Abstract
The outcomes of cervical disc arthroplasty (CDA) following a previous fusion are ill -defined. The aim of this study was to share our experience and to assess mid-term outcomes in patients receiving CDA adjacent to a previous fusion compared with primary CDA.
Patients with cervical radiculopathy and/or myelopathy or patients who had undergone a previous cervical fusion surgery and had developed adjacent segment disease (ASD) between January 2008 and April 2013 were enrolled. Clinical and radiographic outcomes were compared for patients undergoing CDA at a level adjacent to a previous fusion (previous group) and those undergoing primary CDA (primary group).
Fifty-two patients in the primary group and 9 patients in the previous group had adequate follow-up data. The mean follow-up periods were 61.96 months and 61.78 months, respectively. The clinical outcomes all significantly improved after surgery, and no significant difference was found between groups. The disc height and range of motion of the operated level were preserved, and the values were similar between groups. Subsidence occurred in 2 (3.8%) patients in the primary group and 1 (11.11%) patient in the previous group. Heterotopic ossification (HO) was detected in 4 (44.44%) patients in the previous group and 18 (34.62%) patients in the primary group. None of the patients required reoperation.
Patients treated with a Prestige-LP disc maintained improved clinical outcomes and segmental motion in both the primary and previous groups. Additionally, CDA-treated patients who had a previous fusion surgery could safely undergo the surgery with complication rates similar to that of the first CDA surgery after 48 months of follow-up. CDA adjacent to a previous fusion may be an alternative treatment strategy in the future.
Keywords: adjacent segment disease, cervical disc arthroplasty, fusion, prestige-LP, previous cervical surgery
1. Introduction
Anterior cervical discectomy and fusion (ACDF) is the most acceptable surgical treatment for cervical degenerative disc disease with a favorite clinical outcome. Although this procedure has been greatly beneficial for alleviating symptoms and reconstructing cervical stability, researchers have noted that it significantly alters the kinematic characteristics and biomechanical environment.
Intradiscal pressure and segmental motion at levels adjacent to the fusion were significantly increased in biomechanical studies, which was attributed to early disc degeneration at adjacent levels.[1] Hilibrand et al[2] reported an annual incidence of adjacent segment disease (ASD) of 2.9% and predicted that 25.6% of patients would develop ASD, of which two-thirds would require a second surgery within the first 10 years after cervical arthrodesis. The pseudarthrosis rate increased with the number of the fused-level.[3,4] Furthermore, Hilibrand et al[5] demonstrated that the fusion rate was reduced to 63% when a second fusion was performed for ASD, and Xu et al[6] found that patients undergoing a third anterior cervical fusion obtained worse Nurick scores and neurological functions than those undergoing primary surgery.
Due to the drawbacks of ACDF, investigators have developed motion-preserving technologies, such as cervical disc arthroplasty (CDA), to determine whether this technique is beneficial for reducing the rate of ASD and other complications. Recently, several mid- to long-term follow-up studies of the continued safety and efficacy of CDA have been published.[7–10] These studies concluded that CDA could achieve similar or even better outcomes than ACDF with a lower ASD rates. However, patients with previous cervical fusion were excluded from most of these studies, even though a target adjacent to a previous fusion met the criteria for CDA. Although a biomechanical study has demonstrated that patients with adjacent level pathology were potential candidates for arthroplasty,[11] few reports have investigated the outcomes of CDA following a previous fusion. Furthermore, studies in the literature, designed specifically to compare primary CDA and secondary CDA for ASD are sparse.[12]
The current study aims to share our experience regarding the treatment of patients with ASD, to compare the outcomes between primary CDA and CDA adjacent to a previous fusion treated with a Prestige-LP disc (Medtronic Sofamor Danek, Memphis, TN) and to evaluate the mid-to long-term results of CDA for the treatment of cervical degenerative disc disease.
2. Materials and methods
2.1. Patient population
This study was a retrospective study. Between January 2008 and April 2013, we retrospectively reviewed our department database to identify patients who had received CDA. The inclusion criteria were as follows: patients with one-level cervical radiculopathy and/or myelopathy who were unresponsive to at least 6 weeks of conservative treatment, including a soft cervical collar, physiotherapy and anti-inflammatory medications, and patients with a previously successful cervical fusion surgery who were diagnosed with adjacent segment disease. The following patients were excluded: patients with 2 or more levels of symptomatic cervical degenerative disc disease for primary arthroplasty; patients with marked radiographic cervical instability, radiographic confirmation of severe facet joint degeneration, congenital canal stenosis and loss of segmental mobility; patients diagnosed with osteoporosis, a tumor, a surgical site or systemic infection and trauma; and patients with a follow-up period of <48 months. All patients provided written informed consent, and the study protocol was approved by the Ethics Committee of West China Hospital of Sichuan University. The patients were divided into 2 groups (primary and previous). The primary group contained patients who underwent CDA as their first anterior cervical procedure for cervical radiculopathy and/or myelopathy, whereas the previous group included patients who received CDA adjacent to a previous cervical fusion for ASD.
