Abstract
Background
To compare between the sequential and concurrent use of vaginal misoprostol plus Foley catheter for labor induction.
Methods
This single-center, non-blinded randomized study was conducted at the department of Obstetrics and Gynecology, Faculty of medicine, Zagazig University. A total of 160 women with full term singleton pregnancy, cephalic presentation and bishop score ≤ 6 were randomized for labor induction with either concurrent or sequential use of vaginal misoprostol plus Foley catheter (80 cases in each group). The primary outcome measured was induction-to-delivery interval and secondary outcomes mesaured were vaginal delivery within 24 h, number of doses needed to induce labor, need of oxytocin for augmentation of labor, cesarean section rate, maternal or neonatal complications.
Results
The mean induction-to-delivery interval was 22.33 ± 13.28 h versus 18.45 ± 14.34 h (p = 0.041) in sequential and concurrent group, respectively. The percentage of women who completed vaginal delivery within 24 h was 51% versus 61% (p = 0.046) in sequential and concurrent group, respectively. Other maternal and neonatal outcomes were similar in both groups
Conclusion
Concurrent use of vaginal misoprostol plus Foley catheter for labor induction was associated with shorter induction-to delivery interval compared to sequential use, and it increases the rate of vaginal delivery in the first 24 h.
Keywords: Concurrent, Foley catheter, Induction, Labor, Misoprostol, Sequential, Vaginal
Introduction
Induction of labor is a frequently experienced intervention in current obstetrics [1]. Induction of labor designates the sequence of artificial cervical ripening and exciting uterine contractions followed by active labor with the aim of completing a vaginal delivery [2]. Labor induction is not without risk but usually done when the risks of continuation of pregnancy outweigh the hazards of labor induction [3]. Recently with steadily increase in rates of labor induction, implementing effective and safe procedures at proper gestation of pregnancy can significantly decrease maternal and fetal complications [4]. Different mechanical and medical methods are used to induce labor, but all of the existing methods are associated with medical risks [5]. Therefore, while choosing labor induction method, the obstetrician should take into account numerous aspects, like cost-effectiveness, safety, and rate of operative delivery [6]. Currently, the most frequently used mechanical method is Foley catheter balloon, which has a dual mechanism of action through mechanical dilatation of the cervix and release of endogenous prostaglandins [7]. Misoprostol is a synthetic analogue of prostaglandin E 1 that was formerly used for the treatment of gastric ulcers. Subsequently, its action on cervical ripening and myometrial contractility was recognized [8]. The combination of mechanical and pharmacological methods for labor induction has been evaluated, and the results are promising [9]. We designed this study to compare between the sequential and concurrent use of vaginal misoprostol plus Foley catheter for labor induction.
Patients and Methods
Our prospective non-blinded randomized controlled clinical trial was carried out in the Department of Obstetrics and Gynecology, Faculty of medicine, Zagazig University, after approval by the Ethics Committee of Zagazig University and a written informed consent was obtained from all participants.
Inclusion criteria were singleton pregnancy, cephalic presentation, full-term pregnancy (based on the first day of last menstrual period or first-trimester sonography), intact membranes, tracing of fetal heart rate for reassurance and the presence of fetal or maternal indications for induction and unfavorable cervix (bishop score ≤ six). Patients with the following criteria were excluded: previous uterine scar, rupture of membranes, placenta previa, intrauterine fetal death, latex allergy, and the presence of contraindications to vaginal delivery.
Consenting eligible women were formerly enrolled in the study and randomized to either sequential or concurrent use of vaginal misoprostol and Foley catheter. The randomization was computer-created and then opaque, sealed, serially numbered envelopes were used to conceal the allocation which were opened by a person not involved in the study before the procedure. The nature of this trial makes it difficult to blind the staff or women to the interference.
For the sequential group, after exposure of the cervix by means of a sterile speculum, a 18 F Foley catheter was introduced into the cervical canal, and then the catheter was fixed through inflation of the balloon with 30 mL of sterile solution when the catheter was beyond the internal cervical os. Slight traction to the catheter was applied through fixing it to inner thigh. Foley catheter was kept in situ till one of the followings happened: (1) spontaneous expulsion, (2) spontaneous rupture of membranes, or (3) maximum period of 12 h was reached, and then 25 μg misoprostol tablet was inserted in the posterior vaginal fornix immediately after removal of Foley catheter and every 4 h up to a maximum of six doses.
