Abstract
Background/Objective
Whether changes in function provide useful prognostic information beyond that available from present function is uncertain. Our objective was to evaluate the prognostic effect of changes in physical function at different intervals over the prior year on subsequent outcomes after accounting for present function.
Design
Prospective longitudinal study.
Setting
Greater New Haven, Connecticut, from March 1998 to January 2006.
Participants
658 community-living persons, aged 71 years or older, who completed an 18-month comprehensive assessment.
Measurements
Disability in 13 basic, instrumental and mobility activities was assessed at the 18-month comprehensive assessment and at 12, 6, and 3 months prior to 18-months. Time to death and long-term nursing home admission, defined as ≥3 months, were ascertained for up to 5 years after 18-months.
Results
In the bivariate models, disability at 18-months and change in disability between 18-months and each of the three-prior time-points (12, 6, and 3 months) were significantly associated with time to death. The risk of death, for example, increased by 24% for each 1-point increase in 18-month disability score (on a scale from 0 to 13) and by 22% for each 1-point change in disability score between 18-months and prior 12 months (on a scale from −13 to 13). In a set of multivariable models without and with covariates, the associations were maintained for 18-month disability but not for change in disability between 18-months and each of the three-prior time-points. The results were comparable for time to long-term nursing home admission except that two of the associations did not achieve statistical significance.
Conclusion
When evaluating risk for adverse outcomes, such as death and long-term nursing home admission, an assessment of change in physical function at different intervals over the prior year, although a strong bivariate predictor, did not provide useful prognostic information beyond that available from the level of function at the present time.
Keywords: longitudinal study, older persons, disability, prognosis
Among older persons, functional status is a powerful predictor of an array of adverse outcomes, including death,1, 2 long-term nursing home admission,3 use of formal and informal home services,4, 5 and hospital readmission.6 Based on these and other findings, functional status has become a core element of many prognostic indices.7–9 Careful consideration of prognosis is particularly important for clinical decision making in older patients given their high prevalence of competing chronic conditions and diminished life expectency.10
When formulating their prognostic estimates, clinicians often attempt to determine whether their older patients have experienced a decline in their functional status under the assumption that changes in physical function may provide useful prognostic information beyond that available from the level of function at the present time. If this assumption is correct, the inclusion of change in function could enhance the performance of prognostic indices for use by clinicians and investigators.
The objective of the current study was to evaluate the prognostic effect of changes in physical function at different intervals over the prior year on subsequent outcomes after accounting for present function. We used high quality data from a unique longitudinal study of community-living older persons that includes frequent assessments of functional status and ascertainment of two clinically relevant outcomes—death and long-term nursing home admission—over a 5-year period. The results of this study have the potential to inform prognostic estimates and, in turn, enhance clinical decision-making in older patients.
METHODS
Study Population
Participants were drawn from an ongoing longitudinal study of 754 community-living persons, aged≥70, who were initially nondisabled in basic activities of daily living.11, 12 Potential participants were members of a large health plan and were excluded for significant cognitive impairment with no available proxy,13 life expectancy<12 months, plans to move out of the area, or inability to speak English. Only 4.6% of persons refused screening, and 75.2% of those eligible agreed to participate and were enrolled from March 1998 to October 1999. The study was approved by the Yale Human Investigation Committee, and all participants provided informed consent.
Analytic Sample
The current analysis included community-living participants who completed the 18-month comprehensive assessment. Of the 754 participants, 27 (3.6%) refused to complete the assessment, 11 (1.5%) had incomplete disability data, 12 (1.6%) were no longer community-living, and 46 (6.1%) had died, leaving 658 participants in the analytical sample. Compared with these participants, the 96 cohort members not included in the analytical sample were (at baseline) older (80.6 vs. 78.1 years, p<.001), had more chronic conditions (2.0 vs. 1.7, p=.040), and were more likely to be physically frail (61.5% vs. 40.0%, p<.001) and cognitively impaired (18.8% vs. 10.3%, p=.015), as defined below. There were no significant baseline differences according to sex, race/ethnicity, living situation, or education.
