Abstract
Background:
There is no consensus regarding the therapeutic effect of nasointestinal tubes (NITs) versus nasogastric tubes (NGTs) in the management of small-bowel obstruction (SBO). This study aimed to compare the clinical outcomes between the use of NITs and NGTs in the management of SBO.
Methods:
Published studies on comparing NITs with NGTs in the treatment of SBO were searched from electronic databases. Two investigators independently extracted the data; any discrepancies were adjudicated by a third investigator. Pooled odds ratio (OR) and 95% confidence interval (CI) were calculated using Review Manager 5.0.
Results:
An extensive literature search identified 268 relevant publications, 4 of which met the inclusion criteria. There were no significant differences in the nonrequirement of operative intervention between NITs and NGTs groups (OR: 1.79; 95% CI: 0.55, 5.84). Compared with the NGTs, the NITs, which successfully passed through the pylorus, did not decrease the rate of operation in patients with SBO (OR: 2.19; 95% CI: 0.59, 8.15). There was no advantage of NITs over NGTs in patients with partial SBO (P-SBO) (OR: 1.04; 95% CI: 0.23, 4.60). Postoperative complications were compared between the groups (OR: 2.13; 95% CI: 1.09, 4.15).
Conclusion:
The result of this meta-analysis showed no advantage of NITs over NGTs in the management of patients with SBO.
Keywords: decompression, intestinal obstruction, meta-analysis, small bowel
1. Introduction
Although our understanding of the pathophysiology of small-bowel obstruction (SBO) has markedly improved in recent years, this condition remains a major cause of morbidity and mortality in surgical practice.[1] Bowel obstruction is responsible for about 20% of surgical admissions for acute abdomen, and, postoperative SBO accounts for 78% of these admissions.[2,3] Moreover, the mortality rates of SBO in recent clinical reports range from 0 to 12%.[4,5] Many recent studies have claimed that early operative intervention should be performed as soon as lost fluids have been replaced, because there are no reliable clinical criteria for distinguishing strangulated obstruction of the bowel simple, uncomplicated obstruction.[2,6] However, Stewardson advocated that conservative management in patients who have none of the “classic” findings (e.g., progression to necrotic leukocytosis, fever, tachycardia, or localized tenderness) was reasonable, owing to the absence of tendency to increase mortality rate and complications.[7] Surgery could be the second-stage of treatment of treatment if conservative management fails to resolve SBO. Conservative management consists of bowel decompression, colonic irrigation, and replacement of fluids and electrolytes. Tube decompression has been proven to be successful in managing several cases of SBO, and it can be accomplished by intubation with nasointestinal tubes (NITs) or nasogastric tubes (NGTs).[4,8] There is no consensus regarding the therapeutic effect of NITs versus NGTs in the management of SBO. Moreover, previously published reports in this regard have yielded conflicting results. The present study aimed to resolve this issue by performing a meta-analysis comparing the therapeutic effect of NITs and NGTs decompression in the management of SBO.
2. Materials and methods
2.1. Literature search
A systematic search was performed in PubMed (1950 to April 2017), Embase (1974 to April 2017), Cochrane Controlled Trials Register (Issue 1, 2017), Science Citation Index (1945 to April 2017), and Chinese Biomedical Database (1981 to April 2017) for articles comparing NITs with NGTs in the management of SBO. We employed both Medical Subject Headings and free-language terms to search the database. The search terms included: “intestinal obstruction” or “ileus” AND “nasogastric tube,” “nasogastric drainage,” or “short tube” combined with one of the following: “ileus tube,” “small bowel decompression tube,” “long tube” and “nasointestinal tubes”. Searches were restricted to human subjects and studies published in English. All titles and abstracts were reviewed by 2 authors. A comprehensive search of the reference lists of relevant articles was conducted to identify additional articles. Further, abstracts from major gastroenterological meetings such as the Digestive Disease Week of the American Gastroenterological Association and the Cochrane Central Register of Controlled Trials were also searched for relevant articles. When necessary, authors were contacted for additional information, including those of unpublished studies.
2.2. Inclusion and exclusion criteria
The selection criteria were randomized-controlled trials (RCTs) and case–control studies that compared the effect of NITs and NGTs decompression in the management of SBO. Studies in abstract form or meeting reports, without publication of the full paper, were also included in this meta-analysis if the data could be extracted. Studies reported in languages other than English were excluded unless a translation was available.
