Abstract
Background:
A rigid video-stylet intubation device provides safe and accurate access to the trachea by enabling visualization of the airway structures during tracheal intubation. The primary purpose of this study was to examine the effects of glycopyrrolate premedication on tracheal intubation with a rigid video-stylet.
Methods:
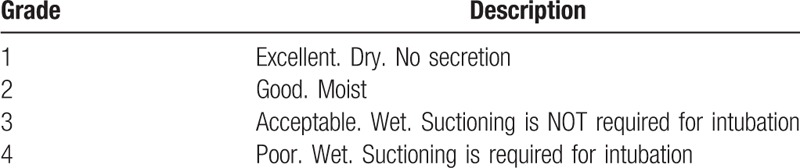
In this prospective, randomized, double-blinded study, 78 patients were randomly assigned to the control group (n = 39; no glycopyrrolate administration) or the glycopyrrolate group (n = 39; 0.005 mg/kg glycopyrrolate, intramuscular injection). A rigid video-stylet was used for tracheal intubation. The degree of oral secretion observed through the video-stylet monitor was assessed using the OptiScope laryngeal view and graded on a 4-point scale (1, excellent; 2, good; 3, poor; and 4, unacceptable). The time to intubation and hemodynamic variables at baseline and 1, 3, and 5 minutes after intubation were recorded.
Results:
The OptiScope laryngeal view grades of the glycopyrrolate group (grade 1 = 16 [41.0%], 2 = 17 [43.6%], 3 = 6 [15.4%], and 4 = 0 [0%]) were significantly higher than those of the control group (grade 1 = 9 [23.1%], 2 = 11 [28.2%], 3 = 18 [46.2%], and 4 = 1 [2.6%]; P = .02). The intubation time was shorter in the glycopyrrolate group (18.5 seconds [15.0–22.0]) than the control group (22.0 seconds [17.9–26.4], P = .02). There was no significant difference in the hemodynamic variables between groups.
Conclusion:
Glycopyrrolate facilitated tracheal intubation with a rigid video-stylet by decreasing oral secretions and providing better visualization and faster intubation with hemodynamic stability.
Trial registry:
www.clinicaltrials.gov; Identifier: NCT03050242.
Keywords: glycopyrrolate, intubation, premedication, video-stylet
1. Introduction
The rigid video-stylet (OptiScope, KoMAC Co, Ltd, Seoul, Republic of Korea) is a novel intubating device that incorporates video technologies into airway management.[1] It consists of a handle with a detachable LCD monitor and a malleable stylet with a camera lens at the tip. By providing a real-time image of airway structures, it increases the intubation success rate and decreases the intubation time.[2–4] The rigid video-stylet requires minimum scooping movements for manipulation and can be used safely, with less trauma to the airways and less hemodynamic instability.[3–5] Moreover, in patients with difficult airways or limited cervical motion, a rigid video-stylet performs better than conventional airway devices.[6–9] However, deterioration of the view might lead to intubation failure, resulting in multiple intubation attempts, a longer intubating time, and desaturation.[1,5] Therefore, unlike the conventional laryngoscope, decreased oral secretion might provide the advantage of better visualization of the rigid video-stylet.
Anticholinergic agents are widely administered prior to endoscopic and airway procedures to reduce oral secretions and to prevent vagal reflex.[10–14] However, anticholinergics are associated with adverse effects on hemodynamic parameters such as tachycardia, arrhythmia, and excessive hypertension. Moreover, these reactions may be exaggerated when combined with tracheal intubation, which provokes strong hemodynamic responses.[10–12] Remifentanil, a rapid-acting opioid, is known to effectively attenuate hemodynamic responses to the painful stimuli of tracheal intubation or surgical incision.[15] Therefore, remifentanil may control adverse hemodynamic responses to anticholinergic agents.
We hypothesized that intramuscular glycopyrrolate premedication might facilitate tracheal intubation with the rigid video-stylet with hemodynamic stability under general anesthesia. This study was designed to evaluate the efficacy and safety of intramuscular glycopyrrolate as a premedication prior to tracheal intubation using a rigid video-stylet. Specifically, we compared the degree of airway secretion and the intubation time between patients who received glycopyrrolate premedication and those who did not. We also compared hemodynamic variables during tracheal intubation.
