Abstract
Background:
Corticosteroids are widely used to treat voice change after thyroidectomy. In this study, we evaluated the effect of a single dose of intravenous dexamethasone after thyroidectomy using a metaanalysis.
Methods:
Relevant studies were identified by searching the following databases: Medline, Embase, and Cochrane through February 2017. We followed PRISMA guidelines. The following search terms were used: “thyroidectomy,” “voice,” “steroid.” Random-effects models were used to estimate standardized mean differences (SMDs) and 95% confidence intervals.
Results:
Our search yielded one retrospective cohort study involving 122 thyroidectomy patients and 3 randomized controlled studies involving 242 thyroidectomy patients. The pooled SMD for voice quality after thyroidectomy was −0.80 (P < .05). Subgroup analysis showed significant voice quality change 1 day after administration of dexamethasone.
Conclusions:
Single-dose intravenous dexamethasone after thyroidectomy significantly improves subjective voice quality on day 1. The effect was not different significantly after day 1.
Level of evidence:
Level 2a.
Keywords: dexamethasone, thyroidectomy, voice
1. Introduction
Thyroidectomy is one of the most frequently performed surgical procedures in the world. Immediate postoperative complications include postoperative pain, nausea and vomiting, bleeding and hematoma, and voice change. Voice change may be a result of post intubation vocal fold edema, neural injury, and/or local tissue changes/inflammation.
Voice change can be permanent or transient. Voice change due to injury to the recurrent laryngeal nerve can cause significant morbidity for patients and injury of the external branch of the superior laryngeal nerve can also cause significant voice change. Other causes of voice change include intubation trauma, cricothyroid dysfunction, psychologic reaction in the postoperative period, edema, and scarring of the strap muscles.[1,2]
Corticosteroids are used widely to treat various diseases because of their anti-inflammatory and immunomodulatory effects. Corticosteroids are used in otolaryngology to treat sinusitis with nasal polyps, allergic rhinitis, and laryngeal edema.[3–5] They can be administered via multiple routes (e.g., intravenous, intramuscular, transoral, inhalational, or intralesional); however, the effect seems to be obvious.[6] Few randomized studies have investigated the role of corticosteroids in the prevention of voice change postthyroid surgery. Among these, some authors showed improved postoperative voice function in the dexamethasone group.[7,8] However, some authors reported no effects of steroids on subjective voice quality after thyroidectomy, indicating that the results remain controversial.[9] This study aimed to better describe the effects of single-dose dexamethasone on subjective voice quality after thyroidectomy.
2. Methods
2.1. Literature search strategy
Institutional review board approval and patient consent were not required due to the nature of this study. A database search (Medline, Embase, Cochrane databases) using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines was conducted with the goal of identifying all eligible studies up to February 2017.[10] The following search terms were used: “thyroidectomy,” “voice,” “steroid.” Two authors (S.H.K, J.S.K.) conducted the literature search independently. The following search details were used to search Medline: (“thyroidectomy”[MeSH Terms] OR “thyroidectomy”[All Fields]) AND (“voice”[MeSH Terms] OR “voice”[All Fields]) AND (“steroids”[MeSH Terms] OR “steroids”[All Fields] OR “steroid”[All Fields] OR “dexamethasone”[MeSH Terms] OR “dexamethasone”[All Fields]). We used analogous search words for other databases.
2.2. Selection of studies
We conducted a metaanalysis on the basis of the proposed reporting checklist from the Meta-analysis of Observational Studies in Epidemiology (MOOSE) group and PRISMA guidelines.[10,11] Reasons for exclusion were noted. Eligible studies met the following inclusion criteria: patients treated with steroids or dexamethasone or corticosteroids, retrospective or prospective studies, and data including subjective voice quality after thyroidectomy reported. Studies excluded from the analysis were studies about postoperative pain or vomiting, case reports or case series, those published in languages other than English, review articles that that did not include original data, and those where treatment options other than steroids were used.
