Abstract
Rationale:
Harsh, abusive and rejecting behavior by parents toward their adolescents is associated with increased risk of many developmental problems for youth.
Objective:
In the present study we address behaviors of co-parents that might help disrupt the hypothesized health risk of harsh parenting.
Method:
Data come from a community study of 451 early adolescents followed into adulthood. During early adolescence, observers rated both parents separately on harshness towards the adolescent. Adolescents reported on their physical health at multiple assessments from age 12 through age 20, and on parental warmth.
Results:
Harsh parenting predicted declines in adolescent self-reported physical health and increases in adolescent body mass index (BMI). Although the health risk associated with harshness from one parent was buffered by warmth from the other parent, warmth from the second parent augmented the association between harshness from the first parent and change over time in adolescent BMI.
Conclusion:
As appropriate, preventive interventions should include a focus on spousal or partner behaviors in their educational or treatment programs. Additional research is needed on the association between self-reported physical health and BMI in adolescence.
Keywords: Child maltreatment, Child rearing, Parenting, Safe, Stable nurturing relationships (SSNRs)
1. Introduction
Harsh parenting is associated with poorer child physical health (Brody et al., 2013; Miller, Chen, & Parker, 2011; Repetti et al., 2002) including long-term effects on health outcomes (Dube et al., 2009; Wegman and Stetler, 2009). This association is often attributed to a causal effect of harsh parenting on the adolescent’s biological functioning (Miller et al., 2011; Shonkoff et al., 2009) and healthrelated behaviors (Anda et al., 1999; Hillis et al., 2001). In other words, harsh parenting is thought to have a negative influence over time on physical health. However, this literature is based principally on cross-sectional retrospective reports, which provide limited evidence for causal claims due to their significant limitations (Hardt and Rutter, 2004). In the present study, we examined the association between parental harshness and changes in adolescent physical health over time using prospective longitudinal data.
As evidenced by the modest effect sizes from prior studies (e.g., Brody et al., 2013), some children and adolescents may be less subject to the hypothesized health risks of harsh parenting than others. Theoretical work suggests that positivity in the context of close relationships (Pietromonaco et al., 2013) is health protective, and this idea is supported by cross-sectional data from both human populations (Schafer et al., 2014) and nonhuman populations (Francis and Meaney, 1999; Meaney and Szyf, 2005). In the current study we assess the degree to which warmth from one parent buffers the hypothesized health risk of harshness from the other parent during adolescence.
1.1. Harsh parenting and physical health
Harsh parenting includes negative affect, potentially physical aggression, and is driven more by the parent’s emotional reactions than the best interests of the child (Rueger et al., 2011). Our hypothesis of harsh parenting predicting changes in physical health draws heavily from the theoretical framework of Biological Embedding (Bush and Boyce, 2014; Hertzman, 2012; Miller et al., 2011). According to this framework, early stress that is chronic and severe potentiates the expression of physiological responses that anticipate continuity in those environmental characteristics. That is, from white blood cell activity, to hormone release, to potentiation of neurotransmitter receptor sites, the body shifts to a high-vigilance state that leads to a “weathering” effect on health including premature aging, and early onset of chronic disease.
In a recent review, Miller et al. (2011) report that child health is affected by stress that is severe, and chronic. They define severe stress as “difficulties that fall outside the normal range of what children normatively experience in developed countries” (p. 960) and chronic stress as “an experience where the stimulus [or threat posed by a stimulus] remains present in the child’s life over a lengthy period of time” (p. 960).” In the current study, we propose that parents who reject, coerce, hit, and are self-centered during a video recorded interaction with their child fall outside the normal range of expected child experience in developed countries. Parenting behavior is stable over time (Schofield and Weaver, 2015), and most children are exposed to their parents’ behavior for almost two decades. This supports classifying harsh parenting as a chronic stressful environment (Brody et al. 2013; Repetti et al., 2002; Shonkoff et al., 2009). Acknowledgement of the potential role of harsh parenting on physical health is particularly important because of the exposure period. The developing brain is relatively more receptive to environmental signals during childhood and adolescence (Barker et al., 2005; Johnson, 2005), and the resulting effects can last throughout the lifespan (McGowan, Sasaki, D’Alessio et al., 2009; Wegman and Steller, 2009).
There are several reasons to expect that harsh parenting could affect adolescent’s metabolism and physical health. Central to the biological embedding framework is biological mediation. For example, when parents are harsh, the adolescent’s emotional needs are unlikely to be met (Cicchetti and Toth, 2005), which results in deficits in emotion regulation (Brody et al., 2013). This process, in turn, could affect health through chronic release of catecholamines and hormones like cortisol from the hypothal-amic-pituitary-adrenal (HPA) axis and the sympathetic-adrenalmedullary systems (Black, 2006). These neurobiological responses to stress that are adaptive under normative conditions of intermittent stress become pathogenic under conditions of chronic or overwhelming stress (Boyce and Ellis, 2005; McEwen, 1998). An additional reason suggested by the biological embedding framework for harsh parenting to affect adolescent’s physical health is that harsh parenting lowers cardiovascular reactivity (Johnston-Brooks et al., 1998). A final reason is that harsh parenting is associated with reductions in the children’s health-promoting behaviors such as practicing safe sex or abstaining from smoking (Anda et al., 1999; Hillis et al., 2001).
Consistent with these ideas, growing up in a harsh family environment is negatively associated with physical health, growth, and development (Mechanic and Hansell, 1989; Montgomery et al., 1997; Russek and Schwartz, 1997; Stein et al., 1994; Weidner et al., 1992; Williamson et al., 2002), and positively associated with obesity (Siervo et al., 2009). Empirical support for a causal effect of harsh parenting on physical health does not yet include prediction from harsh parenting to changes over time in physical health; this absence is widely acknowledged as a significant limitation of existing research (Berger and Zolotor, 2013; Fergusson et al., 2008; Schafer et al., 2014). The meta-analysis on this area of research conducted by Wegman and Stetler (2009) identified only one prospective longitudinal study, and that did not attempt to predict changes in health (White and Widom, 2003). Without prospective longitudinal tests for a health risk of harsh parenting, the empirical support for this widely-assumed link from harsh parenting to later physical health remains severely limited (Hardt and Rutter, 2004). The current study will also add to the small literature testing for a link between parenting and changes in body mass index (Lane et al., 2013; O’Brien et al., 2007).
