Abstract
We aimed to analyze factors related to human immunodeficiency virus (HIV) infection among 15 to 25-year-old rural unmarried Yi adolescents in Liangshan Yi Autonomous Prefecture from 2011 to 2016, and to investigate the relationship among the HIV-related risk factors.
Three sites (Butuo, Zhaojue, and Ganluo counties) with a Yi population were selected from 2011 to 2016 in Liangshan prefecture. We used questionnaires to investigate demographic and behavioral characteristics and performed HIV testing. Logistic regression analysis and multiple correspondence analysis (MCA) were used to analyze the data.
A total of 6311 qualified rural unmarried Yi adolescents were involved in this study, with an HIV infection rate of 4.18% (264/6311). Logistic regression analysis indicated that males (OR = 1.56, 95% CI = 1.17–2.08), illiteracy (OR = 2.70, 95% CI = 1.79–4.08), primary school education or below (OR = 1.62, 95% CI = 1.12–2.36), history of out-migrating for work (OR = 1.58, 95% CI = 1.18–2.13), and injecting drug user (IDU) (OR = 6.42, 95% CI = 3.06–13.46) contributed to the risk of HIV infection. MCA revealed a strong interrelationship between the following risk factors and HIV infection: aged 23 to 25 years, IDU, history of out-migrating for work, and ever having sexual behaviors.
HIV infection among 15 to 25-year-old rural unmarried Yi adolescents in Liangshan is a serious issue. MCA and logistic regression analysis can be used to assess the relationship between risk factors for HIV infection.
Keywords: adolescents, HIV, multiple correspondence analysis, risk factors, sentinel surveillance, Yi people
1. Introduction
Liangshan Yi Autonomous Prefecture is located in southwest China and had a population of 4.97 million people in 2013, of which 50.7% (2.52 million) were Yi ethnicity, making it the largest Yi population in China. From 2011 to 2013, 88.07% of new HIV (uman immunodeficiency virus) infections were in the Yi population.[1,2] As one of the most serious AIDS (acquired immune deficiency syndrome) epidemic areas in China, the first HIV-positive case was reported among injection drug users (IDU) in 1995. Since then, Liangshan has become one of the most severely HIV-affected epidemic regions in China.[1,3] Up to December 2015, a total of 29,987 HIV/AIDS cases had been reported, and the HIV epidemic had spread throughout Liangshan's 17 districts.[2] The region is located along the drug trafficking routes from the “Golden Triangle” to northwest and central China with injected drug use (IDU) know to be the main HIV diffusion pathway.[4–6]
HIV disproportionately affects young people worldwide, and it is more likely to affect youths in developing and undeveloped countries.[7–9] It was estimated that approximately 5 million youths were living with HIV in 2009, with new infections accounting for approximately 40% (0.89 million) of HIV infections in youths globally.[10] Each year, in a resource-limited setting, approximately 0.9 million new HIV infections occur among adolescents, representing 40% of new infections worldwide.[11] Although HIV prevalence has worldwide variation, adolescents have the highest risk of HIV infection compared to all other age groups.[12] In recent decades, the number of new HIV infections among youths has increased both in China and also in the Liangshan prefecture.[10,13]
Adolescence is described as a period of momentous social, psychological, economical, and biological transitions,[8] during which adult supervision decreases while young people still have limited knowledge, economic dependence, self-confidence, and life skills. This can lead to engagement in risk behaviors, such as drug use, multiple partners, and unprotected sexual activities.[14] These behaviors may contribute to the risk of HIV infection, thus, youths are more vulnerable to HIV exposure and infection.
HIV sentinel surveillance (HSS) is an important strategy for monitoring the HIV epidemic. To understand the epidemic of HIV/AIDS in this age group, HSS for rural unmarried young people has been conducted in Liangshan Prefecture since 2011. We previously observed that the incidence of HIV in Yi young people was much higher than Han or other ethnic groups,[15] suggesting that Yi adolescents are at higher risk of HIV infection.
