Abstract
Background
Delaying or slowing age-related cognitive decline is a national priority. Speed of processing training (SOPT) has been effective in healthy middle aged and older community dwelling adults, but has not been examined among older adults in senior living communities, especially those in assisted living.
Design
We conducted a two-arm, parallel, randomized controlled trial.
Setting
Assisted and independent residence settings in 31 senior living communities.
Participants
351 participants were enrolled who were 55–102 years old.
Intervention
The targeted intervention dose was ten hours of computerized SOPT at baseline, and four hour boosters at both five and eleven months vs. the same targeted intervention dose of solving computerized crossword puzzles for the attention control group.
Measures
Useful Field of View (UFOV) scores and improvements ≥ 0.5 SD (≥ 158.4 ms) were the outcomes. Data collection occurred at baseline, post-training, and six and twelve months. Random effects linear mixed effect models estimated SOPT effects in intention-to-treat complete case and multiple imputation analyses.
Results
Mean age was 81.0 years, 73.8% were women, 76.4% lived alone, and 47.0% resided in assisted living. We found statistically significant small standardized effect sizes (Cohen’s ds of 0.25 to 0.40) for SOPT reflecting processing speed improvements on UFOV scores (of 39 to 63 ms), and greater percentages (9.8 to 14.9 percentage point advantages) for achieving ≥ 0.5 SD improvements (≥ 158.4 ms) across the three time periods.
Conclusions
These findings support public health messaging about the potential benefits of SOPT for older adults in senior living communities, and support the feasibility and acceptability of SOPT in assisted and independent living residences for older adults.
Introduction
Age-related cognitive decline is widespread, well-established, and begins as early as ages 25–30 [1, 2]. Building on neuroplasticity theory and evidence [3, 4], numerous cognitive interventions (e.g., memory, reasoning, processing speed) have been developed to slow or reverse age-related cognitive decline [5]. Those interventions rely on experiential training that “alters the synaptic organization of the brain in species as diverse as fruit flies and humans,” with those synaptic alterations leading to behavioral change [6].
Lingering doubts about the efficacy of cognitive training, however, are reflected in the 2014 Stanford Statement [7], two National Academy of Medicine (NAM) reports [8, 9], and the $2M Federal Trade Commission (FTC) 2016 settlement with Lumos Labs [10]. This is surprising given the accumulated evidence from structured reviews and meta-analyses indicating that cognitive training is effective [11–17]. For example, using data from 97 randomized controlled trials (RCTs) with a variety of cognitive training interventions among both cognitively healthy and mildly cognitively impaired (MCI) adults ≥ 60 years old, Mewborn and colleagues [15] reported a Hedges’ g of 0.30 (p < 0.001) which was not significantly moderated by age, education, or cognitive status. Using data from 17 RCTs among older adults all of whom had MCI, Hill and colleagues [16] reported a Hedges’ g of 0.35 (p < 0.001). And focusing just on speed of processing training (SOPT), Edwards and colleagues [17] reviewed 17 RCTs and reported a Cohen’s d of 0.71 (p < 0.001) on the targeted proximal outcome (UFOV, Useful Field of View) [18, 19] as well as transfer to real-world tasks including Cohen’s ds of 0.27 (p < 0.001), 0.36 (p = 0.038), and 0.21 (p = 0.044) on IADLs, driving mobility, and well-being. Moreover, using the Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) study [20–22], Edwards and colleagues reported evidence of far transfer such that SOPT reduced the risk of dementia onset over 10 years by 39% (p = 0.049) [23]. Nonetheless, further research is warranted, especially studies that include population groups not previously studied, deliver higher doses, rely solely on adaptive training, and use attention control groups [8, 9, 17, 24].
We extend the evidentiary base by reporting the results on the targeted proximal outcome (UFOV) [18, 19] from a community-based study that used a partnership model to implement a two-arm, parallel cognitive training RCT [25]. The intervention group received computerized SOPT while the attention control group solved computerized crossword puzzles. Our design makes two novel contributions to the literature: (1) it is the first study to test SOPT in assisted and independent living populations; and, (2) it used a one-year fully adaptive SOPT dose of 18 hours.
Methods
Human Subjects, Protocol, Participant Enrollment, and Setting
Our study (R01 NR-013908) assessed SOPT effects on processing speed (proximal outcome), depressive symptoms (primary outcome), and pain, anxiety, and quality of life (secondary outcomes). We report here only on the efficacy of SOPT on processing speed because it is the focal pathway in the etiologic mechanism [26, 27]. Human subject approval was obtained from the University of Iowa (IRB Protocol 201208786). The protocol was registered with ClinicalTrials.gov on January 3, 2013 (NCT 01763216). Enrollment occurred between May 17, 2013 and October 22, 2015. As the study design is detailed elsewhere [25], only a brief overview is provided.
