Supplemental Digital Content is available in the text
Keywords: aging, neck, shoulder, spondylosis, ultrasound
Abstract
Rotator cuff tendon tears are prevalent in patients with shoulder pain, the third most common musculoskeletal complaint. As shoulders are largely innervated by cervical nerves, it seems possible that rotator cuff pathology could have an association with cervical spine disorders, although few studies have investigated this possibility. This study aimed to explore the association between rotator cuff tendon tears and cervical radiculopathy (at C5 and C6 levels) in the shoulder pain population.
We conducted a retrospective review of a clinical registry of shoulder ultrasound (US) examinations and cervical spine radiographs, recruiting a total of 126 patients with cervical spine radiographs taken within 1 year of US examinations. Foraminal stenosis was grouped into 4 categories: C4/5 intervertebral foramen only, C5/6 intervertebral foramen only, both C4/5 and C5/6 intervertebral foramina, and neither C4/5 nor C5/6 intervertebral foramen. The groups with and without rotator cuff tendon tears were compared for various factors, using the Mann-Whitney U test for continuous variables and the χ2 test for categorical variables. A multivariate analysis was conducted using a logistic regression model to investigate the association between rotator cuff tendon tears and cervical foraminal stenosis.
Patients with rotator cuff tendon tears tended to be older and had more night-time pain. No significant association was identified between rotator cuff tendon tears and cervical foraminal stenosis at C5 and C6 levels. The only factor significantly predicting rotator cuff tendon tears was old age (odds ratio, 1.04; 95% confidence interval: 1.00–1.09).
In patients with shoulder or neck pain, no significant association existed between rotator cuff tendon tears and cervical foraminal stenosis (at the C5 and C6 levels). When patients present with undifferentiated shoulder and neck pain, physicians should take a detailed history, perform physical examinations and imaging studies of both the neck and shoulder regions.
1. Introduction
Shoulder pain is the third most common musculoskeletal complaint (after low back and neck pain), with a prevalence ranging from 6.9% to 26.0% in the general population.[1] The possible causes of shoulder pain are various, and sometimes it is not easily differentiated from other painful conditions of the neck or trunk. Rotator cuff tendon tears are highly prevalent in patients with shoulder pain, often leading to significant disability and decreased quality of life.[2,3] The etiology of rotator cuff tendon tears varies in different age groups. Although acute trauma is more common in young adults, degeneration caused by chronic overuse is prevalent in elderly individuals.[4] Patients with rotator cuff tendon tears may also develop symptoms similar to those of C5 or C6 radiculopathies, that is, pain radiating to the deltoid muscle region and weakness during shoulder abduction. As the shoulders are largely innervated by nerves arising from cervical roots,[5] it seems possible that rotator cuff pathology could have an association with cervical spine disorders, although few studies have investigated this possibility.
Coexistence of shoulder and neck pain is not rare in patients visiting pain clinics. This might be a consequence of the anatomical associations between the 2 regions. There are several muscles directly connecting the shoulder girdle to the cervical spine, for example, the upper trapezius and levator scapulae muscles. A recent systematic review indicated that neck/shoulder pain was related to reduced vascularity and oxygenation at the trapezius muscle while performing upper extremity tasks.[6] Instability of the cervical spine could lead to overuse of these muscles, thereby interfering with normal shoulder kinematics.[7] Another potential link derives from a faulty posture of the spine. A previous study found a higher risk of rotator cuff tendon tears in patients with a kyphotic-lordotic spine than in those with an ideal alignment.[8] Peripheral nerve dysfunction (such as suprascapular or axillary nerve neuropathy) caused by proximal cervical nerve root entrapment (especially at the C5 and C6 root levels) has also been considered a possible cause of painful shoulders.[9–11] In fact, ultrasound (US)-guided intervention for the proximal suprascapular nerve has been shown effective in recalcitrant shoulder pain.[12] Taken together, these observations suggest that clarification of the relationship between shoulder and cervical spine pathologies could be helpful in the diagnosis and treatment of relevant painful syndromes. The present study aimed to explore the association between rotator cuff tendon tears and cervical radiculopathies at the C5 and C6 root levels.
2. Methods
2.1. Study design and participants
This study was a retrospective analysis of patients referred for shoulder US examinations in our musculoskeletal clinics since July 2012. Those who had comprehensive neck radiographs (anteroposterior, lateral, and oblique views) up to 1 year before or after the US assessment were identified. All available US and x-ray images were retrieved for review. Only participants with a complete set of shoulder US scans and cervical radiographs were included. Subjects were excluded if they reported major trauma (e.g., from an automobile accident) to the affected shoulder or rheumatic diseases (e.g., ankylosing spondylitis, rheumatoid arthritis). The study project was approved by the institutional review board of National Taiwan University Hospital (IRB NO. 201709022RINC) and was in compliance with the rules in the Helsinki protocol, and requirement for informed consent was waived because of its retrospective design. The flow diagram of the present study is presented in Figure 1.