2.3. Data extraction
Relevant data from the included studies were extracted using standardized forms and checked by 2 authors (S.H.K, J.S.K.) independently. One investigator (J.S.K.) conducted data extraction, while the other investigator (S.H.K.) checked the results for accuracy. All authors listed above rechecked data and discussed the data together to decide how to deal with any inconsistent results. The following information was independently extracted from each included study: author name, publication year, subjective voice scores before and after dexamethasone therapy, subjective voice scores of control groups, follow-up period in hours. Primary outcomes were subjective voice scores presented by continuous variables. To unify the measure of voice, “0” was designated to indicate a normal voice, while a larger score indicated worse voice quality. To deal with heterogeneity in the follow-up period among studies, follow-up periods of 1 day, 2 days, and more than 7 days were recognized.
2.4. Risk of bias assessment in individual studies
Risk of bias was assessed at the study level using the Cochrane risk of bias assessment instrument for randomized controlled trials (RCTs), and the Newcastle-Ottawa scale for observational studies.[12,13] Cochrane risk of bias was assessed across 6 domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective reporting. Each item was classified as having either a high, low, or unclear risk of bias.
2.5. Statistical analyses
Metaanalysis of the selected studies with a continuous measure was performed with R 3.1.2 statistical software (R Foundation for Statistical Computing, Vienna, Austria), Cochrane Review Manager (RevMan version 5.3; The Cochrane Collaboration, Oxford, England), Comprehensive Meta-Analysis software (version 2.0, Biostat, Inc., Englewood, NJ). Subjective voice scores presented by continuous variables were standardized as mean standard differences at 1 day, 2 days, and more than 7 days. Hedge's g and standard errors were determined for each primary outcome measure.[14] The I2 statistic was employed to quantify heterogeneity, with I2 > 50% representing substantial heterogeneity, 30% ≤ I2 ≤ 50% representing moderate heterogeneity, and I2 < 30% representing low heterogeneity.[15,16] A P-value of the Q statistic that was less than .10 was considered significant. Egger test and funnel plots were applied as visual aids to detect publication bias.[17] Duval and Tweedie proposed a trim and fill method to compensate for missing studies and to correct for overall effect size regarding publication bias; we applied this method in our study.[18,19] We generated a forest plot using the random-effects model to show both random variation within the studies and variation among studies.
3. Results
3.1. Search results
Initial screening of the titles and abstracts for relevance resulted in exclusion of 838 studies that did not meet our inclusion criteria. Duplicate records of 8 articles were also excluded. Out of 874 articles examined in detail, 28 articles that reported the effects of dexamethasone on voice quality score after thyroidectomy were identified. After reviewing the full text, 24 publications were excluded because they failed to meet our eligibility criteria. These articles were excluded due to lack of data or statistics that precluded metaanalysis (N = 9), no control group (N = 10), written in a language other than English (N = 4), review article (N = 1), and duplicated data (N = 1). Thus, 4 articles were included in our quantitative analysis (Tables 1 and 2).[2,7–9] A PRISMA diagram of the study selection progress and main reasons for exclusion are presented in Fig. 1.
Table 1.
Subjective voice outcome for included studies.
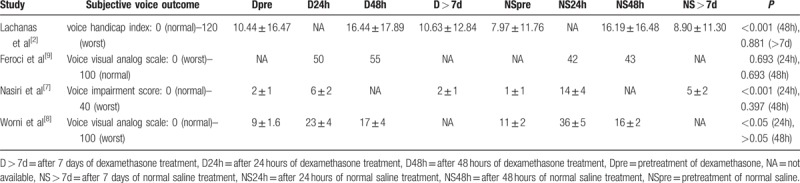
Table 2.
Details of included studies.