All of the studies had diagnostic criteria to define SBO. Patients with a clinical and radiologic diagnosis of SBO, and those whose diagnosis was proved at operation or autopsy were eligible for inclusion in the study. The baseline characteristics of the parents included in our meta-analysis were similar in the 2 groups. Studies on treatment of large bowel obstruction, and those with incomplete data, limited outcomes or multiple publications were excluded.
2.3. Data extraction and quality assessment
Standardized data abstraction sheets were prepared. Data were extracted for author name and year, location of trials, trial design, number of patients in the 2 groups, and the quality assessment of the included studies. Two reviewers (Dong and Huang) independently examined all the studies. Disagreements were resolved by consulting the third reviewer (Zhang). When the results from some or all patients in a clinical trial were published multiple times, only the most complete and updated data were extracted in this meta-analysis. Finally, the manuscripts were studied for their comparability by Dong and Jiang.
The internal validity of the studies based on study design, characteristics of the enrolled patients, losses to follow-up, and funding source were examined independently by 2 eligible reviewers (XD and YS). Any discrepancies between the 2 reviewers were recorded and resolved by consulting a third reviewer (XZ). The quality of the included RCTs was assessed using the modified Jadad scale (MJS).[9] As only 2 RCTs were included in this meta-analysis, the quality assessment of the non-randomized controlled trials (non-RCTs) was based on the list of 12 items proposed by the Methodological Index for Non-Randomized Studies (MINORS).[10]
2.4. Risk of bias
Funnel plot asymmetry was used to measure any publication bias in this meta-analysis. In addition, we evaluated publication bias using Egger's regression test.
2.5. Statistical analysis
Data were extracted by both reviewers and entered into the Cochrane Collaboration Review Manager (RevMan) 5.0 (Copenhagen, 2008). Odds ratio (OR) with 95% confidence interval (CI) was calculated for NITs versus NGTs in the management of patients with SBO. OR <1.0 favored the control group. Moreover, if P < .05 and 95%CI did not include the value 1, the differences were considered to be statistically significant. Heterogeneity among the studies was assessed using the standard I2 statistic. I2 values above 50% indicated significant heterogeneity, those between 25% and 50% indicated moderate heterogeneity, and those below 25% indicated low heterogeneity. If significant heterogeneity existed, it would be inappropriate to combine data for further analysis using a random effects model; hence, the fixed effects model was used. Subgroup analyses were performed according to the type of RCTs or non-RCTs on the respective outcome.
3. Results
3.1. Study selection
A total of 268 relevant publications were identified from the literature search, among which 51 publications were ineligible owing to the publication type; 13 of these were reviews, 34 were case reports, 1 was a guideline, and 3 were comments or letters. Another 204 papers were excluded after examining the titles and abstracts; 189 papers were unrelated, 1 was a technique in surgery, 1 paper was published in multiple journals, and 13 papers did not apply to the study question. On the basis of previously described criteria, 13 potentially appropriate studies were included, and their abstracts and full texts were retrieved for further assessment. Of these potential eligible publications, we excluded another 9 publications, as they did not have a proper control group, and a proper OR could not be calculated. Finally, 4 manuscripts were included in this review.[4,11–13] Two of them were RCTs and 2 were case–control studies. One study was conducted in China while 3 were conducted in United States. All 4 studies were published between 1981 and 2012. Figure 1 shows a flowchart for the selection process of the meta-analysis. The characteristics of the 4 articles included in the meta-analysis are summarized in Table 1, while the outcomes of the meta-analysis are shown in Figure 2.
Figure 1.