For the concurrent group, the 18 F Foley catheter was introduced into the cervical canal using the same technique in the sequential group and, at the same time, 25 μg misoprostol tablet was inserted in the posterior fornix, and then every 4 h up to a maximum of six doses, removal of Foley catheter was practiced under the same conditions of sequential group. For both groups, if frequent and regular uterine contractions were noted (30–50 s every 3 min), the next tablet was not given, failure was considered if active labor did not start 4 h after the last vaginal tablet.
Clinical and demographic data were recorded, primary outcome was induction-to-delivery interval, and secondary outcomes were vaginal delivery within 24 h, number of doses needed to induce labor, need of oxytocin for augmentation of labor, Cesarean section rate, maternal or neonatal complications and abnormalities in uterine contractility like uterine hypertonus (one contraction exceeds two minutes duration), uterine tachysystole (6 or more contractions in 10 min), and if there was non-reassuring fetal heart trace with either condition called uterine hyperstimulation.
According to previous studies which used concurrent vaginal misoprostol plus Foley catheter for induction of labor, the induction-to-delivery intervals were 26.52 ± 15.24 h [10], so the sample size for this study was calculated as 144 women based on an expected mean difference of at least 4 h for induction-to-delivery interval between the two groups with 80% power and α = 0.05.
Collected data were analyzed using Statistical Package for Social Sciences (SPSS version 11.0). The Student’s t test and the Mann–Whitney U test were used for analysis of continuous variables. The Chi-square or Fisher’s exact test were used to compare proportions. Statistical significance was considered when p value <0.05.
Results
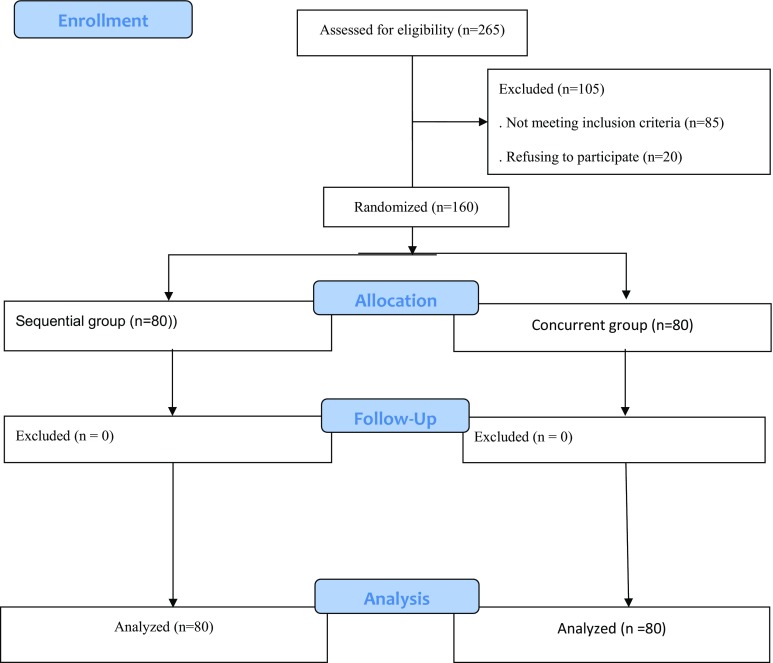
Between January 2016 and January 2017, a total of 265 women were assessed for eligibility; of them 160 gave consent for the study and were randomly allocated to either sequential group (n = 80) or concurrent group (n = 80). No women were excluded from analysis in both groups (Fig. 1).
Fig. 1.
Flow chart of the study
Demographic characteristics of women in both groups were matched (Table 1). The indications for induction of labor were also comparable (Table 2).
Table 1.
Demographic characteristics
| Sequential group (n = 80) | Concurrent group (n = 80) | p value | |
|---|---|---|---|
| Age (years) | 27 ± 3.3 | 27.5 ± 2.9 | 0.81 |
| Parity | |||
| Primigavida | 33 (41%) | 28 (35%) | 0.43 |
| Multigavida | 47 (59%) | 52 (65%) | 0.72 |
| Gestational age (weeks) | 39.7 ± 1.2 | 39.3 ± 1.4 | 0.09 |
| Body mass index | 26.2 ± 7.1 | 26.9 ± 6.8 | 0.84 |
| Bishop score | 2.7 ± 1.4 | 3.2 ± 1.3 | 0.11 |
Data are mean ± SD or number (percentage)
Table 2.