Figure 1.
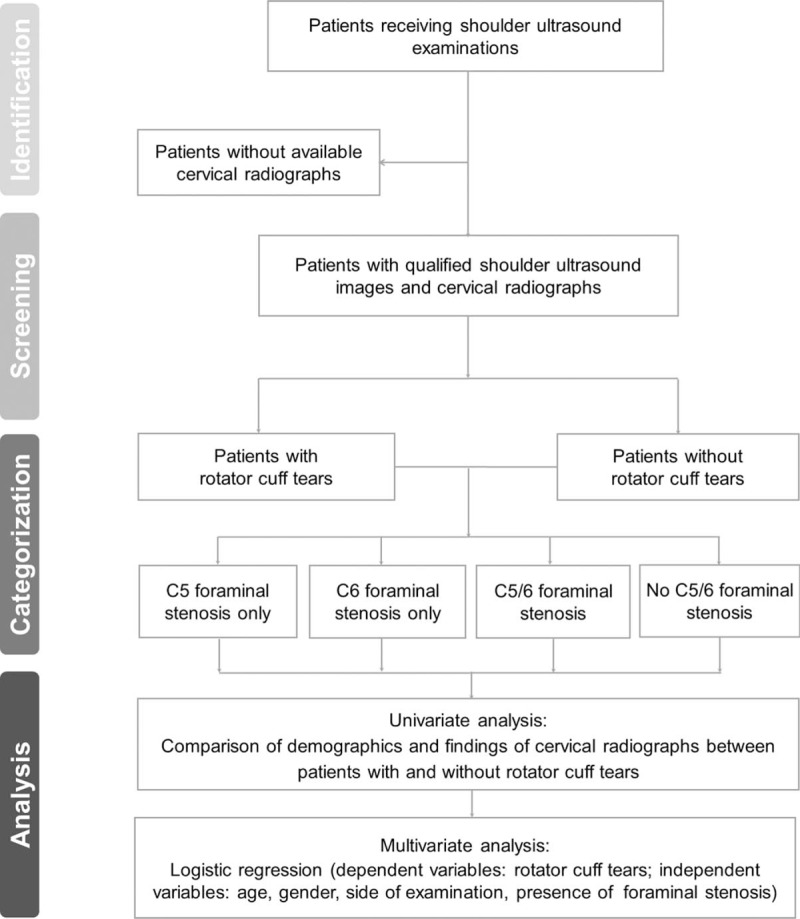
Study flowchart: identification, screening, categorization, and analysis of the association between rotator cuff tendon tears and cervical foraminal stenosis.
2.2. Clinical assessment
Since July 2012, all physicians who referred patients for shoulder US examinations have been required to document the clinical presentations in electronic medical records. The standardized form included shoulder pain duration, visual analogue pain scale scores (at rest, at night, and during overhead activities), and physical examination findings (bicipital groove tenderness; results of the Speed, Yergason, empty can, Neer, and Hawkins-Kennedy painful arc tests; and shoulder range of motion).[13,14]
2.3. Ultrasound imaging
An itemized checklist was used for reporting findings from a sonographic assessment of the shoulder using a linear probe (10–14 MHz, Xario, Toshiba America Medical Systems; 5–18 MHz, HI VISION Ascendus, Hitachi). A standardized scanning protocol was applied, including inspection of the biceps tendon, subscapular tendon, acromioclavicular joint, supraspinatus tendon, infraspinatus tendon, and posterior glenohumeral joint.[2,13,15] Effusion was defined as anechoic compressible fluid beside or inside the tendon or joint. The findings indicative of tendinopathy included decreased echogenicity, increased thickness, and disorganized fiber arrangement. Partial thickness tearing of the rotator cuff tendons was diagnosed based on partial loss of the tendon substance, without connection between the bursal and articular compartments. Full thickness tearing of the rotator cuff tendons was diagnosed if the anechoic discontinuity extended from the bursal side to the articular side, or if complete absence of the tendon was accompanied by a naked humeral head (Fig. 2).[13,16]
Figure 2.