2. Materials and methods
This randomized-controlled study was approved by the Institutional Review Board of Kangbuk Samsung Hospital (Kangbuk Samsung Hospital Institutional Review Board, Seoul, Republic of Korea; approval number: KBSMC 2017-01-001) and internationally registered at ClinicalTrials.gov (NCT03050242). Written informed consent was obtained from all patients enrolled. ASA physical class 1 or 2 patients 19 to 65 years of age scheduled for elective surgery under general anesthesia were included. The exclusion criteria were as follows: body mass index above 30; expected difficult intubation due to intraoral mass, history of difficult intubation, or limited mouth opening.
2.1. Study groups and randomization
Patients were randomly allocated into a control group and a glycopyrrolate group. The randomization was performed by an independent anesthesiologist who used a permuted block randomization algorithm (interactive internet-based response system, http://www.randomization.com) and kept the codes in sealed envelopes, in order. The group allocation was performed by the anesthesiologist the day before surgery. Another investigator who was blinded to the group assignment conducted tracheal intubations and patient assessments. Patients in the control group did not receive premedication. Patients in the glycopyrrolate group received an intramuscular injection of glycopyrrolate (0.005 mg/kg) 1 hour before surgery.
2.2. Anesthesia and parameters investigated
Before entering the operating room, airway assessments including the Mallampati class, interincisor distance, neck extension limitation, and thyromental distance were performed. After the patient entered the operating room, ASA standard monitoring including electrocardiography, noninvasive blood pressure, and pulse oximetry were performed. The baseline mean blood pressure (MBP), heart rate (HR), and peripheral oxygen saturation (SpO2) were recorded. To monitor the depth of anesthesia, the Entropy EasyFit Sensor (GE Healthcare, Helsinki, Finland) was applied. Neuromuscular relaxation was monitored at the adductor pollicis muscle with a TOF Watch SX monitor (Essex Pharma GmbH, Munich, Germany). Preoxygenation with 100% O2 was administered for 3 minutes. Anesthesia was induced with intravenous propofol (1.5 mg/kg) and intravenous remifentanil (1 mcg/kg). After the state entropy decreased below 60, proper mask ventilation was checked and intravenous rocuronium (0.8 mg/kg) was administered. A rigid video-stylet (OptiScope PM201, KoMAC Co, Ltd) was used for tracheal intubation. The intubation was performed using the standard method with the device held in the dominant hand and the chin lifted anteriorly with the nondominant hand.[16] No additional external manipulation facilitating the laryngeal view was conducted. All intubations was conducted by 1 anesthesiologist (E-AC) with an experience of performing more than 30 OptiScope-guided intubations. After the location of the vocal cords was confirmed, the rigid video-stylet was inserted into the trachea and the endotracheal tube was advanced under direct visualization. The rigid video-stylet was then withdrawn and the anesthesia circuit was connected. After ballooning the tracheal tube, proper endotracheal insertion was confirmed with the capnographic wave. A 7-mm tracheal tube was used for female subjects and a 7.5-mm tube was used for male subjects. The amount of oral secretion was observed through the rigid video-stylet monitor and assessed using a 4-point scale, as follows: 1, excellent = dry without secretions; 2, good = moist; 3, poor = wet, but suctioning is not required to intubate; 4, unacceptable = wet, suctioning is required to intubate (Table 1). In case of a grade 4 assessment, oral clearing was performed using the Yankauer suction tip and a second intubation with a rigid video-stylet was conducted. If the second attempt failed, it was recorded as “fail” and conventional laryngoscopic intubation was performed. Time to intubation was defined as the time from the introduction of the rigid video-stylet into the mouth to visualization of the first capnographic wave. For grade 4 patients, the time from the first insertion of the rigid video-stylet to withdrawal and the time from the second insertion to the first capnographic appearance were added. MBP, HR, and SpO2 were obtained at 1, 3, and 5 minutes after intubation. A desaturation event was defined by SpO2 of <90%. After confirming successful tracheal intubation, anesthesia was maintained with the conventional balanced anesthesia method using a continuous remifentanil infusion (0.01–0.15 mcg/kg per min) and 1 to 2 vol % sevoflurane in a 50% air/oxygen mixture.
