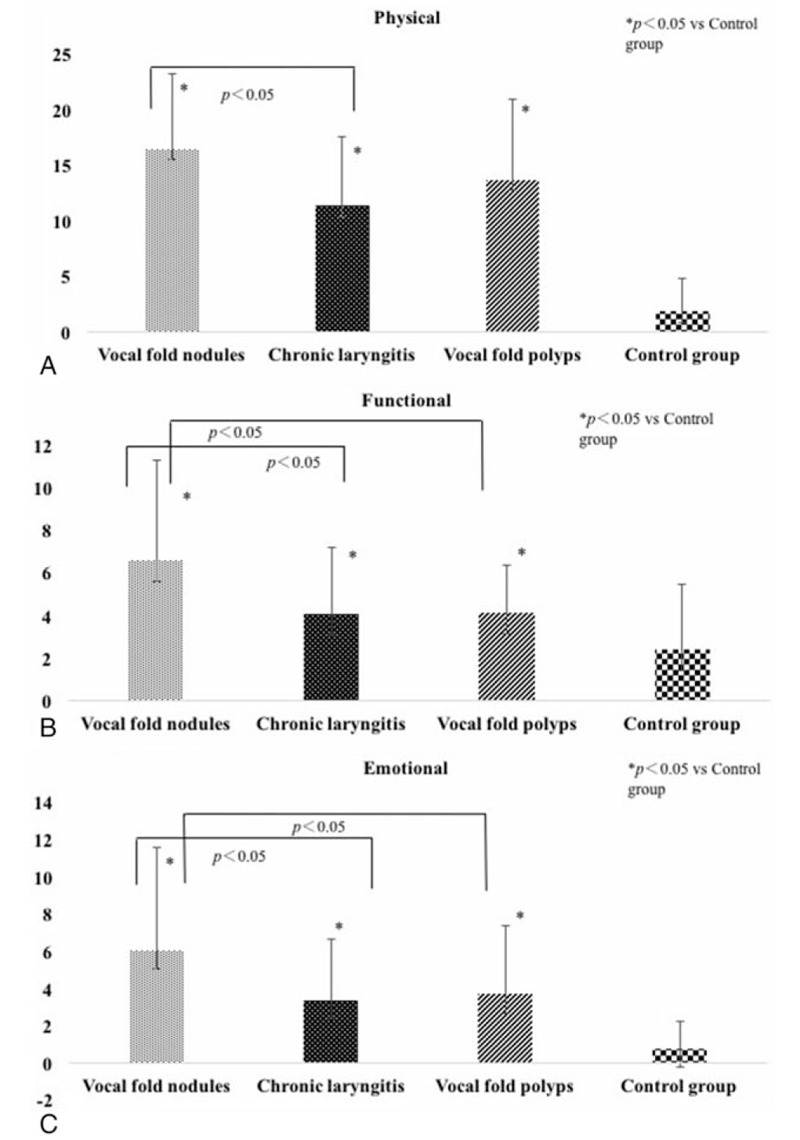
Comparisons of the subscale scores in the pVHI between the 3 subgroups in the dysphonic group and control group. (A) Differences in the pVHI physical domain between the 3 subgroups in the dysphonic group and control group; (B) Differences in the pVHI functional domain between the 3 subgroups in the dysphonic group and control group; (C) Differences in the pVHI emotional domain between the 3 subgroups in the dysphonic group and control group. pVHI = pediatric Voice Handicap Index.
For the pVRQOL, post hoc analysis revealed that the vocal fold nodules group had significantly lower social-emotional scores than the chronic laryngitis group (P < .001) and the control group (P < .001). No other significant differences were found between subgroups for the social-emotional domain (Fig. 3A). Post hoc analysis also showed that the 3 dysphonic subgroups had significantly lower physical-functional subscale scores than the control group (P < .001). The vocal fold nodules group had a significantly lower physical-functional subscale score than the chronic laryngitis group (P < .001) and the vocal fold polyps group (P = .041). There were no significant differences between the chronic laryngitis group and the vocal fold polyps group in two subscales (P = .682) (Fig. 3B).
Figure 3.