Indications for induction of labor
| Sequential group (n = 80) | Concurrent group (n = 80) | p value | |
|---|---|---|---|
| Pregnancy > 40 weeks | 24 (30%) | 21 (27%) | 0.98 |
| Pre-eclampsia | 12 (15%) | 11 (14%) | 1.0 |
| Oligohydramnios | 10 (12%) | 11 (14%) | 0.9 |
| Intrauterine growth restriction | 7 (9%) | 6 (7%) | 0.91 |
| Diabetes mellitus | 10 (13%) | 10 (12%) | 0.92 |
| Abnormal cardiotocography | 9(11%) | 11 (14%) | 0.86 |
| Others | 8(10%) | 10 (12%) | 0.91 |
Data are number (percentage)
Regarding maternal outcome, induction-to-delivery interval was 22.33 ± 13.28 h in sequential group and 18.45 ± 14.34 h in concurrent group with significant difference between two groups (p = 0.041). The percentage of women who completed vaginal delivery within 24 h was 51% in sequential group and 60% in concurrent group with significant difference (p = 0.046). Other secondary outcomes did not significantly differ between groups: spontaneous vaginal delivery (p = 0.72), operative vaginal delivery (p = 0.88), cesarean section delivery (p = 0.87), number of misoprostol doses (p = 0.9), need of oxytocin (p = 0.71), postpartum pyrexia (p = 0.65), postpartum hemorrhage (p = 0.62), and uterine hyperstimulation (p = 0.12) (Table 3).
Table 3.
Maternal outcome
| Sequential group (n = 80) | Concurrent group (n = 80) | p value | |
|---|---|---|---|
| Induction-to-delivery interval (h) | 22.33 ± 13.28 | 18.45 ± 14.34 | 0.041 |
| Vaginal delivery within 24 h | 41 (51%) | 48(60%) | 0.046 |
| Spontaneous vaginal delivery | 58 (72%) | 59(74%) | 0.72 |
| Operative vaginal delivery | 4 (5%) | 3 (4%) | 0.88 |
| Cesarean section delivery | 18 (23%) | 17(21%) | 0.87 |
| Number of misoprostol doses | 2 ± 0.8 | 2 ± 1.1 | 0.9 |
| Need of oxytocin | 24 (30%) | 21 (26%) | 0.71 |
| Postpartum pyrexia | 4 (5%) | 6 (7%) | 0.65 |
| Postpartum hemorrhage | 5 (8%) | 7 (9%) | 0.62 |
| Uterine hyperstimulation | 2 (3%) | 5 (6%) | 0.12 |
Data are mean ± SD or number (percentage)
Additionally, no significant difference in neonatal outcome parameters was found between sequential and concurrent groups (Table 4).
Table 4.
Neonatal outcome
| Sequential group (n = 80) | Concurrent group (n = 80) | p value | |
|---|---|---|---|
| Birth weight (g) | 3522.5 ± 266.4 | 3547.8 ± 256.6 | 0.72 |
| Apgar score (at 1 min) | 7.79 ± 0.33 | 7.91 ± 0.45 | 0.75 |
| Apgar score (at 5 min) | 8.96 ± 0.22 | 8.89 ± 29 | 0.81 |
| Admission in neonatal intensive care unit | 3 (4%) | 4 (5%) | 0.84 |
| Meconium-stained amniotic fluid | 9 (11%) | 7 (9%) | 0.71 |
Data are mean ± SD or number (percentage)
Discussion
After the recent increase in cases of labor induction, combination of induction methods seems to be more beneficial than current approaches particularly in women with an unfavorable cervix [11].
To the best of our knowledge, no studies have compared between the sequential and concurrent use of vaginal misoprostol plus Foley catheter for induction of labor. Nevertheless, some trials have compared those combinations with single method use.
In the present study, both vaginal misoprostol and Foley catheter were used for induction of labor in sequential and concurrent techniques. The findings reported that induction-to-delivery was significantly shorter with concurrent use of vaginal misoprostol and Foley catheter than sequential use.