Table 1.
Four-point grading scale of the OptiScope laryngeal view.
2.3. Sample size estimation
The primary outcome of this study was the degree of oral secretion. From our preliminary study, the degrees of secretion on a 4-point scale were 1.73 ± 0.70 (n = 15) for the glycopyrrolate group and 2.4 ± 0.91 (n = 15) for the control group. Based on the preliminary study, a sample size of 30 patients per group was needed for an alpha error of 0.05 and a power of 80%. Considering a drop-out rate of 30%, 78 patients were required for this study.
2.4. Statistical analysis
The Shapiro–Wilk test was used to test normal distribution for the continuous variables. Continuous variables are stated as mean ± standard deviation or median (interquartile range), and categorical variables are presented as numbers (percentage). The Student t test for normally distributed data and the Mann–Whitney U test for non-normally distributed data were used to compare the 2 groups. Categorical variables were analyzed using the chi-squared test or the Fisher exact test as appropriate. A P value < .05 was considered significant. The MBP and HR values during intubation were compared with the between-subjects effects test using a repeated-measures analysis of variance (ANOVA). IBM SPSS Statistics for Windows, Version 24.0 (IBM Corp, Armonk, NY) was used for data analyses.
3. Results
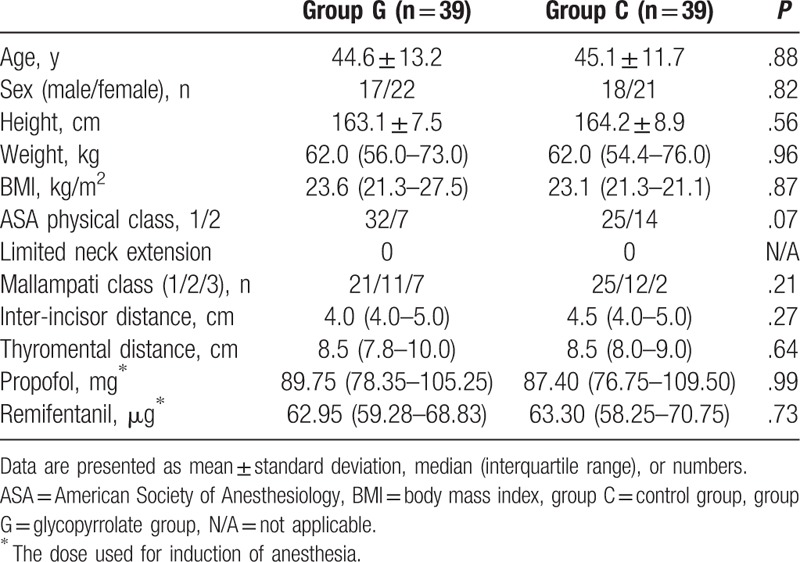
Seventy-eight patients were enrolled in this study between March 2017 and May 2017 (Fig. 1). Baseline characteristics of the patients and airway evaluations were not different between groups (Table 2).
Figure 1.
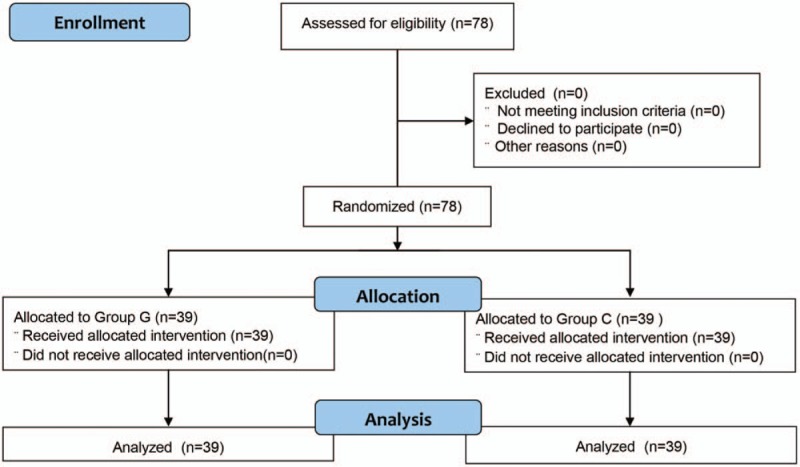
CONSORT flow diagram. Group C = control group, group G = glycopyrrolate group.