2.2. Surgical techniques
All operations were performed by the same senior spine surgeon (HL). After general anesthesia induction, an endotracheal tube was inserted and the surgery was performed in a supine position with slight extension of the head under C-arm fluoroscopic guidance. For patients in the primary group, a standard right-sided anterior cervical approach was used. Complete discectomy and decompression were performed by removing the disc tissue, posterior longitudinal ligament and osteophytes. The endplates were prepared using a burr to ensure that they were flat and parallel to each other with care taken simultaneously to preserve as much cortical bone as possible. After an appropriately sized Implant Trial confirmed the disc space, the corresponding Prestige-LP disc was tapped into the prepared disc space with channels in the endplates. For patients in the previous group, the surgery was performed through the original incision. If an anterior cervical plate was present, it was removed before decompression at the index level, although removal was not mandatory. Other procedures were similar to those in the primary group. C-arm fluoroscopy was used to certify proper placement of the prosthesis. Finally, a drain was inserted before closure of the incision.
2.3. Postoperative management
The drain was removed 2 days after surgery. All patients were encouraged to ambulate postoperatively, were instructed to perform neck function training within the first 3 postoperative weeks and then were immobilized with a collar for 4 weeks. Postoperative nonsteroidal anti-inflammatory drugs were routinely used for 2 weeks unless otherwise contraindicated.
2.4. Data collection
The collected data incorporated population characteristics and clinical and radiological evaluations. The patients were required to undergo regular follow-up visits at routine postoperative intervals of 1 week, 3, 6, and 12 months and yearly thereafter. Patient self-reported outcome questionnaires, including the Japanese Orthopedic Association (JOA), Neck Dysfunction Index (NDI) and visual analog scale (VAS), were administered at all time points. Static and dynamic radiographs and 3-dimensional computed tomography (CT) were performed at every follow-up visit. Magnetic resonance images (MRIs) were obtained only preoperatively and at the 12-month and yearly visits. The radiographic parameters, including cervical lordosis (CL), range of motion (ROM) of C2-C7, disc angle (DA), ROM of the index segment, and disc height (DH), were measured as described in previous studies.[13,14] Lordosis is described as a positive value, and kyphosis is shown as a negative value. All complications were recorded.
The radiographic assessments were made by 2 independent spine surgeons. Radiographic success after CDA was defined as at least 2° of angular motion in flexion-extension. Radiographic evidence of adjacent level changes included the presence of any of the following parameters:[13] new anterior or enlarging osteophyte formation; increased or new narrowing of the disc space defined as ≤ 25% narrowing of the intervertebral disc space; and calcification of the anterior longitudinal ligament. Heterotopic ossification (HO) was evaluated according to McAfee's classification.[15] Subsidence was defined as a greater than 2-mm reduction in the anterior DH or posterior DH immediately after surgery compared with the last follow-up.[16]
2.5. Statistical analysis
For continuous variables, comparison between the 2 groups was performed with an independent t-test or one-way analysis of variance. For categorical variables, the Chi-square test (or Fisher's exact test for small samples) was used. Dunnett's t-test was performed to compare changes from the preoperative values of the JOA, NDI, VAS, and radiographic parameters within the groups. The statistical analysis was performed using the SPSS 19.0 for Windows software (SPSS Inc., Chicago, IL). A P value of .05 was considered significant.
3. Results
3.1. Demographics
Fifty-two patients in the primary group and 9 patients in the previous group had adequate follow-up data. The patients in the primary group included 27 men and 25 women with a mean age of 43.13 years (range, 26–64 years) and a mean follow-up period of 61.96 months (range, 48–108 months). A total of 6 men and 3 women were included in the previous group with a mean age of 46.78 years (range, 38–62 years) and a mean follow-up period of 61.78 months (range, 48–96 months). A total of 10 Prestige-LP discs were implanted in these 9 patients, including 9 one-levels and 1 bi-level (Fig. 1). C5/6 was the most commonly operated level in the primary group, whereas C4/5 and C6/7 were the most commonly treated levels in the previous group. The average time to CDA after anterior fusion was 66.89 months (range, 15–124 months). Detailed patient demographic information is shown in Table 1.
Figure 1.
