Introduction
Benign prostatic hyperplasia and prostatic cancer are one of the common diseases of the elderly male, with millions of men getting affected each year. These commonly result in bladder outlet obstruction symptoms, including lower urinary tract symptoms such as acute urinary retention, hematuria, and urinary tract infections. Different medical and surgical modalities are available for treatment of these pathologies. Among the surgical options, transurethral resection of prostate (TURP) is a standard procedure. Although relatively safe, there is a rare post-surgical complication called prostatosymphyseal fistula, which can be categorically difficult to diagnose and treat. As the name suggests, there is a fistula formation from the urinary tract to pubic symphysis, which can lead to osteitis, osteomyelitis or osteonecrosis of the bone, in addition to urinary tract symptoms.
Case report
The patient is a 57 years old male who presented with one month of progressively worsening pain in the pubic region, right more than left. The pain is worse when standing or walking, without associated history of trauma. The patient was unable to ambulate without the use of a cane. Patient also stated that he was experiencing symptoms related to urinary retention. At presentation, the patient was afebrile, with normal vital signs. There was no elevated white blood cells, or other laboratory abnormalities to suggest infection. Further questioning elucidated a complicated urologic history. Briefly, the patient underwent a Transurethral resection of the prostate (TURP) approximately three months prior to presentation. Although he experienced initial relief of symptoms after the TURP, voiding difficulty returned shortly after TURP. He was then taken for a second TURP one month after the first procedure, with direct vision internal urethrotomy for a distal fossa navicularis stricture. The patient again experienced a short period of symptomatic relief, before the gradual onset of increasing low suprapubic pain.
An outpatient pelvic radiograph performed a week prior was unremarkable for fractures. A magnetic resonance imaging (MRI) of the pelvis demonstrated an anterior defect of the prostatic urethra, which communicates with the pubic symphysis (Fig. 1). The signal abnormality at the pelvic insertion of the left adductor muscles was felt to be related to urine leak. A subsequent computed tomography (CT) cystogram showed extravasation of instilled contrast into the pubic symphysis (Fig. 2). A foley catheter with low intermittent suction was inserted at this time, with great relief of the patient. He was admitted for observation for 4 days, remained afebrile during the admission, and was discharged to home care with an indwelling foley catheter. The patient was planned for robotic versus radical prostatectomy in the eventuality that the fistula does not heal. However, after 4 weeks of indwelling foley catheter, a repeat CT cystogram did not showed any contrast extravasation, compatible with healing of the fistula without residual defect (Fig. 3).
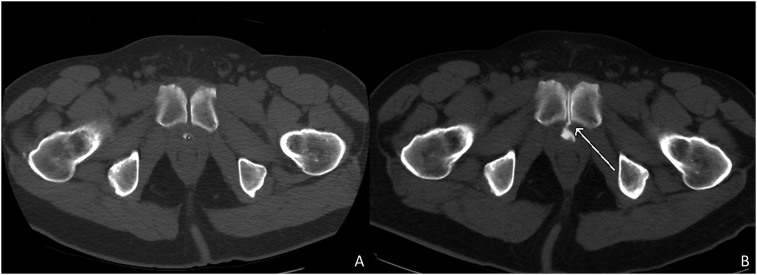
Fig. 1.
T2 weighted MRI image in the axial plane with fat saturation. A T2 hyperintense region is seen in the pubic symphysis and communicates with the prostatic urethra. Slight hyperintensity in the left adductor muscle is thought to be related to urine leak without a discrete collection.
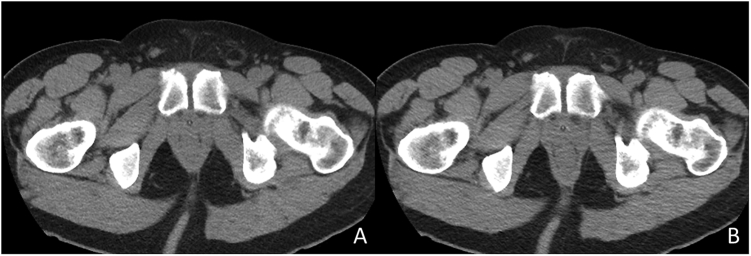
Fig. 2.