Table 2.
Baseline characteristics, airway assessments, and clinical data of subjects.
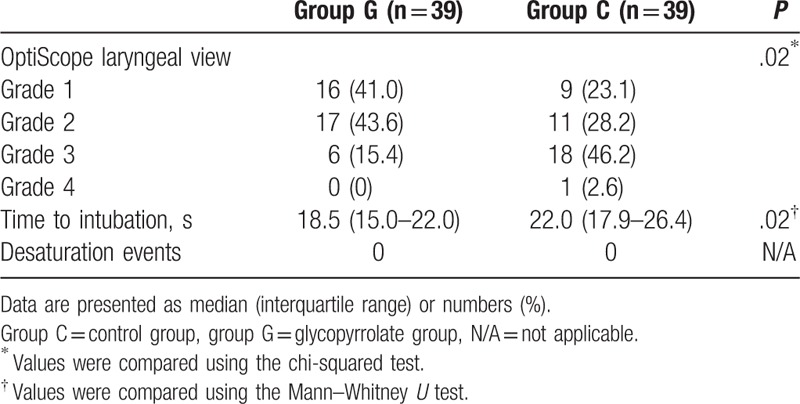
The OptiScope laryngeal view grade of the glycopyrrolate group was higher (grade 1 = 16 [41.0%], 2 = 17 [43.6%], 3 = 6 [15.4%], and 4 = 0 [0%]) than that of the control group (grade 1 = 9 [23.1%], 2 = 11 [28.2%], 3 = 18 [46.2%], and 4 = 1 [2.6%]; P = .02). The time to intubation was shorter in the glycopyrrolate group (18.5 seconds [15.0–22.0]) than in the control group (22.0 seconds [17.9–26.4], P = .02). There was no desaturation event in either group (Table 3).
Table 3.
Degree of secretion, time to intubation, and occurrence of desaturation events during intubation with an OptiScope.
The MAP was not different between groups before induction of anesthesia or at 1, 3, or 5 minutes after intubation (Fig. 2A). The HR was faster in the glycopyrrolate group at 3 (79.0 [13.3] vs 71.2 [12.5], P = .009) and 5 minutes (75.7 [12.1] vs 70.0 [11.3], P = .01) after intubation (Fig. 2B).
Figure 2.
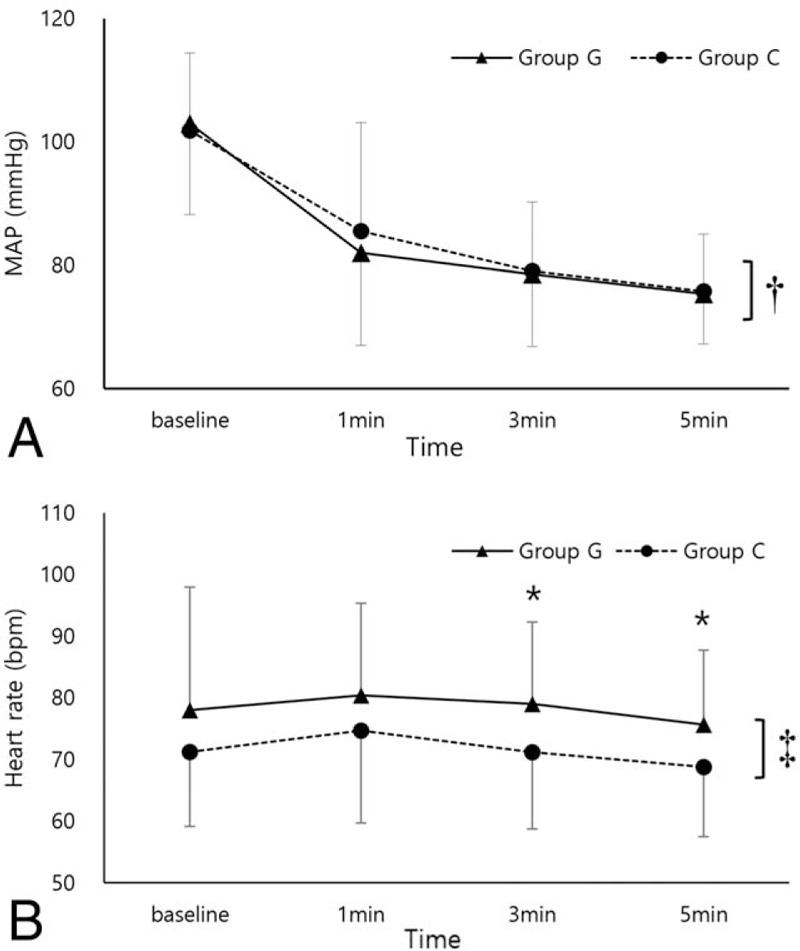
(A) MAP before induction of anesthesia (baseline) and 1, 3, and 5 minutes after intubation (mean [SD]). (B) HR before induction of anesthesia (baseline) and 1, 3, and 5 minutes after intubation (mean [SD]). ANOVA = analysis of variance, Group C = control group, group G = glycopyrrolate group, HR = heart rate, MAP = mean arterial pressure, SD = standard deviation. ∗P < .05; values were compared using the Student t test. †P = .95; compared using the between-subjects effects test of a repeated-measures ANOVA. ‡P = .03; compared using the between-subjects effects test of a repeated-measures ANOVA.
4. Discussion
This prospective randomized-controlled study evaluated whether glycopyrrolate premedication can reduce oral secretions and facilitate tracheal intubation using a rigid video-stylet with hemodynamic stability. We found significant differences in the OptiScope laryngeal view and the intubation time between the groups. In addition, hemodynamic variables remained stable, in the normal range, in both groups.