In this study, we performed HSS for rural unmarried adolescents at 3 sites (Zhaojue, Ganluo, and Butuo) with a majority-Yi population in Liangshan Prefecture. Understanding HIV infection related factors among Yi adolescents in this area is critical in the development of HIV prevention policies and strategies. Therefore, we aimed to analyze factors related to HIV infection and the relationship between these factors among 15 to 25-year-old rural unmarried Yi adolescents in Liangshan Yi Autonomous Prefecture from 2011 to 2016.
2. Materials and methods
2.1. Ethics
All subjects volunteered to participate in the study and signed informed consents before enrollment. This study was approved by the ethics committee of Liangshan Yi Autonomous Prefecture for Disease Control and Prevention (CDC), and the study was carried out in accordance with the Helsinki Declaration of 1964.
2.2. HSS site selection
HSS sites in Liangshan Prefecture were selected to be representative of the prefecture's HIV epidemic, based on data analysis by the Chinese CDC and the Sichuan CDC.[16] Multistage stratified random sampling was performed to acquire the study sample. We selected 3 counties (Zhaojue, Ganluo, and Butuo) with a majority-Yi population, which showed the highest HIV infection rates in Liangshan Prefecture. First, all towns in each of the selected counties were classified according to 3 levels by HIV/AIDS prevalence (mild, medium, or severe level). One town was randomly selected among towns with mild and severe levels, and 2 towns were randomly selected among those with medium levels. Four towns were selected in each surveillance county. Second, 2 villages were randomly selected from each selected town, and approximately 50 unmarried Yi adolescents aged 15 to 25 years old were randomly enrolled in each village. In total, 6311 unmarried Yi adolescents were enrolled in this study from 2011 to 2016 (there were 972, 1057, 1045, 944, 1166, and 1127 participants from 2011 to 2016, respectively).
2.3. Questionnaire
The questionnaire was accompanied by an introduction of the study purpose. It was designed by Sichuan CDC and Liangshan CDC. The questionnaire provided to study participants was 2 pages long and included demographic characteristics, knowledge of HIV prevention, attitude toward premarital sexual behaviors, and behavioral characteristics. The demographic characteristics collected were age, ethnicity, and education level. Knowledge of HIV prevention was assessed via 8 items, each expressed with a 2-point Likert scale of 0 (no) to 1 (yes). A total score greater than 5 was considered to indicate awareness of HIV prevention; otherwise, the respondent was considered unaware of effective HIV prevention principles. Behavioral characteristics included drug use, IDU, sexual behaviors, casual sexual behaviors in the past year, and history of out-migrating for work.
The questionnaire was administered through face-to-face interviews by trained investigators and was anonymous.
2.4. HIV testing
Before the interview, each subject was asked to provide 3 to 5 mL of venous blood for HIV testing. Specimens were tested for HIV at the Liangshan Prefecture CDC. Enzyme-linked immunosorbent assay (ELISA) was used to screen specimens and Western blotting was used for the presence of HIV antibodies. Negative ELISA results indicated no HIV infection, while those with positive results were re-tested for HIV antibodies using Western blot. If the second test for HIV was positive, the serum was confirmed as positive for HIV antibody. If negative, the serum was regarded as negative for HIV antibody.
2.5. Statistical analysis
EpiData (Version 3.1) database was used for data input. All data analyses were performed using Statistical package for the social sciences (SPSS) version 21.0 for Windows (SPSS, Inc, Chicago, IL). Significance level of 0.05 was used for all statistical tests. Categorical variables were expressed as frequencies and percentages. Categorical variables were compared between the 2 investigated groups using the Pearson chi-square (χ2) or Fisher's exact test. Prevalence was calculated using the number of HIV-positive respondents as the numerator and the total number of respondents as the denominator, presented with 95% confidence intervals (CIs). A multivariate logistic regression model was used to evaluate the relationship between demographic and behavioral characteristics and the overall risk of HIV infection over the period from 2011 to 2016. The results were expressed as odds ratios (ORs) and 95% CIs.