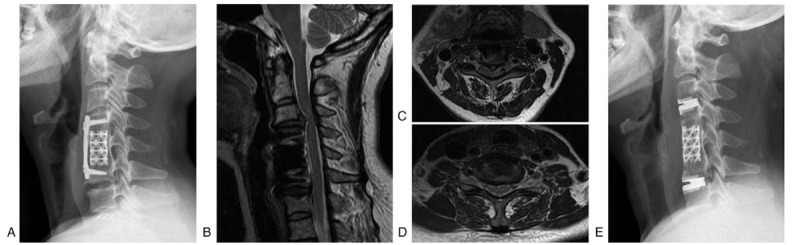
Preoperative lateral radiograph (A) of a 48-year-old woman with a previous C5 corpectomy and fusion with a symptomatic C3/4 (B, C) and C6/7 (B, D) herniated disc unresponsive to conservative treatment. Lateral radiograph (E) 1 week after surgery showing good positioning of the Prestige-LP discs at C3/4 and C6/7.
Table 1.
Summary of the demographics and perioperative parameters of the primary group and previous group (data are displayed as a number or mean ± standard deviation).

3.2. Clinical outcomes
The clinical outcomes were reflected by the JOA, NDI, and VAS scores. All scores were significantly improved after surgery compared with the preoperative values in both groups, and continued improvement was observed throughout the follow-up period (Table 2). Except for the JOA at the 3-month follow-up evaluation (P < .05), no significant differences were observed between the primary and previous groups at any evaluation time point (P > .05).
Table 2.
Mean JOA, NDI, and VAS scores of the 2 groups (mean ± standard deviation).

3.3. Radiographic outcomes
The radiographic results showed a slight increase in CL in the primary group after surgery, but this difference was not significant (P > .05). In the previous group, CL before and after surgery was similar, suggesting that the sagittal balance was preserved (Fig. 2). Furthermore, significant differences in this measurement between the 2 groups were found at the 12-month and 36-month follow-up time points (P < .05). The preoperative overall cervical ROMs in the primary and previous groups were 54.15 ± 13.74° and 40.67 ± 11.67°, respectively, which represented a significant difference at baseline (P < .05). However, the patients in both groups maintained cervical motion throughout the follow-up period. The change trend is shown in Figure 2. No significant difference was observed in the disc angle before and after surgery in either group. However, a tendency toward local kyphosis was found in the previous surgery group (Fig. 3). When all of the operated levels were grouped together, no significant difference was found between the primary and previous groups before surgery (P = .057); however, the patients in the previous group had larger preoperative disc motion (Fig. 3). The disc ROM in the previous group was maintained at 7.73 ± 2.81°, which was similar to the 8.11 ± 3.19° seen in the primary group at the 48-month follow-up. Finally, after surgery, the intravertebral DH was significantly increased in the primary group (P < .05), whereas a nonsignificant increased in this parameter was observed in the previous group (P > .05); additionally, no significant difference in this parameter was found between the 2 groups (P > .05).
Figure 2.
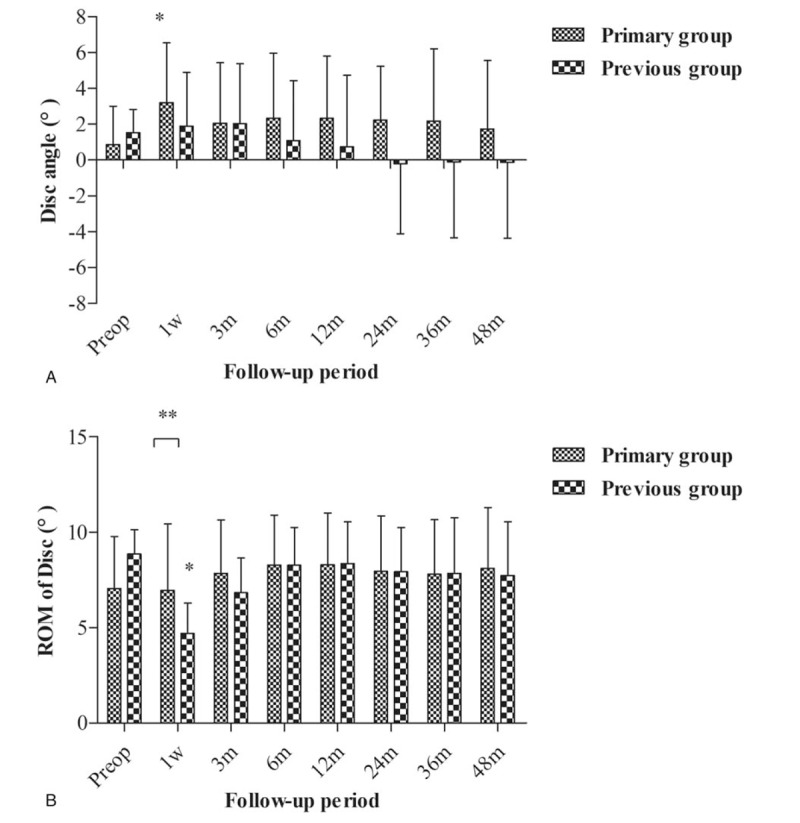
(A) Mean angle of C2–C7 and (B) mean range of motion (ROM) of C2–C7 by time point. The values at 60-month were taken from 25 patients in the primary group and five patients in the previous group. Error bars represent standard deviations. ∗P < .05, using a Dunnet's t-test to compare changes from the preoperative values within the groups. ∗∗P < .05, using an independent t-test to compare the significance between the two groups.