Anticholinergic premedication has long been used in general anesthesia.[16] It reduces oral secretions and provides better conditions for the various procedures to manipulate the airway.[10,12,14] Moreover, anticholinergic administration prior to surgery might prevent vagal overstimulation during surgery that causes severe bradycardia.[11–13] However, its routine use as a premedication for general anesthesia has been questioned for several reasons. First, irritation of the airway by the anesthetic gas is no longer a concern due to modern anesthetic techniques. Second, regarding airway visualization, there are minor benefits of the conventional intubation method using the laryngoscope.[17,18] Last, blocking of the parasympathetic nervous system due to anticholinergic drugs might cause tachyarrhythmias or hypertension during intubation.[18] This effect might be more pronounced in the presence of pre-existing cardiac problems, resulting in myocardial ischemia or infarction, atrioventricular dissociation, and ventricular fibrillation.[11,17,19]
The rigid video-stylet allows faster tracheal intubation and a better intubation success rate than conventional laryngoscopy.[2–4,20] For successful manipulation, good visualization of the laryngeal view is necessary. In this point of view, a previous study demonstrated that adjustment of the airway manipulation maneuvers facilitated the laryngeal view of the rigid video-stylet.[21] Although airway manipulation might improve the laryngeal view, a number of the difficulties of rigid video-stylet use are related to uncontrolled oral secretions.[22] Therefore, we assumed that reduction of the secretions would improve the performance of the rigid video-stylet.
A common method for the reduction of oral secretions is to administer anticholinergic drugs. However, to our knowledge, there have been no previous studies in which anticholinergic premedication improved the performance of tracheal intubation. Some studies have examined various types of endoscopic procedures.[10,14,23,24] In most of those studies, intramuscular anticholinergic agents did not improve the performance of the procedure.[10,14,24] However, in our study, there was a significant reduction in oral secretions in the glycopyrrolate group, and the time necessary for successful intubation was significantly shorter compared to the control group. We presume that the different results were caused by the different characteristics of the procedure. Unlike the endoscopic procedures, tracheal intubation strongly relies on the conditions of the upper airway. Therefore, we report that the antisialogogic effect of glycopyrrolate improved the performance of intubation with the rigid video-stylet.