Based on the logistic regression analysis, multiple correspondence analysis (MCA) was used to investigate the correlation between risk factors for HIV infection. MCA is a graphical method designed for descriptive analysis of large matrices of categorical data, and enables the identification of relationships between a large number of variables simultaneously.[17–20] MCA maps variables as points on a low-dimensional graph, commonly the first 2 dimensions of variation are plotted to display.[17,18,20] Two main applicable conditions were used for the good fit of the MCA model: 1) the cumulative contribution rates of the first 2 factors were more than 75%;[21,22] 2) there is a connection between row and column variables.[19,20] Based on the results of the logistic regression analysis and expertise, we explored the cumulative contribution rate of the first 2 common factors by grouping variable combinations and selecting variables. An applicability test was performed using the chi-square test to improve the interpretability of results. The position and distances of all kinds of scatter in the correspondence analysis charts reflects the interrelationship among factors. The closer the points are on the plot, the more correlated the relationship is.[17,18,20,23]
3. Results
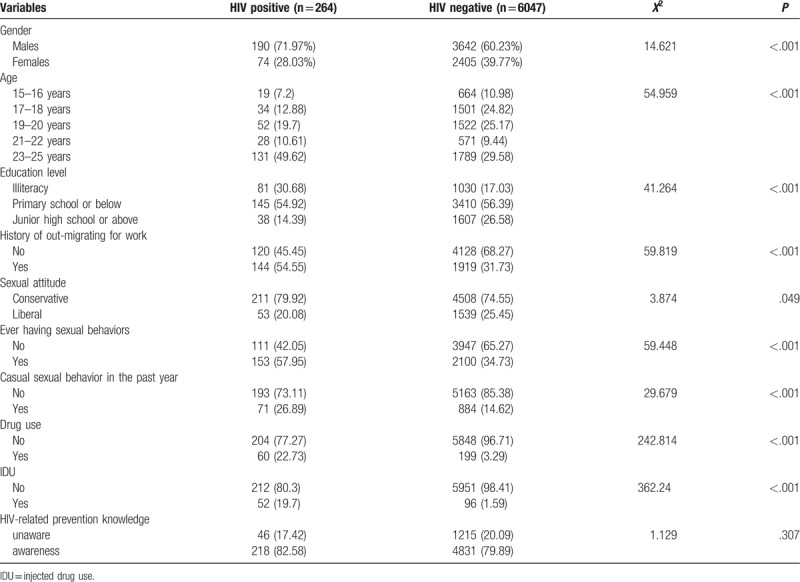
From 2011 to 2016, the HIV infection rate was 4.18% (264/6311) among unmarried Yi adolescents. The prevalence of HIV infection was higher in males (4.96%) than in females (2.99%) (χ2 = 14.621, P < .001) (Table 1). There were significant differences in the HIV infection rates in terms of age, educational level, history of out-migrating for work, sexual attitudes, ever having sexual behaviors, casual sexual behaviors in the past year, drug use, and IDU (P < .05). However, no statistically significant difference was found in terms of the knowledge of HIV-related prevention between HIV infections and non-HIV infections (P > .05).
Table 1.
The characteristics of the HIV in 15 to 25-year-old rural unmarried Yi adolescents.