Figure 3.
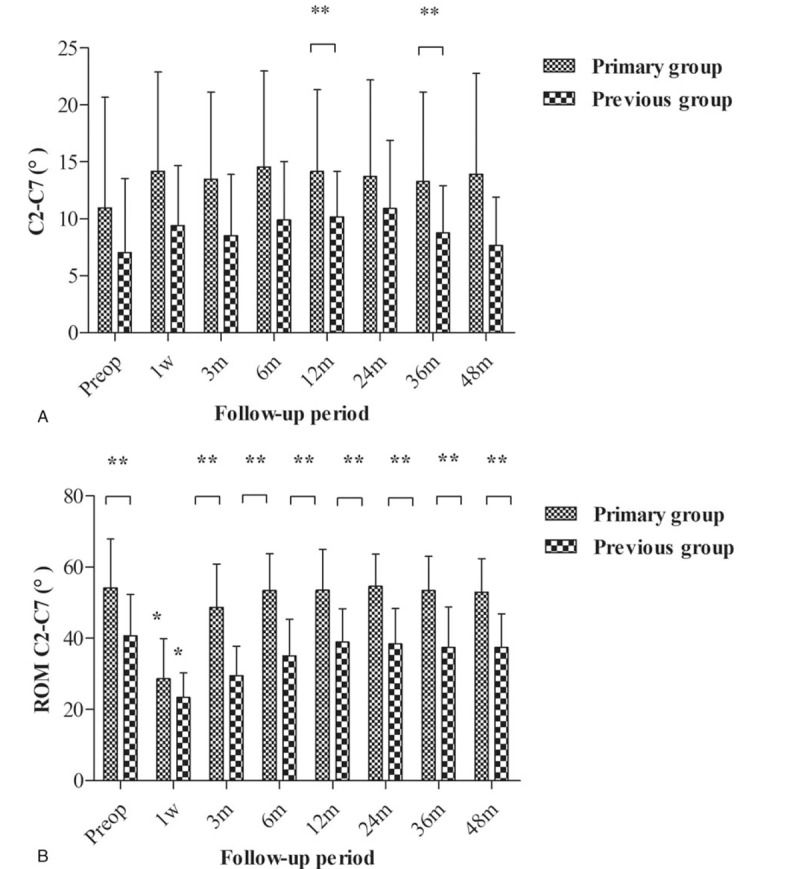
(A) Mean disc angle and (B) mean range of motion (ROM) of disc by time point. The values at 60-months were collected from 25 discs in the primary group and 6 discs in the previous group. Error bars represent standard deviations. ∗P < .05, using a Dunnet's t-test to compare changes from the preoperative values within the groups. ∗∗P < .05, using an independent t-test to compare the significance between the two groups.
3.4. Adverse events
According to the dysphagia rating described by Bazaz et al,[17] 4 (7.69%) patients in the primary group and 1 (11.11%) patient in the previous group experienced mild dysphagia after surgery (Table 3). No intraoperative complications, neurological injuries or reoperations occurred. The rates of subsidence in the primary and previous groups were 3.85% and 11.11%, respectively (Fig. 4). No symptom was found in the 4 patients, and no treatment was undertaken. HO was detected in 4 (44.44%) patients in the previous group, which was similar to the 18 (34.62%) patients detected in the primary group (P > .05). Although HO occurred in many patients, most of the devices remained mobile. Radiographic changes were detected in both groups. A total of 3 (33.3%) patients in the previous group developed radiographic changes compared with 13 (25.0%) patients in the primary group, but the difference between groups was not significant.
Table 3.
Summary of adverse events after surgery.

Figure 4.
