Introduction
Fatty tumors of the retroperitoneum are rare and represent a real dilemma for urologist. Distinguishing between liposarcoma whish is a poor prognosis tumor and lipoma which is a benign tumor is sometimes difficult. We report the case of a 26 year-old, women presenting a giant fatty retroperitoneal mass measuring 17 × 10 cm.
Through this case we report the management of the patient and we discuss diagnostic difficulties and treatment.
Case
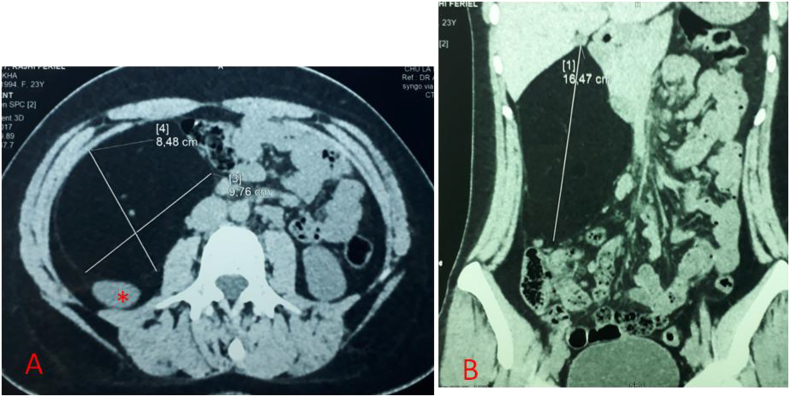
A 26- year-old woman was referred to our center with a giant retroperitoneal mass. The patient complained about abdominal swelling and recurrent episodes of abdominal pain. Computed Tomography (CT) scan of the abdomen and pelvis showed a mass arising in the retroperitoneum. It was a homogenous hypodense mass surrounded by a thin capsule, well limited, measuring 10 × 8 × 17 cm and containing few thin septa. This mass was diagnosed as a lipoma by radiologist (Fig. 1A). The mass was in contact with the inferior vena cava, under the right kidney which was compressed on the posterior abdominal wall and represses the peritoneal containing to the left part of abdomen (Fig. 1B). No significant contrast enhancement was detected. We considered the mass resectable however very close to the right kidney. An open biopsy and intraoperative judgment helped the decision of complete resection of the tumor rather than en-bloc removal of the mass and right kidney.
Fig. 1.
A: Contrast enhanced CT scan in the axial plane showing a giant homogenous mass, mainly consisting of fat tissue surrounded by a thin capsule arising in the retroperitoneum pushing the right kidney to the posterior wall (*). B: Contrast enhanced CT scan in the coronal plane showing a 17 cm retroperitoneal mass repressing organs to the left and lower part of the abdomen.
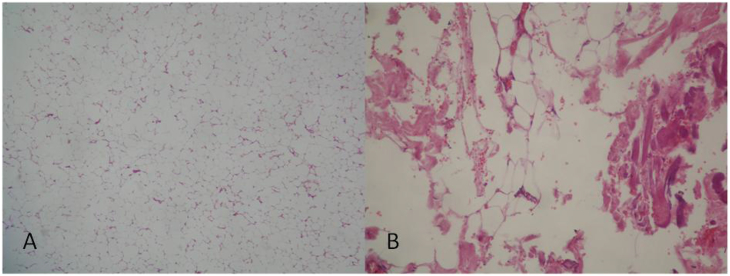
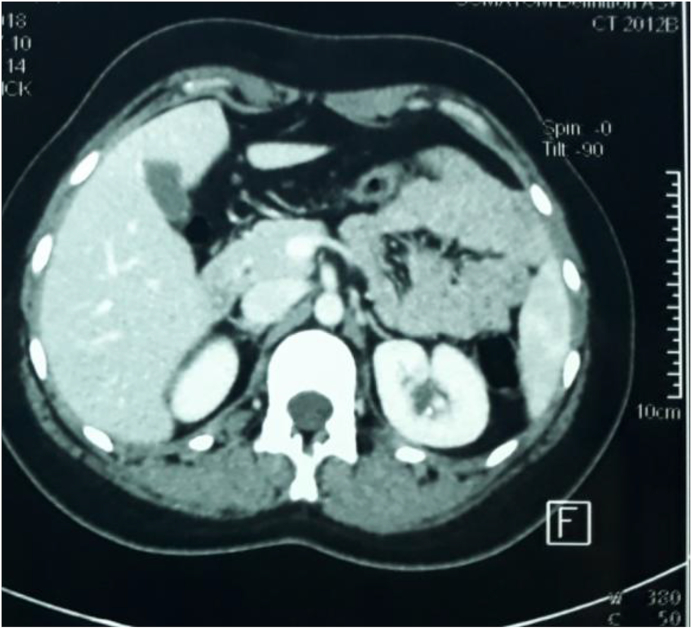
The patient was operated through a Kocher incision. We found a giant clearly encapsulated fatty tumor deriving from the right retroperitoneal fatty tissue. An open biopsy of 3 cm in size was performed. Frozen section examination concluded to a retroperitoneal adipocytic tumor without cytologic atypia. The mass was completely extirpated without resection of adjacent tissue or organs. The patient was discharged on the fourth postoperative day without complications. The final histopathological report showed a well-differentiated liposarcoma of the retroperitoneum with mature adipocytic proliferation and presence of atypical, hyperchromatic stromal cells with lipoblasts (Fig. 2A and B). At 1 year post-surgery, there was no evidence of recurrence on different CT scans (Fig. 3).