Although less effective than atropine, intramuscular glycopyrrolate is associated with tachycardia and hypertension.[10,12] In the present study, we used intravenous remifentanil to blunt the cardiogenic responses related to intubation. Remifentanil is a rapid-acting opioid characterized by a short, context-sensitive half-life.[25,26] When used with hypnotic agents such as propofol, remifentanil effectively reduced sympathetic activation after tracheal intubation.[25] Even though the MAP after intubation was not different between groups, the HR was significantly higher in the glycopyrrolate group, particularly at 3 and 5 minutes after intubation. However, the values remained within the acceptable range throughout the study period (79.0 ± 13.3 after 3 minutes, 75.5 ± 12.1 after 5 minutes). Therefore, we report that when the correct hypnotic and analgesic levels are achieved, glycopyrrolate can be safely administered without a sympathetic over-reactivation due to tracheal intubation.
Our study had some limitations. First, it was performed under general anesthesia. Therefore, we used high-dose propofol and remifentanil to control the sympathetic over-reactivation to endotracheal stimulation, so we could not determine if hemodynamic stability can also be achieved under light sedation. Second, this study included hemodynamically stable patients with normal airways. Therefore, we could not determine if these results might be extrapolated to difficult airway settings or hemodynamically unstable patients. We may assume that glycopyrrolate might improve visualization in patients for whom intubation using the rigid video-stylet is planned. However, whether this can decrease the intubation time or dramatically facilitate the intubation performance in difficult airways requires further study. Moreover, hemodynamically vulnerable patients, such as those with known severe heart and lung diseases, must be treated carefully because there may be an exaggerated reaction to the anticholinergic agent. Finally, even though the investigator was blinded to the group allocation, the investigator might have noticed whether glycopyrrolate had been administered by inspecting reduced salivation during intubation.
In conclusion, we demonstrated that glycopyrrolate premedication improved the efficacy of intubation using a rigid video-stylet and provided hemodynamic stability. Therefore, when the use of a rigid video-stylet is planned for intubation, patients can be safely and effectively pretreated with glycopyrrolate for better performance.
Author contributions
Data curation: Sung-Ha Hwang.
Formal analysis: Sung Hyun Lee.
Methodology: Sung Hyun Lee.
Supervision: Yun-Hong Kim.
Writing – original draft: Eun-Ah Cho.
Writing – review and editing: Kyoung-Ho Ryu.
Footnotes
Abbreviations: ASA = American Society of Anesthesiology, HR = heart rate, MBP = mean blood pressure, SpO2 = peripheral oxygen saturation.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Liem EB, Bjoraker DG, Gravenstein D. New options for airway management: intubating fibreoptic stylets. Br J Anaesth 2003;91:408–18. [DOI] [PubMed] [Google Scholar]
- [2].Szarpak L, Truszewski Z, Czyzewski L, et al. Child endotracheal intubation with a Clarus Levitan fiberoptic stylet vs Macintosh laryngoscope during resuscitation performed by paramedics: a randomized crossover manikin trial. Am J Emerg Med 2015;33:1547–51. [DOI] [PubMed] [Google Scholar]
- [3].Yang M, Kim JA, Ahn HJ, et al. Double-lumen tube tracheal intubation using a rigid video-stylet: a randomized controlled comparison with the Macintosh laryngoscope. Br J Anaesth 2013;111:990–5. [DOI] [PubMed] [Google Scholar]
- [4].Hsu HT, Chou SH, Chen CL, et al. Left endobronchial intubation with a double-lumen tube using direct laryngoscopy or the Trachway® video stylet. Anaesthesia 2013;68:851–5. [DOI] [PubMed] [Google Scholar]
