Abstract
The aim of the study was to identify the effectiveness of posterior pedicle screw instrumentation without osteotomy in the management of adolescent idiopathic scoliosis (AIS).
The AIS patients underwent standing anteroposterior and lateral radiography before and after surgery. Age, sex, Lenke type, preoperative and postoperative Cobb angle, and all the related complications were recorded at final follow-up.
We investigated data from 137 AIS patients who underwent posterior pedicle screw instrumentation without osteotomy from January 2012 to January 2016 with >2 years follow-up. Mean age was 14.3 ± 1.5 years at operation. The preoperative and latest postoperative coronal Cobb angle was 60 ± 12° and 9 ± 5°, respectively. Additionally, complications were noted in 6 patients. However, the prognosis of all the AIS patients was good, and the satisfaction of the Scoliosis Research Society Outcomes Instrument (SRS-22) questionnaire was 4.4 ± 0.5 at final follow-up.
In the management of mild and moderate AIS, satisfactory clinical results can be obtained using posterior pedicle screw instrumentation without osteotomy.
Keywords: adolescent idiopathic scoliosis, Lenke type, osteotomy, pedicle screw instrumentation
1. Introduction
Adolescent idiopathic scoliosis (AIS) is a three-dimensional deformity of the spine, and causes problems as back pain, pulmonary restriction, reduced mobility, and disfigurement.[1,2] The incidence of AIS in the general population ranges from 2% to 3%.[3]
At present, the AIS disease represents a multifactorial condition stemming from genetic, biochemical, nutritional, and biomechanical influences. Scoliosis may also be affected by select neurologic and neuromuscular influences, such as cerebral palsy, paralysis, and muscular dystrophies.[4,5] If the final spinal curvature surpasses a certain critical threshold, the risk of health problem and curve progression would increase. Surgical correction with instrumentation is normally recommended for curvatures exceeding 40° to 50° to stop curvature progression with a view to achieve better truncal balance and cosmesis.[6]
Spinal osteotomy is effective for the treatment of severe spinal deformity and its correct rate is about 51% to 69%.[7] Spinal osteotomy can increase the magnitude of correction both in the coronal and sagittal plane. However, spinal osteotomy may bring higher complication risk, such as blood loss, infections, cerebrospinal fluid leaks, and implant failures.
To identify the clinical outcomes of posterior pedicle screw instrumentation without osteotomy in the management of AIS, we reviewed 137 AIS patients in our institution.
2. Materials and methods
Our institutional review board approved the retrospective review of medical records and the analysis of pertinent data. The analysis data file did not contain any information that could be traced to specific subjects.
The included AIS patients were managed by 1 senior spine surgeon and his team from January 2012 to January 2016. After successful anesthesia, patients were placed in the prone position. Using a midline incision, anatomical exposure of the spine was performed using a subperiosteal dissection of the paraspinal muscles. After confirmation of the location of the bilateral vertebral pedicles, screws were placed in an anatomic position. On the concave side, distraction was performed after single rod rotation. On the convex side, compression was performed after inserting the implant rod. The 2-step locking caps were tightened. Allograft bone material and the disposed laminae and transverse processes were used for fusion. All patients underwent posterior pedicle screw instrumentation without osteotomy. After surgery, every patient wore external brace for half a year.
The hospital charts were reviewed for demographic data. Every patient underwent standing anteroposterior and lateral radiography of the whole spine before and after surgery. The coronal curve was measured by the Cobb method. Coronal balance was measured as the distance between the C7 plumb line and the central sacral line.
3. Results
A total of 137 AIS patients were included in the current study. There were 125 girls and 12 boys with the age of 14.3 ± 1.5 years. All patients were followed up at least for 2 years (range, 2.1–5.6 years).
The preoperative coronal Cobb angle was 60 ± 12°. The latest postoperative coronal Cobb angle was 9 ± 5°. The correction rate of coronal Cobb angle was about 83.5%. The preoperative and postoperative coronal balance was 14 ± 5 mm and 5 ± 3 mm, respectively (Table 1).
Table 1.
Demographic and radiographic data of the 137 adolescent idiopathic scoliosis.

Complications were noted in 6 patients, including rod breakage in 1 patient, neurologic injury in 1 patient, and incisional drainage in 4 patients. Luckily, the prognosis of every AIS patient was good. The satisfaction of the Scoliosis Research Society Outcomes Instrument (SRS-22) questionnaire was 4.4 ± 0.5 at final follow-up (Table 2).
Table 2.
The SRS-22 questionnaire of the 137 adolescent idiopathic scoliosis.

3.1. Representative cases
No. 1 patient, a 16-year-old boy diagnosed Lenke I AIS, underwent posterior pedicle screw instrumentation without osteotomy. The preoperative and postoperative 2 years Cobb angle were 47° and 5° (Fig. 1).
Figure 1.