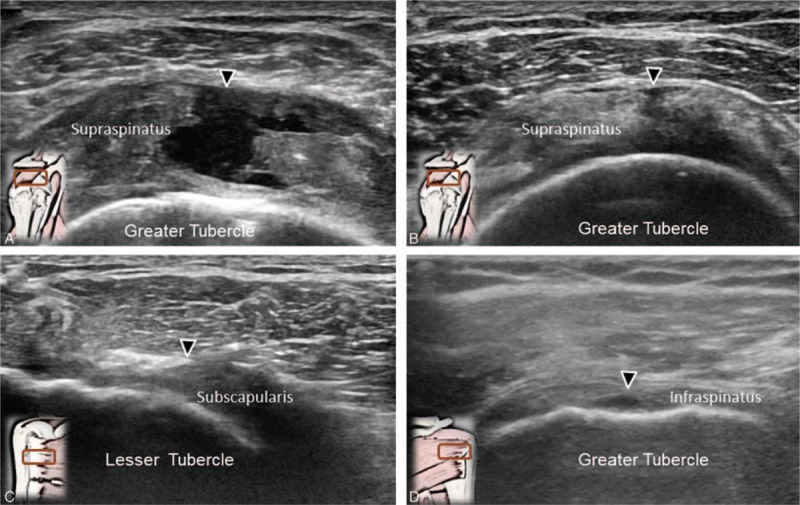
Sonographic imaging of (A) supraspinatus tendon full thickness tear, (B) supraspinatus tendon partial thickness tear, (C) subscapularis tendon tear, and (D) infraspinatus tendon tear. The illustration in the left lower corner represents the position of the transducer. The arrows indicate the sites of tearing.
2.4. Radiographic evaluation
In the present study, each participant was required to have plain radiographs with anteroposterior, lateral, and both oblique views of the cervical spine. For the anteroposterior view, attention was focused on the alignment of the spinous processes and configuration of the facet columns. For the lateral view, disc space narrowing, subchondral sclerosis, and osteophyte formation were examined. Oblique views were evaluated with regard to foraminal stenosis.
Foraminal stenosis of the C5 nerve root indicated stenosis of the C5 intervertebral foramen (between C4 and C5) caused by improper alignment, facet hypertrophy, disc space narrowing, or bony spurs.[17,18] Determination of foraminal stenosis was based mainly on oblique views of cervical radiographs at the site of the affected shoulder (Fig. 3); other views were used for comparison. The same diagnostic standard was applied for determination of foraminal stenosis of the C6 nerve root. All images were reviewed independently by 2 of the authors, and the determination of foraminal pathology was based on consensus of both reviewers, and also on the initial radiologist's report.
Figure 3.
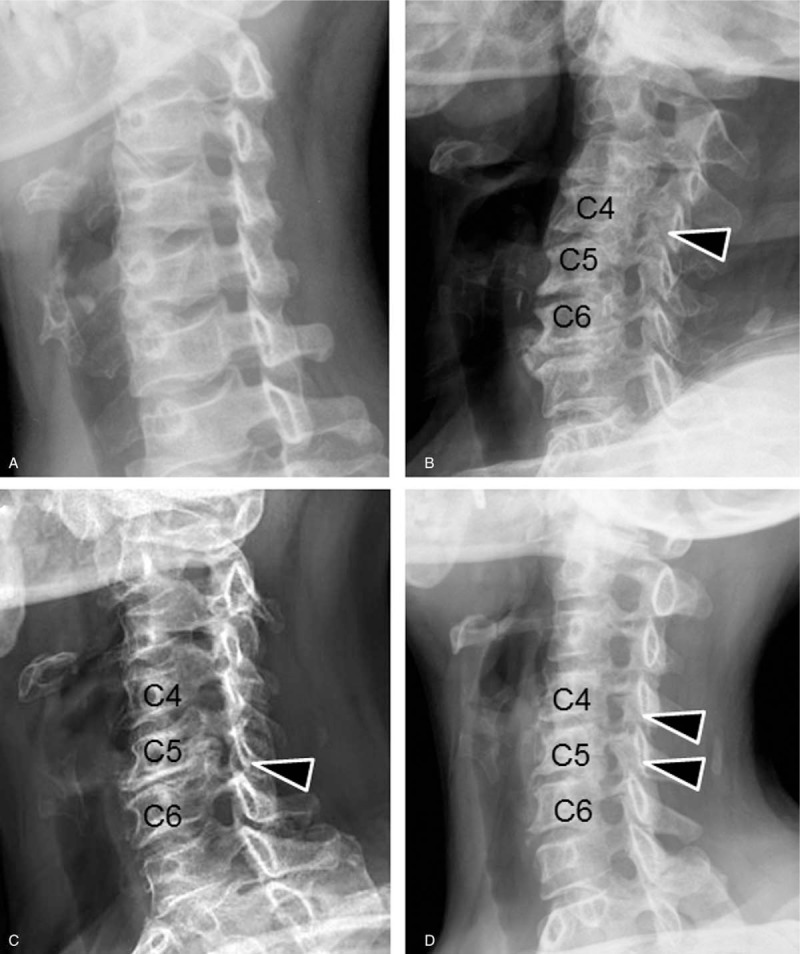
Cervical radiographs (oblique view) with (A) no C4/5 or C5/6 foraminal stenosis, (B) C4/5 foraminal stenosis only, (C) C5/6 foraminal stenosis only, and (D) both C4/5 and C5/6 foraminal stenosis. The arrows indicate the stenotic foramina.