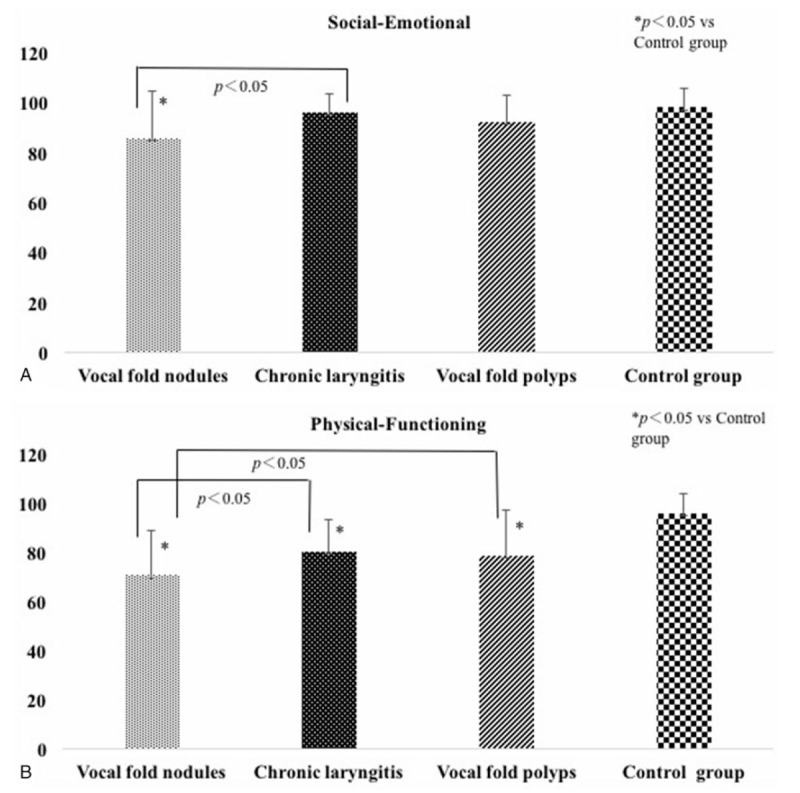
Comparisons of the subscale scores in the pVRQOL between the 3 subgroups in the dysphonic group and control group. (A) Differences in the pVRQOL social-emotional domain between the 3 subgroups in the dysphonic group and control group; (B) Differences in the pVRQOL physical-functional domain between the 3 subgroups in the dysphonic group and control group. pVRQOL = pediatric Voice-Related Quality-of-Life.
4.4. Correlation between the pVHI and pVRQOL in the dysphonic group
The Spearman correlation coefficient between the total score of the pVHI and the pVRQOL was −0.844 in the dysphonic group (P < .001). As shown in Table 2, moderate to strong correlations were found between the total score and the subscale scores of the pVHI (r = 0.603–0.898, P < .001), as well as between the total score and the subscale scores on the pVRQOL (r = 0.605–0.965, P < .001).
Table 2.
Comparisons of the total score and the subscales scores in the pVHI and the pVRQOL between the dysphonic and control groups.

The strongest correlation was found between the physical-functional subscale score and the total score on the pVRQOL (r = 0.965, p < .001), followed by between the physical subscale and the total score on the pVHI (r = 0.898, P < .001). In addition, there were moderate to strong negative correlations between the total scores on the pVHI and the pVRQOL for the 3 dysphonic subgroups: r = −0.735 in the chronic laryngitis subgroup, r = −0.852 in the vocal fold nodules subgroup, and r = −0.920 in the vocal fold polyps subgroup (P < .001).
5. Discussion
Voice disorders are common both in adults and children. Previous studies have confirmed that voice disorders are associated with vocal abuse and vocal misuse in adults and children.[14,15] This applies particularly to boys, who are generally more impulsive and vocally active, and prefer to attend outdoors activities with a great vocal burden enhance the vocal burden than girls.[16–19] In our study, children with voice disorders displayed more vocal abuse habits than did those without voice disorders. Among these vocal abuse habits, shouting loudly was the most common habit in the dysphonic group.
Many objective and subjective methods are used to identify and assess voice disorders, including videostroboscopic examination, aerodynamics, and questionnaires to assess the voice-related quality of life. These are usually combined to evaluate voice quality and voice-related quality of life together. In the present study, we used videostroboscopic examination to diagnose voice disorders, and the pVHI and the pVRQOL questionnaires to assess voice-related quality of life. The scores from both the pVHI and pVRQOL indicated that the children with voice disorders had worse voice-related quality of life than did those without voice disorders (Table 3).
Table 3.
Correlation coefficients between the subscales scores and total score of the pVHI and the pVRQOL in the dysphonic group.