Data Collection
The 18-month comprehensive assessment was completed in the home, while the monthly assessments were completed over the telephone. The research nurses who completed the 18-month assessments were kept blinded to the results of the monthly assessments. The completion rate of the monthly interviews was 99%. When participants were unable to complete the monthly interviews (10.1% of observations), proxy data were obtained using a standard protocol.13 The accuracy of these proxy reports was high.13
Descriptive Characteristics/Covariates
During the comprehensive assessment, data were collected on demographic characteristics, nine self-reported, physician-diagnosed chronic conditions, body mass index, cognitive status,14 depressive symptoms,15 and physical frailty, based on slow gait speed.16
Disability Assessments
Complete details regarding the assessment of disability are provided elsewhere.12, 13, 17 Each month and during the comprehensive assessment, participants were asked, “At the present time, do you need help from another person to (complete the task)?” for each of four basic activities (bathing, dressing, walking, and transferring), five instrumental activities (shopping, housework, meal preparation, taking medications, and managing finances), and three mobility activities (walk 1/4 mile, climb flight of stairs, and lift/carry ten pounds). For these 12 activities, disability was operationalized as the need for personal assistance or unable to do the task. Participants were also asked about a fourth mobility activity, “Have you driven a car during the past month?” Participants who responded “No” were considered to be “disabled” in driving.17 To address the small amount of missing data on disability (1% of observations), multiple imputation was used with 100 random draws per missing observation.18
Outcomes
Deaths were ascertained by review of the local obituaries and/or from an informant during a monthly telephone interview. Information on long-term nursing home admissions was obtained primarily from Medicare claims, using the Minimum Data Set (MDS) and Medicare Provider Analysis and Review (MedPAR) files.16 Based on start and end dates, a long-term admission was defined as greater than 100 days, the maximum duration of Medicare payment. To identify other long-term admissions (13.5% of outcomes), i.e. when Medicare claims were not available, we used information from the monthly interviews. Participants were asked whether they had been admitted to a nursing home during the prior month; if they had, the interviewer noted whether they were currently in a nursing home. The accuracy of this information was almost perfect (Kappa = 0.96).3 Participants who were residents of a nursing home for four consecutive monthly interviews, corresponding to a minimal length of stay of 91 days, were classified as having a long-term admission, as previously described.3
Statistical Analysis
Change in disability was assessed between the 18-month comprehensive assessment and the prior 12, 6, and 3 months, respectively. These intervals were considered to be the most relevant clinically. The two outcomes included time to death and long-term nursing home admission, respectively, over a 5-year period subsequent to 18-months.
For time to death, we estimated three sets of Cox regression models. The bivariate models evaluated the disability score at 18-months and change in disability between 18-months and each of the three-prior time-points (12, 6, and 3 months). The second set of models evaluated the disability score at 18-months together with change in disability for each of the three time-points. The third set of models added a pre-specified list of covariates to the second set of models. To maintain a family-wise Type I error rate of 0.05 for hypothesis testing, the model-derived p-values were adjusted within each set of models for multiple comparisons using the Hochberg method.20 For time to long-term nursing home admission, we followed a similar set of procedures except that a competing risk model was used to account for potential bias due to death.21
The proportional hazards assumption and overall model fit were evaluated for all models. All analyses were conducted using the SAS version 9.4. An adjusted p-value<.05 was considered as statistically significant.