2.4.1. Statistical analysis
The participants were divided into 2 groups, based on the presence or absence of a rotator cuff tendon tear, that is, pathological and control groups. Patients presenting with tears of the subscapularis, supraspinatus, or infraspinatus rotator cuff tendons were included in the pathological group (Fig. 2), whereas those without such tears were treated as controls. Continuous variables (reported as mean ± standard deviation) were compared between the 2 groups using the Mann-Whitney U test, and categorical variables (reported as number, percentage) were compared using the χ2 test.
A multivariate analysis was conducted using a logistic regression model to examine the association between cervical foraminal encroachment and rotator cuff tendon tears. Presence of the latter was treated as the dependent variable, whereas the explanatory variables were age, sex, laterality, and type of foraminal stenosis (divided into 4 categories: C4/5 intervertebral foramen only, C5/6 intervertebral foramen only, both C4/5 and C5/6 intervertebral foramina, neither C4/5 nor C5/6 intervertebral foramen). The data were analyzed using Stata version 11, and a P value <.05 was considered statistically significant.
3. Result
Overall, 136 cases with available cervical radiographs were included from the registry of shoulder US examinations. After 8 cases had been excluded because of lack of ≥1 radiographic views and 2 because of inadequate US image quality, the study finally included 126 participants.
Twenty-five of the patients (19.8%) had rotator cuff tendon tears. Among the group with rotator cuff tendon tears, 12 (48.0%) are with supraspinatus full-thickness tears, 13 (52.0%) with supraspinatus partial thickness tears, 3 (12.0%) with subscapularis tendon tears, and 5 (20%) with infraspinatus tendon tears (the numbers add up to 33 because some patients had tears at >1 tendon).
Among all the participants, 65 (52%) participants had no foraminal stenosis, 21 (16%) had only C4/5, 26 (21%) had only C5/6, and 14 (11%) had both C4/5 and C5/6 foraminal stenoses (Table 1). The Kappa value for agreement between the reviewers in determining foraminal stenosis was 0.88, with a standard error of 0.05.
Table 1.
Baseline characteristics, radiographic findings, sonographic presentations, and clinical symptoms of patients with and without rotator cuff tendon tears.
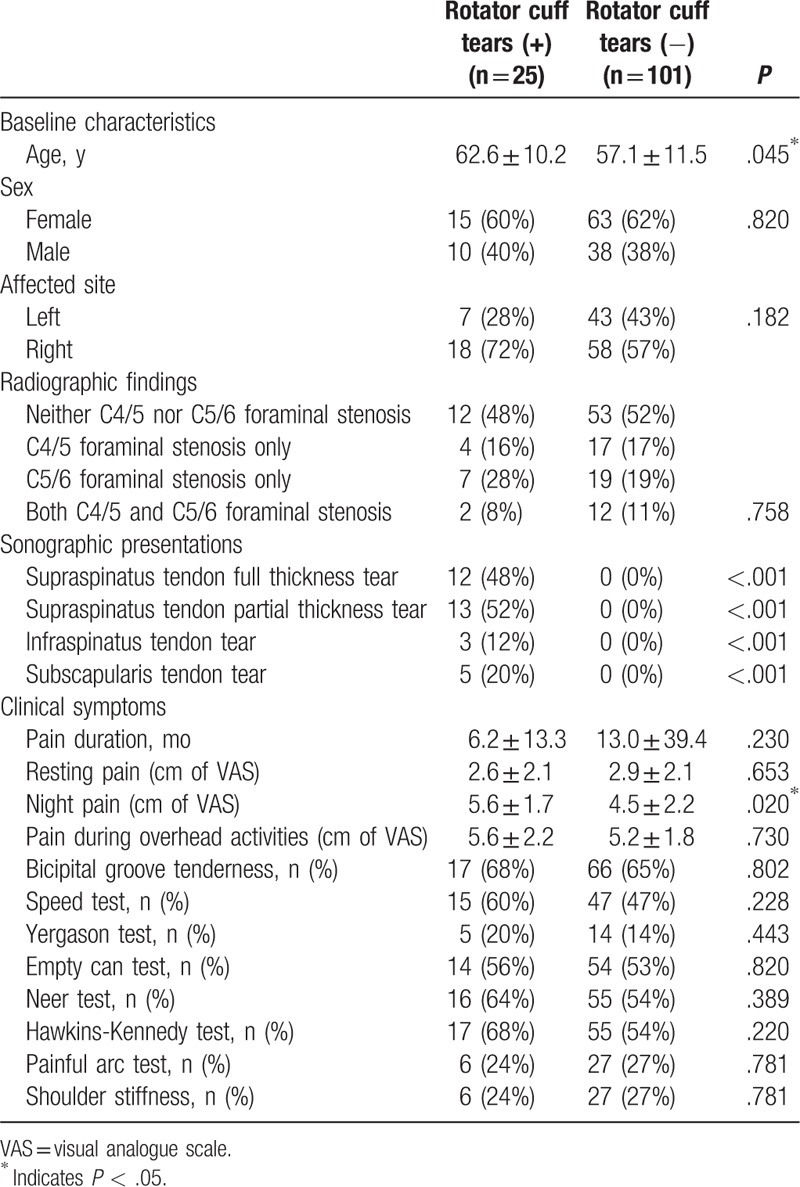
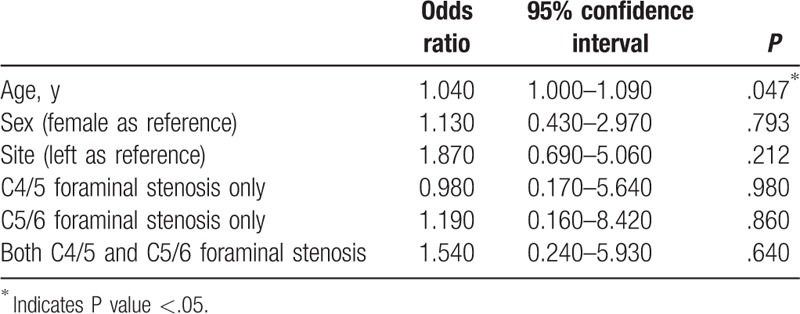