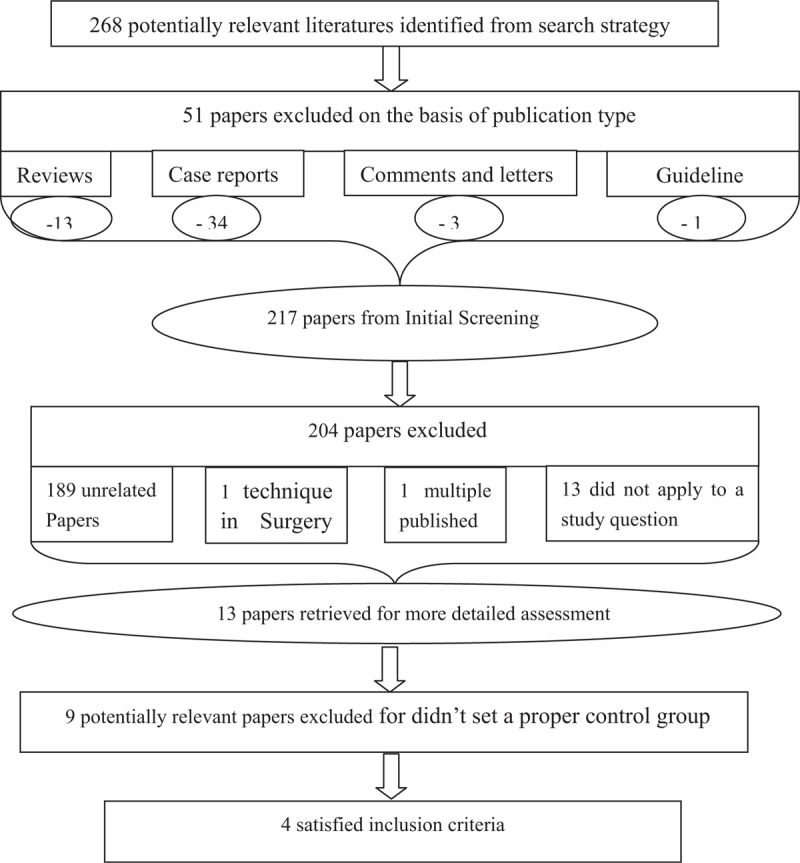
Flowchart of study selection for meta-analysis.
Table 1.
Characteristics of included studies.

Figure 2.
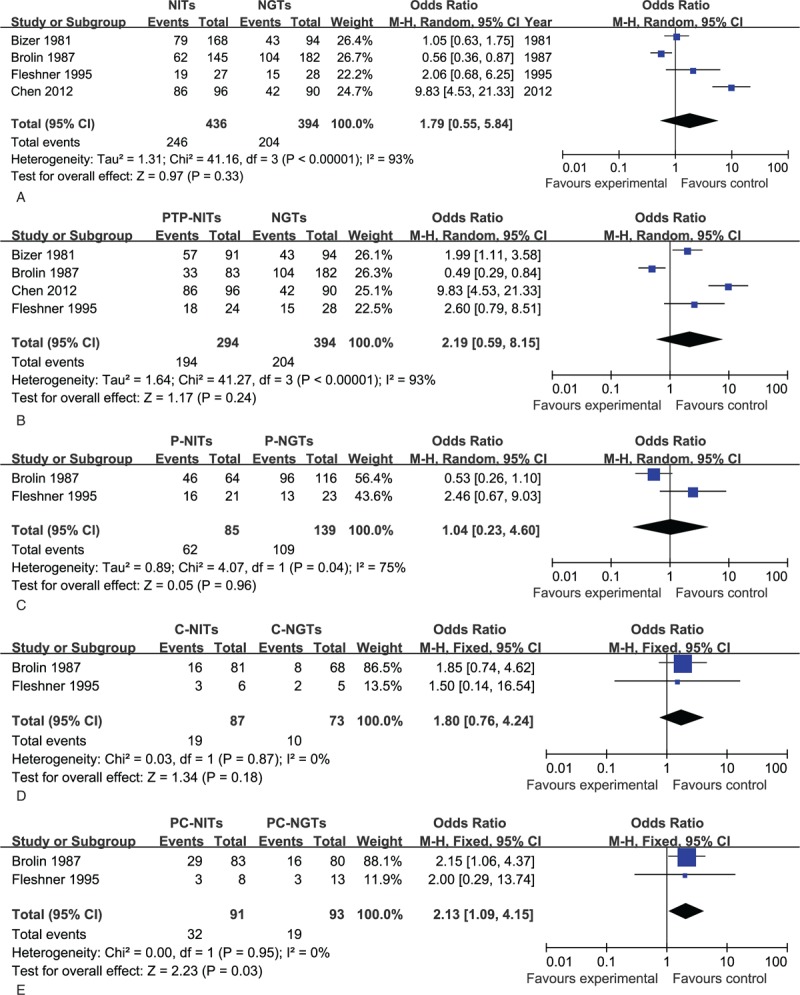
Forest plot of meta-analysis (A) Nasointestinal tubes (NITs) versus nasogastric tubes (NGTs) in the management of small-bowel obstruction (SBO). Total: number of patients with SBO treated with NITs or NGTs, Events: number of patients with SBO required nonoperative intervention; (B) NITs, which successfully passed through the pylorus (PTP-NITs), versus NGTs in the management of SBO; (C) NITs versus NGTs in the management of partial SBO; (D) NITs versus NGTs in the management of complete SBO; (E) Postoperative complications between NITs and NGTs in the management of SBO. NGT = nasogastric tubes, NIT = nasointestinal tubes, P = partial, PC = postoperative complications, PTP = passed through the pylorus, RCT = randomized controlled trials, SBO = small-bowel obstruction.