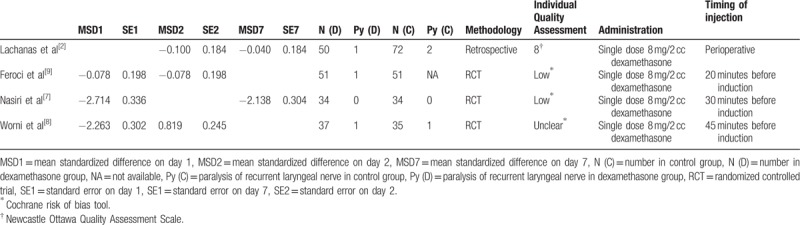
Figure 1.
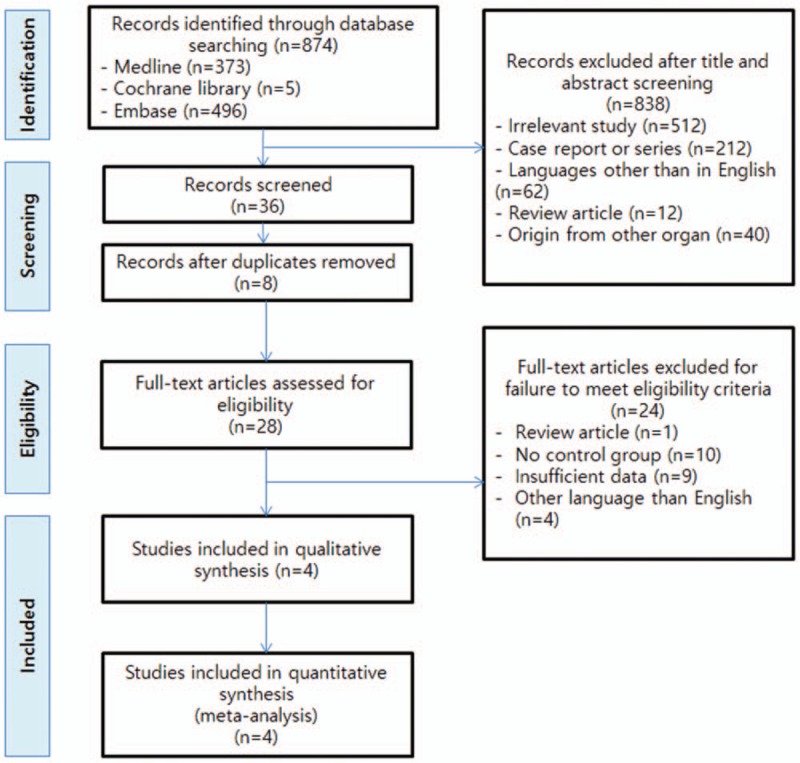
Flow chart of the study literature search (n = number of studies).
3.2. Overall metaanalysis results
Voice outcomes are measure by voice handicap index,[2] voice visual analog scale,[8,9] and voice impairment score.[7] Before obtaining the total effect size, it was necessary to unify the scales for different voices for each study. We postulated the scale between the minimum and maximal range was equivalent in each study. In the Worni and Feroci's study, we used Graph Data Extractor (version 0.0.0.1, Dr A J Matthews) to obtain the mean and standard error of voice outcomes.[8,9] We converted the Feroci's score reversely, because only the Feroci's study was in the opposite order[9]; Converted Feroci's scale = 100 – original Feroci's scale. We obtained the data of Nasiri's study by personal contact.
We used a random effect model considering the variation between and within studies. Analysis of voice quality scores across the first postoperative day revealed a standard mean difference of −1.66 [95% CI, −2.93 to −0.39, P < .05] with substantial heterogeneity (I2 = 97%) (Fig. 2). Analysis of voice quality scores across the second postoperative day showed a standard mean difference of 0.21 [95% CI, −1.04 to 1.46, P > .05] with substantial heterogeneity (I2 = 81%). Analysis of voice quality scores 7 and more days postoperatively showed a standard mean difference of −1.06 [95% CI, −2.61 to 0.48, P > .05] with substantial heterogeneity (I2 = 97%). Total analysis of voice quality scores revealed a standard mean difference of −0.80 [95% CI, −1.54 to −0.05] with substantial heterogeneity (I2 = 95%).