The univariate analyses showed that participants with rotator cuff tendon tears were significantly older than those without such tears (P = .045). There were no significant between-group differences in the distribution of sexes, laterality, and presence of stenosis. In terms of clinical symptoms, no significant differences were observed between the groups, except a higher average level of night-time pain, as measured using the visual analogue scale, in the pathological group (P = .020). Based on the multivariate analysis, the only factor significantly associated with rotator cuff tendon tears was age (odds ratio, 1.04; 95% confidence interval, 1.00–1.09). No significant association was identified between the presence of a rotator cuff tendon tear and cervical foraminal stenosis (Table 2).
Table 2.
Association of rotator cuff tendon tears with cervical foraminal stenosis at the C5 and C6 levels.
4. Discussion
This study was a retrospective analysis of shoulder US and cervical radiographs of patients with shoulder pain. We found that patients with rotator cuff tendon tears tended to be older and had more night-time pain than other patients. No significant association was identified between rotator cuff tendon tears and cervical foraminal stenosis at the C5 and C6 levels. The only factor significantly predicting the presence of rotator cuff tendon tears was old age.
Shoulder and neck pain are common musculoskeletal complaints for which identification of the causes may be challenging.[19] Although a variety of physical signs and tests can help in differentiating the causes of both disorders, they are not specific, and the interpretation of results varies among examiners. In 2010, Hattrup et al performed a comprehensive review investigating rotator cuff tears in patients with cervical radiculopathy.[10] They proposed that the biomechanical connections linking the 2 entities might be mediated by irritation or dysfunction of the suprascapular or axillary nerves, both of which carry fibers from the C5 and C6 nerve roots.[10]
In 2015, Zhang et al[20] conducted a retrospective cohort study by reviewing the diagnoses in medical care records. They found that patients with a diagnosis of rotator cuff pathology were more likely to have a C-spine problem than an L-spine problem. In that study, however, the diagnosis of shoulder or spinal disorders was based on codes from the International Classification of Diseases, Ninth Revision, but without validation by imaging modalities or electrophysiological findings. As shoulder and neck pain are highly prevalent and have a crucial impact on quality of life, we deemed it useful to clarify the relationship between the 2 etiologies by employing more solid diagnostic approaches, that is, US and radiography.