1.2. Parent-child relationship quality and physical health
In contrast to harsh parenting, warmth and nurturance from close relationships-like the parent-adolescent relationship-promotes physical health (Cohen, 2004). This type of support is believed to reduce the effects of stressful events by promoting less threatening interpretations of those events, as well as more effective coping strategies (Cohen, 2004). This health-protective role of a positive parent-adolescent relationship could manifest in at least two different ways. First, a positive parent-adolescent relationship could improve adolescent health directly (Berkman et al., 2000; Pietromonaco et al., 2013). Alternatively, a positive parentadolescent relationship could reduce the health risk associated with harsh parenting (a moderating or buffering effect). Our search of the literature identified no examples of a positive relationship with one parent buffering the health risk of harshness by a second parent. However, the framework of Biological Embedding provides several reasons to expect such moderation.
First, adolescents who receive warmth from a parent show greater emotional regulation (Choe et al., 2013; Cummings et al., 2005; Denham et al., 1997; Eisenberg et al., 1998) and lower stress response (Miller et al., 2009), which are putative mechanisms through which harsh parenting could affect physical health. Second, a positive relationship with one parent could create or reinforce the perception that support is available for the adolescent, which may dampen the child’s psychological and emotional responses to the stress created by the other parent’s harshness (Cohen and Wills, 1985; Wethington and Kessler, 1986). Third, a positive relationship with one parent might also redirect an adolescent’s maladaptive behavioral responses (e.g., risky behavior, aggression) to the other parent’s harshness (Leidy et al., 2011; Wills and Cleary, 1996). Consistent with this reasoning, research on psychosocial adjustment shows warmth from one parent to buffer the effects of harshness from the other parent (McKee et al., 2007), and for supportive parenting to buffer the effects of family socioeconomic adversity (Pettit et al., 1997). Based on these ideas, we predict that a positive relationship with one parent will buffer the hypothesized health risk of harsh parenting from the other parent.
A final question we address in the current study is that of the nature of any longitudinal link from parenting to adolescent physical health. One possibility is that parenting predicts stable long term changes in physical health. This would be reflected by prediction from parenting to the slope term in a growth model of adolescent health (Singer and Willett, 2003). However, a second possibility is that parenting may show only short-term effects on adolescent health, which would be reflected in prediction by harsh parenting to occasion-specific change, but not to overarching change over time. A third possibility is that the hypothesized influence of parental harshness on short-term changes in health will wane over time, as adolescents move out or in other ways decrease the amount of interaction with their parents. Because failure to specify the effects of short-term change could result in spurious effects for a conventional growth model (Hoffman and Stawski, 2009), we consider all these possibilities.
1.3. The current study
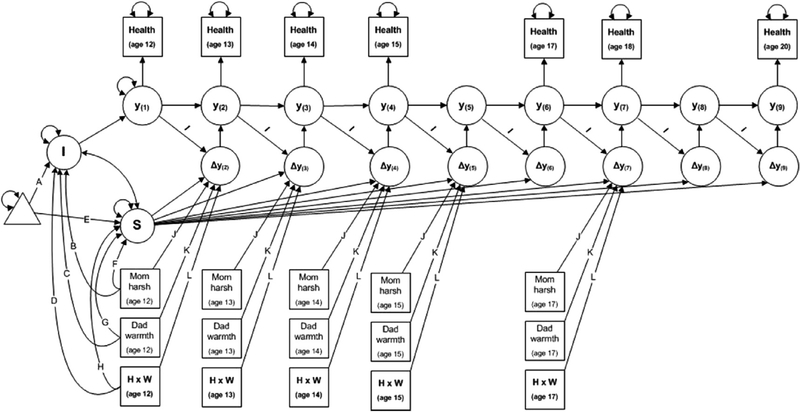
The current study advances the literature on parenting and physical health in several ways. First, unlike most of the studies on parenting behavior and physical health that rely on one-time simultaneous assessments of previous parenting behavior and current health (Miller et al., 2011), we include longitudinal assessments of health outcomes and observed parenting behaviors. Latent change score models (Ferrer and McArdle, 2010) are used to model both growth (i.e., change in level) and occasion-to-occasion associations (quasi-simplex autoregression) in a single overarching model (Fig. 1). That is, this model allows for the estimation of latent trajectories of health outcomes and for time-varying effects of parenting behavior on change in health outcomes at the true score level (free of measurement error). Second, parenting behavior is frequently assessed via self-reports, the limitations of which could affect reliability, validity, and statistical power (Bailey et al., 2012; Forman et al., 2003; Miller et al., 2011). For example, some of the association between self-reported parent behavior and child health may be attributable to genetic predispositions shared between parents and children (i.e., gene-environment correlation; see Plomin, 1994). Observation based assessments of parent behavior have lower heritability than self-reported assessments of parenting (Kendler and Baker, 2007) making them less subject to such misinterpretation. Third, our focus on the simultaneous, potentially interactive influences of both parents on the adolescent’s health more closely reflects the complexity of family system. Fourth, we test for alternative patterns of change over time in adolescent physical health, as well as alternative patterns of prediction from parenting to health over time.
Fig. 1.
Latent change in adolescent physical health, as predicted by mother harshness and father warmth.
2. Method
2.1. Participants
Data for the present study were collected as part of the Iowa Youth and Families Project (IYFP) an investigation originally focused on the effects of economic hardship on parents and their early adolescents. The current analyses focus on the 451 two-parent families in the IYFP. These families were recruited via telephone through the cohort of all seventh-grade students (ages 12e13) in eight counties in north central Iowa who were enrolled in public or private schools during winter and spring of 1989. Specific recruitment procedures are detailed more thoroughly in Conger et al. (1994). Seventy-seven percent of the eligible families agreed to participate in the study. The present study focuses on assessments at age 12, 13, 14, 15, 17, 18, and 20; 94% of the families were retained through the age 20 assessment.
The families in the study lived on farms (about one-third) or in small towns. In 1989 minority families were very rare in rural Iowa, so all of the families were white and spoke English. Annual income ranged from $0 to $135,000 with a mean of $29,642. Fathers’ education ranged from 8 to 20 years with a mean of 13.5 years of education, and the mothers’ education ranged from 8 to 18 years with a mean of 13.4 years. Families ranged from 4 to 13 members with an average of 4.9 members. Adolescents were approximately evenly split across gender (52% female), and 83% did not live with their parents by the final assessment at age 20.