Figure 2.
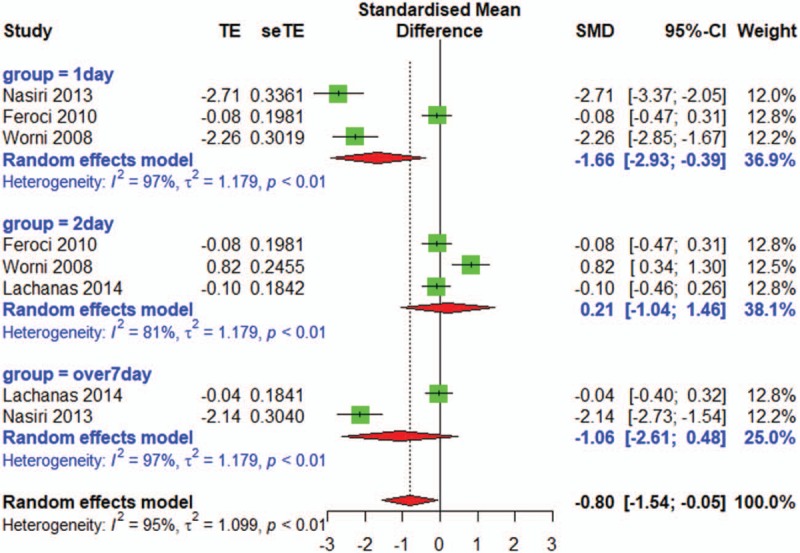
Forest plot shows an effect of single dose dexamethasone on voice quality after thyroidectomy (subgroup; on day 1, on day 2, after day 7).
3.3. Publication bias
To analyze heterogeneity in voice scores, we used a funnel plot (Fig. 3A). The funnel plot showed asymmetry, thus the publication bias existed. We used Duval and Tweedie's trim and fill method to adjust for potentially unpublished reports; this resulted in a significant change in the standardized mean difference (SMD: −0.49, 95% CI [−1.28 to 0.31], P = .23) (Fig. 3B).
Figure 3.
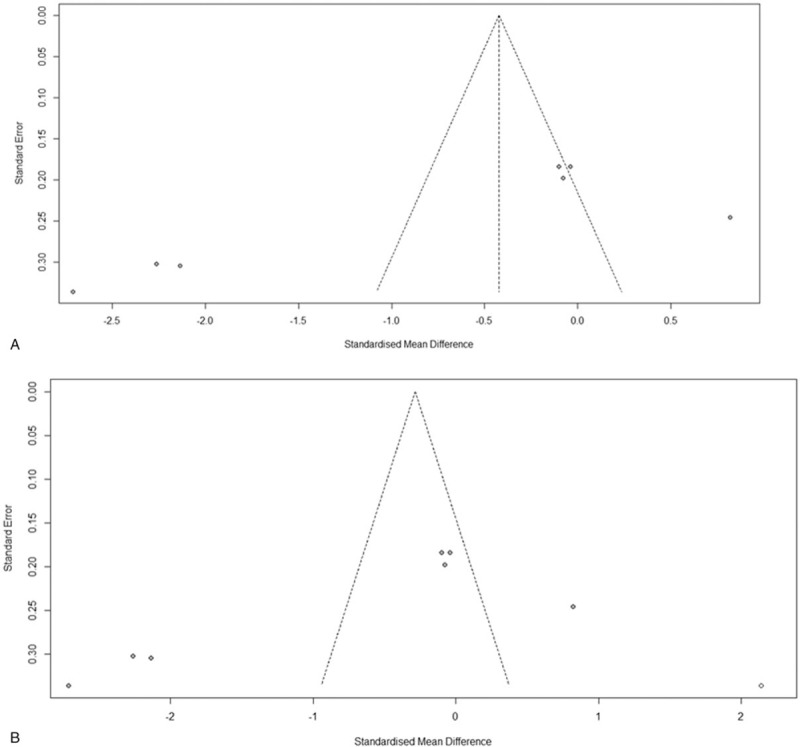
Funnel plot. (A) In the funnel plot, the studies were spread under the line of the 95% CI except 1 outlier study. (B) Duval's trim and fill method estimated the presence of 1 potentially unreported cohorts. After these cohorts were filled, the pooled RR resulted in a significant change in the standardized mean difference (SMD: −0.49, 95% CI [−1.28 to 0.31], P = .23).