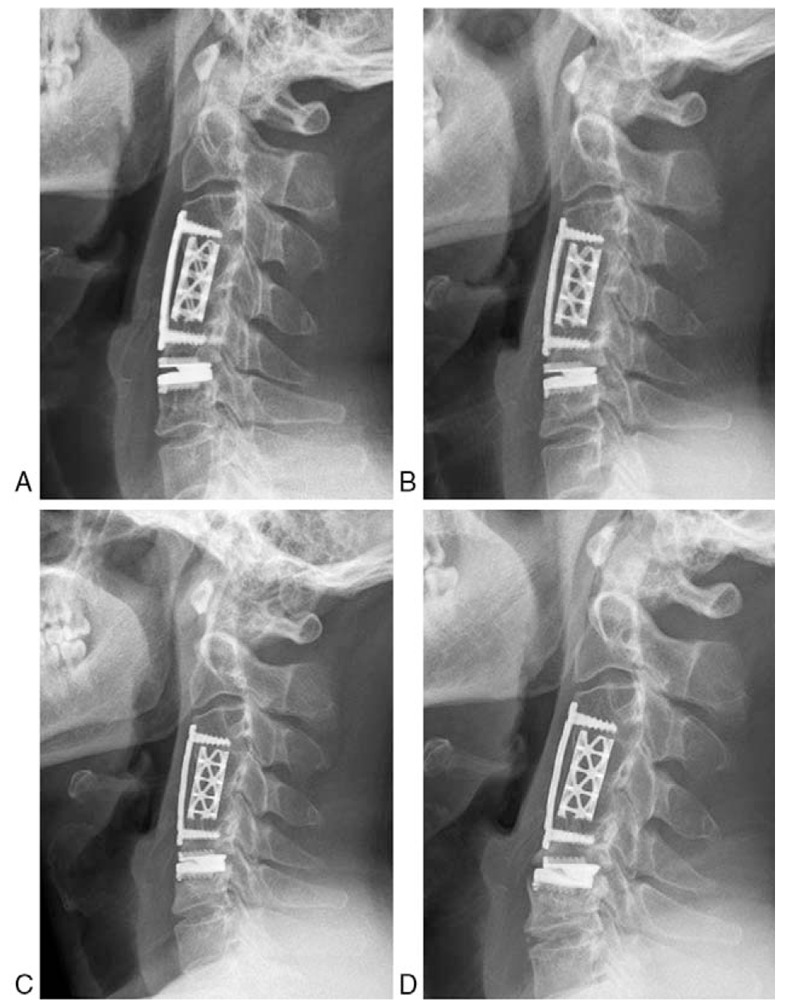
Lateral radiographs showing good positioning of the Prestige-LP disc at 1 week (A) and 6 months (B) after surgery. Subsidence was found 12 months after surgery (C). Aggravated subsidence and Class II HO was detected at the 50-month follow-up (D).
4. Discussion
Accompanied by the frequency with which ACDF is performed, the long-term consequences of ASD may worsen a patient's quality of life. Hilibrand et al[2] reported that 14% of patients received a reoperation after primary ACDF due to ASD. Eck et al[18] also concluded a similar revision rate of 15% with a larger sample. What is the course of action for a surgeon when a patient with myelopathy and/or radiculopathy is correlated with imaging evidence of cervical changes at an adjacent segment? There is no consensus on surgical treatment for ASD among spine surgeons. Matsumoto et al[19] reported that 31 patients underwent open-door expansive laminoplasty for cervical myelopathy caused by adjacent-segment disease. Hilibrand et al[5], Gause et al[20] and Xu et al[6] reported that they performed second anterior cervical fusion adjacent to a prior fusion for ASD. However, compared with primary fusion, the fusion rate was lower and the clinical outcomes were worse during the second fusion surgery.
Fewer publications have reported the outcomes of CDA for ASD. Two case reports have reported the successful restoration of operated-level motion in patients with Klippel-Feil syndrome using CDA.[21,22] Wigfield et al[23] reported that 15 patients underwent Frenchay CDA adjacent to either a previous adjacent-level surgical or congenital fusion. At 2 years, the NDI score improved by 31%, the VAS score improved by 45% and segmental motion was maintained at 6.5°. However, 3 subsequent surgeries were performed for reasons including myelopathy progression, neck pain and brachialgia. Sekhon et al[24] reported 15 patients who had previous spinal surgery including ACDF and posterior foraminotomy, and underwent Bryan CDA. After 2 years, pain relief and neurological function recovery were achieved in all cases. Segmental motion was maintained at 4.3°. Phillips et al[12] conducted a prospective study to compare clinical outcomes for 26 patients who received a PCM disc at a level adjacent to a previous fusion and 126 patients without previous fusion surgery. The patients in both groups showed significant improvement in their VAS and NDI scores after surgery, and the scores were similar between groups at all time points. Revision surgery was required for 2 of the 26 patients for ongoing neck pain and device migration.