2.2. Procedures
During the first year of the project (when the adolescent was in seventh grade), interviewers visited each family at home for approximately 2 h on each of two occasions. During the first visit, each of the participating family members (i.e., mother, father, target adolescent, close-aged sibling) completed a set of questionnaires focusing on individual family member characteristics and family economic circumstances. During the second visit to the home, which occurred within two weeks of the first, the family members were videotaped as they engaged in several different structured interaction tasks (Conger et al., 1994). Similar visits as just described were conducted with families when the adolescent was in eighth, ninth, and tenth grade. During twelfth grade, the adolescents were interviewed together with their families for the last time. From age 19 forward, the target adolescent was interviewed biannually at their residence. The current study includes data from the assessments at grade 7, 8, 9, 10, 12, age 18, and age 20. Seventy percent of adolescents were not living with their parents by age 18. Approval from the Iowa State Institutional Review Board was maintained throughout the study.
2.3. Measures
2.3.1. Harsh parenting
Observations of mother and father harshness toward the adolescent were obtained five times between seventh grade and 12th grade. Videotapes of family interactions during a structured discussion task were coded at a central site using the Iowa Family Interaction Rating Scales (Melby and Conger, 2001), with coders blind to other information about the families. Inter-coder reliability was established by having two coders assess approximately 25% of the tapes, randomly drawn from each assessment period. For assessments at grades 7, 8, and 9, harshness scores reflected the mean of four 5-point ratings of parent behavior directed at the adolescent: hostility (angry or rejecting behavior), angry coercion (demanding, stubborn, coercive), physical attacks (hitting, pushing, pinching, etc.), and antisocial behavior (self-centered, immature, insensitive). These scores were recoded to 9-point scales to make them comparable to observations obtained at later time points. Higher scores indicate harsher parenting. For assessments at grades 10, 12, age 18, and age 20, harshness scores reflected the mean of the same four ratings, coded on 9-point scales. Harshness scores for both parents had acceptable reliability across timepoints (mean α = 0.82; range = 0.77 to 0.88). The average intraclass correlation between observers across the four scales was 0.72.
2.3.2. Physical health
Adolescent physical health was assessed in grades 7, 8, 9, 10, 12, age 18, and age 20. Self-assessed health is a frequently-used outcome in research on the social determinants of health (Abdulrahim & El Asmar, 2012; Mulvaney-Day et al., 2007; Rohrer et al., 2007) and was used in the current study. Adolescents reported on their physical health by answering the following: “How would you rate your overall physical health?” Response categories ranged from 0 = poor to 5 = excellent.
2.3.3. Body mass index (kg/m2)
Height and weight data were collected in grades 7, 8, 9, 10, 12, age 18, and age 20. Self-reported height and weight correlate highly (r > 0.95) with measured anthropometric height and weight (Lassale et al., 2013; Pursey et al., 2014) and were used in the present study.
2.3.4. Parental warmth
Parental warmth was assessed in grades 7, 8, 9, 10, and 12. Adolescents reported on warmth they received from each parent separately using the seven-item warmth scale of the Behavioral Affective Rating Scale (BARS: Conger, 1989). The introduction for the mother scale read “During the past month when you and your [mother] have spent time talking or doing things together, how often did she…” Items included “Let you know she really cares about you” and “let you know that she appreciates you, your ideas, or the things you do.” Items for the father warmth scale paralleled the mother warmth scale. Both mother and father warmth scales showed acceptable reliability across timepoints (mean α = 0.90; range = 0.87 to 0.93).
2.3.5. Control variables
Control variables included family per-capita income-to-needs ratio, adolescent sex, parent education, block-group level population density from the U.S. decennial census, and family size (all taken from the 7th grade assessment).
2.4. Data analysis
We ran models using Mplus version 7 (Muthén and Muthén, 2006), handling missingness with full-information maximumlikelihood estimation. Missingness was less than 20% for all variables, and was unrelated to both health outcomes. Trajectories in health outcomes were specified as a combination of linear change as well as occasion-specific change (Ferrer and McArdle, 2010). Primary analyses consisted of a comparison of four nested models: 1) a linear growth-only model with no occasion-specific change or covariates, 2) Model 1 plus occasion-specific change (constrained to equality across assessments), 3) Model 2 plus intercept and linear slope regressed onto control variables, harsh parenting, warmth, and the interaction term at the first assessment, and 4) Model 3 plus each occasion-specific change score regressed onto control variables, harsh parenting, warmth, and the interaction term from the previous assessment. Model fit was assessed using the Root Mean Square Error of Approximation (Browne and Cudeck, 1993), and the Tucker-Lewis Index (Tucker and Lewis,1973). Acceptable fit is denoted by RMSEA values below 0.06 and TLI values above 0.90 (Hu and Bentler, 1999).
3. Results
Descriptive statistics are presented in Table 1. Adolescent reported physical health at the first assessment had an average of 3.92 and a standard deviation of 0.85. Both self-reported physical health and body mass index showed consistent variability in early to middle adolescence, but adolescents began to diverge in their BMI scores in late adolescence, which is reflected in increasing standard deviations over time.
Table 1.
Descriptive statistics.