Fig. 2.
A: Histological examination showed a mature adipocytic proliferation with variation in cell size. (Hematoxylin-Eosin, x 20). B: Histological examination showed presence of atypical, hyperchromatic stromal cells with a varying number of lipoblasts. (Hematoxylin-Eosin, x 40).
Fig. 3.
Contrast enhanced CT scan in the axial plane after 1 year of follow up, showing no signs of recurrence.
Discussion
Liposarcomas represent the most common type of sarcoma arising in the retroperitoneum. The rarity of retroperitoneal liposarcomas and the variety of histologic subtypes make it difficult to understand and treat this neoplasm.1 The distinction between lipoma and well-differentiated liposarcoma is a frequent diagnostic dilemma. Computed tomography (CT) imaging features that suggest malignancy include large lesion size, presence of thick septa, presence of nodular and/or globular or non adipose masslike areas, and decreased percentage of fat composition.2 Histopathology is fundamental for the diagnostic workup of lipomatous tumors. It can show fibrillar fibrous septa containing enlarged hyperchromatic cells and rare lipoblasts. However, there are some lipoma-like well differentiated liposarcoma that may be extremely difficult to distinguish confidently from lipoma due to their extreme paucity of hyperchromatic cells and lipoblasts.3 In that case an immunohistochemical panel composed of MDM2 and CDK4 is recommended. Fluorescence in situ hybridization (FISH) for MDM2 amplification can be useful to discriminate lipomas from atypical lipomatous tumor and well-differentiated Liposarcomas.4 In our case, MDM2 and CDK4 are unfortunately unavailable. Surgery is the mainstay of treatment of non-metastatic retroperitoneal lipomatous tumors. Whenever is possible, a macroscopically complete resection should be aimed at, often requiring en-bloc removal of adjacent structures.5 In case of unresectability or patients with hematogenous metastases a biopsy should be reserved. Tissue may be obtained through fine-needle aspiration or core-needle biopsy. Percutaneous biopsies are reliable and safe. However, percutaneous techniques have a low subtype specific diagnostic in liposarcoma. In our case, CT scan images and frozen section examination concluded to a retroperitoneal lipoma however final histological examination showed presence of atypical, hyperchromatic stromal cells confirming the diagnosis of well-differentiated liposarcoma. The current guidelines from the National Comprehensive Cancer Network for the surveillance of retroperitoneal sarcomas recommend that patients with low-grade tumors who have been successfully resected should have a follow-up physical examination with imaging (chest/abdominal/pelvic CT) every 3–6 months for 2–3 years, then annually.
Conclusion
The distinction of lipoma-like well-differentiated liposarcoma from lipoma is difficult. The large lesion size, presence of thick septa, presence of nodular areas on CT scan, intraoperative judgment and mature adipose tissue on histology could make the diagnosis. Molecular testing could be useful in the differential diagnosis of lipomatous tumors. The resection should be complete with a strict follow up.
Conflicts of interest
None for all authors.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Vijay A., Ram L. Retroperitoneal liposarcoma : a comprehensive review. Am J Clin Oncol. 2015 doi: 10.1097/COC.0b013e31829b5667. [DOI] [PubMed] [Google Scholar]
- 2.Kransdorf MJ, Bancroft LW, Peterson JJ, et al. Imaging of fatty tumors: distinction of lipoma and well-differentiated liposarcoma. Radiology DOI:10.1148/radiol.2241011113. [DOI] [PubMed]
- 3.Macarenco R.S., Erickson-Johnson M., Wang X. Retroperitoneal lipomatous tumors without cytologic atypia: are they lipomas? A clinicopathologic and molecular study of 19 cases. Am J Surg Pathol. 2009 doi: 10.1097/PAS.0b013e3181b278bf. [DOI] [PubMed] [Google Scholar]
- 4.Clay M.R., Martinez A.P., Weiss S.W. MDM2 amplification in problematic lipomatous tumors: analysis of FISH testing criteria. Am J Surg Pathol. 2015 doi: 10.1097/PAS.0000000000000468. [DOI] [PubMed] [Google Scholar]
- 5.Lucas D.R., Nascimento A.G., Sanjay B.K. Well-differentiated liposarcoma. The Mayo Clinic experience with 58 cases. Am J Clin Pathol. 1994 Nov;102(5):677–683. doi: 10.1093/ajcp/102.5.677. PMID: 7942636. [DOI] [PubMed] [Google Scholar]