Supplemental Digital Content is available in the text
Keywords: heart failure, midregional sequence of the N-terminal pro-A-type natriuretic peptide, N-terminal pro-B-type natriuretic peptide, preserved ejection fraction
Abstract
Objectives:
To explore that if mid-regional sequence of pro-A-type natriuretic peptide (MR-proANP) may have a good value of diagnosis in heart failure with preserved ejection fraction (HFpEF) compared with N-terminal pro-B-type natriuretic peptide (NT-proBNP).
Methods:
Participants with cardiovascular disease who were enrolled in this study were divided into the nonheart failure (non-HF) group (n = 75), HFpEF group (n = 65), and HF with reduced ejection fraction (HFrEF) group (n = 50). The MR-proANP and NT-proBNP levels in plasma from all patients were measured by enzyme-linked immunosorbent assay.
Results:
The plasma levels of MR-proANP and NT-proBNP in HFpEF and HFrEF groups were higher than those in non-HF group (P < .05). MR-proANP levels were significantly different (P < .05) in different New York Heart Association class patients with HFpEF. In the diagnostic analysis area under the curve of MR-proANP (0.844) was higher than that of NT-proBNP (0.518, P < .001). The left atrial volume index in the HFrEF group was higher than HFpEF group (P < .05); however, both of these groups had a higher index than non-HF group (P < .05).
Conclusion:
Results indicated that MR-proANP may be more sensitive and specific than NT-proBNP in diagnosing HFpEF. It may be used as a potential diagnostic biomarker in patients with HFpEF.
1. Introduction
Heart failure (HF) with preserved ejection fraction (HFpEF) is a common clinical syndrome that accounts for nearly half of all HF patients[1,2] and has a prognosis similar to patients with reduced ejection fraction (EF) heart failure with reduced ejection fraction (HFrEF). Compared to HFrEF which is defined as an EF <50%, HFpEF is defined as an EF ≥50%.[3] Conventional echocardiography for the evaluation of cardiac structure and diastolic function has some limitations,[4,5] and invasive examinations are inconvenient and expensive. Considering the complexity and diversity of the pathophysiological mechanisms as well as the heterogeneity of patients with HFpEF,[6] it has been challenging to identify an objective and reliable biomarker to make a diagnosis and evaluate the prognosis.[7]
Currently, natriuretic peptides are the criterion standard of biomarkers in HF and have been extensively investigated in various clinical settings.[8,9] B-type natriuretic peptide (BNP) mainly originates from the left ventricle in both healthy adult humans and patients with left ventricular (LV) dysfunction[10,11] and is de novo synthesized in response to ventricular stretch due to pressure and volume overload.[12] N-terminal pro-B-type natriuretic peptide (NT-proBNP) is a representative cardiac biomarkers that is well-correlated with LV end-diastolic pressure and wall pressure; it not only has high sensitivity and specificity for a differential diagnosis of HF in patients with acute dyspnoea, but also has important value in terms of the diagnosis, evaluation, and prognosis in patients with either acute or chronic HF.[13,14] However, the exact role of NT-proBNP in clinically identifying HFpEF has been less studied. Atrial natriuretic polypeptide (ANP) is mainly secreted from the atria of healthy adult humans and from the left ventricle of patients with LV dysfunction. The clinical application of ANP is limited because of its extremely short half-life; however, its precursor NT-proANP is more stable in plasma and has a longer half-life, but is insufficient for immunoassay detection due to the production of various subfragments. Recently, a midregional sequence of pro-A-type natriuretic peptide (MR-proANP), which is an intermediate of the natriuretic peptides and is more stable, was successfully used in the clinic as a biomarker of the prognosis and diagnosis of acute HF.[15–18] However, whether MR-proANP has potential clinical utility in identifying the response to atrial pressure overload and LV diastolic dysfunction is unknown.
NT-proBNP specifically responds to ventricular pressure. MR-proANP is one of the best indicators of atrial pressure.[19–21] The aim of this study was to compare the diagnostic value of MR-proANP with NT-proBNP in patients with HFrEF and HFpEF as well as whether MR-proANP could increase or even exceed the diagnostic value of NT-proBNP in patients with HFpEF.