| Variable | n | M | SD | Min | Max |
|---|---|---|---|---|---|
| Physical health (age 12) | 451 | 3.92 | 0.85 | 1.00 | 5.00 |
| Physical health (age 13) | 424 | 4.12 | 0.79 | 1.00 | 5.00 |
| Physical health (age 14) | 406 | 3.99 | 0.88 | 1.00 | 5.00 |
| Physical health (age 15) | 403 | 4.04 | 0.85 | 1.00 | 5.00 |
| Physical health (age 17) | 424 | 3.99 | 0.86 | 1.00 | 5.00 |
| Physical health (age 18) | 420 | 3.83 | 0.86 | 1.00 | 5.00 |
| Physical health (age 20) | 416 | 3.78 | 0.82 | 1.00 | 5.00 |
| Body mass index (age 12) | 451 | 20.01 | 3.49 | 10.09 | 34.43 |
| Body mass index (age 13) | 423 | 20.80 | 3.35 | 14.56 | 35.66 |
| Body mass index (age 14) | 407 | 21.22 | 3.25 | 15.00 | 33.72 |
| Body mass index (age 15) | 402 | 21.83 | 3.60 | 15.33 | 38.27 |
| Body mass index (age 17) | 423 | 22.96 | 4.01 | 16.14 | 45.72 |
| Body mass index (age 18) | 419 | 23.73 | 4.27 | 16.07 | 45.89 |
| Body mass index (age 20) | 416 | 24.46 | 4.75 | 13.91 | 50.84 |
| Mother harshness (age 12) | 446 | 2.44 | 1.05 | 1.00 | 6.50 |
| Mother harshness (age 13) | 418 | 2.81 | 1.14 | 1.00 | 7.50 |
| Mother harshness (age 14) | 404 | 3.06 | 1.27 | 1.00 | 8.75 |
| Mother harshness (age 15) | 394 | 3.16 | 1.34 | 1.00 | 8.50 |
| Mother harshness (age 17) | 370 | 3.13 | 1.38 | 1.00 | 8.13 |
| Father harshness (age 12) | 446 | 2.34 | 1.03 | 1.00 | 6.25 |
| Father harshness (age 13) | 416 | 2.72 | 1.11 | 1.00 | 6.50 |
| Father harshness (age 14) | 400 | 2.88 | 1.25 | 1.00 | 8.00 |
| Father harshness (age 15) | 377 | 2.91 | 1.29 | 1.00 | 8.13 |
| Father harshness (age 17) | 346 | 2.63 | 1.20 | 1.00 | 7.63 |
| Mother warmth (age 12) | 451 | 5.34 | 1.03 | 1.25 | 7.00 |
| Mother warmth (age 13) | 424 | 5.28 | 1.05 | 1.13 | 7.00 |
| Mother warmth (age 14) | 407 | 5.30 | 1.08 | 1.88 | 7.00 |
| Mother warmth (age 15) | 403 | 5.14 | 1.14 | 1.13 | 7.00 |
| Mother warmth (age 17) | 424 | 5.27 | 1.10 | 1.13 | 7.00 |
| Father warmth (age 12) | 451 | 5.29 | 1.19 | 1.00 | 7.00 |
| Father warmth (age 13) | 424 | 5.24 | 1.22 | 1.00 | 7.00 |
| Father warmth (age 14) | 407 | 5.08 | 1.32 | 1.00 | 7.00 |
| Father warmth (age 15) | 403 | 4.90 | 1.30 | 1.00 | 7.00 |
| Father warmth (age 17) | 424 | 4.95 | 1.16 | 1.00 | 7.00 |
| Parent education (age 12) | 451 | 13.48 | 2.13 | 8.00 | 20.00 |
| Family income (age 12) | 451 | 2.86 | 2.00 | −3.95 | 19.03 |
| Population density (age 12) | 416 | 0.08 | 0.18 | 0.00 | 1.23 |
3.1. Physical health
Table 2 contains fit indices from the nested models, with the results for physical health on the left. The baseline model (Model 1) was a linear change model. Adding occasion-specific change (Model 2) improved model fit for physical health (Δχ2 = 23.3, df = 1, p < 0.001 for mother harshness, Δχ2 = 22.7, df = 1, p < 0.001 for father harshness). Adding occasion-specific change (Model 2) did not improve model fit for body mass index (BMI; Δχ2 = 0.02, df = 1, p = 0.89 for mother harshness, Δχ2 = 0.5, df = 1, p = 0.48 for father harshness). Therefore, occasion-specific change was not included in later BMI models. Model 3 added parent behavior at the first assessment (i.e., harshness from one parent, warmth from the second parent, and the statistical interaction between the two) as predictors of initial status and linear change, which resulted in significantly improved fit across all four substantive models. Model 3 was the final model for BMI given the absence of occasion-specific change. Model 4 added parent behavior as predictors of occasion-specific change (constrained to equality over time), which significantly improved model fit for the mother harshness model, Δχ2 = 8.0, df = 3, p = 0.046, but not for the father harshness model, Δχ2 = 0.8, df = 3, p = 0.85. Model 4 was selected as the final model for physical health predicted from mother harshness.
Table 2.
Fit indices for nested models predicting physical health from parental harshness and warmth.
| Model | Physical health |
Body mass index |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mother harshness |
Father harshnes |
Mother harshnes |
Father harshnes |
|||||||||||||
| χ2 | df | TLI | RMSEA | χ2 | df | TLI | RMSEA | χ2 | df | TLI | RMSEA | χ2 | df | TLI | RMSEA | |
| 1 | 300.2 | 163 | 0.886 | 0.045 | 313.1 | 163 | 0.883 | 0.045 | 254.3 | 128 | 0.954 | 0.055 | 275.8 | 128 | 0.937 | 0.059 |
| 2 | 276.9 | 162 | 0.906 | 0.040 | 290.4 | 162 | 0.898 | 0.042 | 254.1 | 127 | 0.954 | 0.055 | 275.3 | 127 | 0.937 | 0.059 |
| 3 | 245.8 | 156 | 0.920 | 0.035 | 253.0 | 156 | 0.912 | 0.037 | 285.1 | 142 | 0.957 | 0.047 | 304.9 | 142 | 0.951 | 0.050 |
| 4 | 237.8 | 153 | 0.921 | 0.035 | 252.2 | 153 | 0.912 | 0.037 | – | – | – | – | – | – | – | – |
Note. Model 1: linear change model; Model 2: linear change and occasion-specific change; Model 3: parenting predicting linear change; Model 4: parenting predicting occasion-specific change; TLI Tucker-Lewis Index; RMSEA root mean square error of approximation.
As a formal test for differences between mother and father harshness, both were included in a simultaneous model for each outcome. Equating the corresponding coefficients across parents led to significantly worse model fit for physical health (Δχ2 = 25.1, df = 9, p = 0.003), but a nonsignificant change in fit for BMI (Δχ2 = 10.5, df = 6, p = 0.11). Consequently, the results presented below for BMI are from this combined model, in which the main and moderating effects are equated across parents.