3.2. NITs versus NGTs in the management of SBO
Four studies investigated the role of NITs versus NGTs in the management of SBO (Fig. 2A).[4,11–13] A total of 830 patients with SBO were included, of which 436 were treated with NITs and 394 were assigned to NGTs decompression. The effectiveness of NITs and NGTs in the treatment of SOB was 56.4% and 51.8%, respectively. Using random effects model, we did not find any significant differences in the nonrequirement of operative intervention between NITs and NGTs groups. The pooled OR estimated from these studies was 1.79 (95%CI: 0.55, 5.84). Significant differences were found between NITs and NGTs in the treatment of SBO in 2 studies;[12,13] however, no significant differences were found in the remaining 2 studies.[4,11] One of the RCTs indicated inherent superiority of NITs over NGTs in the treatment of SBO; however, the conclusion was inconsistent with that of the other RCTs. One of the case–control studies believed that NITs was associated with a significantly greater length of hospital stay, longer duration of postoperative bowel obstruction and higher risk of postoperative complications. Conversely, the other case–control study found no advantage of one type of tube over the other in the treatment of patients with SBO.
3.3. NITs, which successfully passed through the pylorus (PTP-NITs), versus NGTs in the management of SBO
A total of 294 patients managed with NITs, which successfully passed through the pylorus were included in the meta-analysis (Fig. 2B). Meanwhile, 394 patients were treated with NGTs decompression.[4,11–13] The results of this meta-analysis showed that there was no significant difference between PTP-NITs and NGTs with respect to the nonrequirement of operative intervention (OR: 2.19; 95%CI: 0.59, 8.15).
3.4. NITs versus NGTs in the management of partial SBO (P-SBO)
Two studies had information on NITs versus NGTs in the management of P-SBO; 53 out of the 224 patients with P-SBO required operation,[4,12] namely 23 out of 85 (27.1%) patients treated with NITs and 30 out of 139 (21.6%) treated with NGTs (Fig. 2C). The included studies indicated that there was no scientific evidence for greater effectiveness of NITs than that of NGTs in the treatment of P-SBO. There was no statistically significant difference in the rate of nonoperation between the groups (OR: 1.04; 95%CI: 0.23, 4.60).
3.5. NITs versus NGTs in the management of complete SBO (C-SBO)
Two selected studies had information on NITs versus NGTs in the management of C-SBO;[4,12] 29 out of 160 patients (18.1%) with C-SBO were successfully treated with tube decompression, including 19 patients treated with NITs and 10 patients treated with NGTs (Fig. 2D). There was no significant difference between NITs and NGTs in the treatment of C-SBO. The pooled OR for patients with C-SBO successfully treated with NITs compared with NGTs was 1.80 (95%CI: 0.76, 4.24).
3.6. Postoperative complications
Two studies described the postoperative complications between NITs and NGTs in the management of SBO; a total of 51 patients (27.7%; 31 from the NITs group and 19 from the NGTs group) experienced postoperative complications (Fig. 2E).[4,12] Fleshner et al[4] reported no deaths in the 2 groups in their study. Conversely, Brolin et al[12] reported that 9 of the 163 patients in their study died after operation. The OR for the postoperative complications between the 2 groups was 2.13 (95%CI: 1.09, 4.15).
3.7. Publication bias
Figure 3 shows a funnel plot of the 4 studies included in this meta-analysis that evaluated the relationship between NITs and NGTs in the treatment of SBO. The funnel plot was slightly asymmetrical in distribution; however, Egger's regression test indicated no significant publication bias in this meta-analysis (P = 0.43).
Figure 3.