3.4. Sensitivity analysis
A sensitivity analysis to evaluate the stability of the results was performed by removing each study one by one. The pooled risk ratio in the overall comparison and the stratified analyses did not change significantly, indicating a stable and robust outcome (Fig. 4B). To find outliers in the funnel plot, we also constructed a Baujat plot, which is a scatter plot that shows heterogeneity and standardized differences simultaneously (Fig. 4A).[20]
Figure 4.
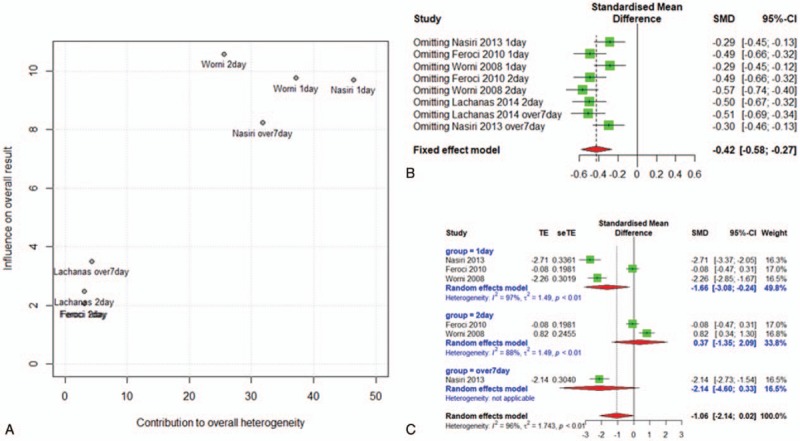
(A) A Baujat plot showed Nasiri and Worni et al's study (2008) as an outlier study. (B) Sensitivity analysis. The pooled risk ratio in the overall comparison and the stratified analyses were not significantly changed, indicating a stable and robust outcome. (C) A RCT group showed similar results to the overall metaanalysis.
3.5. Analysis of RCTs
Two methodologies are presented in this metaanalysis, RCTs (3 studies) and retrospective studies (1 study). When the only retrospective study was excluded, we can make a group of 3 RCTs. This RCT group showed similar results to the overall metaanalysis (postoperative day 1: SMD −1.66 [95% CI, −3.08 to −0.24, P < .05], postoperative day 2: SMD 0.37 [95% CI, −1.35 to 2.09, P > .05], after postoperative day 7: SMD −2.14 [95% CI, −4.60 to 0.33]) (Fig. 4C).
4. Discussion
Preoperative administration of dexamethasone reduces swelling and inflammation after many surgeries including cardiac surgery, orthopedic surgery, endoscopic sinus surgery, and tonsillectomy.[21,22] Dexamethasone is a type of steroid that binds to the glucocorticoid receptor, which is how it exerts its antiinflammatory effects; the activated glucocorticoid receptor complex upregulates the expression of antiinflammatory genes.[23]
Dexamethasone is also effective at treating swallowing impairment, nausea, and vomiting after thyroidectomy.[24,25] Given voice preservation is a major outcome measure after thyroidectomy, we conducted a metaanalysis to the effect of dexamethasone injection on voice quality.