The pVHI physical subscale and the pVRQOL physical-functioning subscale were the most significantly impaired subscales in the dysphonic group. These findings were in agreement with those of other studies.[9,12,13,20–22] The strongest correlation was found between the pVRQOL physical-functioning subscale and the pVRQOL total score, and between the pVHI physical subscale and the pVHI total score. These results suggested that, among all aspects of voice-related quality of life, voice disorders affect the physical aspects the most. It is possible that the symptoms related to physical function, such as hoarseness and a harsh or unstable voice, are more easily observed by parents. In clinical practice, parents may complain that their older children's self-confidence or mood was affected by voice disorders. In this study, the mean age of the children was just about 5 years. At this young age, they may not be able to accurately and verbally express their emotions, such as frustration or irritation. Moreover, they may have limited social activities. Therefore, these negative effects of functional and emotional aspects could be easily ignored by their parents. These results suggested that in addition to treatment by clinicians of the physical symptoms in children with voice disorders, parents and clinicians should also consider the emotional and functional aspects and design a holistic treatment approach.
Our results suggested that different voice disorders have different effects on voice-related quality of life, as identified in both the pVHI and the pVRQOL, and in the 3 dysphonic subgroups. The vocal fold nodules and vocal fold polyps groups had worse voice-related quality of life than the chronic laryngitis subgroup. The voice-related quality of life in vocal fold nodule groups was more severe than that of vocal fold polyps groups. In fact, the vocal fold nodules and polyps were benign lesions caused by vocal abuse and misuse. The difference may be related with the different duration of the symptoms, level of parents’ anxiety, the lack of vocal hygiene knowledge of the parents, and the sample size between vocal fold polyps and vocal nodules groups. It is notable that the pVHI, which was similar to the adult version of the VHI 21, showed more differences in subscale scores between the three dysphonic subgroups than the pVRQOL. This might be related to the greater number of items in the pVHI than the pVRQOL. Our data suggested that the pVHI may provide more useful details regarding the effects of different types of voice disorders on the quality of life than the pVRQOL.
Correlational analysis showed that the scores for the two questionnaires were moderately to strongly correlated. Because both the pVHI and the pVRQOL were based on similar concepts for measuring voice-related quality of life, they may reflect parents’ perceptions on the functional, physical, and emotional aspects of voice disorders in their children. This finding was comparable to the findings of previous studies, which reported a strong correlation between the VHI and VRQOL in adult (r = −0.85 in Portone study, r = −0.90 in Gunther study).[23,24] However, the correlations differed among the dysphonic subgroups. The highest correlation was for the vocal fold polyps subgroup (r = −0.920), followed by the vocal fold nodules subgroup (r = −0.852), and chronic laryngitis subgroup (r = −0.735). These results suggested that both questionnaires have some limitations and that the combined use of both would provide more accurate information for assessing voice-related quality of life in children.
6. Conclusion
Children with voice disorders had poorer voice-related quality of life than did those without voice disorders. The pVHI and pVRQOL were useful tools for assessing children's voice-related quality of life. The pVHI showed more significant differences in the subscale scores between the different subgroups within the dysphonic group than the pVRQOL.
Author contributions
Data curation: Mengjie Huang, Dan Lu.
Methodology: Mengjie Huang, Jingsi Dong.
Writing-original draft: Dan Lu.
Writing – review and editing: Hui yang, Ivy K-Y. Cheng.
Supplementary Material
Footnotes
Abbreviations: pVHI = pediatric Voice Handicap Index, pVRQOL = pediatric Voice-Related Quality-of-Life.
The work was supported by the Sichuan Science and Technology Department Fund (grant numbers: 2017SZ0015,2016FZ0106, 2012FZ0014).
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article.