US has proven to be a valuable tool for delineating shoulder pathologies, with sensitivity and specificity comparable to magnetic resonance imaging.[21] In addition to traditional B-mode and Doppler US imaging, the development of elastography further allows the physicians to evaluate elastiticy of tendons and muscles on shoulder girdles.[22–24] A recent US study using shear wave elastography demonstrated tendon softening in rotator cuff disorders.[25] In the present study, we targeted a population with rotator cuff tendon tears, which are common and more easily defined than other shoulder pathologies on the basis of high resolution US imaging. The prevalence of rotator cuff tendon tears in our study was 19.8%, which is similar to that observed (22.6%) in a larger cohort including 907 patients with shoulder pain.[3] In contrast to that study, our participants also had pain resembling cervical radiculopathy, and therefore were also examined using cervical radiography. Our data might reflect that in patients with concomitant shoulder and neck pain, or with pain of an undifferentiated shoulder or cervical origin, the prevalence of rotator cuff tendon tears is not higher than in the general population with shoulder pain.
In contrast to the antecedent studies that targeted nonspecific neck pain,[19,20] our research focused on neural foraminal stenosis at the C5 and C6 levels. This choice was based on the sensory and motor innervations of the shoulder, that is, the suprascapular (70%) and axillary (30%) nerves,[26,27] both of which receive fibers from the C5 and C6 roots. Furthermore, to examine whether a synergistic effect existed regarding entrapment of both nerve roots, we specifically distinguished four groups with respect to the type of C4/5 and C5/6 foraminal stenosis. Despite this distinction, no association was observed between rotator cuff tendon tears and cervical foraminal stenosis. Therefore, based on our findings, we conclude that although foraminal stenosis might cause cervical nerve entrapment, it is unlikely that the shoulder kinematics are affected enough to produce subsequent rotator cuff tendon tears.
In the multivariate analysis, the only factor significantly related to rotator cuff tendon tears was increased age. Age is a known risk factor for rotator cuff tendon tears, and older patients are prone to develop large-sized tears.[28] The pathophysiology includes decreased vascular supply near the insertion of rotator cuff tendons on the greater tubercles, as well as repeated micro-trauma.[28] Likewise, aging causes disc degeneration of the cervical spine, followed by subsequent facet hypertrophy and osteophyte formation owing instability. A previous study indicated that inferior facet hypertrophy significantly decreased the width of the cervical intervertebral foramina in older adults, causing symptoms of nerve entrapment.[29] Therefore, based on our analysis, we can say that rather than a likely association between rotator cuff tendon tears and cervical spine problems, increased age might be playing a much more important role in this concomitance of both disorders. Furthermore, older adults account for the majority of patients visiting pain clinics, and the aging process appears to contribute strongly to both shoulder and cervical degenerative pathologies.
In the present study, we also observed that patients with rotator cuff tendon tears reported higher levels of pain at night than those without. Rotator cuff tendon tears do not always lead to pain and may actually be asymptomatic if the rupture size is small.[30] As all of our patients were referrals for an ultrasound examination due to various shoulder symptoms, it could be concluded that small tears were not prevalent in our population. As night-time pain is indicative of a chronic inflammatory process with an increase in blood flow,[31] we speculated that large-sized tears caused persistent inflammation and thus more pain at night in our group.
Our study had several limitations. First, the diagnosis of cervical radiculopathy at the C5 and C6 levels was based on radiography, which is less sensitive than magnetic resonance imaging. However, considering the cost and insurance coverage, patients undergoing cervical x-ray imaging significantly outnumbered those receiving magnetic resonance imaging (which also yielded greater statistical power for a retrospective analysis). Additionally, to increase the diagnostic sensitivity, we enrolled patients only if they had cervical radiographs for four view planes. Second, all the cervical radiographs were not taken on the same dates as the shoulder ultrasound scans. However, the longest interval permitted between the 2 imaging sessions was 1 year. As cervical foraminal stenosis is mostly derived from degeneration and develops during a duration of many years, this timing allowance remained in accordance with a cross-sectional design. Third, the study did not include healthy controls because the data were extracted from a medical registry of shoulder patients. Although we speculate that the prevalence of shoulder and cervical pathologies might be lower in asymptomatic participants, a prospective study using a control group would be needed to show this definitively.
5. Conclusion
In patients with shoulder and neck pain, no association existed between rotator cuff tendon tears and cervical foraminal stenosis at the C5 and C6 levels. Aging seemed to be the main contributor to this coexistence of both disorders. When patients present with undifferentiated shoulder and neck pain, physicians should obtain a detailed history and perform physical examination and imaging studies for both the neck and shoulder regions.