2. Methods
2.1. Study group
Participants with cardiovascular disease were enrolled in the study and classified into the following 3 groups: HFpEF group (66 patients), HFrEF group (50 patients), and non-HF group (76 patients). The main inclusion criteria of HFpEF were the presence of HF symptoms, New York Heart Association (NYHA) class II-IV, an LV ejection fraction (LVEF) >50%, an E/A ratio <1, and comorbidity of randomized and well-controlled underlying diseases that are risk factors of HFpEF [e.g., hypertension (HTN), coronary artery disease, diabetes). The criteria of HFrEF were the presence of HF symptoms and an LVEF <50%.[22] The non-HF group consisted of age- and sex-matched patients who were hospitalized due to cardiovascular disease but had no symptoms of HF. The study complies with the Declaration of Helsinki and Ethics Committee of First Affiliated Hospital of Chongqing Medical University.
2.2. Echocardiograph study
Transthoracic echocardiography was performed by a digital Acuson Sequoia C256 device with a 2.3 to 3.5 MHz probe (Siemens, Munich, Germany). The main parameters evaluated were LVEF, LAEDD (left atrial end-diastolic diameter), LVEDD (left ventricular end-diastolic diameter), LAVI (left atrial volume index), and E/A ratio.
2.3. Blood sampling and Assays
Fasting venous blood samples were obtained after admission and before administration of therapy. Blood samples were immediately centrifuged at 3000 rpm at 4°C, and sample aliquots were stored at −80°C for further analysis.
2.4. Measurement of plasma MR-proANP, ANP, and NT-proBNP levels
Plasma MR-proANP levels were measured by using MR-proANP ELISA Kit provided by MyBioSource (MyBioSource Inc, San Diego, CA). Briefly, serial dilutions (39–2500 pmol/L) of recombinant MR-proANP were made. The data were analyzed using ELISA CAL software by fitting 4-parameter logistic transformation of standard recombinant MR-proANP. Plasma levels of NT-proBNP were measured with specific assay kits provided by Cusabio Biotech Co, Ltd (Wuhan, China). Briefly, serial dilutions (12.5–200 ng/L) of recombinant NT-proBNP were made. The data were analyzed using Curve Expert 1.3 software by fitting a 4-parameter logistic transformation of standard recombinant NT-proBNP.
2.5. Statistical analysis
All values are reported as the mean ± SD, medians (interquartile range), or percentages. Differences in characteristics among the subjects in each group were assessed using χ2 test for dichotomous variables. Normality testing of the data used Kolmogorov-Smirnov Z method. Comparison of the MR-proANP and NT-proBNP levels in the different HF groups was performed using Kruskal-Wallis H (K) method. Comparison of the MR-proANP levels among different HF groups in LAVI and NYHA grade were performed with analysis of variance (ANOVA) method. The correlation of MR-proANP and NT-proBNP with other variables was calculated using the Spearman correlation. Comparison of the diagnostic capabilities of MR-proANP and NT-proBNP with regard to HFpEF was conducted by using a receiver operating characteristic curve (ROC) curve.
3. Results
3.1. Clinical characteristics
The baseline characteristics of participants are listed in Table 1. Among 3 groups, there was no difference in age, sex, body mass index, and percentage of patients with HTN, diabetes (DM), atrial fibrillation (AF), or coronary heart disease (CHD) (P > .05). There was a lower level of estimated glomerular filtration rate (eGFR) in the HFrEF group than that in the non-HF group, but there was no significant difference among 3 groups. The echocardiogram data, including the LVEDD, LAEDD, and mitral early diastolic flow speed and late diastolic flow speed, showed no difference.
Table 1.
Patient characteristics among 3 groups.