References
- [1].Roy N, Merrill RM, Thibeault S, et al. Prevalence of voice disorders in teachers and the general population. J Speech Lang Hear Res 2004;47:281–93. [DOI] [PubMed] [Google Scholar]
- [2].Seifpanahi S, Izadi F, Jamshidi AA, et al. Prevalence of voice disorders and associated risk factors in teachers and nonteachers in Iran. J Voice 2016;30:506e519-523. [DOI] [PubMed] [Google Scholar]
- [3].Connor NP, Cohen SB, Theis SM, et al. Attitudes of children with dysphonia. J Voice 2008;22:197–209. [DOI] [PubMed] [Google Scholar]
- [4].Akif Kilic M, Okur E, Yildirim I, et al. The prevalence of vocal fold nodules in school age children. Int J Pediatr Otorhinolaryngol 2004;68:409–12. [DOI] [PubMed] [Google Scholar]
- [5].Romak JJ, Orbelo DM, Maragos NE, et al. Correlation of the Voice Handicap Index-10 (VHI-10) and Voice-Related Quality of Life (V-RQOL) in patients with dysphonia. J Voice 2014;28:237–40. [DOI] [PubMed] [Google Scholar]
- [6].Lam PK, Chan KM, Ho WK, et al. Cross-cultural adaptation and validation of the Chinese Voice Handicap Index-10. Laryngoscope 2006;116:1192–8. [DOI] [PubMed] [Google Scholar]
- [7].Mozzanica F, Robotti C, Ginocchio D, et al. Cross-Cultural Adaptation and Validation of the Italian Version of the Voice Symptom Scale (I-VoiSS). J Voice 2017;31:773.e1–0. [DOI] [PubMed] [Google Scholar]
- [8].Niebudek-Bogusz E, Kuzanska A, Woznicka E, et al. Assessment of the voice handicap index as a screening tool in dysphonic patients. Folia Phoniatr Logop 2011;63:269–72. [DOI] [PubMed] [Google Scholar]
- [9].Zur KB, Cotton S, Kelchner L, et al. Pediatric Voice Handicap Index (pVHI): a new tool for evaluating pediatric dysphonia. Int J Pediatr Otorhinolaryngol 2007;71:77–82. [DOI] [PubMed] [Google Scholar]
- [10].Boseley ME, Cunningham MJ, Volk MS, et al. Validation of the Pediatric Voice-Related Quality-of-Life survey. Arch Otolaryngol Head Neck Surg 2006;132:717–20. [DOI] [PubMed] [Google Scholar]
- [11].Naraghi M, Adil S, Bastaninejad S, et al. Evaluation of Pediatric Voice Handicap Index and Pediatric Voice Related Quality of Life before and after adenotonsillectomy in pediatric population. Int J Pediatr Otorhinolaryngol 2015;79:388–91. [DOI] [PubMed] [Google Scholar]
- [12].Lu D, Huang M, Li Z, et al. Adaptation and validation of Mandarin Chinese version of the pediatric Voice Handicap Index (pVHI). Int J Pediatr Otorhinolaryngol 2018;104:19–24. [DOI] [PubMed] [Google Scholar]
- [13].Lu D, Huang M, Li Z, et al. Validation of the Mandarin Chinese Version of the Pediatric Voice-Related Quality of Life (pVRQOL). J Voice 2017. [DOI] [PubMed] [Google Scholar]
- [14].Martins RH, Hidalgo Ribeiro CB, Fernandes de Mello BM, et al. Dysphonia in children. J Voice 2012;26:674e617-620. [DOI] [PubMed] [Google Scholar]
- [15].Eisenbeis JF, Fuller DP. Voice disorders: abuse, misuse and functional problems. Mo Med 2008;105:240–3. [PubMed] [Google Scholar]
- [16].D’Oosterlinck F, Broekaert E, De Wilde J, et al. Characteristics and profile of boys and girls with emotional and behavioural disorders in Flanders mental health institutes: a quantitative study. Child Care Health Dev 2006;32:213–24. [DOI] [PubMed] [Google Scholar]
- [17].Pawlowski CS, Tjornhoj-Thomsen T, Schipperijn J, et al. Barriers for recess physical activity: a gender specific qualitative focus group exploration. BMC Public Health 2014;14:639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Mohammadzadeh A, Sandoughdar N. Prevalence of voice disorders in Iranian primary school students. J Voice 2017;31:263e213-263 e218. [DOI] [PubMed] [Google Scholar]
- [19].Pawlowski CS, Andersen HB, Troelsen J, et al. Children's physical activity behavior during school recess: a pilot study using GPS, accelerometer, participant observation, and go-along interview. PLoS One 2016;11:e0148786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Schindler A, Tiddia C, Ghidelli C, et al. Adaptation and validation of the Italian Pediatric Voice Handicap Index. Folia Phoniatr Logop 2011;63:9–14. [DOI] [PubMed] [Google Scholar]
- [21].Park SS, Kwon TK, Choi SH, et al. Reliability and validity of the Korean version of Pediatric Voice Handicap Index: in school age children. Int J Pediatr Otorhinolaryngol 2013;77:107–12. [DOI] [PubMed] [Google Scholar]
- [22].Gasparini G, Behlau M. Quality of life: validation of the Brazilian version of the voice-related quality of life (V-RQOL) measure. J Voice 2009;23:76–81. [DOI] [PubMed] [Google Scholar]
- [23].Portone CR, Hapner ER, McGregor L, 3rd, et al. Correlation of the Voice Handicap Index (VHI) and the Voice-Related Quality of Life Measure (V-RQOL). J Voice 2007;21:723–7. [DOI] [PubMed] [Google Scholar]
- [24].Gunther S, Rasch T, Klotz M, et al. [Determination of subjective impairment in dysphonia. A methodological comparison]. HNO 2005;53:895–900. 902-904. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