In the current study, patients in both groups showed good recovery of symptoms, suggesting positive effects of the procedure. However, patients in the previous group had an increased NDI score after surgery. This increase may be associated with a higher ratio of myelopathy in the previous group. Before surgery, the overall cervical ROM did not have the same baseline, and the ROM of the operated disc was larger in the previous group, suggesting that a level adjacent to the fusion site made a greater contribution to the overall cervical ROM. After surgery, the Prestige-LP disc was able to preserve the ROM of the operated level, but the differences between the primary and previous groups were not significant except for data from the 60-month follow-up. Furthermore, we did not find that the ROM of the operated disc in the previous group generally increased over the levels seen in the primary group, as described by a previous study.[12] Based on previous studies, the C5/6 level had the greatest physiological motion,[25,26] and the postoperative ROM of the disc differed by the level at which it was implanted.[12] However, in our series, only 1 of 9 C5/6 levels was observed in the previous group, whereas 42 of 52 C5/6 levels were observed in the primary group. In addition, a biomechanical study indicated that a CDA adjacent to a fused level increased motion at the arthroplasty level.[11] Thus, we hypothesized that the level of implantation and abnormal biomechanical situation of the cervical spine in the previous group might explain these results.
According to previous biomechanical studies, an artificial disc at a level adjacent to fusion may provide a protective effect for adjacent levels by decreasing the abnormal hypermobility and in turn the increased stresses noted at an adjacent level.[11,27] However, the relatively higher stress on the artificial disc adjacent to the fusion raised concerns among surgeons for a higher risk of device dislocation or subsidence and accelerated device wear. In the current study, subsidence was found in both groups without a significant difference. Subsidence is most frequently reported within the first 3 months after surgery.[28] However, due to immobilization with the neck collar at the early stage after surgery, no subsidence occurred within the first 3 months in our series. One case of subsidence occurred in the previous group after 6 months, whereas 2 occurrences of subsidence were reported after 12 months in the primary group. A stress shield effect after surgery causing bone loss around the “rails” and increased forces from the adjacent fusion mass may explain these results. Moreover, a change in the center of rotation (COR) may contribute to a change in DH.[29]
HO is a well-known phenomenon following CDA. HO has been considered to damage the function of artificial discs. In the literature, the incidence of HO after CDA is discrepant, with a range from 0 to 80% for a variety of artificial cervical discs.[30,31] In our series, the overall incidence of HO was 35.00% and the incidence of Class III and IV HO was 11.76% in the primary group, which was consistent with the date from one long-term FDA-IDE trial on the Prestige-LP disc.[8] Both the overall rate of HO and the rates of Class III and Class IV were similar to the rates for those who underwent primary CDA, suggesting that CDA adjacent to a previous fusion did not increase the risk of HO.
Whether the process of adjacent disc degeneration is altered by CDA has not been addressed. In the current study, the incidence rates of radiographic changes at an adjacent level were 25.0% and 33.3% over a 48-month periods in the primary and previous groups, respectively. Goffin et al[32] reported a greater than 90% rate of adjacent-level radiographic degeneration after ACDF with 8.6 years of follow-up. Xu et al[6] reported that 27 of 108 patients required a third fusion surgery as a result of recurrent ASD within 30.3 months after a second fusion surgery. Compared with fusion surgery, CDA may have an advantage over fusion in reducing the rate of ASD and subsequent surgeries.
The current study had several limitations. First, this study is a retrospective study of primary CDA versus CDA for a previous fusion with a low level of evidence. Therefore, the results are influenced by some biases, including different numbers of patients, inclusion criteria, baseline situations and follow-up periods. This study is exploratory and has a nonconsecutive case series that is in contrast with the Phillips study, which avoided such selection bias. Second, due to the limited number of patients and the mid-term follow-up time, the study underpowered to detect a difference in either clinical or radiographic outcomes. The data in the previous group were not adequate to reach a strong conclusion. For example, the P-value of preoperative ROM of the operated level was .057, which was insufficient to detect a difference in the limited number of patients in the previous group. This study exhibited a conceptual practice at an early stage, and thus the results should be interpreted carefully. Third, patients in the previous group were inhomogeneous, for example, variable degrees of cervical degeneration were detected among the previous fusion group. Additionally, some patients underwent one-level fusion with ACDF, whereas others underwent multilevel fusion with ACDF or anterior cervical corpectomy and fusion (ACCF) before CDA. Additionally, 1 patient received a 2-level CDA.