We initially targeted assisted living residences at senior living communities in eastern Iowa. Residence directors were contacted, followed by site visits presenting the study, elaborating research team and residence responsibilities, and reviewing the senior living community. The study’s protocol was then individualized to each residence including assistance and guidance to identify, enroll, and train ten participants. Honorariums were initially provided to offset start-up costs, and again after the recruitment target was met or exceeded.
Because of the initially slower engagement rate among assisted living residences, we extended eligibility to their co-residing independent living residences. Inclusion criteria were age ≥ 55 years old, ability to sign meaningful informed consent, and sufficient vision and dexterity to use a computer monitor, keyboard, and mouse. Baseline telephone interviews were conducted by research staff using REDCap (Nashville, Tennessee) [28] and averaged 35 minutes. Follow-up telephone interviews averaged 30 minutes and were conducted 5–8 weeks after baseline (post-training), and at six and twelve months. In addition, versions 6 (MS DOS) and/or 7 (MS Windows) of the UFOV [18, 19] were administered at the senior living communities after each telephone interview.
Randomization
The study biostatistician (MPJ) computer-generated 42 sequential randomization letters separately for each assisted and independent living residence at each of the 31 senior living communities using a 1:1 allocation ratio and permuted blocks of size two and four. Letters were sealed in opaque envelopes, securely stored in the project coordinator’s (MMD) office, and opened by her only after the matching baseline interview and UFOV were completed, ensuring complete blinding at baseline. Research staff were further blinded when conducting follow-up interviews.
Intervention
We used second-generation versions of the SOPT used in ACTIVE [20–22] that were enhanced by Posit Science Corporation (https://www.brainhq.com/why-brainhq/about-the-brainhq-exercises/attention/double-decision). The CD-ROM-based Road Tour was used for participants until Posit Science replaced it with the web-based Double Decision. At its least challenging level (https://www.brainhq.com/why-brainhq/about-the-brainhq-exercises/attention/double-decision), SOPT participants see either a car or truck in the center of the computer screen and a route 66 road sign along with seven rabbit distractor signs in near-periphery locations. The goal is to view the computer screen as quickly as possible (measured in ms) but still correctly identify whether it contained the car or truck and where the route 66 sign was located. Over time, the number of distractors increases, the route 66 sign may move to far-periphery orbits, the car and truck morph to become more alike, and the background image becomes more complicated, all of which increase the challenge level. The initial challenge level is determined by the program’s assessment of each participant. The challenge level increases (adapts) only after the correct identification of the car vs. truck and peripheral location of the route 66 sign in ≥ 75% of the trials. Participants were asked to complete ten hours of training within six weeks of baseline, and four additional hours at both months five and eleven. SOPT electronically tracked completion time.
Attention Control
Attention control participants used Boatload Puzzles, LLC’s Boatload of Crosswords (https://www.boatloadpuzzles.com/playcrossword). These participants see a traditional puzzle format on the monitor. The main differences from a paper and pencil puzzle are that Boatload of Crosswords participants use the mouse and keyboard to enter their answers to the row and column clues, select the size and complexity of the puzzle, and may use radio buttons to show incorrect entries in red font, fill in letters or words, or solve the entire puzzle. Attention control participants had the same training schedule. Boatload of Crosswords was neither adaptive nor recorded the amount of time completed.
Outcomes
Two UFOV [18, 19] outcomes were used. The first was the number of ms (range = 51 to 1,500) spent completing each of three sub-tests measuring processing speed, divided attention, and selective attention which ranged from 17 to 500 ms each and reflect the time that the UFOV images were shown (stimulus duration) for correct identification of the car or truck and the location of the route 66 sign. UFOV has excellent reliability and validity, with 89% sensitivity and 81% specificity in identifying drivers with prior crash histories [18, 19]. The second outcome was a binary indicator for improvements from baseline to the designated follow-up ≥ 0.5 standard deviation (SDs; 158.4 ms based on the baseline SD pooled across treatment groups and residences), a widely-recognized medium standardized effect size [29] and clinically meaningful threshold [30]. Indeed, at 55 mph (80.7 fps) a ≥ 0.5 SD improvement translates into braking a car to a stop in 12.7 fewer feet [31].
Hypotheses, Sample Size and Power
We hypothesized that the SOPT group would achieve greater improvements in both UFOV [18, 19] outcomes compared to the attention control group. Based on one-year results from ACTIVE and the Iowa Healthy and Active Minds Study (IHAMS) [32], one-tailed tests of our directional hypotheses, and a 10% attrition rate [30], we estimated ≥ 80% power with 300 baseline participants. This was conservative, because we allowed participants flexibility to vary their own session lengths to minimize fatigue and boredom, and used two rounds of booster training. Therefore, here we only consider two-tailed p values ≤ 0.05 as statistically significant.