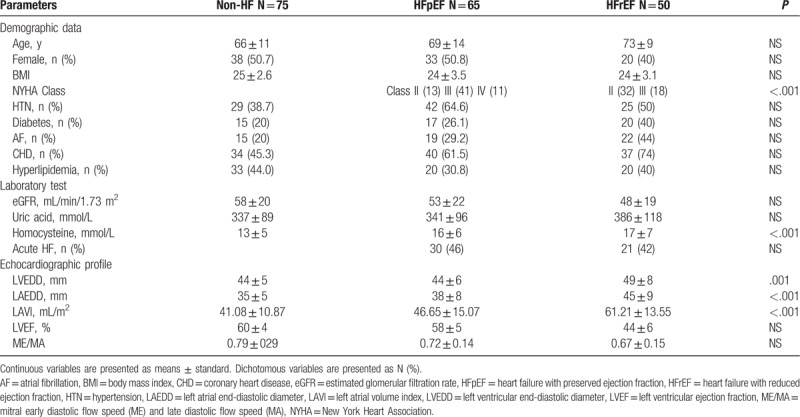
3.2. LAVI in different groups
To examine the relationship of the LAVI in different groups, we used ANOVA to compare differences of LAVI among 3 groups (Table 1). The LAVI in non-HF, HFpEF, and HFrEF groups were significantly different (P < .05). Among them, LAVI in HFrEF group was higher than HFpEF group (P < .05), and both values were higher than non-HF group (P < .05).
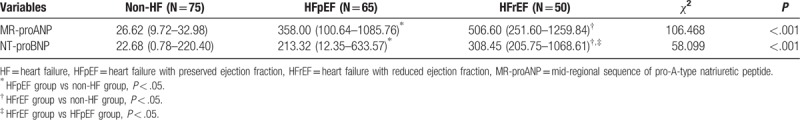
3.3. Plasma levels of MR-proANP and NT-proBNP among different groups
Table 2 shows that plasma levels of MR-proANP and NT-proBNP in the non-HF, HFpEF, and HFrEF groups were significantly different (P < .05). Plasma levels of MR-proANP in HFpEF and HFrEF groups were higher than those in non-HF group, but differences between HFpEF and HFrEF groups had no difference (P > .05). NT-proBNP levels of HFrEF group were higher than HFpEF group (P < .05), and both were higher than non-HF group (P < .05).
Table 2.
Comparison of mid-regional sequence of pro-A-type natriuretic peptide and N-terminal pro-B-type natriuretic peptide among 3 groups.
3.4. Correlation of MR-proANP and NT-proBNP with other variables
We used Spearman correlation to analyze relationship between either MR-proANP or NT-proBNP with other variables. The results are shown in Table S1. It was demonstrated that the correlation of MR-proANP with eGFR, CHD, DM, HTN, or AF was not significant. MR-proANP showed a weak positive correlation with age and LAVI (r = 0.208, P = .008; r = 0.105, P = .047, respectively). The correlations of NT-proBNP with age, eGFR, CHD, HTN, or AF were not significant.
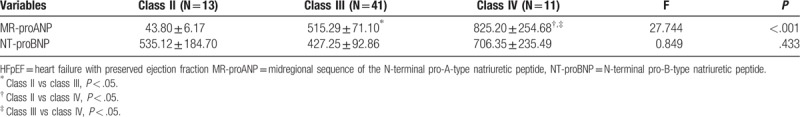
3.5. Correlation of different NYHA class with MR-proANP in HFpEF
To explore relationship between severity of HF symptoms and plasma levels of MR-proANP in patients with HFpEF, ANOVA is used to compare difference of NYHA class with MR-proANP in Table 3. The analysis showed that the MR-proANP levels among NYHA class II, III, and IV were significantly different. The MR-proANP level of class III was significantly higher than class II (P < .05), but lower than class IV (P < .05). The NT-proBNP levels of class II, III, and IV were not significantly different (P > .05).
Table 3.
Comparison of different New York Heart Association class with either mid-regional sequence of pro-A-type natriuretic peptide or N-terminal pro-B-type natriuretic peptide in Heart failure with preserved ejection fraction group.