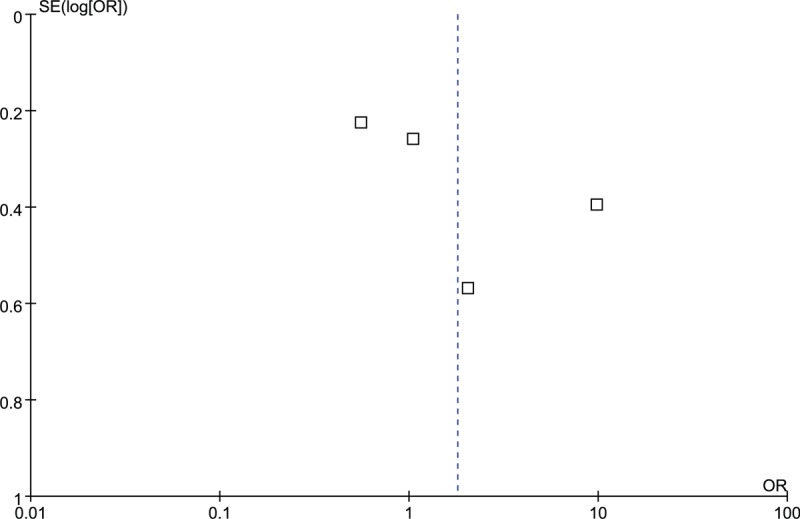
Funnel plots of studies included in this meta-analysis.
4. Discussion
Bowel obstruction was first described centuries ago, in Hippocratic writings. Although the current state of knowledge about diagnostic techniques and advanced treatment technology has dramatically reduced the mortality associated with bowel obstruction, there is considerable controversy regarding the management of patients with SBO. Many surgeons believed that patients with SBO undergoing operative intervention had a lower frequency of recurrence and a longer time interval to recurrence.[2,14] As the accurate identification of patients with SBO who could avoid operation with tube decompression is difficult, increasing number of clinicians recommend an initial trial of tube decompression in the absence of clinical evidence of strangulation, especially with NITs.[11,15] The role of tube decompression in SBO has been evaluated in several studies, with varying outcomes. However, no reliable conclusions have been drawn on whether NIT decompression is superior to NGT decompression in the treatment of patients with SBO.
There is little information in the literature regarding NITs versus NGTs in the management of SBO. Early attempts to use NITs in the treatment of SBO were made in 1933 by Wangensteen and Paine.[16] In 1938, Abbott and Johnston[17] reported a nonoperative technique of advancing the Miller–Abbott tube passing through the pylorus to the point of obstruction, which showed an 80% success rate. In 1976, Johnson et al[18] believed that the technique of intubation under direct endoscopic vision was not only rapid but also easy, and should be widely accepted. Theoretically, the NITs have several advantages over the NGTs in the treatment of SBO. With bowel peristalsis and the weighted tip, the NITs can spontaneously remove the kinks in the obstructed small-bowel loops as it passes distally through the bowel.[19,20] It is also effective in suctioning retained gastric and intestinal fluid close to the point of obstruction.[21] This could reduce the intraluminal pressure between the tube and the point of obstruction, reducing the ischemic necrosis of the bowel. However, a major issue with NITs was delay of passage from the stomach into the small bowel, which also increased the risk of complication. In the present study, no significant difference in the therapeutic effect of NITs versus NGTs was observed. This is consistent with the results of the study by Fleshner et al but not with those of the study by Chen et al.[4,13] We also found a correlation between unsuccessful passage of the NITs through the pylorus and the requirement for operative intervention. Chen et al[13] stated that the successful passage of the NITs through the pylorus was of “significant predictive value” with respect to avoidance of operation. They attributed this difference to the advanced quality of the tube and the technique of endoscopic placement. However, we found no advantage of PTP-NITs over NGTs in the treatment of patients with SBO.
Generally, P-SBO was more likely to respond to NITs decompression, while patients with C-SBO required an operative intervention. Over four-fifths of the patients with C-SBO required operative intervention, whereas four-fifths of the patients with P-SBO required tube decompression. Brolin et al[12] recommended that operative intervention to stabilize the C-SBO should not be delayed, whereas patients with P-SBO who showed no clinical signs of strangulation were more likely to respond to tube decompression. Wolfson et al[22] showed that 64% of patients with C-SBO and only 17% of patients with P-SBO required operative intervention. They stated that most patients with features of C-SBO would ultimately require an operation, whereas patients with P-SBO were associated with a greater likelihood of success with NITs decompression. The efficacy of NITs decompression in the treatment of SBO has recently been described by Gowen,[15] as it has significant clinical and economic advantages over the NGT approach. Gowen even claimed that patients who fail to undergo decompression with NGTs are candidates for NITs decompression. Conversely, we found no difference in the efficacy of NITs versus NGTs in the management of P-SBO. The results of this meta-analysis also showed no superiority of NITs versus NGTs in the treatment of patients with C-SBO.