Analyses
We compared the SOPT vs. attention control groups and those in assisted vs. independent living on demographic, socioeconomic, comorbidity, and self-rated health measures, as well as the baseline study outcomes using chi-squared and Student’s t-tests. Retention to the final interview was modeled using multiple logistic regression. Multiple imputation for missing data on the study outcomes was conducted prior to any analyses and used the demographic, socioeconomic, comorbidity, and self-rated health measures, as well as the baseline UFOV. To adjust for the clustering of participants within senior living communities, intention-to-treat (ITT) analyses used random effects in linear mixed effect models (LMEMs) to predict average treatment effects (ATEs) on changes in the UFOV scores from baseline to each follow-up, and to estimate marginal means. Because this study outcome is continuous, coefficients from these models represent mean differences in the UFOV scores. These analyses were done using both a complete case analysis as well as the multiple imputation approach. Ad hoc analyses tested for heterogeneity of treatment effects (HTEs) for the Road Tour (n = 46) vs. Double Decision (n = 127) platforms, and for dosing effects using similar methods. ITT analyses using random effects LMEMs were also used to estimate ATEs on improvements from baseline UFOV scores ≥ 0.5 SD by each follow-up period, and to estimate marginal means. Because this study outcome is binary, these coefficients represent mean differences in the proportion of participants achieving such improvements. All analyses were conducted using IBM SPSS Software, v25.
Results
Descriptive
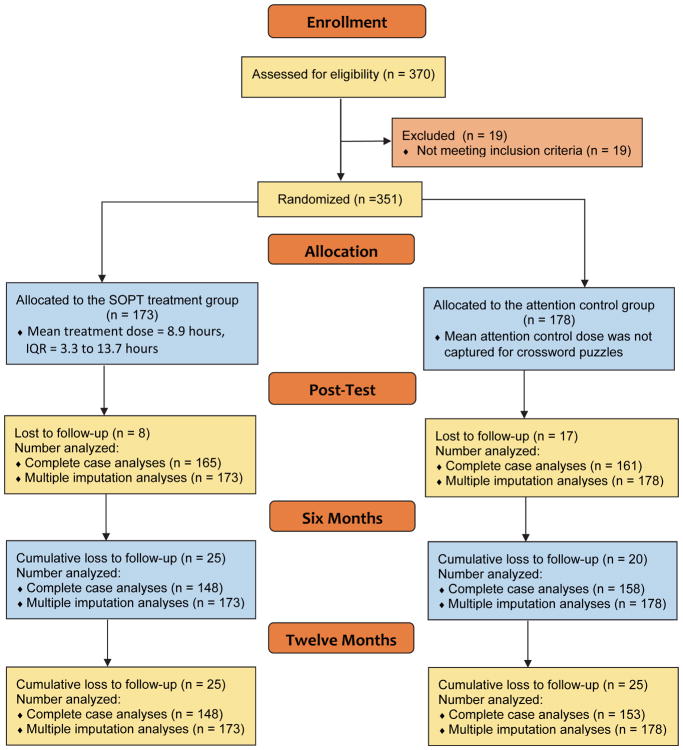
Figure 1 contains the CONSORT flow chart. After consenting, 19 potential participants were excluded prior to randomization due to health issues (3), being too busy (10), moving away (1), vision or computer issues (3), or cognitive impairment (2). We randomized 351 participants and achieved retention rates of 96.0%, 92.3%, and 86.0% at post-training, six months, and twelve months. Table 1 contains selected demographic, socioeconomic, comorbidity, self-rated health, and study outcomes at baseline for the SOPT vs. attention control groups. Mean age was 81.0 years, 73.8% were women, 76.4% lived alone, and 47.0% resided in assisted living. The only significantly different comparison was educational attainment, with more highly educated participants in the attention control group (a potential bias to attention control). The mean treatment dose electronically captured for the SOPT group by study completion was 8.9 hours (IQR = 3.3 to 13.7 hours), but was significantly lower for the assisted vs. independent living participants (7.5 vs. 10.1 hours, p = 0.006). Mean treatment dose for the attention control group was not captured. Assisted living participants also had substantially slower UFOV scores (668.1 ms vs. 447.8 ms, p < 0.001).
Figure 1.
CONSORT Flow Chart.
Table 1.