Author contributions
All authors have read and approved the final manuscript. K-VC conceived and designed the study, recruited the study subjects, and planned and performed the statistical analysis. W-TW and LO made critical revisions to the manuscript. D-SH conceived and designed the study. K-VC performed the analysis and interpretation of the data, and wrote the draft; recruited the study subjects, and performed the analysis and interpretation of the data; responsible for acquisition, analysis and interpretation of the data. D-SH and C-PL contributed to study supervision and critical revision of the manuscript. LO contributed to study supervision.
Conceptualization: Wei-Ting Wu, Chih-Peng Lin.
Data curation: Ke-Vin Chang.
Formal analysis: Ke-Vin Chang.
Investigation: Wei-Ting Wu, Ke-Vin Chang, Chih-Peng Lin.
Methodology: Ke-Vin Chang.
Resources: Levent Özçakar.
Supervision: Der-Sheng Han, Chih-Peng Lin.
Validation: Levent Özçakar.
Writing – original draft: Wei-Ting Wu, Ke-Vin Chang.
Writing – review & editing: Wei-Ting Wu, Ke-Vin Chang, Der-Sheng Han, Chih-Peng Lin, Levent Özçakar.
Supplementary Material
Footnotes
Abbreviations: US = ultrasound, VAS = visual analogue scale.
Supplementary data
Ethics approval and consent to participate
The research was approved by the institutional review board of National Taiwan University Hospital (IRB NO. 201709022RINC).The need for informed consent was waived due to the retrospective nature of the research. The data were processed and analyzed anonymously.
The authors report no conflicts of interests.
Funding: The present study is supported by National Taiwan University Hospital, Bei-Hu Branch, Ministry of Science and Technology (MOST 106–2314-B-002 -078 -MY2 and 106–2314-B-002–180-MY3), and Taiwan Society of Ultrasound in Medicine.
Availability of data and materials: The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request: contact Dr. Ke-Vin Chang (kvchang011@gmail.com).
Supplemental Digital Content is available for this article.
References
- [1].Luime JJ, Koes BW, Hendriksen IJ, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol 2004;33:73–81. [DOI] [PubMed] [Google Scholar]
- [2].Hung CY, Chang KV, Ozcakar L, et al. Can quantification of biceps peritendinous effusion predict rotator cuff pathologies?: A retrospective analysis of 1352 shoulder ultrasound. Am J Phys Med Rehabil 2016;95:161–8. [DOI] [PubMed] [Google Scholar]
- [3].Chang KV, Chen WS, Wang TG, et al. Associations of sonographic abnormalities of the shoulder with various grades of biceps peritendinous effusion (BPE). Ultrasound Med Biol 2014;40:313–21. [DOI] [PubMed] [Google Scholar]
- [4].Lazarides AL, Alentorn-Geli E, Choi JH, et al. Rotator cuff tears in young patients: a different disease than rotator cuff tears in elderly patients. J Shoulder Elbow Surg 2015;24:1834–43. [DOI] [PubMed] [Google Scholar]
- [5].Chang KV, Lin CP, Hung CY, et al. Sonographic nerve tracking in the cervical region: a pictorial essay and video demonstration. Am J Phys Med Rehabil 2016;95:862–70. [DOI] [PubMed] [Google Scholar]
- [6].Gold JE, Hallman DM, Hellström F, et al. Systematic review of quantitative imaging biomarkers for neck and shoulder musculoskeletal disorders. BMC Musculoskelet Disord 2017;18:395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Falla D, Cescon C, Lindstroem R, et al. Muscle pain induces a shift of the spatial distribution of upper trapezius muscle activity during a repetitive task: a mechanism for perpetuation of pain with repetitive activity? The Clin J Pain 2017;33:1006–13. [DOI] [PubMed] [Google Scholar]
- [8].Yamamoto A, Takagishi K, Kobayashi T, et al. The impact of faulty posture on rotator cuff tears with and without symptoms. J Shoulder Elbow Surg 2015;24:446–52. [DOI] [PubMed] [Google Scholar]
- [9].Caridi JM, Pumberger M, Hughes AP. Cervical radiculopathy: a review. HSS J 2011;7:265–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Hattrup SJ, Cofield RH. Rotator cuff tears with cervical radiculopathy. J Shoulder Elbow Surg 2010;19:937–43. [DOI] [PubMed] [Google Scholar]
- [11].Bachasson D, Singh A, Shah SB, et al. The role of the peripheral and central nervous systems in rotator cuff disease. J Shoulder Elbow Surg 2015;24:1322–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chang KV, Hung CY, Wang TG, et al. Ultrasound-guided proximal suprascapular nerve block with radiofrequency lesioning for patients with malignancy-associated recalcitrant shoulder pain. J Ultrasound Med 2015;34:2099–105. [DOI] [PubMed] [Google Scholar]