RESULTS
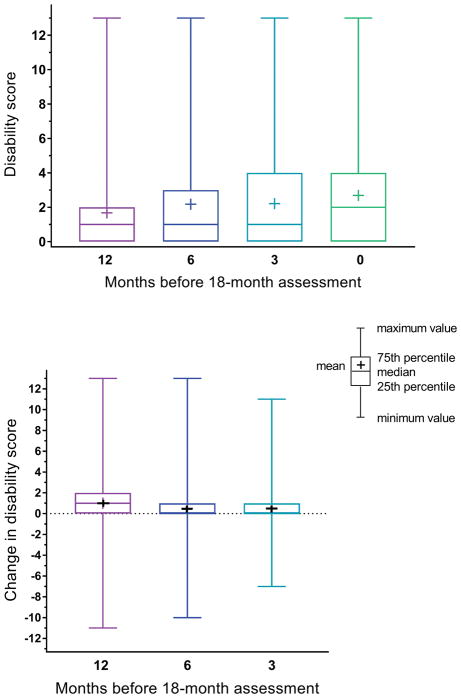
The characteristics of participants in the analytic sample are provided in Table 1. The top panel of Figure 1 shows the distribution of disability scores at 18-months and at 12, 6, and 3 months prior to 18-months. Over the course of a year, the mean disability scores increased from 1.7 to 2.7. The distribution of changes in disability scores between 18-months and 12, 6, and 3 months prior to 18-months is shown in the bottom panel of Figure 1. Although there was considerable variability at each time point, mean changes were largest at 12 months and comparable at 6 and 3 months. Of the 658 participants, 169 (25.7%) died over a median of 31.6 months, while 104 (15.8%) had a long-term nursing home admission over a median of 29.5 months.
Table 1.
Characteristics of the Analytic Sample at 18 Months
| Characteristic | N=658 |
|---|---|
| Age in years, mean (SD) | 79.6 (5.1) |
| Female sex, n (%) | 429 (65.2) |
| Non-Hispanic white, n (%) | 596 (90.6) |
| Education in years, mean (SD) | 12.0 (2.8) |
| Living alone, n (%) | 274 (41.6) |
| Number of chronic conditions,a mean (SD) | 1.9 (1.3) |
| Body mass index,b n (%) | |
| Normal/underweight | 267 (40.6) |
| Overweight | 241 (36.6) |
| Obese | 150 (22.8) |
| Cognitive impairment,c n (%) | 93 (14.1) |
| Depressive symptoms,d n (%) | 112 (17.0) |
| Physically frail,e n (%) | 274 (41.6) |
| Number of disabilities,f mean (SD) | 2.7 (2.8) |
Abbreviation: SD, standard deviation.
Included hypertension, myocardial infarction, congestive heart failure, stroke, diabetes mellitus, arthritis, hip fracture, chronic lung disease, and cancer.
Categorized into three groups based on published cut-points (<25, 25.0–29.9, and ≥30 kg/m2, respectively),25 as previously described.3
Defined as score less than 24 on Folstein Mini-Mental State Examination.
Defined as score of 20 or greater on Center for Epidemiological Studies-Depression Scale.
Based on slow walking speed as described in the Methods.
Of 13 possible: 4 basic, 5 instrumental, and 4 mobility.
Figure 1.
Distribution of disability scores at 18-months (denoted as “0”) and at 12, 6, and 3 months prior to 18-months (top panel) and changes in disability scores between 18-months and 12, 6, and 3 months prior to 18-months (bottom panel). Positive change scores denote worsening disability. The schematic diagram provides descriptive labels for the relevant components of the box plots. For the top panel, the values for minimum and 25th percentile are equivalent.
The top panel of Table 2 provides the longitudinal associations between the disability scores and time to death over 5 years. In the bivariate models, disability at 18-months and change in disability between 18-months and each of the three-prior time-points (12, 6, and 3 months) were significantly associated with time to death. The risk of death, for example, increased by 24% for each 1-point increase in 18-month disability score (on a scale from 0 to 13) and by 22% for each 1-point change in disability score between 18-months and prior 12 months (on a scale from −13 to 13). In each of the three multivariable models without covariates, the associations were maintained for 18-month disability but not for change in disability. The results were comparable for the multivariable models with covariates, although the hazard ratios were modestly diminished for 18-month disability. For 18-months alone, the adjusted hazard ratio (95% CI) was 1.21 (1.13, 1.30).
Table 2.