One previous metaanalysis reported no effectiveness of single perioperative dexamethasone to improve voice quality after thyroidectomy.[26] The study included 4 individual studies using separate estimate of τ2 for each subgroup; preoperative, day 1, day 2. However, he did not obtain the total effect size, which is showed as SMD: −0.80 [95% CI, −1.54 to −0.05] from our metaanalysis's result. Without showing the significance of overall effect size, the Cheng's study concluded that the dexamethasone was ineffective to reduce voice dysfunction only through subgroup analysis. One more thing to point out is the method to perform subgroup analysis. In a situation of only a few studies available to perform subgroup analysis like Cheng's and our metaanalysis, the estimate of τ2 within subgroups are usually inexact.[27] It makes more sense to use a common τ2 in these metaanalysis.
We found that the effect of dexamethasone after thyroidectomy differed according to postoperative day. A single dose of dexamethasone prophylactically (8 mg/2 cc) before thyroidectomy reduced nausea, vomiting, pain, and hoarseness. Nasiri et al[7] also reported that single dose administration decreased early postthyroidectomy voice change. On day 1, voice quality after single dexamethasone administration was different from that of the control group (Fig. 2). Of the 4 studies included, 3 were randomized prospective studies where dexamethasone was administrated before induction of anesthesia (20–45 minutes before induction)[7–9] However, on day 2 and after 7 days, the results of single dexamethasone administration were not different from those in the control groups. The half-life of dexamethasone is approximately 36 to 54 hours.[28] Moreover, the wash-out period of dexamethasone is approximately 7 days.[29] Thus, the observational periods of the 4 included studies are reasonable.
A recent study demonstrated that the prophylactic administration of dexamethasone significantly reduced the incidence and severity of postoperative sore throat and vocal fold edema within 1 day after general endotracheal anesthesia.[30] The authors explained that dexamethasone effectively decreases structural injury to the vocal cords caused by endotracheal tubes within 24 hours. Endotracheal intubation, as commonly used in general anesthesia, can lead to edema of the vocal folds, pathologic changes, and nerve damage. The pressure of the cuff causes neuropraxia of the recurrent laryngeal nerve, which results in nerve paralysis.[31] Our metaanalysis showed that a single preoperative dose of dexamethasone effectively decreases edema of vocal folds within 1 day; however, it has no effect on neuropraxia after 1 day. A previous report supported our results, demonstrating that dexamethasone was ineffective for neuropraxia of the inferior alveolar nerve and lingual nerve 24 hours following removal of the mandibular 3rd molar tooth.[32]
Recurrent laryngeal nerve palsy was verified in 6 cases (3 by Lachanas et al, 1 by Feroci et al, and 2 by Worni et al). However, these cases were excluded from voice analysis because these can be a confounding factor.
All of the studies differed from each other in patient population, circumstances, and follow-up length. Therefore, we analyzed heterogeneity to evaluate outliers, and performed a subgroup analysis. A Baujat plot is a simple graphical method to find the study that most strongly influences the overall results and overall heterogeneity. We found that the outlier data were the day 1 results of Nasiri et al and Worni et al[7,8,20] (Fig. 4A). Sensitivity analysis showed that the SMD was robust (−0.29, −0.29, respectively) when the studies of Nasiri et al and Worni et al was omitted (Fig. 4B). The only retrospective study was that of Lachanas et al.[2] When the study of Lachanas et al was omitted, the SMD did not change significantly (Fig. 4B). Subgroup analysis focusing on 3 RCTs showed similar results to the overall metaanalysis, suggesting that a single preoperative dose of dexamethasone has an effect on the first postoperative day; however, these effects disappear after 2 days.
One limitation of the present study was that it included non-RCT studies. However, a metaanalysis including only RCTs was not possible due to the limited number of published RCT studies. Moreover, metaanalyses using observational studies have become widely accepted.[11] Our sensitivity analysis and analysis of RCTs also showed stable and robust outcomes when the observational study was omitted.
