Introduction
Testicular cancer, which accounts for only 1% of all male cancers, is the most common cancer in men aged from 15 to 35 years. Germ cell tumors account for 90%–95% of cases. Of these germ-tumors, the non-seminomatous form (NSGCT) is the most common metastasis affecting the lungs, liver, central nervous system and bone in order of frequency. The frequency of brain metastases is very low, not exceeding 1.2%. The treatment is based on excision and chemotherapy and the prognosis remains moderately good with a 5-year survival rate of around 96%.
Case report
This is a 26-year-old man with a history of testicular mixed NSTCG confirmed after orchidectomy stage of pericardial, pulmonary, peritoneal and lymph node metastasis under radiotherapy and chemotherapy who is admitted for an intracranial hypertension syndrome with gait and left coordination disorder of a rapidly progressive installation. The neurological examination shows a static and kinetic left cerebellar syndrome. CT scan showed a 4-cm irregular mass of the posterior fossa with perilesional edema and significant mass effect on the bulb and the 4th ventricle (Fig. 1). MRI showed the unique left cerebellar hemorrhagic and hyper perfused (2–3 times the normal perfusion) lesion exerting a mass effect on the 4th ventricle and the bulb. On T1, it was hypo-intese but hyper-intense on T2 weighted images with intensive enhancement and surrounded by perilesional edema (Fig. 2). The patient underwent an excision of a greyish firm and hemorrhagic lesion by a sub-occipital approach. The histopathological examination objectivied a large cerebellar infiltration by tumor proliferation of reticulate and microalveolar architecture (Shiller-Dural body) (Fig. 3a). There are two components intimately entangled: Yolk sac components (95%) (Fig. 3b) and seminomatous ones (5%) (Fig. 3c). The immunohistochemical study showed that the Yolk sac components are positive for APF, NSE and CK (Fig. 3d). The seminomatous components are positive for PLAP (Fig. 3e). After surgery the patient underwent radiotherapy and chemotherapy and he has kept as a sequela a left kinetic cerebellar syndrome at 13 months postoperatively.
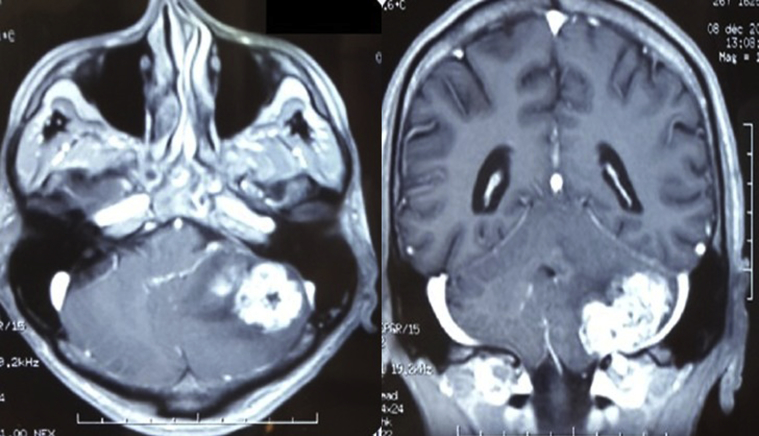
Fig. 1.
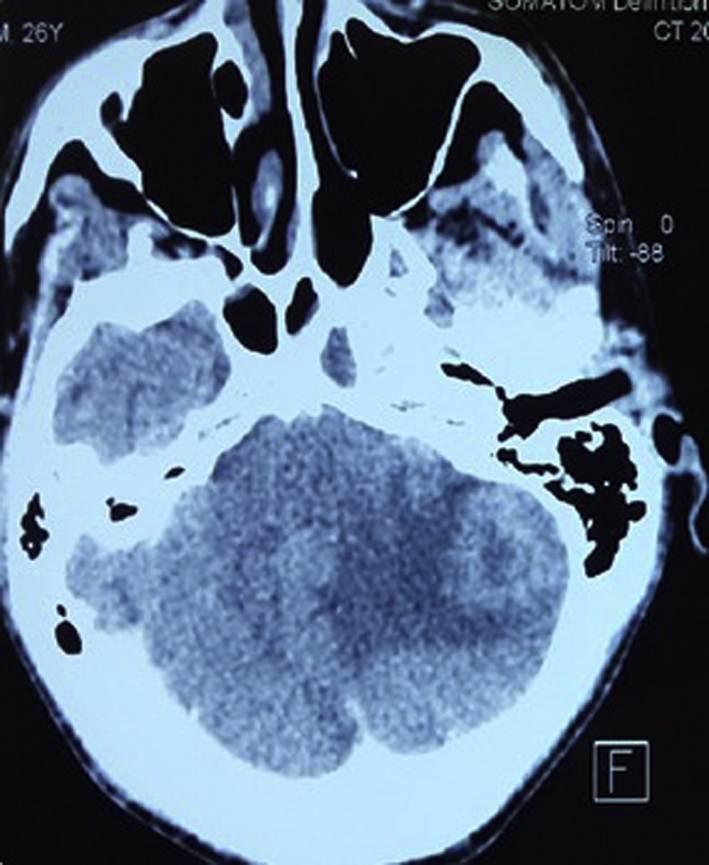
Lesion of the posterior fossa with perilesional edema and significant mass effect on the bulb and the fourth ventricle.
Fig. 2.
The left cerebellar hemorrhagic lesion: On T1: hypo-intense; hyper-intense on T2 weighted images with intensive enhancement and perilesional edema.