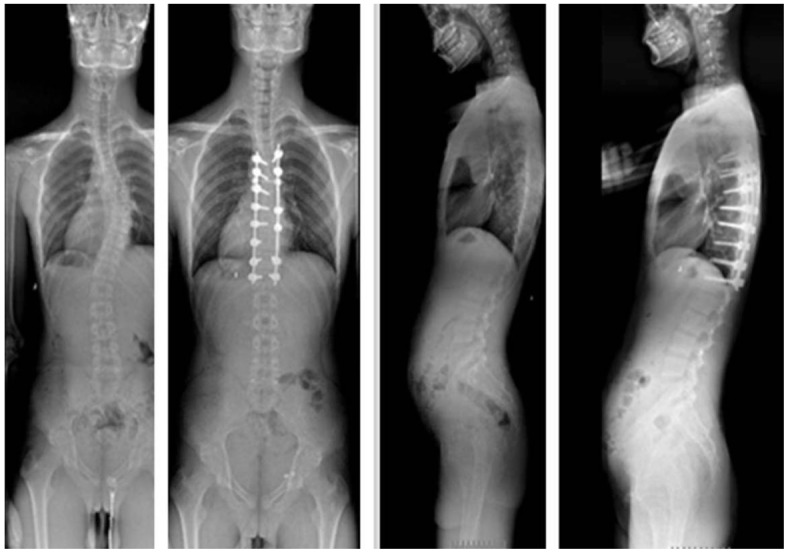
One Lenke I patient underwent posterior pedicle screw instrumentation without osteotomy.
No. 2 patient, a 12-year-old girl diagnosed Lenke V AIS, underwent posterior pedicle screw instrumentation without osteotomy. The preoperative and postoperative 2 years Cobb angle were 43° and 2° (Fig. 2).
Figure 2.
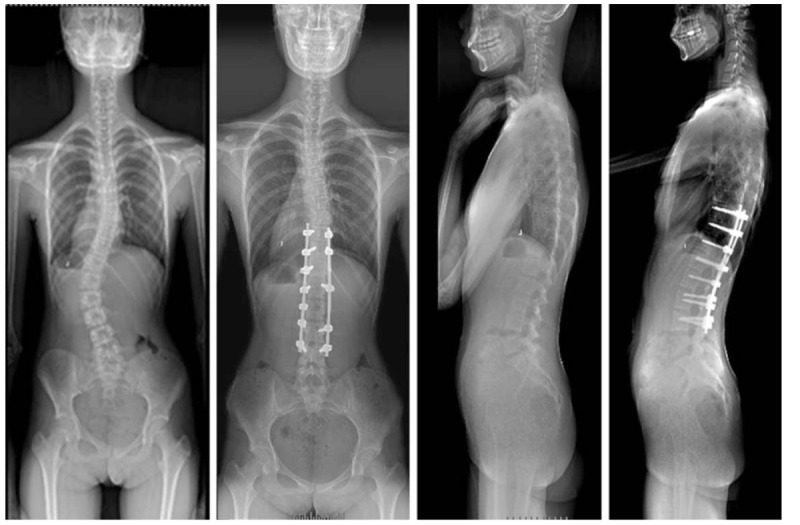
One Lenke V patient underwent posterior pedicle screw instrumentation without osteotomy.
4. Discussion
The management of spinal deformity in the adult has gone through a significant evolution during the past decades. The treatment options of AIS include serial observation and bracing, but ultimately many AIS patients still require operative intervention with the goal to achieve a stable well-balanced spine. Additionally, spinal osteotomy is usually used to obtain better coronal and sagittal balance in spinal deformity surgery. However, the results of the current study showed posterior pedicle screw instrumentation without osteotomy could acquire satisfactory improvement in the management of mild and moderate AIS.
Several different types of osteotomies, such as Smith-Petersen osteotomy, pedicle subtraction osteotomy, vertebral column resection, and bone-disc-bone osteotomy have been reported.[8,9] Spinal osteotomy is an effective and useful technique for severe spinal deformity and its correction rate is 51% to 69%.[7] However, the current study showed the correction rate of coronal Cobb angle was about 83.5%. In addition, spinal osteotomy may bring higher complication risk, such as blood loss, infections, cerebrospinal fluid leaks, and implant failures. According to the results by Smith et al,[10] the most common complication was rod breakage, and its incidence was 31.7% for 3-column osteotomy in 82 adult spinal deformity patients (68 patients were treated with pedicle subtraction osteotomy and 14 patients were treated with vertebral column resection). However, the current study showed the incidence of rod breakage was about 0.7% (1/137). Thus, it may be no need to do osteotomy in the management of mild and moderate AIS.
To our knowledge, several articles reported the incidence of neurologic deficits was about 1.0% to 30.8% in spinal scoliosis correction.[11–13] However, the results of the current study showed it was about 0.7% (1/137). In recent years, intraoperative neuromonitoring has become a standard of care in spinal deformity surgery to minimize the incidence of neurological deficit. With its assistance, the incidence of neurologic injury has declined.[14,15] As the sensitivity was 100% and specificity was 93% to 100% for transcranial electric motor evoked potentials, the neurological injury rate was 0% for AIS cases, and it was significantly lower than that in previous studies.[15] However, only a certain number of hospital in China have intraoperative neural electrophysiological monitoring. Thus, wake-up test is still a simple and effective way to find out whether there was neurological deficit. As neurologic deficit was the most terrible complication, spine surgeons should take all measures to avoid.