5. Conclusion
Our finding that single-dose administration of dexamethasone may improve voice quality, especially on day 1 after thyroidectomy, should be interpreted cautiously. The observed difference in voice quality on day 1 after steroid administration may not translate into a clinically significant difference given the absence of differences between groups at days 2 and >7. Well-designed future clinical studies are needed to overcome the limitations of this metaanalysis and will provide additional clinical evidence regarding the effects of dexamethasone on voice quality after thyroidectomy.
Author contributions
Conceptualization: So Eun Lee.
Data curation: So Eun Lee.
Formal analysis: Jong Seung Kim, Sam Hyun Kwon.
Funding acquisition: Jong Seung Kim, Sam Hyun Kwon.
Investigation: Sam Hyun Kwon.
Methodology: Sam Hyun Kwon.
Project administration: Sam Hyun Kwon.
Resources: Jong Seung Kim, Sam Hyun Kwon.
Software: Jong Seung Kim.
Supervision: Jong Seung Kim.
Validation: Jong Seung Kim.
Visualization: Jong Seung Kim.
Writing – original draft: Jong Seung Kim.
Writing – review & editing: Jong Seung Kim, Sam Hyun Kwon, Eun Jung Lee, Min Hee Lee.
Footnotes
Abbreviations: CI = confidence interval, MOOSE = Meta-analysis of Observational Studies in Epidemiology, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses, RCT = randomized controlled trial, SMDs = standardized mean differences.
Funding: This paper was supported by Fund of Biomedical Research Institute, Chonbuk National University Hospital.
The authors have no conflicts of interest to disclose.
References
- [1].Hong KH, Yang YS, Lee HD, et al. The effect of total thyroidectomy on the speech production. Clin Exp Otorhinolaryngol 2015;8:155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lachanas VA, Exarchos S, Tsiouvaka S, et al. Does perioperative dexamethasone affect voice-related quality of life after thyroidectomy? Eur Arch Otorhinolaryngol 2014;271:3073–6. [DOI] [PubMed] [Google Scholar]
- [3].Kiris M, Muderris T, Yalciner G, et al. Intrapolyp steroid injection for nasal polyposis: randomized trial of safety and efficacy. Laryngoscope 2016;126:1730–5. [DOI] [PubMed] [Google Scholar]
- [4].Mansfield LE. Beclomethasone HFA for the treatment of allergic rhinitis. Expert Opin Pharmacother 2015;16:2849–57. [DOI] [PubMed] [Google Scholar]
- [5].Ingle JW, Helou LB, Li NY, et al. Role of steroids in acute phonotrauma: a basic science investigation. Laryngoscope 2014;124:921–7. [DOI] [PubMed] [Google Scholar]
- [6].Wang CT, Lai MS, Hsiao TY. Comprehensive outcome researches of intralesional steroid injection on benign vocal fold lesions. J Voice 2015;29:578–87. [DOI] [PubMed] [Google Scholar]
- [7].Nasiri S, Shafag S, Khorgami Z, et al. Does corticosteroid have any beneficial effect on voice change after thyroidectomy? Am Surg 2013;79:1258–62. [PubMed] [Google Scholar]
- [8].Worni M, Schudel HH, Seifert E, et al. Randomized controlled trial on single dose steroid before thyroidectomy for benign disease to improve postoperative nausea, pain, and vocal function. Ann Surg 2008;248:1060–6. [DOI] [PubMed] [Google Scholar]
- [9].Feroci F, Rettori M, Borrelli A, et al. Dexamethasone prophylaxis before thyroidectomy to reduce postoperative nausea, pain, and vocal dysfunction: a randomized clinical controlled trial. Head Neck 2011;33:840–6. [DOI] [PubMed] [Google Scholar]
- [10].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009;62:e1–34. [DOI] [PubMed] [Google Scholar]
- [11].Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- [12].Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. [DOI] [PubMed] [Google Scholar]