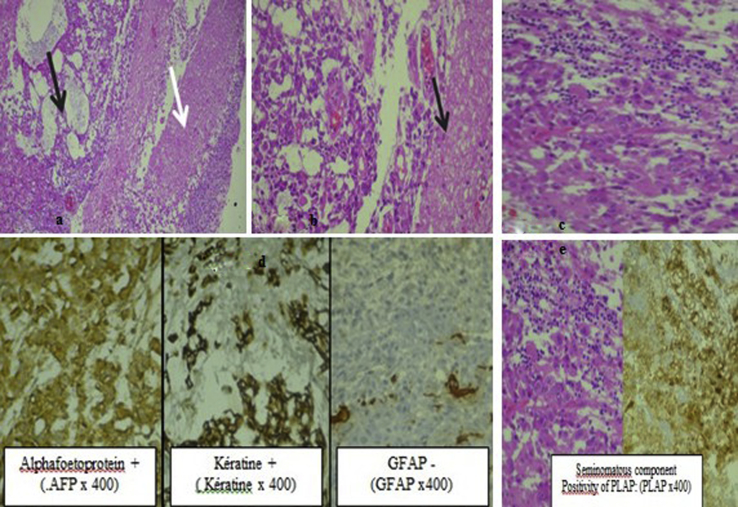
Fig. 3.
a: Cerebral infiltration (white arrow) by tumor proliferation of reticulate and microalveolar architecture (black arrow) (HE x 200) b: Yolk sac component: tumor proliferation of reticulate and micro-alveolar architecture (Shiller-Dural body). Note the glial tissue at the right side (HE x 400) c: Seminomatous component (HEx400) d: immunohistochemical study:Yolk sac component positivity e: immunohistochemical study Seminomatous component Positivity of PLAP (PLAP x400).
Discussion
Non-seminomatous germ-cell tumors (NSGCT) account for 40% of testicular tumors. They associates with variable percentages the different tumor components as embryonic carcinoma, teratoma, yolk sac tumor and choriocarcinoma. A seminomatous component may also persist in these TGNS.1These are embryonic tumors that develop from totipotent stem cells. They affect younger patients, from puberty to age of 35. These are rapidly systemic diseases as opposed to other forms.2 Its metastasis are made mainly by lymphatic and hematogenous way. The sites of predilection for lymph node metastases are lumbo-aortic. Heterogeneous metastatic spread primarily concerns the lung, secondarily the liver, and more rarely the brain and bone.1 The cerebral localization, in the IGCCCG register, remains rare not exceeding 1.2%.
In the rare cases of these reported metastases, the clinical symptoms had no specificity.
Radilogically, these lesions also show no specificity and presented as often haemorrhagic lesions heterogeneously inhanced which is correlated to our case.
With regard to treatment, it must strive to be surgical where it is possible.3 Chemotherapy finds here all its indications given the chemo sensitivity of these lesions. Radiation therapy has only been shown to have a healing effect in small tumors; in fact, according to Peckham and Barrett, the success rates of radiotherapy for the elimination of NSGCT metastases are: 100% for metastases less than 1 cm in diameter, 75% for those between 1 cm and 2 cm, 31% for those over 2 cm and 0% for those over 6 cm.4 In some cases, radiosurgery may be discussed and the experience of cyberknife treatment remains very limited.
Patient survival was higher in cases of synchronous metastasis compared with metachronous one that appear after induction chemotherap. In the case of metachronous metastases that appear after induction chemotherapy, patient survival was lower if other metastatic metachronous sites were present.5 It is likely that the blood-brain barrier decreased the effectiveness of chemotherapy on brain metastases.5
In cases of isolated metachronic brain metastasis, local treatment with radiotherapy or surgery may be sufficient.
The prognosis is more pejorative in case of multiple metastases but, on the other hand, it is more favorable for patients in whom the cerebral metastases are present from the onset of the pathology comparing to those in whom it occurs during the evolution. The presence of trophoblastic contingents could influence survival.3
Conclusion
The cerebral metastasis of TGNS remains a rare pathology. The clinic is very variant and the imaging is not characteristic enough. The treatment combines surgery, chemotherapy and radiotherapy. The prognosis is good in case of single lesion and becomes more pejorative in case of multiple metastases.
Conflicts of interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Contributor Information
Mehdi Borni, Email: borni.mehdi13@gmail.com.
Fatma Kolsi, Email: kolsineifar.fatma@gmail.com.
Brahim Kammoun, Email: kammoun.brahim28@gmail.com.
Rim Kallel, Email: rim.kallel@yahoo.fr.
Ghassen Souissi, Email: souissighassen@yahoo.fr.
Mohamed Zaher Boudawara, Email: zaher.boudawara@rns.tn.
References
- 1.http://www.urofrance.org/congres-et-formations/formation-initiale/referentiel-du-college/tumeurs-du-testicule.html.
- 2.http://www.arcagy.org/infocancer/localisations/cancers-masculins/cancer-du-testicule/formes-de-la-maladie/les-tumeurs-germinales.html.
- 3.Tumeurs germinales du testicule et métastases cérébrales : quand le cerveau prime sur le testicule. P. Beuzeboc, B. Debre, V. Laurence, F. Selle, J.P. Lotz. Correspondances en Onco-Urologie - Vol. II - n° 2 - avril-mai-juin 2011 9.
- 4.Peckham M.J., Barrett A., Liew K.H. The treatment of metastatic germ-cell testicular tumours with bleomycin, etoposide and cis-platin (BEP) Br J Canc. 1983;47:613–6199. doi: 10.1038/bjc.1983.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Azar J.M., Schneider B.P., Einhorn L.H. Is the blood-brain barrier, relevant in metastatic germ cell tumor? Int J Radiat Oncol Biol Phys. 2007;69:163–166. doi: 10.1016/j.ijrobp.2007.02.042. [DOI] [PubMed] [Google Scholar]