CT axial images at similar levels obtained during (2A) and after voiding cystogram (2B). After withdrawing the Foley catheter, contrast is seen communicating with the urethra as well as in the pubic symphysis.
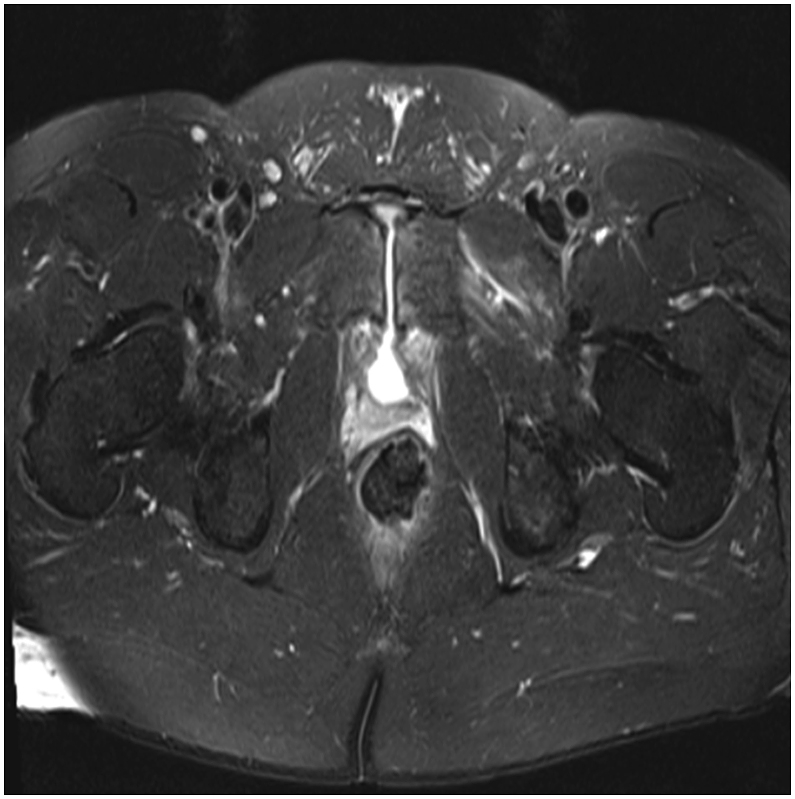
Fig. 3.
A repeat CT cystogram during (3A) and after voiding cystogram (3B) performed after placement of indwelling Foley for 4 weeks. There is no evidence of contrast in the pubic symphysis, consistent with healing of the prostatosymphyseal fistula.