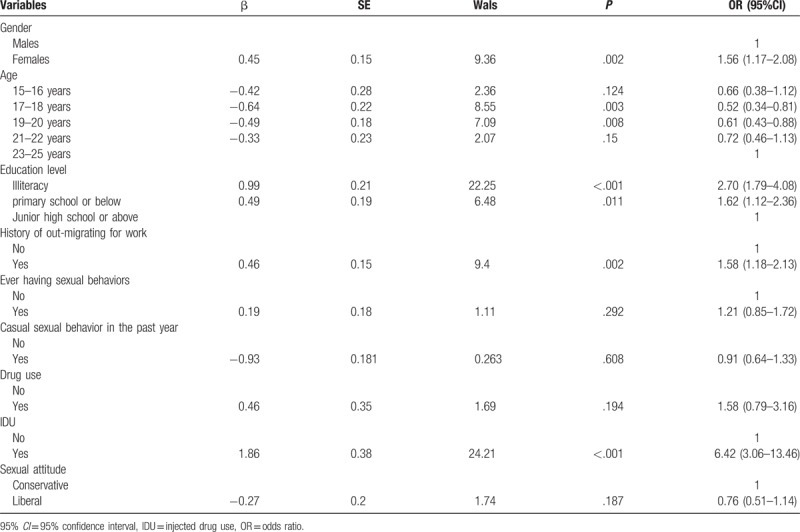
Multivariate logistic regression analysis showed that, among rural unmarried Yi adolescents, significantly higher HIV risk was observed with males (OR = 1.56, 95% CI = 1.17–2.08), illiteracy (OR = 2.70, 95% CI = 1.79–4.08), primary school education or below (OR = 1.62, 95% CI = 1.12–2.36), history of out-migrating for work (OR = 1.58, 95% CI = 1.18–2.13), and IDU (OR = 6.42, 95% CI = 3.06–13.46) (Table 2). Compared to rural unmarried Yi adolescents in the 23 to 25-year-old age group, the 17 to 18-year-old age group (OR = 0.52, 95% CI = 0.34–0.81) and 19 to 20 year-old age group (OR = 0.61, 95% CI = 0.43–0.88) had a lower risk of HIV infection.
Table 2.
Multivariate logistic regression analysis of factors associated with HIV positivity in rural unmarried Yi adolescents.
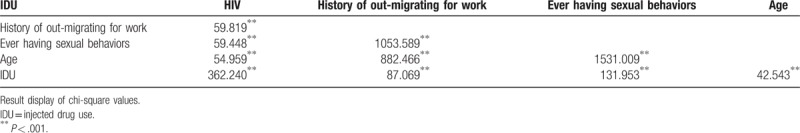
Based on the multivariate logistic regression analysis and expertise, 5 variables (HIV infection, history of out-migrating for work, ever having sexual behaviors, IDU, and age) were selected for the MCA. The correlation analysis indicated that all selected factors were strongly correlation with each other (Table 3).
Table 3.
The correlation analysis of research variables.
We observed that the contribution rates of the first and second dimension were 48.7% and 38.5%, respectively, with a cumulative contribution rate of 87.2%, and the MCA fitted well. The MCA results are displayed in Figure 1. We observed a close relationship among IDU, ever having sexual behaviors, history of out-migrating for work, 23 to 25 years old and HIV positivity, while a moderate correlation was found among those without a history of out-migrating for work and IDU, having no sexual behaviors, 15 to 18 years old and HIV negativity.
Figure 1.
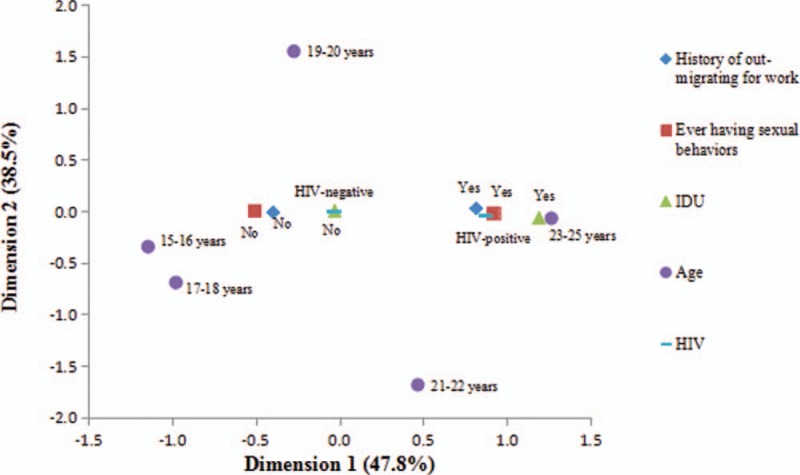
Correspondence plot of data from 15 to 25-year-old rural unmarried Yi adolescents.