Baseline Characteristics and Study Outcomes by Treatment Group.
| Participant Characteristics and Study Outcomes | Crosswords Attention Control Group N = 178 |
SOPT Intervention Group N = 173 |
P Value |
|---|---|---|---|
| Demographics | |||
| Age | 81.3 | 80.7 | 0.519 |
| Males | 27.5% | 24.9% | 0.569 |
| Marital Status | 0.749 | ||
| Married | 26.4% | 26.6% | |
| Single | 9.6% | 8.1% | |
| Widowed | 51.1% | 54.3% | |
| Divorced | 12.4% | 10.4% | |
| Living Alone | 75.8% | 76.9% | 0.819 |
| Assisted Living | 46.6% | 47.4% | 0.885 |
| Socioeconomic Status | |||
| Education | 0.035 | ||
| High school or less | 29.8% | 33.5% | |
| Some college | 32.0% | 31.8% | |
| College graduate | 18.0% | 24.9% | |
| Graduate school | 20.2% | 9.8% | |
| Annual Income | 0.296 | ||
| Not reported | 34.8% | 34.1% | |
| Under $25K | 24.7% | 22.5% | |
| $25K to < $50K | 27.5% | 23.1% | |
| $50K or more | 12.9% | 20.2% | |
| Comorbidity | |||
| Mean Number of Chronic Conditions | 4.3 | 4.6 | 0.250 |
| Self-Rated Health | |||
| Self-Rated Health | 0.945 | ||
| Excellent | 7.9% | 6.9% | |
| Very Good | 34.3% | 34.1% | |
| Good | 36.0% | 33.5% | |
| Fair | 19.1% | 22.5% | |
| Poor | 2.8% | 2.9% | |
| Study Outcome | |||
| UFOV Score11 | 540.26 | 564.33 | 0.479 |
Retention Analysis
In the multivariable logistic regression of retention at twelve months (not shown), baseline predictors were SOPT vs. attention control, assisted vs. independent living, UFOV scores, age, sex, and education. Overall, the model fit the data well (AUC = 0.75, Hosmer-Lemeshow statistic = 5.47, p = 0.706). The only two significant adjusted odds ratios (AORs), however, were 1.04 (p = 0.002) for education and 0.33 (p = 0.003) for assisted vs. independent living, indicating that those with higher education were more likely, while assisted living participants were less likely to finish the study.
UFOV Scores
Table 2 contains the results of the ITT random effects LMEMs of the UFOV follow-up scores predicted by the baseline UFOV score, SOPT vs. attention control, assisted vs. independent living, and the random effects for clustering. In the complete case analyses, UFOV scores were reduced by 39.1 ms (p = 0.028), 62.6 ms (p = 0.002), and 42.8 ms (p = 0.045) more in the SOPT vs attention control group by post-training, six months, and twelve months. These reductions reflect standardized effect sizes (Cohen’s ds) of 0.25, 0.40, and 0.27. The estimated marginal means for the SOPT vs. attention control groups were 415.4 vs. 454.5 ms at post-training, 397.9 vs. 460.5 ms at six months, and 360.0 vs. 402.9 ms at twelve months. Those in assisted living had 86.1 ms (p = 0.001), 72.8 ms (p = 0.008), and 49.7 ms (p = 0.095) higher (slower) UFOV scores at post-training, six months, and twelve months than those in independent living. In sensitivity analyses (not shown), we added the potential interaction between SOPT and assisted living (ps = 0.659, 0.208, and 0.214 at post-training, six months, and 12 months), and main effects for age (ps = 0.295, 0.694, and 0.079), gender (ps = 0.415, 0.343, and 0.513), and education (ps = 0.536, 0.920, and 0.629), but found no significant effects.
Table 2.
Intention-to-Treat Results from the Random Effects Linear Mixed Effect Models Predicting Changes in UFOV Scores from Baseline to Post-Training (PT), Baseline to Six Months (6M), and Baseline to Twelve Months (12M), with Complete Case and Multiple Imputation Analyses.
| Complete Case Analysis (NPT = 323, N6M = 302, N12M = 270) | Multiple Imputation Analysis (All N = 351) | |||
|---|---|---|---|---|
| Regression Coefficient (b) | p-value | Regression Coefficient (b) | p-value | |
| Baseline to Post-Training | ||||
| SOPT Treatment | −39.09 | 0.028 | −38.12 | 0.033 |
| Assisted Living | 86.10 | 0.001 | 76.94 | 0.002 |
| Baseline UFOV Score | 0.67 | 0.001 | 0.64 | 0.001 |
| Random Effect for Cluster | N/A | 0.162 | N/A | |
| Baseline to Six Months | ||||
| SOPT Treatment | −62.60 | 0.002 | −52.19 | 0.010 |
| Assisted Living | 72.29 | 0.008 | 55.97 | 0.057 |
| Baseline UFOV Score | 0.60 | 0.001 | 0.59 | 0.001 |
| Random Effect for Cluster | N/A | 0.054 | N/A | |
| Baseline to Twelve Months | ||||
| SOPT Treatment | −42.83 | 0.045 | −47.15 | 0.029 |
| Assisted Living | 49.68 | 0.095 | 57.54 | 0.008 |
| Baseline UFOV Score | 0.62 | 0.001 | 0.60 | 0.001 |
| Random Effect for Cluster | N/A | 0.673 | N/A | |
Note: Because this study outcome is continuous, coefficients from these models represent mean differences in UFOV score changes.