3.6. The diagnostic capabilities of MR-proANP and NT-proBNP in HFpEF
In order to compare diagnostic capabilities of MR-proANP and NT-proBNP on HFpEF, ROC was applied (Table 4). Figure 1 shows that area under the curve of MR-proANP was higher than that of NT-proBNP; thus, MR-proANP may be superior to NT-proBNP as HFpEF diagnostic indicator. The asymptotic significance of NT-proBNP was 0.698, which was greater than 0.05. Thus, NT-proBNP may not be a meaningful diagnosis indicator of HFpEF. The asymptotic significance of MR-proANP was <0.001. Therefore, MR-proANP may be a specific diagnostic biomarker for HFpEF.
Table 4.
Area under the curve of mid-regional sequence of pro-A-type natriuretic peptide and N-terminal pro-B-type natriuretic peptide in heart failure with preserved ejection fraction group.
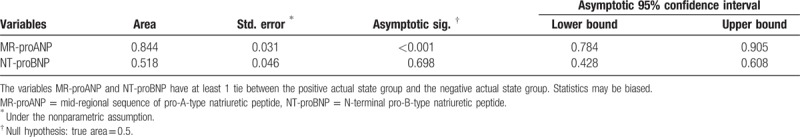
Figure 1.
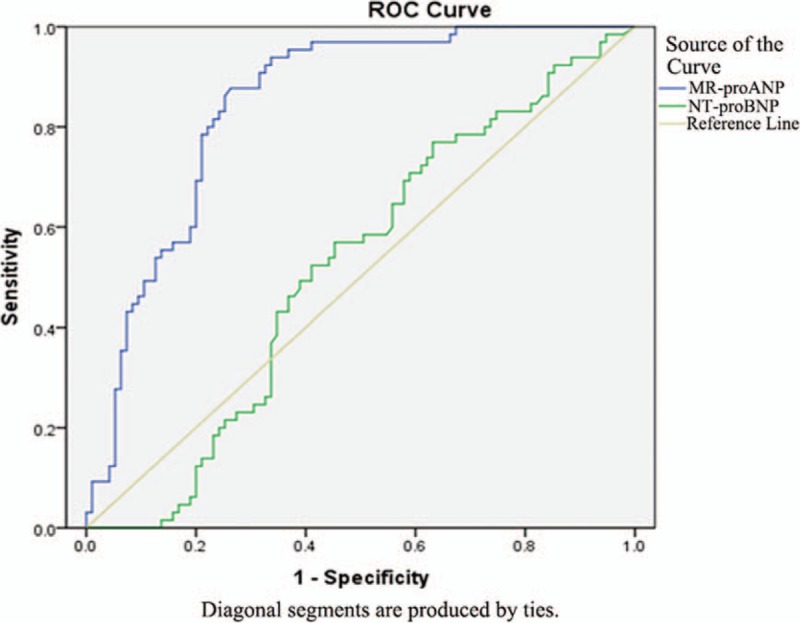
ROC was used for comparison of MR-proANP and NT-proBNP in patients with HFpEF. HFpEF = heart failure with preserved ejection fraction, MR-proANP = mid-regional sequence of pro-A-type natriuretic peptide, NT-proBNP = N-terminal pro-B-type natriuretic peptide, ROC = Receiver operating characteristic curve.
4. Discussion
For the first time, diagnostic and assessment values of MR-proANP and NT-proBNP were compared in patients with HFrEF and HFpEF, and main findings were as follows: plasma levels of MR-proANP and NT-proBNP in patients with chronic HF were significantly higher than those in patients without HF; plasma level of MR-proANP was positively correlated with NYHA class in HFpEF patients and also had a good correlation with age and LAVI, but plasma level of NT-proBNP had no correlation; and plasma MR-proANP may be superior to plasma NT-proBNP as a diagnostic biomarker for patients with HFpEF.
It is generally believed that the pathogenesis of HFpEF is mainly involved in LV active diastolic abnormalities and increased LV stiffness, leading to limited LV filling and an elevated LV end-diastolic pressure.[23] The neuroendocrine hormone response also presented significantly increased natriuretic peptide levels. More importantly, recent studies suggested that atrial structure and functional change could play a primary role in the pathogenesis of HFpEF rather than just a consequence of LV systolic function failure in HFrEF patients.[24–26] Left atrial (LA) enlargement, atrial compliance decrease, loss of atrial synchronization, and increased atrial volume load were closely related to reduced LV diastolic function. In particular, the LA volume and LA pressure, both of which theoretically mediated atrial ANP secretion, were direct indicators of LV diastolic dysfunction.