4. Discussion
This study found that HIV prevalence of 15 to 25-year-old rural unmarried Yi adolescents in Liangshan Yi Autonomous Prefecture from 2011 to 2016 was 4.18%, much higher than the national HIV infection rate of 0.037% (501,000/1,367,820) in 2014,[24] 0.17% in Sichuan Province,[25] and 0.54% to 0.56% in Liangshan prefecture in 2012.[26] The Yi people, with a population of approximately 8 million, live primarily in rural areas (usually in mountainous regions) and most often in the poorest rural areas.[27] AIDS, which has been described as a “disease of poverty,” is not a result of poverty itself, but is related to economic, culture, and gender inequality as factors affecting behavior, that have potential implications for the spread of HIV.[28]
We found that history of out-migrating for work was strongly associated with a HIV positive result, which indicates that out-migrating for work is a high risk factor for HIV infection in this population. In order to improve their living conditions and income, an increasing number of Yi people, especially young people, leave the mountainous regions for work.[29] In our analysis, 32.69% of adolescents had experience of migrant work. These migrant workers may work far from home, away from restraints exerted by their parents, and often travel from place to place with constant changes in living conditions, which may increase risky sexual activities, such as having multiple casual sexual partners, engaging in sex with commercial sex workers, and drug use.[30,31] Meanwhile, the educational level of Yi people is generally low, and we found that illiteracy rates reached 17.60% among the rural unmarried Yi adolescents. A lower level of education may be associated with poor HIV-related knowledge and low self-perceived risk, and might be related to the increasing HIV prevalence among young people.[10] Due to low education and lack of skills, these migrant youths are marginalized in society, culture, and the economy, and they are vulnerable to engage in risk behaviors for HIV infection.[32,33]
Ever having sexual behaviors was most closely associated with HIV-positive and out-migrating for work. We observed that 44.65% of respondents had had sex before, and that 42.12% of which happened their first sexual behavior when aged younger than 18 years old, and the minimum age was only 10 years old. These results demonstrate that premarital sex was common among Liangshan rural unmarried Yi adolescents, which was attributed to the unique sex culture of the Yi ethnicity (i.e., early first sexual behavior, open concept of sex, tolerance of premarital sex, and frequent casual sexual behaviors).[34,35] Although multivariable logistic regression results did not find a significant association between sexual behavior (OR = 1.21, 95% CI = 0.85–1.72) with the risk of HIV infection, the MCA showed that HIV-positive was strongly associated with sexual behavior. The main reason for this is that MCA can present the relationship of multiple variables simultaneously and discover underlying factors.[20,22]
Our previous study found that the HIV epidemic has gradually changed, with a shift in high-risk behaviors from IDU to heterosexual behaviors among youths aged between 15 and 24 years, with approximately 68.4% of new HIV infections spread through unsafe sexual behaviors in 2014.[13] These results indicated that sexual behaviors play a critical role in HIV infection in this area, and 4 factors in the Yi population contributing to high risk behaviors of HIV infection and unsafe sexual contact have been identified. First, almost all Yi people maintain traditional social norms and values, such as levirate marriage, which results in HIV transmission from an infected widow her to brother in law.[36,37] Second, Yi people are tolerant of casual and multiple sexual behaviors for unmarried adolescents and males, which occurs in the context of their social activities such as “Ganchang,” and is therefore part of the Yi lifestyle.[38] Previous studies have estimated that the proportion of concurrent sexual partnerships of Yi people were higher than some parts of sub-Saharan Africa.[38,39] Third, Yi people have shown negative attitudes toward condoms, since condoms were considered as a means of birth control and distrust. Fourth, the tradition of “son preference” widely exists in Yi people, and HIV-infected husbands do not use a condom during intercourse within marriage because they wish to have a son, a practice that can spread HIV infection within the family.[40] Therefore, these cultures and traditions contribute to the spread of HIV infection through sexual behaviors in this ethnic group.
With a combination of MCA and Logistics regression analyses, we found that IDU (OR = 6.44, 95% CI = 3.07–2.11) had a profound impact on HIV infection among the rural unmarried Yi adolescents. The following 3 factors could explain the close association between IDU and HIV infection in this area: Liangshan is located on a major drug trafficking route[4] and has a long history of opium cultivation and opium/heroin trade;[41] the “sharing” of Yi people's traditional culture makes them more likely to share syringes when IDU;[29] they are unaware of the importance of needle exchange due to lacking education and health knowledge. Therefore, IDU is still serious among Yi adolescents in this area.