Longitudinal Associations between Disability Scores and Subsequent Outcomes over 5 Years a
| Disability Scores b | Bivariate Models | Multivariable Models without Covariates c | Multivariable Models with Covariates d | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| HR (95% CI) | p-value | HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Time to Death | ||||||
| 18-months | 1.24 (1.18–1.30) | <.001 | ||||
|
| ||||||
| 18-months – 12 m | 1.22 (1.12–1.33) | <.001 | 1.03 (0.94–1.12) | .599 | 1.07 (0.97–1.17) | .527 |
| 18-months | 1.22 (1.15–1.29) | <.001 | 1.17 (1.08–1.27) | <.001 | ||
|
| ||||||
| 18-months – 6 m | 1.16 (1.05–1.28) | <.001 | 0.98 (0.91–1.07) | .599 | 1.00 (0.92–1.08) | .766 |
| 18-months | 1.24 (1.17–1.31) | <.001 | 1.22 (1.13–1.31) | <.001 | ||
|
| ||||||
| 18-months – 3 m | 1.26 (1.14–1.39) | <.001 | 1.08 (0.98–1.19) | .599 | 1.10 (0.99–1.22) | .766 |
| 18-months | 1.21 (1.15–1.28) | <.001 | 1.17 (1.09–1.26) | <.001 | ||
|
| ||||||
| Time to Long-term Nursing Home Admission | ||||||
| 18-months | 1.21 (1.15–1.27) | <.001 | ||||
|
| ||||||
| 18-months – 12 m | 1.13 (1.04–1.22) | .006 | 0.94 (0.87–1.02) | .353 | 1.04 (0.97–1.21) | .832 |
| 18-months | 1.25 (1.17–1.33) | <.001 | 1.17 (1.10–1.25) | .030 | ||
|
| ||||||
| 18-months – 6 m | 1.15 (1.05–1.26) | .006 | 0.99 (0.91–1.08) | .801 | 1.02 (0.95–1.09) | .832 |
| 18-months | 1.21 (1.14–1.29) | <.001 | 1.19 (1.12–1.26) | .115 | ||
|
| ||||||
| 18-months – 3 m | 1.09 (0.98–1.21) | .124 | 0.94 (0.85–1.03) | .353 | 0.97 (0.88–1.06) | .832 |
| 18-months | 1.23 (1.16–1.30) | <.001 | 1.12 (1.04–1.22) | .013 | ||
Abbreviation: HR, hazard ratio; CI, confidence interval
For each of the three sets of models, p-values were adjusted for multiple comparisons using the Hochberg method.
Disability was assessed at the 18-month comprehensive assessment. Changes in disability were assessed between 18-months and the prior 12, 6, and 3 months. The hazard ratios are per each 1-point increase in disability score (0–13) for 18-months and per each 1-point change in disability score (−13 to 13) between 18-months and prior monthly assessment.
The models included only 18-months and change in disability scores.
In addition to 18-month and change in disability scores, the models included the following covariates assessed during the 18-month comprehensive assessment: age, sex, race/ethnicity, years of education, living situation, number of chronic conditions, body mass index, cognitive impairment, depressive symptoms, and physical frailty as defined in the Methods.
The bottom panel of Table 2 provides the corresponding associations for time to long-term nursing home admission. The results were generally comparable to those for time to death except that two of the associations did not achieve statistical significance: (1) change in disability between 18-months and prior 3 months in the bivariate model, and (2) 18-month disability in the multivariable model that included covariates and change in disability between 18-months and prior 6 months. Otherwise, in both sets of multivariable models, 18-month disability was significantly associated with time to long-term nursing home admission, while change in disability was not. For 18-months alone, the adjusted hazard ratio (95% CI) was 1.12 (1.04, 1.20).
DISCUSSION
In this prospective longitudinal study of community-living older persons, we found that an assessment of change in physical function at different intervals over the prior year, although a strong bivariate predictor of adverse outcomes, did not provide useful prognostic information beyond that available from the level of function at the present time. These results suggest that a single assessment of functional status may sufficiently capture the physical domain of functioning, making an assessment of change unnecessary or even redundant.
Functional status is a powerful predictor of risk, largely because it reflects the cumulative impact of disease and physiologic changes over time. By integrating decrements across different organ systems, functional status provides clinicians with a single patient-centered measure that conveys substantial prognostic information. When assessing physical function, the results of the current study suggest that it is more important to determine where a patient is, rather than where she has been. By obviating the need to assess changes in function over time, our results should simplify prognostic estimates and, in turn, facilitate clinical decision-making in older patients.