NT-proBNP has high sensitivity and specificity for differential diagnosis of dyspnoea in patients with acute HF, has become one of the most common classical biomarkers for diagnosis and management of HF, and has been recommended by many international guidelines.[3,22] However, several factors such as anemia, advanced age, renal insufficiency, and infection can affect clinical judgment, and previous studies specific to HFpEF patients have been inadequate.[27,28] Meanwhile, ANP secreted by atrial myocytes react to atrial stretch and volume overload, but its application as a biomarker is highly limited due to its extremely short half-life. Interestingly, NT-proANP (as a precursor of ANP), despite its high stability and longer half-life in plasma, has no easily measured biological activity and cannot be widely used in clinical practice due to some factors.
Recent studies found that MR-proANP, which was derived from the intermediate portion of NT-proANP protein after its degradation mainly of the N- and C-termini, was more stable and has a longer half-life. Therefore, in response to changes in LA pressure and LV diastolic dysfunction, NT-proANP might have a better value.[29–31] Maisel et al[32] included 1641 patients with acute dyspnoea, and results showed that diagnostic value of MR-proANP (120 pmol/L or higher) in acute HF was not inferior to NT-proBNP (100 pg/mL or higher), especially for HF patients who did not present diagnostic NT-proBNP values. In fact, most previous studies focused on patients with either acute or chronic HF, including HFpEF and HFrEF patients, and rather than concentrating on directly comparing these 2 groups.[33–35] Our results showed that patients with chronic HF had higher plasma levels of MR-proANP and NT-proBNP compared to those in patients without HF. Particularly, MR-proANP and NT-proBNP had good correlations with NYHA class in both HFpEF and HFrEF patients. In addition, diagnostic curve analysis showed that plasma level of MR-proANP for HFpEF patients may be superior to the NT-proBNP levels with better sensitivity and specificity (area under the curve: 0.844).
Recently, 1 prospective study conducted by Bakkestrøm et al[36] aimed to assess changes in the LA volume early after myocardial infarction in 62 patients with an LVEF ≥45%. Based on the relationship between invasive hemodynamics and natriuretic peptides, LA remodeling was characterized by a lower and higher MR-proANP levels (4 months, 175 ± 48 vs 129 ± 56 pg/L, P = .002). Accordingly, our study showed that LAVI in all patients with HF was higher than that in patients without HF, but correlation analysis suggested that plasma levels of MR-proANP in HFpEF group had a strong correlation with age and LAVI. Therefore, our results also demonstrated that MR-proANP was an indicator of atrial volume load.
Currently, several clinical studies have shown that many factors such as age, obesity, chronic kidney disease, female sex, and HTN were independent risk factors of HFpEF, all of which could play an important role in pathogenesis and progression of HFpEF.[37–40] In this study, both age and LAVI showed significantly positive correlations with HFpEF, but there was no significant correlation with HFpEF and CKD, female sex, or HTN, which might be attributed to small sample size of study. In the early stages of HF, the pressure in the atria is gradually increasing, and the tension in the atria is more susceptible to stress than in the ventricle. Therefore, ANP, which is a response to atrial tension, is more sensitive than BNP in the early stage of HF, which may be of value in judging patients in the gray area of HF. In this study, there was a significant difference in MR-proANP of different NYHA class patients with HFpEF, and there was no difference in NT-proBNP, suggesting that MR-proANP may be more sensitive than NT-proBNP in early diagnosis of HF.
5. Conclusion
In summary, our study demonstrated that plasma level of MR-proANP was significantly elevated in patients with HF and had more sensitivity and specificity in diagnosing patients with HFpEF. Moreover, as a strong indicator of atrial volume overload and LV diastolic dysfunction for those HFpEF patients, plasma level of MR-proANP may be superior to NT-proBNP levels in terms of diagnostic value.