MCA results showed a strong relationship between the 23 and 25-year-old group and HIV infection. The older adolescents are entering society and demanding more money and higher social status, and they are inclined engage in high risk behaviors, such as drug trafficking, and casual and commercial sexual behaviors.[8,42] Wang et al[32] showed that the rate of sexual risk behaviors among unmarried people increased significantly with age. We also found that older age adolescents were closely correlated with out-migrating for work than younger ages, and out-migrating may increase their HIV-related risk behaviors as described above.
There are 2 strengths that should be mentioned in our study. First, it is the first time the interrelationship between factors related to HIV infection among the Yi adolescents in poor areas has been investigated. Second, a combination of logistic regression analysis and MCA allows for the visual display of the correlation among multiple variables, and can reveal potential factors.
The study had one limitation that should be considered. All variables were self-reported, and it was difficult to obtain answers to many sensitive questions by face-to-face investigation, such as those relating to sexual behavior and drug use. The sexual tradition of Yi people is “can do but cannot say,” and thus the real situation of their sexual behaviors may be underestimated.
5. Conclusions
HIV infection among 15 to 25-year-old rural unmarried Yi adolescents in Liangshan Prefecture is severe, and risk factors that have a strong association with HIV infection include being aged 23 to 25 years old, IDU, history of out-migrating for work, and ever having sexual behaviors. MCA and logistic regression analysis can be used to evaluate the internal relationships among factors related to HIV infection. It is necessary to develop policies to alleviate poverty, improve education level, and change traditions regarding sexual behaviors, so as to decrease the transmission of HIV in this area.
Author contributions
Data curation: Lei Nan, Suhua Zhang, Lin Xiao, Jianxin Zhang, Zhuo Wang.
Investigation: Chunnong Ji-ke, Qixing Wang, Qiang Liao, Gang Yu, Lin Xiao, Yuhan Gong, Ke Wang, Ju Wang.
Project administration: Shujuan Yang.
Writing – original draft: Rong Pei, Shujuan Yang.
Footnotes
Abbreviations: 95% CI = 95% confidence interval, AIDS = acquired immune deficiency syndrome, CDC = Center for Disease Control and Prevention, HIV = human immunodeficiency virus, HSS = HIV sentinel surveillance, IDU = injected drug use, MCA = multiple correspondence analysis, OR = odds ratio, SPSS = statistical package for the social sciences.
Funding: This research was supported by grant funding from the National Natural Science Foundation of China (81703279); project of health economics evaluation of influence and control mode in anti-poverty by relocating in other places for the risk of HIV infection in Liangshan Yi Autonomous (H170614); HIV/AIDS control and prevention project in Liangshan (h61236); project of Health and Family Planning Commission of Sichuan Province (16PJ259).
The authors have no conflicts of interest to disclose.