In bivariate analysis, we found that changes in disability over the course of 3 to 12 months were significantly associated with time to death and long-term nursing home admission with only one exception. These associations were greatly diminished, however, after accounting for disability at the present time. In contrast, disability at the present time remained strongly associated with both outcomes in models that included change in disability and a comprehensive set of covariates.
To our knowledge, relatively few prior studies have evaluated the independent effect of changes in physical function over time. Our findings are consistent with those of an earlier study that evaluated the effect of change in physical performance on the risk of disability in activities of daily living.22 For each of three timed tests, nondisabled older persons who had a large decline in physical performance over one year were significantly more likely to develop disability at three years than those who improved or showed no change. After adjusting for 1-year scores, however, change in physical performance was no longer associated with the risk of disability. Similar findings were subsequently reported using data from the InCHIANTI Study.23
Our study has several strengths, including assessment of a comprehensive set of basic, instrumental, and mobility activities, consistency of results for changes in function over three different periods of time, and an analytic plan that adjusted for multiple statistical comparisons and accounted for potential bias due to death for the outcome of long-term nursing home admission. Our results should be interpreted, however, in the context of potential limitations. Outcomes were limited to time to death and long-term nursing home admission over 5 years. These are two of the most clinically relevant outcomes for older persons. The consistency of our results, moreover, suggest that they likely apply to other distal outcomes. Because study participants were members of a single health plan in a small urban area, the results may not be generalizable to older persons in other settings. Although the demographic characteristics of the cohort reflect those of older persons in New Haven County, Connecticut, which are similar to the characteristics of the US population as a whole, with the exception of race and ethnic group,24 our results should be confirmed in other studies.
In summary, when evaluating risk for adverse outcomes, an assessment of change in physical function at different intervals over the prior year, although a strong bivariate predictor, may not provide useful prognostic information beyond that available from the level of function at the present time.
Acknowledgments
The work for this report was funded by a grant from the National Institute on Aging (R01AG17560). The study was conducted at the Yale Claude D. Pepper Older Americans Independence Center (P30AG21342). Dr. Gill is the recipient of an Academic Leadership Award (K07AG043587) from the National Institute on Aging.
We thank Denise Shepard, BSN, MBA, Andrea Benjamin, BSN, Barbara Foster, and Amy Shelton, MPH for assistance with data collection; Wanda Carr and Geraldine Hawthorne, BS, for assistance with data entry and management; Peter Charpentier, MPH for design and development of the study database and participant tracking system; and Joanne McGloin, MDiv, MBA for leadership and advice as the Project Director.
Footnotes
Conflicts of Interest:
The authors have no conflicts of interest.
Author Contributions:
Dr. Gill had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors meet the criteria for authorship stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals.
Study concept and design: Gill, Allore
Acquisition of data: Gill, Gahbauer, Leo-Summers
Analysis and interpretation of data: Gill, Han, Gahbauer, Leo-Summers, Allore
Preparation of manuscript: Gill, Han, Allore
Critical revision of the manuscript for important intellectual content: Gill, Han, Gahbauer, Leo-Summers, Allore
Statistical analysis: Han, Allore
We certify that this work is novel: the study shows that an assessment of change in physical function does not provide useful prognostic information beyond that available from the level of function at the present time.
Role of the Sponsors:
The organizations funding this study had no role in the design or conduct of the study; in the collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript.