Although the complications of NITs decompression are relatively rare, they have been well described.[23,24] Some of them are: gastrointestinal obstruction, gastrointestinal ulceration and hemorrhage, gastrointestinal perforation, sinusitis and otitis media, and knotting of the NITs. Fleshner et al[4] and Chen et al[13] reported that all of their patients who underwent placement of NITs were discharged without complications. Snyder et al.[25] reported a 4% overall incidence of complications associated with the use of NITs. Several studies have indicated that none of the patients with SBO died owing to delay in operative intervention.[15,25] In an article by Fleshner et al,[4] there was no statistically significant difference in the incidence of postoperative complications and operative mortality between the use of NITs and NGTs in the treatment of SBO. Conversely, in the present study, evidence demonstrated the superiority of NGTs over NITs with regard to the incidence of postoperative complications. Brolin et al[12] reported that compared to NGTs decompression, NITs decompression had a greater tendency to prolong medical treatment and delay operation. Consequently, there was a higher incidence of postoperative complications and mortality associated with NITs.
This study has some limitations that may have affected its results. First, potential publication bias might exist, as three-fourths of the included studies were conducted in American individuals. Second, most of the studies were case–control studies, with poor methodological quality. Third, only a few articles with a small number of patients with SBO were included. There was significant heterogeneity between the studies, and the random effect models was used for calculating OR. Further, the results of the meta-analysis were also presented in a descriptively manner. Further large-scale RCTs in this regard are warranted.
5. Conclusions
In summary, although some clinicians prefer NITs over NGTs, there are no data demonstrating that NITs are superior to NGTs in the treatment of SBO. Therefore, routine NITs decompression in patients with SBO after admission is still debatable. Further large-scale RCTs of NITs versus NGTs for the treatment of patients with SBO are warranted.
5.1. Ethical review
Ethical approval was not necessary, because this article is a meta-analysis and it does not involve the participation of ethics committee.
Acknowledgments
We would like to thank Dr Ying Zhou and Dr Qiubo Zhang for their editorial assistance.
Author contributions
Conceptualization: Xianwen Dong, Shiliang Huang, Xuesong Zhang.
Data curation: Xianwen Dong, Shiliang Huang, Zhouhua Jiang, Yufei Song.
Formal analysis: Xianwen Dong, Shiliang Huang, Zhouhua Jiang, Yufei Song, Xuesong Zhang.
Investigation: Xianwen Dong, Shiliang Huang.
Methodology: Xianwen Dong, Shiliang Huang, zhouhua Jiang, Yufei Song.
Project administration: Xuesong Zhang.
Software: Xianwen Dong.
Supervision: Xuesong Zhang.
Writing – original draft: Xianwen Dong, Shiliang Huang.
Writing – review & editing: Xuesong Zhang.
Footnotes
Abbreviations: C = complete, CI = confidence interval, MINORS = Methodological Index for Non-Randomized Studies, MJS = modified Jadad scale, NGT = nasogastric tubes, NIT = nasointestinal tubes, OR = odds ratio, P = partial, PC = postoperative complications, PTP = passed through the pylorus, RCT = randomized controlled trial, SBO = small-bowel obstruction.
The authors have no conflicts of interest to disclose.