Discussion
Chronic pelvic pain after surgical and non-surgical treatment of prostate cancer has been commonly attributed to osteitis pubis, osteonecrosis or osteomyelitis.1 Fistulization into rectum and perineum is also known.2 However, direct fistula formation from the urinary tract into the pubic symphysis, also known as prostato-symphyseal fistula (PSF), is a rare complication. Isolated cases are reported in literature after TURP, prostate cancer treatment, bladder tumors, salvage cryotherapy, transrectal biopsy of prostate, radical prostatectomy and radiotherapy, with the largest case series including only 16 patients.2 The diagnosis is often delayed due to the unexpected orthopedic and infective symptoms similar to our patient. Common symptoms include difficulty ambulating, pain in the suprapubic or pelvic, lower abdominal, inguinal or groin regions. Even radiological investigations may yield nonspecific findings like osteitis pubis or urinoma. It is usually due to persistent symptoms that alerts the clinician for an alternative diagnosis. Complications like UTI, infected urinomas, osteomyelitis or more debilitating cavitation and chronic pelvic sepsis may occur by the time of diagnosis. Cystoscopy with a rigid scope also has a limited role in assessment of anterior structures including anterior part of the prostate.3
The most common risk factor for osteitis pubis and subsequent PSF is a capsular trauma. This could be secondary to weakening caused by prior radiotherapy or inadvertent perforation during surgery.3 During PVP, there is creation of a possible hypo-vascular zone beyond what is visualized, which may ultimately necrose and slough off. Bleeding caused by capsular perforation and the subsequent use of prolonged coagulation leading to tissue necrosis may be additional contributing factor in pathogenesis. Augmented by the use of indwelling catheter, secondary bacterial infection can inoculate the pubic symphysis resulting in osteomyelitis of the pubis and subsequently PSF.4
The initial work up can reveal leukocytosis, elevated ESR and CRP. Blood cultures are usually sterile. CT and MRI are usually used for initial work up of these symptoms. CT images at excretory phase can be used to assess the presence of urine within the joint space. It can also demonstrate an abscess formation.5 MRI is more sensitive in its capacity to show inflammatory changes within the pubis or the adjacent soft tissues and evidence of osteomyelitis.4 Definitive diagnosis is provided by cystoscopy, which can reveal the actual fistulous tract from prostate to the pubic symphysis.
Conservative management with catheterization alone is the initial approach; however it eventually requires a surgical repair. Radical prostatectomies and open fistula repair with omental or peritoneal flaps have been successfully performed. Reconstructions of the lower urinary tract is however limited if the patient had prior pelvic radiation.2 Minimally invasive robotic surgery involving prostatectomy and reconstruction has also been reported as a safe treatment modality, with instrument proficiency and ability to mobilize omentum robotically being the main considerations.3
Conclusion
Prostatosymphyseal fistula is a rare complication secondary to various therapeutic options for prostate hyperplasia and prostate cancer. It is very debilitating for the patient. Delay in presentation and limited role of diagnostic modalities make it a clinical dilemma. Even after diagnosis, the management is complicated with a multidisciplinary involvement of urology, orthopedic surgery and infectious disease specialists. Hence, the clinician performing procedures like TURP, PVP or radiotherapy should be cognizant of the possibility of PSF, especially if the patient returns with orthopedic or early neurological or persistent infective symptoms.
Consent
The appropriate consent was obtained.
Conflicts of interest
There is no conflict of interest.
Disclosure
There is no financial or personal relationships to disclose.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eucr.2018.07.018.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Knoeller S.M., Uhl M., Herget G.W. Osteitis or osteomyelitis of the pubis? A diagnostic and therapeutic challenge: report of 9 cases and review of the literature. Acta Orthop Belg. 2006;72(5):541. [PubMed] [Google Scholar]
- 2.Bugeja S., Andrich D.E., Mundy A.R. Fistulation into the pubic symphysis after treatment of prostate cancer: an important and surgically correctable complication. J Urol. 2016;195(2):391–398. doi: 10.1016/j.juro.2015.08.074. [DOI] [PubMed] [Google Scholar]
- 3.Whelan L., Mullarkey E., Woo H.H. Prostatosymphyseal fistula treated by robotic assisted radical prostatectomy. Case Rep Urol. 2015:2015. doi: 10.1155/2015/582705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plateau B., Ruivard M., Montoriol P. Prostatosymphyseal fistula and osteomyelitis pubis following transurethral resection of the prostate: CT and MRI findings. J Med Imaging Rad Oncol. 2015;59(6):713–715. doi: 10.1111/1754-9485.12304. [DOI] [PubMed] [Google Scholar]
- 5.Kats E., Venema P., Kropman R., Kieft G. Diagnosis and treatment of osteitis pubis caused by a prostate-symphysis fistula: a rare complication after transurethral resection of the prostate. Br J Urol. 1998;81:927–928. doi: 10.1046/j.1464-410x.1998.00606.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.