5. Conclusion
Analysis of our results indicated that patients treated with the Prestige-LP disc maintained improved clinical outcomes and segmental motion. Additionally, CDA for the treatment of patients with a previous fusion surgery can be safely performed with a rate of complications similar to a first surgery with CDA over a 48-month follow-up. CDA adjacent to a previous fusion may be an alternative treatment strategy in the future. However, the current study was performed as a pilot study with relatively low evidence, and thus surgeons should interpret the results with caution Future prospective studies with large sample sizes that include longer follow-up are needed to confirm these findings.
Author contributions
Conceptualization: Ting-kui Wu, Yang Meng, Hao Liu, Bei-yu Wang.
Data curation: Ting-kui Wu, Yang Meng, Ying Hong.
Formal analysis: Ting-kui Wu, Yang Meng, Bei-yu Wang, Chen Ding.
Funding acquisition: Hao Liu, Bei-yu Wang.
Investigation: Xin Rong.
Methodology: Ting-kui Wu, Yang Meng, Hao Liu, Ying Hong, Xin Rong, Chen Ding.
Resources: Hao Liu, Ying Hong.
Software: Ting-kui Wu, Xin Rong, Chen Ding.
Supervision: Yang Meng, Hao Liu.
Validation: Hao Liu, Bei-yu Wang, Hua Chen.
Visualization: Yang Meng.
Writing – original draft: Ting-kui Wu.
Writing – review & editing: Yang Meng, Hao Liu, Hua Chen.
Footnotes
Abbreviations: ACCF = anterior cervical corpectomy and fusion, ACDF = anterior cervical discectomy and fusion, ASD = adjacent segment disease, CDA = cervical disc arthroplasty, CL = cervical lordosis, CT = computed tomography, DA = disc angle, DH = disc height, HO = heterotopic ossification, JOA = Japanese Orthopedic Association, MRI = magnetic resonance image, NDI = Neck Dysfunction Index, ROM = range of motion, VAS = visual analog scale.
T-kW and YM contributed equally to this work and should be considered as co-first authors.
This study is supported by the Application Base Research Program of Department of Science and Technology of Sichuan Province, China (No.2016JY0055) and the Department of Science and Technology of Sichuan Province, China (No. 2014SZ0236).
The authors have no conflicts of interest to disclose.
References
- [1].Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 2002;27:2431–4. [DOI] [PubMed] [Google Scholar]
- [2].Hilibrand AS, Carlson GD, Palumbo MA, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 1999;81:519–28. [DOI] [PubMed] [Google Scholar]
- [3].Brodke DS, Zdeblick TA. Modified Smith-Robinson procedure for anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 1992;17(10 suppl):S427–430. [DOI] [PubMed] [Google Scholar]
- [4].Bohlman HH, Emery SE, Goodfellow DB, et al. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 1993;75:1298–307. [DOI] [PubMed] [Google Scholar]
- [5].Hilibrand AS, Yoo JU, Carlson GD, et al. The success of anterior cervical arthrodesis adjacent to a previous fusion. Spine 1997;22:1574–9. [DOI] [PubMed] [Google Scholar]
- [6].Xu R, Bydon M, Macki M, et al. Adjacent segment disease after anterior cervical discectomy and fusion: clinical outcomes after first repeat surgery versus second repeat surgery. Spine 2014;39:120–6. [DOI] [PubMed] [Google Scholar]
- [7].Phillips FM, Geisler FH, Gilder KM, et al. Long-term outcomes of the US FDA IDE prospective, randomized controlled clinical trial comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2015;40:674–83. [DOI] [PubMed] [Google Scholar]
- [8].Gornet MF, Burkus JK, Shaffrey ME, et al. Cervical disc arthroplasty with prestige LP disc versus anterior cervical discectomy and fusion: seven-year outcomes. Int J Spine Surg 2016;10:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Lanman TH, Burkus JK, Dryer RG, et al. Long-term clinical and radiographic outcomes of the Prestige LP artificial cervical disc replacement at 2 levels: results from a prospective randomized controlled clinical trial. J Neurosurg Spine 2017;27:7–19. [DOI] [PubMed] [Google Scholar]
- [10].Zigler JE, Delamarter R, Murrey D, et al. ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease five-year results of a food and drug administration study. Spine 2013;38:203–9. [DOI] [PubMed] [Google Scholar]
- [11].Gandhi AA, Kode S, DeVries NA, et al. Biomechanical analysis of cervical disc replacement and fusion using single level, two Level, and hybrid constructs. Spine (Phila Pa 1976) 2015;40:1578–85. [DOI] [PubMed] [Google Scholar]