- [5].Ko DD, Kang H, Yang SY, et al. A comparison of hemodynamic changes after endotracheal intubation by the OptiScope and the conventional laryngoscope. Korean J Anesthesiol 2012;63:130–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Seo H, Kim E, Son JD, et al. A prospective randomised study of a rigid video-stylet vs. conventional lightwand intubation in cervical spine-immobilised patients. Anaesthesia 2016;71:1341–6. [DOI] [PubMed] [Google Scholar]
- [7].Weiss M, Schwarz U, Gerber AC. Difficult airway management: comparison of the Bullard laryngoscope with the video-optical intubation stylet. Can J Anaesth 2000;47:280–4. [DOI] [PubMed] [Google Scholar]
- [8].Kim JK, Kim JA, Kim CS, et al. Comparison of tracheal intubation with the Airway Scope or Clarus Video System in patients with cervical collars. Anaesthesia 2011;66:694–8. [DOI] [PubMed] [Google Scholar]
- [9].Hung KC, Tan PH, Lin VC, et al. A comparison of the Trachway intubating stylet and the Macintosh laryngoscope in tracheal intubation: a manikin study. J Anesth 2013;27:205–10. [DOI] [PubMed] [Google Scholar]
- [10].Malik JA, Gupta D, Agarwal AN, et al. Anticholinergic premedication for flexible bronchoscopy: a randomized, double-blind, placebo-controlled study of atropine and glycopyrrolate. Chest 2009;136:347–54. [DOI] [PubMed] [Google Scholar]
- [11].Mirakhur RK, Clarke RSJ, Dundee JW, et al. Anticholinergic drugs in anaesthesia. Anaesthesia 1978;33:133–8. [DOI] [PubMed] [Google Scholar]
- [12].Mirakhur RK, Dundee JW, Connolly JD. Studies of drugs given before anaesthesia. XVII: anticholinergic premedicants. Br J Anaesth 1979;51:339–45. [DOI] [PubMed] [Google Scholar]
- [13].Coventry DM, McMenemin I, Lawrie S. Bradycardia during intra-abdominal surgery. Anaesthesia 1987;42:835–9. [DOI] [PubMed] [Google Scholar]
- [14].Cowl CT, Prakash UB, Kruger BR. The role of anticholinergics in bronchoscopy. A randomized clinical trial. Chest 2000;118:188–92. [DOI] [PubMed] [Google Scholar]
- [15].Albertin A, Casati A, Federica L, et al. The effect-site concentration of remifentanil blunting cardiovascular responses to tracheal intubation and skin incision during bispectral index-guided propofol anesthesia. Anesth Analg 2005;101:125–30. [DOI] [PubMed] [Google Scholar]
- [16].Mirakhur RK. Preanaesthetic medication: a survey of current usage. J R Soc Med 1991;84:481–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Pisano A. Atropine for premedication: is no longer the time to be nostalgic. Minerva Anestesiol 2014;80:123–4. [PubMed] [Google Scholar]
- [18].Falick YS, Smiler BG. Is anticholinergic premedication necessary? Anesthesiology 1975;43:472–3. [DOI] [PubMed] [Google Scholar]
- [19].Eikard B, Andersen JR. Arrhythmias during halothane anaesthesia II: the influence of atropine. Acta Anaesthesiol Scand 1977;21:245–51. [DOI] [PubMed] [Google Scholar]
- [20].Mihai R, Blair E, Kay H, et al. A quantitative review and meta-analysis of performance of non-standard laryngoscopes and rigid fibreoptic intubation aids. Anaesthesia 2008;63:745–60. [DOI] [PubMed] [Google Scholar]
- [21].Lee AR, Yang S, Shin YH, et al. A comparison of the BURP and conventional and modified jaw thrust manoeuvres for orotracheal intubation using the Clarus Video System. Anaesthesia 2013;68:931–7. [DOI] [PubMed] [Google Scholar]
- [22].Halligan M, Charters P. A clinical evaluation of the Bonfils intubation fibrescope. Anaesthesia 2003;58:1087–91. [DOI] [PubMed] [Google Scholar]
- [23].Kim EJ, Um MY, Kim KO, et al. Safety and efficacy of glycopyrrolate as a premedication for endoscopic submucosal dissection: a randomized, double-blind, placebo-controlled study. Endoscopy 2017;49:949–56. [DOI] [PubMed] [Google Scholar]
- [24].Cattau EL, Jr, Artnak EJ, Castell DO, et al. Efficacy of atropine as an endoscopic premedication. Gastrointest Endosc 1983;29:285–8. [DOI] [PubMed] [Google Scholar]
- [25].Burkle H, Dunbar S, Van Aken H. Remifentanil: a novel, short-acting, mu-opioid. Anesth Analg 1996;83:646–51. [DOI] [PubMed] [Google Scholar]
- [26].Dershwitz M, Randel GI, Rosow CE, et al. Initial clinical experience with remifentanil, a new opioid metabolized by esterases. Anesth Analg 1995;81:619–23. [DOI] [PubMed] [Google Scholar]