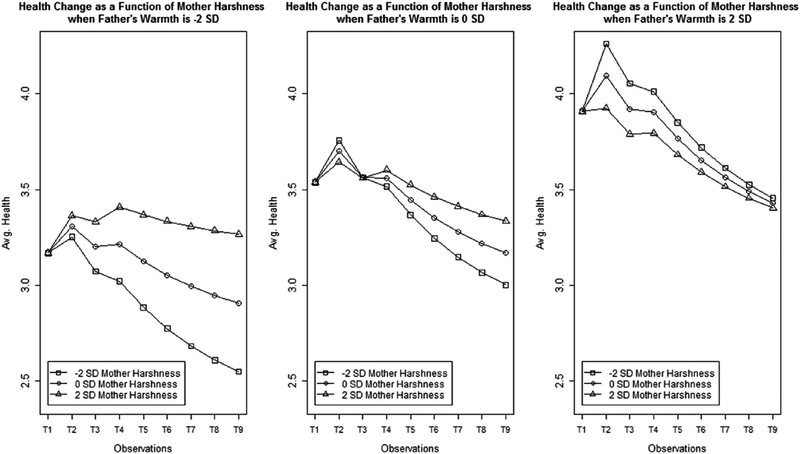
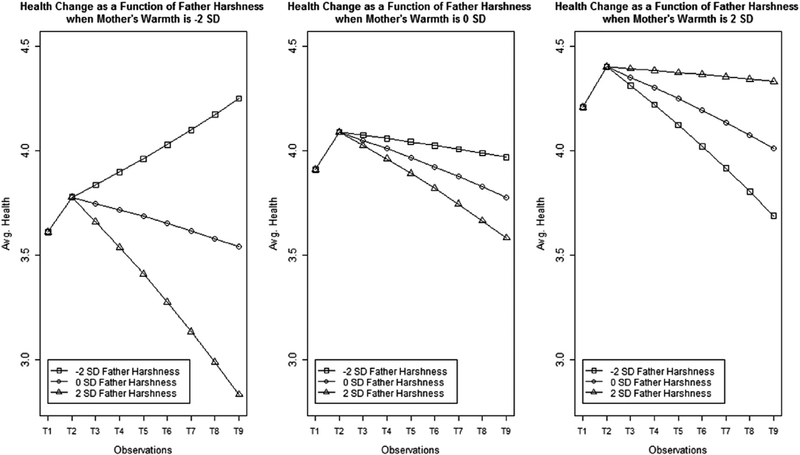
Table 3 contains coefficients from the final models. First and foremost, parent harshness was not associated with differences in the intercept, or level of self-reported physical health at age 12, which reduces the possibility that later associations between harshness and health are actually due to preexisting differences caused by unobserved third variables. Second, parent harshness was associated with difference in the slope, or decrease over time in physical health. Mother harshness predicted a linear decrease over time in adolescent-reported physical health, and that association was buffered by father warmth (b = 0.02, SE = 0.01). However, mother harshness also showed occasion-specific associations with change over time in health, which was also moderated by father warmth (b = −0.02, SE = 0.01). The reversed direction of the occasion-specific moderating effect show that the association between harsh mothering and physical health attenuates in late adolescence. As shown in Fig. 2, this attenuation emerges as fathers increase on warmth. Furthermore, adolescents show the most benefit from father warmth when mother harshness is low, and the least benefit from father warmth when mother harshness is high. Father harshness also predicted a linear decrease over time in adolescent-reported physical health, and that association was moderated by mother warmth. As shown in Fig. 3, the decline in health associated with father harshness attenuates as mother warmth increases. Higher physical health at age 12 was associated with parent education (b = 0.04, SE = 0.01), family income (b = 0.04, SE = 0.01), and being male (b = 0.27, SE = 0.05), but these covariates did not predict change over time in physical health.
Table 3.
Coefficients and standard errors from final models predicting physical health and body mass index from parental harshness and warmth (N = 451).
| Path from Fig. 1 | Physical health |
Body mass index |
||
|---|---|---|---|---|
| Mother |
Father |
Mother |
Father |
|
| Harshness | Harshness | Harshness | Harshness | |
| A. Intercept (I) | 3.92 (0.05)* | 3.91 (0.05)* | 20.12 (0.17) * | 20.06(0.17)* |
| B.Harshness predicting I | −0.02 (0.04) | −0.02 (0.04)* | 0.11 (0.10) | 0.11 (0.10) |
| C.Warmth predicting I | 0.20 (0.04) | 0.11 (0.04) | −0.14 (0.09) | −0.14 (0.09) |
| D.Harshness x warmth predicting I | −0.04 (0.04)* | −0.08 (0.04)* | 0.01 (0.10) | 0.01 (0.10) |
| E.Linear change (S) | −0.21 (0.04) * | −0.22 (0.04) | 0.53 (0.02)* | 0.58 (0.02)* |
| F. Harshness predicting S | 0.00 (0.01) | 0.00 (0.01) | 0.01 (0.01) | 0.01 (0.01) |
| G. Warmth predicting S | −0.02 (0.01)* | −0.01 (0.01)* | 0.00 (0.01) | 0.00(0.01) |
| H. Harshness x warmth predicting S | 0.02 (0.01)* | 0.02 (0.01) | 0.03 (0.01)* | 0.03(0.01)* |
| I. Occasion-specific change (Sʹ) | 0.04 (0.01)* | 0.04 (0.01) * | – | – |
| J. Harshness predicting Sʹ | −0.02 (0.01) | – | – | – |
| K. Warmth predicting Sʹ | 0.01 (0.01) | – | – | – |
| L. Harshness x warmth predicting Sʹ | −0.02 (0.01)* | – | – | – |
Note.
p < 0.05.
Fig. 2.
Change in adolescent physical health, as predicted by mother harshness and father warmth.
Fig. 3.
Change in adolescent physical health, as predicted by father harshness and mother warmth.
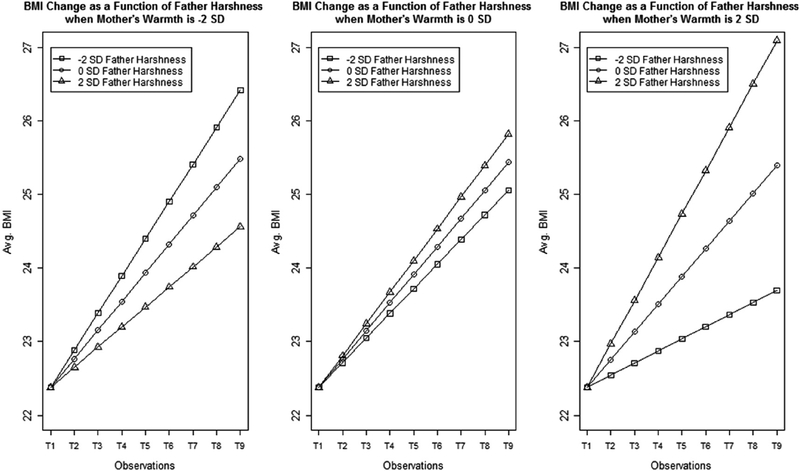
3.2. Body mass index
Parent harshness was not associated with differences in the intercept, or level of body mass index at age 12. This reduces the possibility that later associations between harshness and body mass index are actually due to preexisting differences caused by unobserved third variables. Father harshness predicted a linear increase over time in adolescent body mass index, and that association was moderated by mother warmth (Fig. 4), such that the increase over time in body mass index associated with father harshness augments as mother warmth increases. Mother harshness also predicted a linear increase over time in adolescent body mass index, and that association was similarly moderated by father warmth. Lower BMI at age 12 was associated with lower family income (b = −0.18, SE = 0.07), and BMI increased over time more rapidly for males (b = 0.15, SE = 0.04).