References
- [1].Zhang G, Gong Y, Wang Q, et al. Outcomes and factors associated with survival of patients with HIV/AIDS initiating antiretroviral treatment in Liangshan Prefecture, southwest of China: a retrospective cohort study from 2005 to 2013. Medicine 2016;95:e3969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Zhao QG, Gong YH, Liao Q, et al. Estimation on the HIV-1 incidence in Liangshan Yi Autonomous Prefecture, under BED-capture enzyme immunoassay, from 2011 to 2013. Zhonghua Liu Xing Bing Xue Za Zhi 2016;37:1105–7. [DOI] [PubMed] [Google Scholar]
- [3].Deng L, Liu Z, Zhang S, et al. Survival time and related influencing factors of AIDS patients in Liangshan prefecture, Sichuan province, during 2008–2013. Zhonghua Liu Xing Bing Xue Za Zhi 2015;36:569–75. [PubMed] [Google Scholar]
- [4].Ruan Y, Chen K, Hong K, et al. Community-based survey of HIV transmission modes among intravenous drug users in Sichuan, China. Sex Transm Dis 2004;31:623–7. [DOI] [PubMed] [Google Scholar]
- [5].Li L, Wei D, Hsu WL, et al. CRF07_BC strain dominates the HIV-1 epidemic in injection drug Users in Liangshan Prefecture of Sichuan, China. AIDS Res Hum Retroviruses 2015;31:479–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ruan Y, Qin G, Liu S, et al. HIV incidence and factors contributed to retention in a 12-month follow-up study of injection drug users in Sichuan Province, China. J Acquir Immune Defic Syndr 2005;39:459–63. [DOI] [PubMed] [Google Scholar]
- [7].Binagwaho A, Fuller A, Kerry V, et al. Adolescents and the right to health: eliminating age-related barriers to HIV/AIDS services in Rwanda. AIDS Care 2012;24:936–42. [DOI] [PubMed] [Google Scholar]
- [8].Pettifor A, Bekker LG, Hosek S, et al. Preventing HIV among young people: research priorities for the future. J Acquir Immune Defic Syndr 2013;63(suppl 2):S155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Tang W, Babu GR, Li J, et al. The difference between HIV and syphilis prevalence and incidence cases: results from a cohort study in Nanjing, China, 2008–2010. Int J STD AIDS 2015;26:648–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Zhang X, Tang W, Li Y, et al. The HIV/AIDS epidemic among young people in China between 2005 and 2012: results of a spatial temporal analysis. HIV Med 2017;18:141–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Reif LK, Bertrand R, Benedict C, et al. Impact of a youth-friendly HIV clinic: 10 years of adolescent outcomes in Port-au-Prince, Haiti. J Int AIDS Soc 2016;19:20859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Jaspan HB, Flisher AJ, Myer L, et al. Sexual health, HIV risk, and retention in an adolescent HIV-prevention trial preparatory cohort. J Adolesc Health 2011;49:42–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Yang SJ, Wang QX, Yao YN, et al. HIV-1 incidence surveillance among young people aged between 15-24 years in Liangshan Yi autonomous prefecture during 2011–2014. Chin J AIDS STD 2017;23:811–4. [Google Scholar]
- [14].Geary CW, Burke HM, Johnson L, et al. Personal involvement of young people in HIV prevention campaign messages: the role of message format, culture, and gender. Health Educ Behav 2008;35:190–206. [DOI] [PubMed] [Google Scholar]
- [15].Liu L, Feng L, Luo YJ, et al. HIV epidemic trend among drug users in Sichuan Preovince, 1995–2012. Chin J Dis Control Prev 2014;18:702–5. [Google Scholar]
- [16].Zhang SH, Luo M, Yang SJ, et al. HIV-infection related behaviors and preventive measures among unmarried youths from the rural areas in Liangshan prefecture, 2011–2013. Zhonghua Liu Xing Bing Xue Za Zhi 2017;38:486–90. [DOI] [PubMed] [Google Scholar]
- [17].Zhou YB, Wang QX, Liang S, et al. Geographical variations in risk factors associated with HIV infection among drug users in a prefecture in Southwest China. Infect Dis Pov 2015;4:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Cavalcante Mdo S, Kerr LR, Brignol SM, et al. Sociodemographic factors and health in a population of children living in families infected with HIV in Fortaleza and Salvador, Brazil. AIDS Care 2013;25:550–8. [DOI] [PubMed] [Google Scholar]
- [19].Sourial N, Wolfson C, Zhu B, et al. Correspondence analysis is a useful tool to uncover the relationships among categorical variables. J Clin Epidemiol 2010;63:638–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Pei HB, Wu JQ, Zhou Y, et al. Multiple correspondence analysis of married women's contraceptive methods related to their demographic characteristic. Chin J Health Stat 2011;5:530–6. [Google Scholar]