Two ad hoc HTE analyses (not shown) were conducted. The first tested the equivalence of the Road Tour vs. Double Decision using a similar LMEM, but with three instead of two treatment groups. Significantly (p = 0.002) greater improvements (190.1 ms) were found among the Double Decision vs. Road Tour users, but only at six months, with these driven by assisted living participants. The second ad hoc HTE analysis tested for dosing effects. Significantly greater improvements were observed for those with ≥ 8 hours of SOPT at post-training (a 70.4 ms difference, p = 0.047) and twelve months (an 85.6 ms difference, p = 0.035).
UFOV Score Improvements > 0.5 SDs
Table 3 contains the results of the ITT random effects LMEMs of improvements ≥ 0.5 SD in UFOV follow-up scores predicted by the baseline UFOV score, SOPT vs. attention control, assisted vs. independent living, and the random effects for clustering. In the complete case analyses, improvements ≥ 0.5 SD occurred for 9.8% (p = 0.036), 10.3% (p = 0.034), and 14.9% (p = 0.003) more participants in the SOPT vs attention control group by post-training, six months, and twelve months. The estimated marginal means of achieving ≥ 0.5 SD improvements for the SOPT vs. attention control groups were 35.0% vs. 25.2%, 39.1% vs. 28.7%, and 40.4% vs. 25.5% at post-training, six months, and twelve months. The effects for assisted vs. independent living were not statistically significant at post-training (p = 0.206), six months (p = 0.176), or twelve months (p = 0.692). In sensitivity analyses (not shown), we added the potential interaction between SOPT and assisted living (ps = 0.941, 0.428, and 0.971), and main effects for age (ps = 0.605, 0.322, and 0.417), gender (ps = 0.317, 0.633, and 0.614), and education (ps = 0.953, 0.469, and 0.836), but found no significant effects.
Table 3.
Intention-to-Treat Results from the Random Effects Linear Mixed Effect Models Predicting Improvements (Reductions) in UFOV Scores ≥ 0.5 Standard Deviation from Baseline to Post-Training (PT), Baseline to Six Months (6M), and Baseline to Twelve Months (12M), with Complete Case and Multiple Imputation Analyses.
| Complete Case Analysis (NPT = 327, N6M = 306, N12M = 273) | Multiple Imputation Analysis (All N = 351) | |||
|---|---|---|---|---|
| Regression Coefficient (b) | p-value | Regression Coefficient (b) | p-value | |
| Baseline to Post-Training | ||||
| SOPT Treatment | 0.098 | 0.036 | 0.088 | 0.056 |
| Assisted Living | −0.080 | 0.206 | −0.055 | 0.380 |
| Baseline UFOV Score | 0.001 | 0.001 | 0.001 | 0.001 |
| Random Effect for Cluster | N/A | 0.138 | N/A | |
| Baseline to Six Months | ||||
| SOPT Treatment | 0.103 | 0.034 | 0.080 | 0.084 |
| Assisted Living | −0.89 | 0.176 | −0.047 | 0.467 |
| Baseline UFOV Score | 0.001 | 0.001 | 0.001 | 0.001 |
| Random Effect for Cluster | N/A | 0.049 | N/A | |
| Baseline to Twelve Months | ||||
| SOPT Treatment | 0.149 | 0.003 | 0.126 | 0.016 |
| Assisted Living | −0.028 | 0.692 | −0.02 | 0.547 |
| Baseline UFOV Score | 0.001 | 0.001 | 0.001 | 0.001 |
| Random Effect for Cluster | N/A | 0.349 | N/A | |
Note: Because this study outcome is binary, these coefficients represent mean differences in the proportion of participants achieving improvements in UFOV scores ≥ 0.5 SDs.
Discussion
This is the first RCT to test SOPT in assisted and independent living populations. As a result, our participants (47% in assisted living) were older and less healthy than those in prior SOPT RCTs [25]. Indeed, the mean ages in ACTIVE and IHAMS were 74 and 62 years old [33, 34], while the mean age in our study was 81 years old [25]. Consistent with being older, our participants reported more health conditions (means = 4.5 vs. 2.2 in ACTIVE) and were more likely to report fair or poor health (24% vs. 14% in ACTIVE) [25, 33]. We also used a one-year training dose of 18 hours for all participants, with all SOPT sessions being fully adaptive.