Fig. 4.
Change in adolescent body mass index (BMI), as predicted by mother harshness and father warmth.
Supplemental analyses considered the possible mediating roles of smoking, overeating, suicide ideation, parent income, parent education, population density, and family structure on the associations between parent harshness and physical health outcomes. None of these covariates functioned as mediators or changed the pattern of results.
4. Discussion
In this study we analyzed change in self-reported physical health and body mass index (BMI) during adolescence. As predicted, ado-lescents who experience harshness from either parent showed significant decreases in physical health and significant increases in BMI. These differences were not evident at the beginning of adolescence but became evident over time and persisted into young adulthood; they suggest that the associations between parent harshness and adolescent health are not due to preexisting differences. In all but one instance, the differences that did emerge persisted even after most adolescents were no longer living with their parents. These results show that differences in health associated with harsh parenting can persist, consistent with findings from other studies of parental harshness and physical health (e.g., Brody et al., 2013). Results were modest in size, but were consistent with the findings from a recent meta-analytic summary of the effect of child maltreatment on physical health in adulthood (Wegman and Stetler, 2009). Harsh parenting predicted change in both health indices, which increases our confidence in these associations.
The current study extends prior research by showing that observed harsh parenting predicts change over time in selfreported adolescent health and body mass index. These findings support including harsh parenting in the category of stressful environments that affect health (Shonkoff et al., 2009). To our knowledge, this study is also the first to identify moderation of the association between harsh parenting and changes over time in physical health (for similar results with cross-sectional data see Schafer et al., 2014). A positive relationship with one parent buffered the associations between observed harsh parenting from the second parent and changes over time in physical health. The pattern of moderation for self-reported physical health is consistent with theoretical work on the salience of close relationships for physical health (Pietromonaco et al., 2013). In contrast to the results for overall physical health, the results for BMI suggest that the health risk of harsh parenting increases as warmth from the other parent increases. Additional research is needed to further understand the nature of the correlation between self-reported physical health and body mass index. They appear to respond differently to the combination of warmth from one parent and harshness from a second parent.
The association between harsh parenting and health outcomes was usually time-invariant, but there was one exception. Mother harshness predicted both long-term change and short-term changes in physical health in such a way that, when combined, suggested the hypothesized health risk of mother harshness attenuated over time. According to the framework of biological embedding, the prediction to long-term changes in health would be explained by shifts in inflammation due to increased white blood cell activity, hormone release (Black, 2006), and long-term potentiation of specific neural pathways. This prediction to shortterm change suggests that mother harshness is linked to physical health in a different manner than father harshness, potentially due to the greater amount of time adolescents typically spend with mothers than fathers (Coltrane and Shih, 2010). Additional research is needed to further clarify the degree to which this or other potential mediating processes account for the links between parent harshness and physical health documented in the current study.
4.1. Limitations
One limitation of the current study is the ethnic homogeneity of the sample. Although socioeconomically diverse, all the participants were white. Replication across other groups will increase our confidence in the generalizability of the findings. Another limitation of the current study is our focus on two health outcomes: adolescent reported health and BMI. Although some work suggests the magnitude of association between harsh parenting and child physical health is equal across subjective and objective measures of health (Wegman and Stetler, 2009), similar longitudinal tests across additional health outcomes will strengthen our confidence in the present findings. The moderating role of parent-child warmth was generally supported, but it is possible that expanding the range of health outcomes to other dimensions may offer more or less support. We may have omitted important variables from the model (biological or environmental, such as school and community factors) that could have altered the pattern of results. Finally, this nonexperimental design cannot directly address questions of causality.
5. Implications and contributions
One practical implication of these findings is that although interventions often focus on extreme maltreatment and deprivation, harsh parenting may also affect adolescent health. A second point concerns the observed protective effect of warmth from a second parent. This finding echoes results from the developmental psychology literature suggesting that perceiving support from one friend can buffer hostility or bullying from other peers (Adams et al., 2011; Parker and Asher, 1993; Peters et al., 2011). The protective, buffering role of safe, stable, nurturing relationships on adolescent health and on the intergenerational transmission of child maltreatment has also been documented (Merrick et al., 2013; Schofield et al., 2013). As such, preventive interventions that enhance and promote safety, stability, and nurturance as key dimensions of supportive intra- and inter-familial relationships might help to promote positive health in adolescence and beyond. Continued study of differences across individuals and contexts, as well as the role of safe, stable, nurturing environments, is necessary to more fully understand the association between harsh parenting and adolescent health, and provide support for children and families who experience it.
Acknowledgements
This research is currently supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (HD064687). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. Support for earlier years of the study also came from multiple sources, including the National Institute of Mental Health (MH00567, MH19734, MH43270, MH59355, MH62989, MH48165, MH051361), the National Institute on Drug Abuse (DA05347), the National Institute of Child Health and Human Development (HD027724, HD051746, HD047573), the Bureau of Maternal and Child Health (MCJ-109572), and the MacArthur Foundation Research Network on Successful Adolescent Development Among Youth in High-Risk Settings. Authors report no conflicts of interest. The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.socscimed.2016.03.027.