5.1. Limitations
First, this study was limited to a single center and had a small number of patients, especially in HFrEF group. Second, this study used only echocardiography and E/E’ ratio is excluded because of the study design. Furthermore, there was lack of any invasive measurement of left ventricular diastolic function. Finally, it would be more accurate to assess cardiac function by using the 6-minute walk test and treadmill exercise test in combination with NYHA class.
Author contributions
Conceptualization: Kun Cui, Wei Huang, Han Lei.
Data curation: Kun Cui, Wei Huang, Han Lei.
Formal analysis: Wei Huang, Han Lei.
Funding acquisition: Kun Cui, Han Lei.
Investigation: Wei Huang, Han Lei.
Methodology: Wei Huang, Han Lei.
Project administration: Kun Cui, Wei Huang, Jinqi Fan, Han Lei.
Resources: Jinqi Fan, Han Lei.
Software: Kun Cui, Jinqi Fan, Han Lei.
Supervision: Kun Cui, Jinqi Fan, Han Lei.
Validation: Kun Cui, Han Lei.
Visualization: Han Lei.
Writing – original draft: Kun Cui, Jinqi Fan, Han Lei.
Writing – review and editing: Jinqi Fan, Han Lei.
Supplementary Material
Footnotes
Abbreviations: AF = atrial fibrillation, ANP = atrial natriuretic polypeptide, ANOVA = analysis of variance, BMI = body mass index, BNP = B-type natriuretic peptide, CHD = coronary heart disease, DM = diabetes, EF = ejection fraction, eGFR = estimated glomerular filtration rate, HF = heart failure, HFpEF = heart failure with preserved ejection fraction, HFrEF = heart failure with reduced ejection fraction, HTN = hypertension, LA = left atrial, LAEDD = left atrial end-diastolic diameter, LAVI = left atrial volume index, LV = left ventricular, LVEDD = left ventricular end-diastolic diameter, LVEF = LV ejection fraction, MR-proANP = midregional sequence of pro-A-type natriuretic peptide, NT-proBNP = N-terminal pro-B-type natriuretic peptide, ROC = receiver operating characteristic curve.
Ethics approval and consent to participate: This study was approved by Ethics Committee of The First Affiliated Hospital of Chongqing Medical University Participants have provided their written informed consent to participate in this study.
Funding: This work was sponsored by Key Projects of Chongqing General Hospital and Under (Grant No. Y2016ZDXM02).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Ceia F, Fonseca C, Mota T, et al. Prevalence of chronic heart failure in Southwestern Europe: the EPICA study. Eur J Heart Fail 2002;4:531–9. [DOI] [PubMed] [Google Scholar]
- [2].Van Riet EE, Hoes AW, Limburg A, et al. Prevalence of unrecognized heart failure in older persons with shortness of breath on exertion. Eur J Heart Fail 2014;16:772–7. [DOI] [PubMed] [Google Scholar]
- [3].Yancy CW, Jessup M, Bozkurt B, et al. ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;128:1810–52. [DOI] [PubMed] [Google Scholar]
- [4].Bytyçi I, Bajraktari G. Left atrial changes in early stages of heart failure with preserved ejection fraction. Echocardiography 2016;33:1479. [DOI] [PubMed] [Google Scholar]
- [5].Omar AM, Bansal M, Sengupta PP. Advances in echocardiographic imaging in heart failure with reduced and preserved ejection fraction. Circ Res 2016;119:357–74. [DOI] [PubMed] [Google Scholar]
- [6].Argulian E, Messerli FH. Misconceptions and facts about ’diastolic’ heart failure. Am J Med 2014;127:1144–7. [DOI] [PubMed] [Google Scholar]
- [7].Meijers WC, Van der Velde AR, De Boer RA. Biomarkers in heart failure with preserved ejection fraction. Neth Heart J 2016;24:252–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ibrahim N, Januzzi JL. The potential role of natriuretic peptides and other biomarkers in heart failure diagnosis, prognosis and management. Expert Rev Cardiovasc Ther 2015;13:1017–30. [DOI] [PubMed] [Google Scholar]