The mean training dose for the SOPT participants was 8.9 hours, but was significantly lower among SOPT participants in assisted vs. independent living (7.5 vs. 10.1 hours). We found statistically and clinically relevant effects of SOPT on processing speed that included Cohen’s ds of 0.25 to 0.40 for reducing UFOV scores across the three time periods, and 9.8 to 14.9 percentage point advantages for the SOPT group in achieving ≥ 0.5 SD improvements across the three time periods. SOPT participants completing ≥ 8 hours of training had significantly greater improvements than those completing less training time.
The magnitude of our results are consistent with the conclusions reached in structured reviews and meta-analyses reporting significant but small standardized effect sizes for cognitive training overall [11–16], but extends those results to assisted and independent living populations. They differ, however, from Edwards et al.’s meta-analysis of SOPT [17], which reported large standardized effect sizes on UFOV scores. These differences are consistent with the conclusion of Simons et al. [35] who reported “extensive evidence that brain-training interventions improve performance on the trained tasks, less evidence … on closely related tasks, and little evidence … on distantly related tasks or … everyday cognitive performance.”
Our findings have important implications for the care of older adults. They provide further evidence supporting public health messaging about the potential benefits of SOPT. Moreover, our findings provide support for the use of SOPT with the generally older and less healthy adults in both independent and assisted living residences, because SOPT benefits were not significantly different between these groups and their outcomes were comparable to prior studies of younger and healthier older adults. Furthermore, our findings support the feasibility and acceptability of taking SOPT into senior living communities, although mean SOPT training time completed was only half of the targeted time, with those in assisted living having lower completion rates than those in independent living, likely due to their lower retention rates. Thus, future studies of these populations should consider higher target doses with participant incentives to enhance completion rates.
Our study is not without limitations. Two design modifications after enrollment began resulted in including participants in independent living and shifting from the Road Tour to Double Decision platforms. No cognitive acuity measures other than UFOV were included because of concerns about respondent burden, and therefore participants with MCI or early dementia may have been included. The training for the attention control group was not adaptive. Only SOPT was used rather than a broader spectrum of targeted cognitive training, and the training dose, although 4–8 hours greater than that used in ACTIVE, may not have been sufficient. Nearly all of our participants were white (98.3%) and had above average educational attainment and income levels. The multiple imputation assumed non-informative drop out. Finally, the thematic similarity between SOPT and UFOV raise the question of whether our findings merely reflect “training to the test” [32, 34]. Simons et al. [35], however, reported that there is evidence that cognitive interventions, including SOPT, improved closely related tasks in addition to their effects on the trained tasks, and Edwards et al. [17] reported that SOPT effects transfer to IADLs, driving mobility, and well-being.
Key Points.
Question
Can speed of processing training (SOPT) improve the processing speed of older Americans in both assisted and independent living residences?
Findings
SOPT participants had significantly improved processing speed (39 to 63 ms on UFOV scores; Cohen’s ds of 0.25 to 0.40), and greater percentages (9.8 to 14.9 percentage point advantages) for achieving ≥ 0.5 SD improvements (≥ 158.4 ms) across the three time periods.
Meaning
Although the standardized effect sizes were small, our results support public health messaging about the potential benefits of SOPT for older adults in senior living communities, and the feasibility and acceptability of SOPT treatment in both assisted and independent living residences.
Acknowledgments
Funding Source:
NIH R01-NR013908
Conflicts. Drs. Smith and Jones, and Ms. Dotson state that they have no financial conflicts, no personal conflicts, and no conflicts of interest to declare. Dr. Wolinsky reports that from December 2007 to March 2009 he had a part-time consulting arrangement (15 days total) with Posit Science Corporation to support additional analyses of the first five-years of the ACTIVE follow-up data that had neither been identified in the original ACTIVE protocols nor funded by the various NIH grants supporting ACTIVE. That arrangement was approved in advance by the ACTIVE Executive Committee (which included the NIH project officers), and was approved by the Provost of the University of Iowa. Since 2009, Dr. Wolinsky has received no compensation of any kind from Posit Science Corporation, and he states that he has no other financial conflicts, no other personal conflicts, and no other conflicts of interest to declare.
Author Contributions. Drs. Smith and Jones, Ms. Dotson, and Dr. Wolinsky have each made substantial contributions to: (1) the conception and design of the study, or acquisition of the data, or analysis and interpretation of the data; and, (2) drafting the article or revising it critically for important intellectual content. Moreover, they have each (3) granted final approval of the current version for publication. Accordingly, all authors meet the criteria for authorship as stated in the ICMJE’s Uniform Requirements for Manuscripts Submitted to Biomedical Journals.