References
- Abdulrahim S, El Asmar K, 2012. Is self-rated health a valid measure to use in social inequities research? Evidence from the PAPFAM women’s data in six Arab countries. Int. J. Equity Health 11, 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Santo JB, Bukowski WM, 2011. The presence of a best friend buffers the effects of negative experiences. Dev. Psychol 47, 1786–1791. [DOI] [PubMed] [Google Scholar]
- Anda RF, Croft JB, Felitti VJ, Nordenberg D, Giles WH, Williamson DF, Giovino GA, 1999. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA 282, 1652–1658. [DOI] [PubMed] [Google Scholar]
- Bailey HN, DeOliveira CA, Wolfe VV, Evans EM, Hartwick C, 2012. The impact of childhood maltreatment history on parenting: a comparison of maltreatment types and assessment methods. Child Abuse Negl. 36, 236–246. [DOI] [PubMed] [Google Scholar]
- Barker DJP, Osmond C, Forsén TJ, Kajantie E, Eriksson JG, 2005. Trajectories of growth among children who have coronary events as adults. N. Engl. J. Med 353, 1802–1809. [DOI] [PubMed] [Google Scholar]
- Berger RP, Zolotor AJ, 2013. Is there an association between physical punishment in childhood and physical health in adulthood? Pediatrics 132, e500–e501. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE, 2000. From social integration to health: Durkheim in the new millennium. Soc. Sci. Med 51, 843–857. [DOI] [PubMed] [Google Scholar]
- Black PH, 2006. The inflammatory consequences of psychologic stress: relation to insulin resistance, obesity, atherosclerosis and diabetes mellitus, type II. Med. Hypotheses 67, 879–891. [DOI] [PubMed] [Google Scholar]
- Boyce WT, Ellis BJ, 2005. Biological sensitivity to context: I. An evolutionarydevelopmental theory of the origins and functions of stress reactivity. Dev. Psychopathol 17, 271–301. [DOI] [PubMed] [Google Scholar]
- Brody Gene H., Tianyi Yu, Beach Steven R.H., Kogan Steven M., Michael Windle, Philibert RA, 2013. Harsh parenting and adolescent health: a longitudinal analysis with genetic moderation. Health Psychol. 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck R, 1993. Alternative ways of assessing model fit In: Bollen KA, Long JS (Eds.), Testing Structural Equation Models. Sage, Beverly Hills, CA, pp. 136–162. [Google Scholar]
- Bush NR, Boyce WT, 2014. The contributions of early experience to biological development and sensitivity to context In: Lewis M, Rudolph KD (Eds.), Handbook of Developmental Psychopathology (3rd ed.). Springer Science + Business Media, New York, NY, US, pp. 287–309. [Google Scholar]
- Choe DE, Olson SL, Sameroff AJ, 2013. Effects of early maternal distress and parenting on the development of children’s self-regulation and externalizing behavior. Dev. Psychopathol 25, 437–453. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL, 2005. Child maltreatment. Annu. Rev. Clin. Psychol 1, 409–438. [DOI] [PubMed] [Google Scholar]
- Cohen S, 2004. Social relationships and health. Am. Psychol 59, 676–684. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA, 1985. Stress, social support, and the buffering hypothesis. Psychol. Bull 98, 310–357. [PubMed] [Google Scholar]
- Coltrane S, Shih KY, 2010. Gender and the division of labor In: Chrisler JC, McCreary DR (Eds.), Handbook of Gender Research in Psychology, Gender Research in Social and Applied Psychology, vol. 2 Springer, New York, NY, pp. 401–422. [Google Scholar]
- Conger RD, 1989. Behavioral Affect Rating Scale (BARS): Young Adult Perception of Parents’ Hostility and Warmth: Iowa Youth and Families Project. Iowa State University, Ames, IA. [Google Scholar]
- Conger RD, Elder GH Jr., Lorenz FO, Simons RL, Whitbeck LB, 1994. Families in Troubled Times: Adapting to Change in Rural America. Aldine de Gruyter, Hawthorne, NY, US. [Google Scholar]
- Cummings EM, Keller PS, Davies PT, 2005. Towards a family process model of maternal and paternal depressive symptoms: exploring multiple relations with child and family functioning. J. Child Psychol. Psychiatry 46, 479–489. [DOI] [PubMed] [Google Scholar]
- Denham SA, Mitchell-Copeland J, Strandberg K, Auerbach S, Blair K, 1997. Parental contributions to preschoolers’ emotional competence: direct and indirect effects. Motiv. Emot 21, 65–86. [Google Scholar]
- Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB, 2009. Cumulative childhood stress and autoimmune diseases in adults. Psychosom. Med 71, 243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL, 1998. Parental socialization of emotion. Psychol. Inquiry 9, 241–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ, 2008. Exposure to childhood sexual and physical abuse and adjustment in early adulthood. Child Abuse Negl 32, 607–619. [DOI] [PubMed] [Google Scholar]
- Ferrer E, McArdle JJ, 2010. Longitudinal modeling of developmental changes in psychological research. Curr. Dir. Psychol. Sci 19, 149–154. [Google Scholar]
- Forman DR, O’Hara MW, Larsen K, Coy KC, Gorman LL, et al. , 2003. Infant emotionality: observational methods and the validity of maternal reports. Infancy 4, 541–565. [Google Scholar]
- Francis DD, Meaney MJ, 1999. Maternal care and the development of stress responses. Curr. Opin. Neurobiol 9, 128–134. [DOI] [PubMed] [Google Scholar]
- Hardt J, Rutter M, 2004. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J. Child Psychol. Psychiatry 45, 260–273. [DOI] [PubMed] [Google Scholar]
- Hertzman C, 2012. Putting the concept of biological embedding in historical perspective. PNAS Proc. Natl. Acad. Sci. U. S. A 109, 17160–17167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillis SD, Anda RF, Felitti VJ, Marchbanks PA, 2001. Adverse childhood experiences and sexual risk behaviors in women: a retrospective cohort study. Fam. Plan. Perspect 33, 206–211. [PubMed] [Google Scholar]
- Hoffman L, Stawski RS, 2009. Persons as contexts: evaluating between-person and within-person effects in longitudinal analysis. Res. Hum. Dev 6, 97–120. [Google Scholar]
- Hu L, Bentler PM, 1999. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model 6, 1–55. [Google Scholar]
- Johnson MH, 2005. Sensitive periods in functional brain development: problems and prospects. Dev. Psychobiol 46, 287–292. [DOI] [PubMed] [Google Scholar]
- Johnston-Brooks CH, Lewis MA, Evans GW, Whalen CK, 1998. Chronic stress and illness in children: the role of allostatic load. Psychosom. Med 60, 597–603. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Baker JH, 2007. Genetic influences on measures of the environment: a systematic review. Psychol. Med 37, 615–626. [DOI] [PubMed] [Google Scholar]
- Lane SP, Bluestone C, Burke CT, 2013. Trajectories of BMI from early childhood through early adolescence: SES and psychosocial predictors. Br. J. Health Psychol 18, 66–82. [DOI] [PubMed] [Google Scholar]