References
- [1].Dijkstra FR, Nieuwenhuijzen M, Reijnen MM, et al. Recent clinical developments in pathophysiology, epidemiology, diagnosis and treatment of intra-abdominal adhesions. Scand J Gastroenterol 2000;232:52–9. [PubMed] [Google Scholar]
- [2].Davidson AT., Sr Early operation in the treatment of small bowel obstruction. J Natl Med Assoc 1981;73:245–6. [PMC free article] [PubMed] [Google Scholar]
- [3].Popoola D, Lou MA, Mansour AY, et al. Small bowel obstruction: review of nine years of experience. J Natl Med Assoc 1984;76:1089–94. [PMC free article] [PubMed] [Google Scholar]
- [4].Fleshner PR, Siegman MG, Slater GI, et al. A prospective, randomized trial of short versus long tubes in adhesive small-bowel obstruction. Am J Surg 1995;170:366–70. [DOI] [PubMed] [Google Scholar]
- [5].Becker WF. Acute adhesive ileus; a study of 412 cases with particular reference to the abuse of tube decompression in treatment. Surg Gynecol Obstet 1952;95:472–6. [PubMed] [Google Scholar]
- [6].Franklin ME, Jr, Gonzalez JJ, Jr, Miter DB, et al. Laparoscopic diagnosis and treatment of intestinal obstruction. Surg Endosc 2004;18:26–30. [DOI] [PubMed] [Google Scholar]
- [7].Stewardson RH, Bombeck CT, Nyhus LM. Critical operative management of small bowel obstruction. Ann Surg 1978;187:189–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Gowen GF. Long tube decompression is successful in 90% of patients with adhesive small bowel obstruction. Am J Surg 2003;185:512–5. [DOI] [PubMed] [Google Scholar]
- [9].Oremus M, Wolfson C, Perrault A, et al. Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer's disease drug trials. Dement Geriatr Cogn Disord 2001;12:232–6. [DOI] [PubMed] [Google Scholar]
- [10].Slim K, Nini E, Forestier D, et al. Methodological index for nonrandomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003;73:712–6. [DOI] [PubMed] [Google Scholar]
- [11].Bizer LS, Liebling RW, Delany HM, et al. Small bowel obstruction: the role of nonoperative treatment in simple intestinal obstruction and predictive criteria for strangulation obstruction. Surgery 1981;89:407–713. [PubMed] [Google Scholar]
- [12].Brolin RE, Krasna MJ, Mast BA. Use of tubes and radiographs in the management of small bowel obstruction. Ann Surg 1987;206:126–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Chen XL, Ji F, Lin Q, et al. A prospective randomized trial of transnasal ileus tube vs nasogastric tube for adhesive small bowel obstruction. World J Gastroenterol 2012;18:1968–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Williams SB, Greenspon J, Young HA, et al. Small bowel obstruction: conservative vs. surgical management. Dis Colon Rectum 2005;48:1140–6. [DOI] [PubMed] [Google Scholar]
- [15].Gowen GF. Rapid resolution of small-bowel obstruction with the long tube, endoscopically advanced into the jejunum. Am J Surg 2007;193:184–9. [DOI] [PubMed] [Google Scholar]
- [16].Wangensteen OH, Paine JR. Treatment of intestinal obstruction by suction with a duodenal tube. JAMA 1933;101:1532–9. [Google Scholar]
- [17].Abbott WO, Johnston CG. Intubatic studies of the human small intestine. X. a non-surgical method of treating, localizing and diagnosing the nature of obstructive lesions. Surg Gynecol Obstet 1938;66:691. [Google Scholar]
- [18].Johnson FW, Goodale RL, Leonard AS, et al. Rapid long tube intubation of the jejunum by a new endoscopic device. Am J Surg 1976;131:91–3. [DOI] [PubMed] [Google Scholar]
- [19].Dennis C. The gastrointestinal sump tube. Surgery 1969;66:309–12. [PubMed] [Google Scholar]
- [20].Cantor MO., Jr New simplified intestinal decompression tube. Am J Surg 1946;72:137–42. [DOI] [PubMed] [Google Scholar]
- [21].Maglinte DD, Kelvin FM, Micon LT, et al. Nasointestinal tube for decompression or enteroclysis: experience with 150 patients. Abdom Imaging 1994;19:108–12. [DOI] [PubMed] [Google Scholar]
- [22].Wolfson PJ, Bauer JJ, Gelernt IM, et al. Use of the long tube in the management of patients with small-intestinal obstruction due to adhesions. Arch Surg 1985;120:1001–6. [DOI] [PubMed] [Google Scholar]
- [23].Hunter TB, Fon GT, Silverman ME. Complications of intestinal tubes. Am J Gastroenterol 1981;76:256–61. [PubMed] [Google Scholar]
- [24].Hafner CD, Wylie JH, Jr, Brush BE. Complications of gastrointestinal intubation. Arch Surg 1961;83:147–60. [DOI] [PubMed] [Google Scholar]
- [25].Snyder CL, Ferrell KL, Goodale RL, et al. Nonoperative management of small-bowel obstruction with endoscopic long intestinal tube placement. Am Surg 1990;56:587–92. [PubMed] [Google Scholar]