- [21].Zhang WT. Advanced Tutorial of SPSS Statistical Analysis. Beijing: Higher Education Press; 2004. [Google Scholar]
- [22].Li BH, Dong SF, Sun ZQ. An application of correspongdence analysis method in the study of disease etiology. Chin J Epidemiol 2007;28:914–7. [PubMed] [Google Scholar]
- [23].Luo S, Ma JL, Chen JW. The use of subgroup-correspondence analysis in epidemiology study. Chin J Health Stat 2008;25:280–2. [Google Scholar]
- [24].Li KJ, Feng LY, Shi SH, Shi XZ, et al. Multiple correspondence analysis and its application in the study of factors influencing working-satisfaction. Chin J Health Stat 2007;24:19–21. [Google Scholar]
- [25].China national report. 2015 China AIDS Response Progress Report. In. Beijing, 2015. [Google Scholar]
- [26].Liang L, Liu L, Pei XD, et al. Detection on HIV in Sichuan Province, 2008–2011. J Prev Med Inf 2013;29:453–6. [Google Scholar]
- [27].Gong YH, Wang QX, Nan L, et al. HIV detection in Liangshan Prefecture of Sichuan from 2007 to 2012. Mod Prev Med 2014;41:3790–2. [Google Scholar]
- [28].Zhou YB, Wang QX, Liang S, et al. Geographical variations in risk factors associated with HIV infection among drug users in a prefecture in Southwest China. Infect Dis Poverty 2015;4:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Barnett A, Whiteside A. AIDS in the Twenty-first Century: Disease and Globalization 2. 2006;New York: Palgrave Macmillan, 416. [Google Scholar]
- [30].Yang SJ, Luo M, Zhang SH, et al. Overview on culture and customs related to AIDS epidemic and prevention among Yi people in Liangshan. Chin J Aids STD 2017;23:101–4. [Google Scholar]
- [31].Dai W, Gao J, Gong J, et al. Sexual behavior of migrant workers in Shanghai, China. BMC Public Health 2015;15:1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Wang KW, Wu JQ, Zhao HX, Li YY, et al. Unmarried male migrants and sexual risk behavior: a cross-sectional study in Shanghai, China. BMC Public Health 2013;13:1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Petter P, Robert G, Sarah R. Sarah Russell: squaring the circle: AIDS, poverty,and human development. PLoS Med 2007;4:1571–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Song Y, Kang D, Wang G, et al. HIV/AIDS-related knowledge and behaviors among rural married migrant women in Shandong Province, China: a comparison study. Arch Sex Behav 2015;44:367–74. [DOI] [PubMed] [Google Scholar]
- [35].Nan L, Wang QX, Xu SY, et al. A study on the role of casual sex in HIV infection among unmarried adlecents from rural areas in Liangshan Prefecture. Chin J AIDS STD 2013;6:413–5. [Google Scholar]
- [36].Yang Y, Wu CL, Liu P, et al. Situation of casual sexual behaviors and geographic sexual networks among Yi ethnic villagers in one county of Liangshan Prefecture. J Prev Med Inform 2012;28:184–6. [Google Scholar]
- [37].Zhou YB, Wang QX, Liang S, et al. HIV-, HCV-, and co-infections and associated risk factors among drug users in southwestern China: a township-level ecological study incorporating spatial regression. PLoS One 2014;9:e93157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Dai S, Shen Z, Zha Z, et al. Seroprevalence of HIV, syphilis, and hepatitis C virus in the general population of the Liangshan Prefecture, Sichuan Province, China. J Med Virol 2012;84:1–5. [DOI] [PubMed] [Google Scholar]
- [39].Yang Y, Luan RS, Liu P, et al. Casual sex and concurrent sexual partnerships among young people from an Yi community with a high prevalence of HIV in China. Asian J Androl 2012;14:758–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Mah TL. Prevalence and correlates of concurrent sexual partnerships among young people in South Africa. Sex Transm Dis 2010;37:105–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Zhou RN, Zhou DM. Situational neutral social networks and HIV risk-study on the HIV risk by sexual transmission in Liangshan. Open Times 2012;2:145–8. [Google Scholar]
- [42].Zhou YB, Liang S, Wang QX, et al. The geographic distribution patterns of HIV-, HCV- and co-infections among drug users in a national methadone maintenance treatment program in Southwest China. BMC Infect Dis 2014;14:10. [DOI] [PMC free article] [PubMed] [Google Scholar]