Funding. This study was funded by the National Institute of Nursing Research (NINR; R01 NR-013908). The NINR, however, had no role in (a) the design and conduct of the study, (b) the collection, management, analysis, and interpretation of data, (c) the preparation, review, or approval of the manuscript, or (d) the decisions to submit and publish the manuscript. Posit Science Corporation provided free copies of Road Tour and Double Decision for use by study participants. Posit Science Corporation, however, had no role in (a) the design and conduct of the study, (b) the collection, management, analysis, and interpretation of data, (c) the preparation, review, or approval of the manuscript, or (d) the decisions to submit and publish the manuscript. NINR and Posit Science Corporation had neither seen the results presented here in any form, nor had they been given access to the manuscript before its acceptance for publication. Licenses for Boatload of Crosswords were purchased from Boatload Puzzles, LLC using NINR grant funds.
Footnotes
Impact Statement:
The authors certify that this work is novel. It is the first study to test SOPT in the rapidly expanding assisted and independent living populations, and it uses a one-year fully adaptive targeted training dose of 18 hours. This work demonstrates the feasibility and acceptance of SOPT in senior living communities, and shows that SOPT significantly and clinically improved processing speed in both assisted and independent living.
References
- 1.Salthouse TA. When does age-related cognitive decline begin? Neurobiol Aging. 2009;30:507–514. doi: 10.1016/j.neurobiolaging.2008.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finch CE. The neurobiology of middle-age has arrived. Neurobiol Aging. 2009;30:515–520. doi: 10.1016/j.neurobiolaging.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 3.Merzenich M. Soft-Wired: How the New Science of Brain Plasticity Can Change Your Life. 2. San Francisco CA: Parnassas Publishing; 2013. [Google Scholar]
- 4.Doidge N. The Brain’s Way of Healing: Stories of Remarkable Recoveries and Discoveries. New York NY: Penguin Publishing Group; 2016. [Google Scholar]
- 5.Salthouse TA. Do cognitive interventions alter the rate of age-related cognitive change? Intelligence. 2015;53:86–91. doi: 10.1016/j.intell.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kolb B, Whishaw IQ. Brain plasticity and behavior. Annu Rev Psychol. 1998;49:43–64. doi: 10.1146/annurev.psych.49.1.43. doi.org/0066-4308/98/0201-0043. [DOI] [PubMed] [Google Scholar]
- 7.Stanford Center on Longevity, Berlin Max Planck Institute for Human Development. A Consensus on the Brain Training Industry from the Scientific Community. Stanford CA: Stanford Center on Longevity; http://longevity3.stanford.edu/blog/2014/10/15/the-consensus-on-the-brain-training-industry-from-the-scientific-community/ [Google Scholar]
- 8.Blazer DG, Yaffee K, Liverman CT, editors. Cognitive Aging: Progress in Understanding and Opportunities for Action. Washington DC: National Academy of Medicine; 2015. org/10.17226/21693. [PubMed] [Google Scholar]
- 9.Leshner AI, Landis S, Stroud C, Downey A, editors. Preventing Cognitive Decline and Dementia: A Way Forward. Washington DC: National Academy of Medicine; 2017. org/10.17226/24782. [PubMed] [Google Scholar]
- 10.Federal Trade Commission. Lumosity to Pay $2 Million to Settle FTC Deceptive Advertising Charges for Its “Brain Training” Program. Washington DC: Federal Trade Commission; Jan 5, 2016. https://www.ftc.gov/news-events/press-releases/2016/01/lumosity-pay-2-million-settle-ftc-deceptive-advertising-charges. [Google Scholar]
- 11.Kelly ME, Loughrey D, Lawlor BA, Robertson IH, Walsh C, Brennan S. The impact of cognitive training and mental stimulation on cognitive ability and everyday functioning of health older adults: a systematic review and meta-analysis. Ageing Res Rev. 2014;15:28–43. doi: 10.1016/j.arr.2014.02.044. [DOI] [PubMed] [Google Scholar]
- 12.Kueder AM, Parisi JM, Gross AL, Rebok G. Computerized cognitive training with older adults: a systematic review. PLoS ONE. 2012;7:e40588. doi: 10.1371/journal.pone.0040588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lampit A, Hallock H, Valenzuela M. Computerized cognitive training in cognitively healthy older adults: a systematic review and meta-analysis of effect modifiers. PLoS Med. 2014;11:e1001756. doi: 10.1371/journal.pmed.1001756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lampit A, Valenzuela MJ, Gates NJ. Computerized cognitive training is beneficial for older adults. J Amer Geriatr Soc. 2015;63:2610–2612. doi: 10.1111/jgs.1382. [DOI] [PubMed] [Google Scholar]