- [9].Gaggin HK, Jr, Januzzi JL., Jr Natriuretic peptides in heart failure and acute coronary syndrome. Clin Lab Med 2014;34:43–58. [DOI] [PubMed] [Google Scholar]
- [10].O’Hanlon R, O'Shea P, Ledwidge M, et al. The biologic variability of B-type natriuretic peptide and N-terminal Pro-B-type natriuretic peptide in stable heart failure patients. J Card Fail 2007;13:50–5. [DOI] [PubMed] [Google Scholar]
- [11].Christenson RH, Azzazy HME, Duh SH, et al. Impact of increased body mass index on accuracy of B-type natriuretic peptide (BNP) and N-terminal proBNP for diagnosis of decompensated heart failure and prediction of all-cause mortality. Clin Chem 2010;56:633–41. [DOI] [PubMed] [Google Scholar]
- [12].Woods RL. Cardioprotective functions of atrial natriuretic peptide and B-type natriuretic peptide: a brief review. Clin Exp Pharmacol Physiol 2004;31:791–4. [DOI] [PubMed] [Google Scholar]
- [13].Madamanchi C, Alhosaini H, Sumida A, et al. Obesity and natriuretic peptides, BNP and NT-proBNP: mechanisms and diagnostic implications for heart failure. Int J Cardiol 2014;176:611–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Troughton R, Michael Felker G, Jr, Januzzi JL., Jr Natriuretic peptide-guided heart failure management. Eur Heart J 2014;35:16–24. [DOI] [PubMed] [Google Scholar]
- [15].Wild PS, Schnabel RB, Lubos E, et al. Midregional proadrenomedullin for prediction of cardiovascular events in coronary artery disease: results from the AtheroGene study. Clin Chem 2011;58:226–36. [DOI] [PubMed] [Google Scholar]
- [16].Tzikas S, Keller T, Ojeda FM, et al. MR-proANP and MR-proADM for risk stratification of patients with acute chest pain. Heart 2013;99:388–95. [DOI] [PubMed] [Google Scholar]
- [17].Hausfater P, Claessens YE, Martinage A, et al. Prognostic value of PCT, Copeptin, MR-proADM, MR-proANP and CT-proET-1 for severe acute dyspnea in the emergency department: the BIODINER study. Biomarkers 2017;22:28–34. [DOI] [PubMed] [Google Scholar]
- [18].Francis GS, Felker GM, Tang WH. A test in context: critical evaluation of natriuretic peptide testing in heart failure. J Am Coll Cardiol 2016;67:331–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].De Vito P. Atrial natriuretic peptide: an old hormone or a new cytokine? Peptides 2014;58:108–16. [DOI] [PubMed] [Google Scholar]
- [20].Morgenthaler NG, Struck J, Thomas B, et al. Immunoluminometric assay for the midregion of pro-atrial natriuretic peptide in human plasma. Clin Chem 2004;50:234–6. [DOI] [PubMed] [Google Scholar]
- [21].Nishikimi T, Kuwahara K, Nakao K. Current biochemistry, molecular biology, and clinical relevance of natriuretic peptides. J Cardiol 2011;57:131–40. [DOI] [PubMed] [Google Scholar]
- [22].McMurray JJ, Adamopoulos S, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. [Turk Kardiyoloji Dernegi arsivi: Turk Kardiyoloji Derneginin yayin organidir]. Eur Heart J 2015;11:110–10. [PubMed] [Google Scholar]
- [23].Shah SJ, Gheorghiade M. Heart failure with preserved ejection fraction. Expert Rev Cardiovasc Ther 2011;12:743. [DOI] [PubMed] [Google Scholar]
- [24].Welles CC, Ku IA, Kwan DM, et al. Left atrial function predicts heart failure hospitalization in subjects with preserved ejection fraction and coronary heart disease: longitudinal data from the heart and soul study. J Am Coll Cardiol 2011;59:673–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Habibi M, Chahal H, Opdahl A, et al. Association of CMR-measured LA function with heart failure development: results from the MESA study. JACC Cardiovasc Imaging 2014;7:570–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Goette A, Kalman JM, Aguinaga L, et al. EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition, characterisation, and clinical implication. Heart Rhythm 2016;32:247–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Roberts E, Ludman AJ, Dworzynski K, et al. The diagnostic accuracy of the natriuretic peptides in heart failure: systematic review and diagnostic meta-analysis in the acute care setting. BMJ 2015;350:h910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Maisel A, Mueller C, Jr, Adams KA, et al. State of the art: using natriuretic peptide levels in clinical practice. Eur J Heart Fail 2008;10:824–39. [DOI] [PubMed] [Google Scholar]