- [13].Chang SF, Lin PL. Systematic literature review and meta-analysis of the association of sarcopenia with mortality. Worldviews Evid Based Nurs 2016;13:153–62. [DOI] [PubMed] [Google Scholar]
- [14].Chang KV, Wu WT, Han DS, et al. Static and dynamic shoulder imaging to predict initial effectiveness and recurrence after ultrasound-guided subacromial corticosteroid injections. Arch Phys Med Rehabil 2017;98:1984–94. [DOI] [PubMed] [Google Scholar]
- [15].Ozcakar L, Kara M, Chang KV, et al. EURO-MUSCULUS/USPRM Basic Scanning Protocols for shoulder. Eur J Phys Rehabil Med 2015;51:491–6. [PubMed] [Google Scholar]
- [16].Chang KV, Chen WS, Wang TG, et al. Quantitative ultrasound facilitates the exploration of morphological association of the long head biceps tendon with supraspinatus tendon full thickness tear. PLoS One 2014;9:e113803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Sato T, Masui K. Morphologic differences in intervertebral foramina: a radiographic study of cervical spine positions in asymptomatic men. J Manipulative Physiol Ther 2013;36:327–32. [DOI] [PubMed] [Google Scholar]
- [18].Green C, Butler J, Eustace S, et al. Imaging modalities for cervical spondylotic stenosis and myelopathy. Adv Orthop 2012;2012:908324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Tsunoda D, Iizuka Y, Iizuka H, et al. Associations between neck and shoulder pain (called katakori in Japanese) and sagittal spinal alignment parameters among the general population. J Orthop Sci 2013;18:216–9. [DOI] [PubMed] [Google Scholar]
- [20].Zhang AL, Theologis AA, Tay B, et al. The association between cervical spine pathology and rotator cuff dysfunction. J Spinal Disord Tech 2015;28:E206–11. [DOI] [PubMed] [Google Scholar]
- [21].Roy JS, Braen C, Leblond J, et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med 2015;49:1316–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Guo M, Lu M, Zhang H, et ak. A rod-like acoustic radiation force in ultrasound-based elastography: a simulation study. In: The International Conference on Health Informatics: 2014: Springer; 2014: 148–151. [Google Scholar]
- [23].Hu Z, Zhang H, Yuan J, et al. An H∞ strategy for strain estimation in ultrasound elastography using biomechanical modeling constraint. PLoS One 2013;8:e73093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Lu M, Zhang H, Wang J, et al. Reconstruction of elasticity: a stochastic model-based approach in ultrasound elastography. Biomed Eng Online 2013;12:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hou SW, Merkle AN, Babb JS, et al. Shear wave ultrasound elastographic evaluation of the rotator cuff tendon. J Ultrasound Med 2017;36:95–106. [DOI] [PubMed] [Google Scholar]
- [26].Chang KV, Hung CY, Wu WT, et al. Comparison of the effectiveness of suprascapular nerve block with physical therapy, placebo, and intra-articular injection in management of chronic shoulder pain: a meta-analysis of randomized controlled trials. Arch Phys Med Rehabil 2016;97:1366–80. [DOI] [PubMed] [Google Scholar]
- [27].Nam YS, Jeong JJ, Han SH, et al. An anatomic and clinical study of the suprascapular and axillary nerve blocks for shoulder arthroscopy. J Shoulder Elbow Surg 2011;20:1061–8. [DOI] [PubMed] [Google Scholar]
- [28].Sambandam SN, Khanna V, Gul A, et al. Rotator cuff tears: an evidence based approach. World J Orthop 2015;6:902–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Humphreys SC, Hodges SD, Patwardhan A, et al. The natural history of the cervical foramen in symptomatic and asymptomatic individuals aged 20-60 years as measured by magnetic resonance imaging. A descriptive approach. Spine 1998;23:2180–4. [DOI] [PubMed] [Google Scholar]
- [30].Yamamoto A, Takagishi K, Kobayashi T, et al. Factors involved in the presence of symptoms associated with rotator cuff tears: a comparison of asymptomatic and symptomatic rotator cuff tears in the general population. J Shoulder Elbow Surg 2011;20:1133–7. [DOI] [PubMed] [Google Scholar]
- [31].Terabayashi N, Watanabe T, Matsumoto K, et al. Increased blood flow in the anterior humeral circumflex artery correlates with night pain in patients with rotator cuff tear. J Orthop Sci 2014;19:744–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