- 15.Mewborn CM, Lindbergh CA, Miller LS. Cognitive interventions for cognitively healthy, mildly impaired, and mixed samples of older adults: a systematic review and meta-analysis of randomized controlled trials. Neuropsychol Rev. 2017 doi: 10.1007/s11065-017-9350-8. in press. org/10.1007/s11065-017-9350-8. [DOI] [PubMed]
- 16.Hill NT, Mowszowski L, Naismith SL, Chadwick VL, Valenzuela M, Lampit A. Computerized cognitive training in older adults with mild cognitive impairment or dementia: a systematic review and meta-analysis. Am J Psychiatry. 2017;174:329–240. doi: 10.1176/appi.ajp.2016.16030360. [DOI] [PubMed] [Google Scholar]
- 17.Edwards JD, Fasusto BA, Tetlow AM, Corona RT, Valdes EG. Systematic review and meta-analyses of useful field of view cognitive training. Neurosci Biobehav Rev. 2018;74:72–91. doi: 10.1016/j.neubiorev.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 18.Edwards JD, Vance DE, Wadley VG, Cissell GM, Roenker DL, Ball KK. Reliability and validity of useful field of view test scores as administered by personal computer. J Clin Exp Neuropsychol. 2005;27:529–543. doi: 10.1080/13803390490515432. [DOI] [PubMed] [Google Scholar]
- 19.Visual Awareness, Inc. UFOV User’s Guide, Version 6.0.9. Birmingham, AL: Visual Awareness, Inc; 2004. [Google Scholar]
- 20.Ball KK, Berch DB, Helmers KF, et al. Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA. 2002;288:2271–2281. doi: 10.1001/jama.288.18.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Willis SL, Tennstedt SL, Marsiske M, et al. Long-term effects of cognitive training on everyday functional outcomes in older adults. JAMA. 2006;296:2805–2814. doi: 10.1001/jama.296.23.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rebok GL, Ball KK, Quey LT, et al. Cognitive training: results from the ACTIVE study at 10 years. J Amer Geriatr Soc. 2014;62:16–24. doi: 10.1111/jgs.12607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Edwards JD, Xu H, Clark DO, Guey LT, Ross LA, Unverzagt FW. Speed of processing training results in lower risk of dementia. Alzheimers Dement. 2017;3:603–611. doi: 10.1016/j.trci.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Howren MB, Vander Weg MW, Wolinsky FD. Computerized cognitive training interventions to improve neuropsychological outcomes: evidence & future directions in the CER era. J Comp Eff Res. 2014;3:145–154. doi: 10.2217/CER.14.6. [DOI] [PubMed] [Google Scholar]
- 25.Smith M, Jones MP, Dotson MM, Wolinsky FD. Cognitive training and processing speed in assisted and independent living: the Mood Study randomized controlled trial. J Clin Trials. 2018:8. doi: 10.1111/jgs.15423. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salthouse TA. The processing-speed theory of adult age differences in cognition. Psych Rev. 1996;103:401–428. doi: 10.1037/0033-295X.103.3.403. [DOI] [PubMed] [Google Scholar]
- 27.Lovden M, Backman L, Lindenberger U, Schaefer S, Schmiedek F. A theoretical framework for the study of adult cognitive plasticity. Psych Bull. 2010;136:659–676. doi: 10.1037/a0020080. [DOI] [PubMed] [Google Scholar]
- 28.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. doi.org.10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Mahwah NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 30.Norman G, Sloan J, Wyrwich K. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. http://www.jstor.org/stable/3768017. [DOI] [PubMed] [Google Scholar]
- 31.Green M. How long does it take to stop? Methodological analysis of driver perception-brake times. Trans Hum Factors. 2000;2:195–216. doi: 10.1207/STHF0203_1. [DOI] [Google Scholar]
- 32.Wolinsky FD, Vander Weg MW, Howren MB, Jones MP, Dotson MM. A randomized controlled trial of cognitive training using a visual speed of processing intervention in middle aged and older adults. PLoS ONE. 2013;8:e61624. doi: 10.1371/journal.pone.0061624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wolinsky FD, Vander Weg MW, Howren MB, Jones MP, Dotson MM. Effects of cognitive speed of processing training on a composite neuropsychological outcome: results at one-year from the IHAMS randomized controlled trial. Int Psychoger. 2016;28:317–330. doi: 10.1017/S1041610215001428. [DOI] [PubMed] [Google Scholar]
- 34.Wolinsky FD, Vander Weg MW, Howren MB, et al. Interim analyses from a randomised controlled trial to improve visual processing speed in older adults: the Iowa Healthy and Active Minds Study. BMJ Open. 2011;1(2):e000225. doi: 10.1136/bmjopen-2011-000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Simons DJ, Boot WR, Charness N, et al. Do “brain-training” programs work? Psychol Sci Pub Interest. 2016;17(3):103–186. doi: 10.1177/1529100616661983. [DOI] [PubMed] [Google Scholar]