- [13].Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hedges LV. Distribution theory for Glass's estimator of effect size and related estimators. J Educ Behav Stat 1981;6:107–28. [Google Scholar]
- [15].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [17].Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med 2006;25:3443–57. [DOI] [PubMed] [Google Scholar]
- [18].Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000;56:455–63. [DOI] [PubMed] [Google Scholar]
- [19].Sutton AJ, Duval SJ, Tweedie RL, et al. Empirical assessment of effect of publication bias on meta-analyses. BMJ 2000;320:1574–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Baujat B, Mahe C, Pignon JP, et al. A graphical method for exploring heterogeneity in meta-analyses: application to a meta-analysis of 65 trials. Stat Med 2002;21:2641–52. [DOI] [PubMed] [Google Scholar]
- [21].Ghiasi A, Shafiee A, Salehi Omran A, et al. The effect of continuous low dose methylprednisolone infusion on inflammatory parameters in patients undergoing coronary artery bypass graft surgery: a randomized-controlled clinical trial. Acta Med Iran 2015;53:104–11. [PubMed] [Google Scholar]
- [22].Altamimi S, Robertson G, Jastaniah W, et al. Single-dose oral dexamethasone in the emergency management of children with exacerbations of mild to moderate asthma. Pediatr Emerg Care 2006;22:786–93. [DOI] [PubMed] [Google Scholar]
- [23].Park SK, Kim J, Kim JM, et al. Effects of oral prednisolone on recovery after tonsillectomy. Laryngoscope 2015;125:111–7. [DOI] [PubMed] [Google Scholar]
- [24].Exarchos ST, Lachanas VA, Tsiouvaka S, et al. The impact of perioperative dexamethasone on swallowing impairment score after thyroidectomy. A retrospective study of 118 total thyroidectomies. Clin Otolaryngol 2016;41:615–8. [DOI] [PubMed] [Google Scholar]
- [25].Varma SL, Trivedi JK, Anand M, et al. Post dexamethasone plasma cortisol levels in depressives treated with imipramine and electroconvulsive therapy. Indian J Psychiatry 1989;31:78–82. [PMC free article] [PubMed] [Google Scholar]
- [26].Cheng SP, Liu TP, Yang PS, et al. Effect of perioperative dexamethasone on subjective voice quality after thyroidectomy: a meta-analysis and systematic review. Langenbecks Arch Surg 2015;400:929–36. [DOI] [PubMed] [Google Scholar]
- [27].Borenstein M, Hedges LV, Higgins JP, et al. Introduction to Meta-Analysis. Chichester, UK: Wiley; 2009. [Google Scholar]
- [28].Cross KP, Paul RI, Goldman RD. Single-dose dexamethasone for mild-to-moderate asthma exacerbations: effective, easy, and acceptable. Can Fam Physician 2011;57:1134–6. [PMC free article] [PubMed] [Google Scholar]
- [29].Ghulam R, Trivedi JK, Singh N, et al. Post dexamethasone plasma cortisol levels as indicator of tricyclic response in major depression. Indian J Psychiatry 1990;32:351–5. [PMC free article] [PubMed] [Google Scholar]
- [30].Park SH, Han SH, Do SH, et al. Prophylactic dexamethasone decreases the incidence of sore throat and hoarseness after tracheal extubation with a double-lumen endobronchial tube. Anesth Analg 2008;107:1814–8. [DOI] [PubMed] [Google Scholar]
- [31].Eidi M, Seyed Toutounchi SJ, Kolahduzan K, et al. Comparing the effect of dexamethasone before and after tracheal intubation on sore throat after tympanoplasty surgery: a randomized controlled trial. Iran J Otorhinolaryngol 2014;26:89–98. [PMC free article] [PubMed] [Google Scholar]
- [32].Von Arx DP, Simpson MT. The effect of dexamethasone on neurapraxia following third molar surgery. Br J Oral Maxillofac Surg 1989;27:477–80. [DOI] [PubMed] [Google Scholar]