As for incisional drainage, the incidence was 2.9% (4/137) according to the result of the current study. However, in recent 2 years, we used absorbable sutures instead of ordinary silk thread to close the incision, and we found that the incidence of incisional drainage was declined. The reason may be that absorbable sutures have better histocompatibility with human body.
5. Conclusion
In conclusion, in the management of mild and moderate AIS, satisfactory clinical results can be obtained using posterior pedicle screw instrumentation without osteotomy. Certainly, large scale and long term follow-up is needed to determine the effectiveness of posterior pedicle screw instrumentation without osteotomy in the management of severe AIS.
Author contributions
Conceptualization: Ning Li, Ming-kui Shen, Lei Xia.
Data curation: Ning Li, Chen Xu, Ming-kui Shen, Ming Luo, Lei Xia.
Formal analysis: Ning Li, Ming Luo, Jie Wang.
Investigation: Chen Xu, Ming Luo, Jie Wang.
Methodology: Ning Li, Chen Xu, Ming-kui Shen, Ming Luo, Jie Wang.
Resources: Ming-kui Shen.
Supervision: Lei Xia.
Writing – original draft: Ning Li, Ming Luo, Lei Xia.
Writing – review & editing: Chen Xu, Lei Xia.
Footnotes
Abbreviation: AIS = adolescent idiopathic scoliosis.
NL and CX have contributed equally to this work.
This paper is neither the entire paper nor any part of its content has been published or has been accepted elsewhere.
Consent for publication: Yes, the Open Access-License to Publish was completed.
Ethics approval and consent to participate: This study was approved by the Institutional Review Board in Zhengzhou University.
The authors declare that they have no funding.
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflicts of interest in connection with the submitted article.
References
- [1].Fong DY, Lee CF, Cheung KM, et al. A meta-analysis of the clinical effectiveness of school scoliosis screening. Spine (Phila Pa 1976) 2010;35:1061–71. [DOI] [PubMed] [Google Scholar]
- [2].Weinstein SL, Dolan LA, Cheng JC, et al. Adolescent idiopathic scoliosis. Lancet 2008;371:1527–37. [DOI] [PubMed] [Google Scholar]
- [3].Giampietro PF. Genetic aspects of congenital and idiopathic scoliosis. Scientifica (Cairo) 2012;2012:152365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kouwenhoven JW, Castelein RM. The pathogenesis of adolescent idiopathic scoliosis: review of the literature. Spine (Phila Pa 1976) 2008;33:2898–908. [DOI] [PubMed] [Google Scholar]
- [5].Lombardi G, Akoume MY, Colombini A, et al. Biochemistry of adolescent idiopathic scoliosis. Adv Clin Chem 2011;54:165–82. [DOI] [PubMed] [Google Scholar]
- [6].Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis. Cochrane Database Syst Rev 2015;CD010663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Lenke LG, Sides BA, Koester LA, et al. Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res 2010;468:687–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Enercan M, Ozturk C, Kahraman S, et al. Osteotomies/spinal column resections in adult deformity. Eur Spine J 2013;22(suppl):S254–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Xia L, Li P, Wang D, et al. Spinal osteotomy techniques in management of severe pediatric spinal deformity and analysis of postoperative complications. Spine (Phila Pa 1976) 2015;40:E286–92. [DOI] [PubMed] [Google Scholar]
- [10].Smith JS, Shaffrey CI, Klineberg E, et al. Complication rates associated with 3-column osteotomy in 82 adult spinal deformity patients: retrospective review of a prospectively collected multicenter consecutive series with 2-year follow-up. J Neurosurg Spine 2017;27:444–57. [DOI] [PubMed] [Google Scholar]
- [11].Hamilton DK, Smith JS, Sansur CA, et al. Rates of new neurological deficit associated with spine surgery based on 108,419 procedures: a report of the scoliosis research society morbidity and mortality committee. Spine (Phila Pa 1976) 2011;36:1218–28. [DOI] [PubMed] [Google Scholar]
- [12].Qiu Y, Wang S, Wang B, et al. Incidence and risk factors of neurological deficits of surgical correction for scoliosis: analysis of 1373 cases at one Chinese institution. Spine (Phila Pa 1976) 2008;33:519–26. [DOI] [PubMed] [Google Scholar]
- [13].Xia L, Li N, Wang D, et al. One-stage posterior spinal osteotomy in severe spinal deformities: a total of 147 cases. Clin Spine Surg 2017;30:E448–53. [DOI] [PubMed] [Google Scholar]
- [14].Thirumala PD, Crammond DJ, Loke YK, et al. Diagnostic accuracy of motor evoked potentials to detect neurological deficit during idiopathic scoliosis correction: a systematic review. J Neurosurg Spine 2017;26:374–83. [DOI] [PubMed] [Google Scholar]
- [15].Zuccaro M, Zuccaro J, Samdani AF, et al. Intraoperative neuromonitoring alerts in a pediatric deformity center. Neurosurg Focus 2017;43:E8. [DOI] [PubMed] [Google Scholar]