- Lassale C, Peneau S, Touvier M, Julia C, Galan P, Hercberg S, 2013. Validity of web-based self-reported weight and height: results of the Nutrinet-Sante study. J. Med. Internet Res 15 (8), e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leidy MS, Schofield TJ, Miller MA, Parke RD, Coltrane S, et al. , 2011. Fathering and adolescent adjustment: variations by family structure and ethnic background. Fathering 9, 44–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee L, Roland E, Coffelt N, Olson AL, Forehand R, et al. , 2007. Harsh discipline and child problem behaviors: the roles of positive parenting and gender. J. Fam. Violence 22, 187–196. [Google Scholar]
- McEwen BS, 1998. Protective and damaging effects of stress mediators. N. Engl. J. Med 338, 171–179. [DOI] [PubMed] [Google Scholar]
- McGowan PO, Sasaki A, D’Alessio AC, Dymov S, Labonté B, Szyf M, Turecki G, Meaney MJ, 2009. Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nat. Neurosci 12, 342–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meaney MJ, Szyf M, 2005. Maternal care as a model for experience-dependent chromatin plasticity? Trends Neurosci. 28, 456–463. [DOI] [PubMed] [Google Scholar]
- Mechanic D, Hansell S, 1989. Divorce, family conflict, and adolescents’ well- being. J. Health Soc. Behav 30, 105–116. [PubMed] [Google Scholar]
- Melby JN, Conger RD, 2001. The Iowa family interaction rating scales: instrument summary In: Kerig P, Lindahl K (Eds.), Family Observational Coding Systems: Resources for Systematic Research. Erlbaum, Mahwah, NJ. [Google Scholar]
- Merrick MT, Leeb RT, Lee RD, 2013. Examining the role of safe, stable, and nurturing relationships in the intergenerational continuity of maltreatment e introduction to the special issue. J. Adolesc. Health 53 (5), S1–S3. [DOI] [PubMed] [Google Scholar]
- Miller G, Chen E, Cole SW, 2009. Health psychology: developing biologically plausible models linking the social world and physical health. Annu. Rev. Psychol 60, 501–524. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Parker KJ, 2011. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol. Bull 137, 959–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery SM, Bartley MJ, Wilkinson RG, 1997. Family conflict and slow growth. Arch. Dis. Child 77, 326–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulvaney-Day NE, Alegría M, Sribney W, 2007. Social cohesion, social support, and health among Latinos in the United States. Soc. Sci. Med 64, 477–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO, 2006. Mplus User’s Guide, fourth ed. Muthén & Muthén, Los Angeles, CA. [Google Scholar]
- O’Brien M, Nader PR, Houts RM, Bradley R, Friedman SL, et al. , 2007. The ecology of childhood overweight: a 12-year longitudinal analysis. Int. J. Obes 31, 1469–1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker JG, Asher SR, 1993. Peer acceptance and later personal adjustment: are low-accepted children at risk? Psychol. Bull 102, 357–389. [DOI] [PubMed] [Google Scholar]
- Peters E, Riksen-Walraven M, Cillessen ANH, de Weerth C, 2011. Peer rejection and HPA activity in middle childhood: friendship makes a difference. Child. Dev 82, 1906–1920. [DOI] [PubMed] [Google Scholar]
- Pettit GS, Bates JE, Dodge KA, 1997. Supportive parenting, ecologicalcontext, and children’s adjustment: a seven-year longitudinal study. Child. Dev 68, 908–923. [DOI] [PubMed] [Google Scholar]
- Pietromonaco PR, Uchino B, Dunkel-Schetter C, 2013. Close relationship processes and health: implications of attachment theory for health and disease. Health Psychol. 32, 499–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plomin R, 1994. Genetics and Experience. Sage, Newbury Park, CA. [Google Scholar]
- Pursey K, Burrows TL, Stanwell P, Collins CE, 2014. How accurate is web- based self-reported height, weight, and body mass index in young adults? J. Med. Internet Res 16 (1), e4 10.2196/jmir.2909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE, 2002. Risky families: family socialenvironments and the mental and physical health of offspring. Psychol. Bull 128, 330–366. [PubMed] [Google Scholar]
- Rohrer JE, Arif A, Denison A, Young R, Adamson S, 2007. Overall self-rated health as an outcome indicator in primary care. J. Eval. Clin. Pract 13, 882–888. [DOI] [PubMed] [Google Scholar]
- Yu Rueger, S., Katz RL, Risser HJ, Lovejoy MC, 2011. Relations between parental affect and parenting behaviors: a meta-analytic review. Parent. Sci. Pract 11, 1–33. [Google Scholar]
- Russek LG, Schwartz GE, 1997. Perceptions of parental caring predict health status in midlife: a 35-year follow-up of the Harvard Mastery of Stress Study. Psychosom. Med 59, 144–149. [DOI] [PubMed] [Google Scholar]
- Schafer MH, Morton PM, Ferraro KF, 2014. Child maltreatment and adult health in a national sample: heterogeneous relational contexts, divergent effects? Child Abuse Negl. 38, 395–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schofield TJ, Weaver JM, 2015. Democratic parenting beliefs and observed parental sensitivity: reciprocal influences between coparents. J. Fam. Psychol (advance online publication). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schofield TJ, Lee RD, Merrick MT, 2013. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: a metaanalysis. J. Adolesc. Health 53 (5), S32–S38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT, McEwen BS, 2009. Neuroscience, molecular biology, and the childhood roots of health disparities building a new framework for health promotion and disease prevention. JAMA 301, 2252–2259. [DOI] [PubMed] [Google Scholar]
- Siervo M, Wells JC, Cizza G, 2009. The contribution of psychosocial stress to the obesity epidemic: an evolutionary approach. Horm. Metab. Res 41, 261–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD, Willett JB, 2003. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford University Press, New York, NY. [Google Scholar]
- Stein A, Woolley H, Cooper SD, Fairburn CG, 1994. An observational study of mothers with eating disorders and their infants. J. Child Psychol. Psychiatry 35, 733–748. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C, 1973. A reliability coefficient for maximum likelihood factor analysis. Psychometrika 38, 1–10. [Google Scholar]
- Wegman HL, Steltler C, 2009. A meta-analytic review of the effects of childhood abuse on medical outcomes in adulthood. Psychosom. Med 71, 805–812. [DOI] [PubMed] [Google Scholar]
- Weidner G, Hutt J, Connor SL, Mendell NR, 1992. Family stress and coronary risk in children. Psychosom. Med 54, 471–479. [DOI] [PubMed] [Google Scholar]
- White HR, Widom CS, 2003. Does childhood victimization increase the risk of early death? A 25-year prospective study. Child Abuse Negl. 27, 841–853. [DOI] [PubMed] [Google Scholar]
- Williamson DF, Thompson TJ, Anda RF, Dietz WH, Felitti V, 2002. Body weight and obesity in adults and self-reported abuse in childhood. Int. J. Obes 26, 1075–1082. [DOI] [PubMed] [Google Scholar]
- Wills TA, Cleary SD, 1996. How are social support effects mediated? A test with parental support and adolescent substance use. J. Personal. Soc. Psychol 71, 937–952. [DOI] [PubMed] [Google Scholar]
- Wethington E, Kessler RC, 1986. Perceived support, received support, and adjustment to stressful life events. J. Health Soc. Behav 27, 78–89. [PubMed] [Google Scholar]