- [12].Phillips FM, Allen TR, Regan JJ, et al. Cervical disc replacement in patients with and without previous adjacent level fusion surgery: a prospective study. Spine (Phila Pa 1976) 2009;34:556–65. [DOI] [PubMed] [Google Scholar]
- [13].Kim SW, Limson MA, Kim SB, et al. Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. Eur Spine J 2009;18:218–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Grasso G. Clinical and radiological features of hybrid surgery in multilevel cervical degenerative disc disease. Eur Spine J 2015;24:842–8. [DOI] [PubMed] [Google Scholar]
- [15].McAfee PC, Cunningham BW, Devine J, et al. Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech 2003;16:384–9. [DOI] [PubMed] [Google Scholar]
- [16].Gercek E, Arlet V, Delisle J, et al. Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J 2003;12:513–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine (Phila Pa 1976) 2002;27:2453–8. [DOI] [PubMed] [Google Scholar]
- [18].van Eck CF, Regan C, Donaldson WF, et al. The revision rate and occurrence of adjacent segment disease after anterior cervical discectomy and fusion: a study of 672 consecutive patients. Spine 2014;39:2143–7. [DOI] [PubMed] [Google Scholar]
- [19].Matsumoto M, Nojiri K, Chiba K, et al. Open-door laminoplasty for cervical myelopathy resulting from adjacent-segment disease in patients with previous anterior cervical decompression and fusion. Spine (Phila Pa 1976) 2006;31:1332–7. [DOI] [PubMed] [Google Scholar]
- [20].Gause PR, Davis RA, Smith PN, et al. Success of junctional anterior cervical discectomy and fusion. Spine J 2008;8:723–8. [DOI] [PubMed] [Google Scholar]
- [21].Reyes-Sanchez A, Zarate-Kalfopulos B, Rosales-Olivares LM. Adjacent segment disease in a patient with klippel-feil syndrome and radiculopathy: surgical treatment with two-level disc replacement. SAS J 2007;1:131–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Yi S, Kim SH, Shin HC, et al. Cervical arthroplasty in a patient with Klippel–Feil syndrome. Acta Neurochir 2007;149:805–9. discussion 809. [DOI] [PubMed] [Google Scholar]
- [23].Wigfield CC, Gill SS, Nelson RJ, et al. The new Frenchay artificial cervical joint: results from a two-year pilot study. Spine (Phila Pa 1976) 2002;27:2446–52. [DOI] [PubMed] [Google Scholar]
- [24].Sekhon LH, Sears W, Duggal N. Cervical arthroplasty after previous surgery: results of treating 24 discs in 15 patients. J Neurosurg Spine 2005;3:335–41. [DOI] [PubMed] [Google Scholar]
- [25].Barbagallo GM, Assietti R, Corbino L, et al. Early results and review of the literature of a novel hybrid surgical technique combining cervical arthrodesis and disc arthroplasty for treating multilevel degenerative disc disease: opposite or complementary techniques? Eur Spine J 2009;18(suppl 1):29–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Matsumoto M, Okada E, Ichihara D, et al. Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 2010;35:36–43. [DOI] [PubMed] [Google Scholar]
- [27].Liao Z, Fogel GR, Pu T, et al. Biomechanics of hybrid anterior cervical fusion and artificial disc replacement in 3-level constructs: an in vitro investigation. Med Science Monit 2015;21:3348–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Thaler M, Hartmann S, Gstottner M, et al. Footprint mismatch in total cervical disc arthroplasty. Eur Spine J 2013;22:759–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Ryu WHA, Kowalczyk I, Duggal N. Long-term kinematic analysis of cervical spine after single-level implantation of Bryan cervical disc prosthesis. Spine J 2013;13:628–34. [DOI] [PubMed] [Google Scholar]
- [30].Park JH, Rhim SC, Roh SW. Mid-term follow-up of clinical and radiologic outcomes in cervical total disk replacement (Mobi-C): incidence of heterotopic ossification and risk factors. Eur Spine J 2011;20:2282–3. [DOI] [PubMed] [Google Scholar]
- [31].Wu J-C, Huang W-C, Tsai T-Y, et al. Multilevel arthroplasty for cervical spondylosis more heterotopic ossification at 3 years of follow-up. Spine 2012;37:E1251–9. [DOI] [PubMed] [Google Scholar]
- [32].Goffin J, Geusens E, Vantomme N, et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech 2004;17:79–85. [DOI] [PubMed] [Google Scholar]