There have been many studies which compared the induction-to-delivery interval between combined Foley catheter plus vaginal misoprostol and vaginal misoprostol alone. Lanka et al. [10] stated that combined use of Foley catheter and vaginal misoprostol has resulted in statistically insignificant but clinically relevant reduction in induction-to-delivery interval compared to vaginal misoprostol alone, while other trials [12, 13] found significant reduction in induction-to-delivery interval with the combination of Foley catheter and vaginal misoprostol.
On the other hand, combined use of Foley catheter with oral misoprostol has been studied, and it was found that induction-to-delivery interval was significantly shorter with this combination when compared with oral misoprostol alone [6] or vaginal misoprostol alone [9].
In the present study, the synergistic effect of concurrent use of Foley catheter plus vaginal misoprostol was reflected in the high rate of vaginal deliveries in the first 24 h, and this result was in agreement with that reported by Levine et al. [14], who found that combination of misoprostol and Foley catheter leads to twice the chance of delivering before either single-agent method. But an inconsistent result was reported by Lanka et al., who found no statistically significant difference in the percentage of vaginal deliveries in the first 24 h between combination group and vaginal misoprostol only group.
This study reported that uterine hyperstimulation was not significantly different between concurrent and sequential use of Foley catheter plus vaginal misoprostol, and Lanka et al. documented that uterine hyperstimulation was significantly less with combined Foley catheter plus misoprostol regimen than misoprostol alone, and therefore, we may assume that addition of Foley catheter either concurrently or sequentially to vaginal misoprostol may play a regulatory role for uterine contractions, the proposal, which requires additional trials to specify.
In the current study, there was no statistically significant difference in neonatal outcome between the two groups; a previous study [10] found that the addition of Foley catheter to low-dose misoprostol resulted in reduction in the incidence of meconium-stained liquor compared with low-dose misoprostol alone.
A sequential regimen of intracervical Foley catheter followed by misoprostol for cervical ripening and induction of labor was adopted by a small number of studies. Kehl et al. [15] have compared sequential use of double-balloon catheter and oral misoprostol with oral misoprostol alone and reported that this sequential combination neither results in reduction in induction-to-delivery interval nor increases the percentage of delivery within 48 h, and the inconsistency of these findings with our results appears to be as a result of difference in type of catheters used, route of misoprostol administration, and time lag between catheter removal and misoprostol insertion. However, when the sequential use of intracervical Foley catheter and intravaginal misoprostol was practiced, it was found that there was a significant shortening of induction-to-delivery interval, more vaginal deliveries within 12 h, and less Cesarean section compared with vaginal misoprostol alone [11].
Despite the fact that the randomized design provided strength to this study, it was limited by the inability to blind the interventions. Also, the study was not powerful enough to detect statistically significant difference in most of maternal outcomes and neonatal outcomes. Accordingly, further multicenter trials with huge sample size are needed to confirm the safety and effectiveness of those methods.
In conclusion, the current study declares that concurrent use of vaginal misoprostol plus Foley catheter for induction of labor was associated with a statistically significant reduction in induction-to-delivery interval and statistically significant increase in a number of vaginal deliveries in first 24 h compared to the sequential use. No statistically significant difference in neonatal outcomes was detected between the two groups.
Ibrahim Abd Elgafor el Sharkwy, MD
is an Assistant professor, Faculty of Medicine, Zagazig University, Zagazig, Egypt. He has many papers published in the field of Obstetrics and Gynecology. His fields of interest are feto-maternal medicine and laparoscopic surgery.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Ibrahim Abd Elgafor el Sharkwy (MD) is Assistant Professor of Faculty of Medicine, Zagazig University, Zagazig, Egypt.
Contributor Information
Ibrahim Abd Elgafor El Sharkwy, Phone: 00966554818576, Email: ibrahimsharkwy@yahoo.com.
Elsayed Hamdy Noureldin, Phone: 00966558982184, Email: Elsayed_hamdi2002@yahoo.com.
Ekramy Abd Elmoneim Mohamed, Phone: 00966538162924, Email: Drekramy2000@gmail.com.
Sherine Attia Shazly, Phone: 0001225570423, Email: Sherinshazly73@gmail.com.
References
- 1.Geeta K, Swamy MD. Current methods of labor induction. Semin Perinatol. 2012;36(5):348–352. doi: 10.1053/j.semperi.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 2.Induction of Labor. Royal College of Obstetricians. and Gynaecologists. 2008: Available: http://www.rcog.org.uk. Accessed 2012 June 26.