- [29].Gegenhuber A, Struck J, Dieplinger B, et al. Comparative evaluation of B-type natriuretic peptide, mid-regional pro-A-type natriuretic peptide, mid-regional pro-adrenomedullin, and Copeptin to predict 1-year mortality in patients with acute destabilized heart failure. J Card Fail 2007;13:42–9. [DOI] [PubMed] [Google Scholar]
- [30].Elmas E, Brueckmann M, Lang S, et al. Midregional pro-atrial natriuretic peptide is a useful indicator for the detection of impaired left ventricular function in patients with coronary artery disease. Int J Cardiol 2008;128:244–9. [DOI] [PubMed] [Google Scholar]
- [31].Gegenhuber A, Struck J, Poelz W, et al. Midregional pro-A-type natriuretic peptide measurements for diagnosis of acute destabilized heart failure in short-of-breath patients: comparison with B-type natriuretic peptide (BNP) and amino-terminal proBNP. Clin Chem 2006;52:827–31. [DOI] [PubMed] [Google Scholar]
- [32].Maisel A, Mueller C, Nowak RM, et al. Midregion prohormone adrenomedullin and prognosis in patients presenting with acute dyspnea: results from the BACH (Biomarkers in Acute Heart Failure) trial. J Am Coll Cardiol 2011;58:1057–67. [DOI] [PubMed] [Google Scholar]
- [33].Von Haehling HS, Jankowska EA, Morgenthaler NG, et al. Comparison of midregional pro-atrial natriuretic peptide with N-terminal pro-B-type natriuretic peptide in predicting survival in patients with chronic heart failure. J Am Coll Cardiol 2007;50:1973–80. [DOI] [PubMed] [Google Scholar]
- [34].Shah RV, Truong QA, Gaggin HK, et al. Mid-regional pro-atrial natriuretic peptide and pro-adrenomedullin testing for the diagnostic and prognostic evaluation of patients with acute dyspnoea. Eur Heart J 2012;33:2197–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Serge M, Roberto L, Emanuele C, et al. The predictive value of stable precursor fragments of vasoactive peptides in patients with chronic heart failure: data from the GISSI-heart failure (GISSI-HF) trial. Eur J Heart Fail 2010;12:338–47. [DOI] [PubMed] [Google Scholar]
- [36].Bakkestrøm R, Andersen MJ, Ersbøll M, et al. Early changes in left atrial volume after acute myocardial infarction. Relation to invasive hemodynamics at rest and during exercise. Int J Cardiol 2016;223:717–22. [DOI] [PubMed] [Google Scholar]
- [37].Winter LJMB, Rutten FH, Cramer MJM, et al. High prevalence of previously unknown heart failure and left ventricular dysfunction in patients with type 2 diabetes. Diabetologia 2012;55:2154–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Daniels LB, Clopton P, Potocki M, et al. Influence of age, race, sex, and body mass index on interpretation of midregional pro atrial natriuretic peptide for the diagnosis of acute heart failure: results from the BACH multinational study. Eur J Heart Fail 2012;14:22–31. [DOI] [PubMed] [Google Scholar]
- [39].Magaña-Serrano JA, Almahmeed W, Gomez E, et al. Prevalence of heart failure with preserved ejection fraction in Latin American, Middle Eastern, and North African Regions in the I PREFER study (Identification of Patients With Heart Failure and PREserved Systolic Function: an epidemiological regional study. Am J Cardiol 2011;108:1289–96. [DOI] [PubMed] [Google Scholar]
- [40].Mureddu GF, Agabiti N, Rizzello V, et al. Prevalence of preclinical and clinical heart failure in the elderly. A population-based study in Central Italy. Eur J Heart Fail 2012;14:718–29. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