References
- 1.Manton KG. A longitudinal study of functional change and mortality in the United States. J Gerontol. 1988;43:S153–161. doi: 10.1093/geronj/43.5.s153. [DOI] [PubMed] [Google Scholar]
- 2.Gill TM, Robison JT, Tinetti ME. Difficulty and dependence: two components of the disability continuum among community-living older persons. Ann Intern Med. 1998;128:96–101. doi: 10.7326/0003-4819-128-2-199801150-00004. [DOI] [PubMed] [Google Scholar]
- 3.Gill TM, Allore HG, Han L. Bathing disability and the risk of long-term admission to a nursing home. J Gerontol A Biol Sci Med Sci. 2006;61:821–825. doi: 10.1093/gerona/61.8.821. [DOI] [PubMed] [Google Scholar]
- 4.Kemper P. The use of formal and informal home care by the disabled elderly. Health Serv Res. 1992;27:421–451. [PMC free article] [PubMed] [Google Scholar]
- 5.Coughlin TA, McBride TD, Perozek M, et al. Home care for the disabled elderly: predictors and expected costs. Health Serv Res. 1992;27:453–479. [PMC free article] [PubMed] [Google Scholar]
- 6.Greysen SR, Stijacic Cenzer I, Auerbach AD, et al. Functional impairment and hospital readmission in Medicare seniors. JAMA Intern Med. 2015;175:559–565. doi: 10.1001/jamainternmed.2014.7756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee SJ, Lindquist K, Segal MR, et al. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295:801–808. doi: 10.1001/jama.295.7.801. [DOI] [PubMed] [Google Scholar]
- 8.Yourman LC, Lee SJ, Schonberg MA, et al. Prognostic indices for older adults: a systematic review. JAMA. 2012;307:182–192. doi: 10.1001/jama.2011.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schonberg MA, Davis RB, McCarthy EP, et al. Index to predict 5-year mortality of community-dwelling adults aged 65 and older using data from the National Health Interview Survey. J Gen Intern Med. 2009;24:1115–1122. doi: 10.1007/s11606-009-1073-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gill TM. The central role of prognosis in clinical decision making. JAMA. 2012;307:199–200. doi: 10.1001/jama.2011.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gill TM, Desai MM, Gahbauer EA, et al. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135:313–321. doi: 10.7326/0003-4819-135-5-200109040-00007. [DOI] [PubMed] [Google Scholar]
- 12.Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004;291:1596–1602. doi: 10.1001/jama.291.13.1596. [DOI] [PubMed] [Google Scholar]
- 13.Gill TM, Hardy SE, Williams CS. Underestimation of disability among community-living older persons. J Am Geriatr Soc. 2002;50:1492–1497. doi: 10.1046/j.1532-5415.2002.50403.x. [DOI] [PubMed] [Google Scholar]
- 14.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 15.Kohout FJ, Berkman LF, Evans DA, et al. Two shorter forms of the CES-D Depression Symptoms Index. J Aging Health. 1993;5:179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 16.Gill TM. Disentangling the disabling process: insights from the Precipitating Events Project. Gerontologist. 2014;54:533–549. doi: 10.1093/geront/gnu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gill TM, Gahbauer EA, Murphy TE, et al. Risk factors and precipitants of long-term disability in community mobility: a cohort study of older persons. Ann Intern Med. 2012;156:131–140. doi: 10.1059/0003-4819-156-2-201201170-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gill TM, Guo Z, Allore HG. Subtypes of disability in older persons over the course of nearly 8 years. J Am Geriatr Soc. 2008;56:436–443. doi: 10.1111/j.1532-5415.2007.01603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feinstein AR. Clinical epidemiology: the architecture of clinical research. Philadelphia: W.B. Saunders; 1985. [Google Scholar]
- 20.Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75:800–802. [Google Scholar]
- 21.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 22.Gill TM, Williams CS, Mendes de Leon CF, et al. The role of change in physical performance in determining risk for dependence in activities of daily living among nondisabled community-living elderly persons. J Clin Epidemiol. 1997;50:765–772. doi: 10.1016/s0895-4356(97)00065-6. [DOI] [PubMed] [Google Scholar]
- 23.Stenholm S, Guralnik JM, Bandinelli S, et al. The prognostic value of repeated measures of lower extremity performance: should we measure more than once? J Gerontol A Biol Sci Med Sci. 2014;69:894–899. doi: 10.1093/gerona/glt175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.US Census Bureau. [Accessed January 10, 2018];American FactFinder. http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml.
- 25.Executive summary of the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Arch Intern Med. 1998;158:1855–1867. doi: 10.1001/archinte.158.17.1855. [DOI] [PubMed] [Google Scholar]