- 3.Mozurkewich E, Chilimigras J, Koepke K, Keeton K, King VJ. Indications for induction of labor: a best-evidence review. BJOG. 2009;116(5):626–636. doi: 10.1111/j.1471-0528.2008.02065.x. [DOI] [PubMed] [Google Scholar]
- 4.Gulmezoglu AM, Crowther CA, Middleton P, Healy E. Induction of labor for improving birth outcomes for women at or beyond term. Cochrane Database Syst Rev 2012; CD004945. doi:10.1002/14651858.CD004945.pub3. [DOI] [PMC free article] [PubMed]
- 5.Jozwiak M, Bloemenkamp KW, Kelly AJ, Mol BW, Irion O, Boulvain M. Mechanical methods for induction of labour. Cochrane Database Syst Rev. 2012;3:333. doi: 10.1002/14651858.CD001233.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Kehl S, Ehard A, Berlit S, Spaich S, Sutterlin M, Siemer J. Combination of misoprostol and mechanical dilation for induction of labor: a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2011;159:315–319. doi: 10.1016/j.ejogrb.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 7.Cromi A, Ghezzi F, Uccella S, Agosti M, Serati M, Marchitelli G, et al. A randomized trial of preinduction cervical ripening: dinoprostone vaginal insert versus double-balloon catheter. Am J Obstet Gynecol. 2012;207:125-e1. doi: 10.1016/j.ajog.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 8.Adeniyi AA, Odukogbe AA, Olayemi A, Oladokun O, Adeniji AO, Aimakhu CO, et al. Randomization of two dosing regimens of vaginal misoprostol for cervical ripening and labor induction in a low resource setting. Niger J Clin Pract. 2014;17:287–291. doi: 10.4103/1119-3077.130227. [DOI] [PubMed] [Google Scholar]
- 9.Hill JB, Thigpen BD, Bofill JA, Magann E, Moore LE, Martin JN., Jr A randomized clinical trial comparing vaginal misoprostol versus cervical Foley plus oral misoprostol for cervical ripening and labor induction. Am J Perinatol. 2009;26:33–38. doi: 10.1055/s-0028-1091396. [DOI] [PubMed] [Google Scholar]
- 10.Lanka S, Surapaneni T, Nirmalan PK. Concurrent use of Foley catheter and misoprostol for induction of labor: a randomized clinical trial of efficacy and safety. J Obstet Gynaecol Res. 2014;40:1527–1533. doi: 10.1111/jog.12396. [DOI] [PubMed] [Google Scholar]
- 11.Ande AB, Ezeanochie CM, Olagbuji NB. Induction of labor in prolonged pregnancy with unfavorable cervix: comparison of sequential intracervical Foley catheter-intravaginal misoprostol and intravaginal misoprostol alone. Arch Gynecol Obstet. 2012;285:967–971. doi: 10.1007/s00404-011-2094-4. [DOI] [PubMed] [Google Scholar]
- 12.Carbone JF, Tuuli MG, Fogertey PJ, Roehl KA, Macones GA. Combination of Foley bulb and vaginal misoprostol compared with vaginal misoprostol alone for cervical ripening and labor induction: a randomized controlled trial. Obstet Gynecol. 2013;121:247–252. doi: 10.1097/AOG.0b013e31827e5dca. [DOI] [PubMed] [Google Scholar]
- 13.Hussein M. A comparison between vaginal misoprostol and a combination of misoprostol and Foley catheter for cervical ripening and labor induction in early third Trimester pregnancy. Am J Obstet Gynecol. 2012;206:147. doi: 10.1016/j.ajog.2011.10.325. [DOI] [Google Scholar]
- 14.Levine LD, Downes KL, Elovitz MA, Parry S, Sammel MD, Srinivas SK. Mechanical and pharmacologic methods of labor induction: a randomized controlled trial. Obstet Gynecol. 2016;6:1357–1364. doi: 10.1097/AOG.0000000000001778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kehl S, Ziegler J, Schleussner E, Tuschy B, Berlit S, Kirscht J, et al. Sequential use of double-balloon catheter and oral misoprostol versus oral misoprostol alone for induction of labor at term (CRB plus trial): a multicentre, open-label randomized controlled trial. BJOG. 2015;122:129–136. doi: 10.1111/1471-0528.13116. [DOI] [PubMed] [Google Scholar]