Abstract
Background:
Diabetes self-management (DSM) applications (apps) have been designed to improve knowledge of diabetes and self-management behaviors. However, few studies have systematically examined if diabetes apps followed the American Association of Diabetes Educators (AADE) Self-Care Behaviors™ guidelines. The purpose of this study was to compare the features of current DSM apps to the AADE7™ guidelines.
Methods:
In two major app stores (iTunes and Google Play), we used three search terms “diabetes,” “blood sugar,” and “glucose” to capture a wide range of diabetes apps. Apps were excluded based on five exclusion criteria. A multidisciplinary team analyzed and classified the features of each app based on the AADE7™. We conducted interviews with six diabetes physicians and educators for their opinions on the distribution of the features of DSM apps.
Results:
Out of 1050 apps retrieved, 173 apps were identified as eligible during November 2015 and 137 apps during December 2017. We found an unbalanced DSM app development trend based on AADE7™ guidelines. Many apps were designed to support the behaviors of Healthy Eating (77%), Monitoring (76%), Taking Medication (58%), and Being Active (45%). On the other hand, few apps explored the behaviors of Problem Solving (31%), Healthy Coping (10%), and Reducing Risks (5%). From interviews, we identified the main reasons why only a few apps support the features related to Problem Solving, Healthy Coping, and Reducing Risks.
Conclusions:
Future diabetes apps should attempt to incorporate features under evidence-based guidelines such as AADE7™ to better support the self-management behavior changes of people with diabetes.
Keywords: diabetes mellitus, features, guidelines, mobile applications, self-management
Diabetes Self-Management Education (DSME)
DSME is important for clinical management of people with diabetes.1 It is an organized process of teaching people with diabetes to learn to manage symptoms, treatments, lifestyle changes, and psychosocial, cultural, and spiritual consequences associated with diabetes.1 A systematic review reported that DSME helped people with diabetes improve diabetes knowledge, record eating habits, and increase the frequency and accuracy of blood glucose monitoring.2 DSME also benefits people with diabetes by helping improve control of blood glucose1,2 and reduce the risk for diabetes complications.3
Diabetes Self-Management (DSM) Applications (Apps)
Mobile health can provide chronic disease management assistance outside hospitals4 because DSM is a daily task and requires support between office visits on an ongoing basis. There has been rapid development of health apps in recent years. A new study that was conducted by Research 2 Guidance in 2016 reported that the number of mobile health apps reached 259 000.5 With the explosion of health apps, the number of apps developed for providing assistance to people with diabetes also has increased significantly.6
Research has indicated that people with diabetes benefit from using diabetes apps. Hou et al conducted a systematic review to assess the clinical effectiveness of diabetes apps in controlling hemoglobin A1c (HbA1c).7 They reported on 10 studies related to type 2 diabetes that showed a decrease in HbA1c.7-17 Similarly, a systematic review of 12 randomized controlled trials by Wu et al reported that using diabetes apps was associated with a significantly reduced HbA1c.8,10-12,16,18-25
Currently, very few studies have evaluated the coherence between features of diabetes apps and evidence-based guidelines such as from the American Association of Diabetes Educators (AADE). Chomutare et al analyzed the functions of 101 DSM apps from Apple iPhone, Google Android, BlackBerry, and Nokia Symbian.26 The authors found that features of diabetes apps on the online market did not cover evidence-based recommendations. The results showed that the four most popular features were insulin and medication recording (62%), data export and communication (60%), diet recording (47%), and weight management (43%).26 They found a lack of other important features such as diabetes education, social media integration, and alerts.26 Similarly, in 2013, Breland et al compared features of 227 DSM apps from Apple App Store to the AADE7™.27 They found that the apps followed only some of the seven self-management behaviors by AADE7™.27 Out of 227 apps, 109 apps provided features for Self-monitoring, 106 apps for Medication, 102 apps for Healthy Eating, 67 apps for Problem Solving, 56 apps for Being Active.27 Only 27 apps addressed Reducing Risks, and 13 apps dealt with Healthy Coping.27 However, Breland et al’s study did not examine the entirety of the mobile apps for adherence to AADE7™. Instead, they only reviewed the App Store description of the 227 apps. Because Chomutare et al mentioned that there were differences between the actual features in the apps and features promoted in the description pages in their limitations,26 Breland et al’s results may have been different if all 277 apps were downloaded for review.
Evidence-Based Guidelines for Feature Analysis
Based on seven systematic reviews,28-34 the AADE Research Committee assessed the state of the evidence regarding the basic self-care behaviors guidelines for people with diabetes in 2007.35 In this study, we chose the AADE7™ as the DSM guidelines for feature analysis of the selected apps because both the American Diabetes Association (ADA)36 and the American Geriatrics Society (AGS)37 have suggested people with diabetes follow the AADE7™ for DSM.38,39 The seven self-care behaviors defined in the AADE7™ are Healthy Eating, Being Active, Monitoring, Taking Medication, Problem Solving, Reducing Risks, and Healthy Coping.35 Under each of the seven behaviors, AADE7™ provide a list of self-care behaviors that are essential to successful DSM.
The objective of our study was to compare features of DSM apps that are currently available on the main app stores to the evidence-based AADE7™.
Methods
Identification of Apps
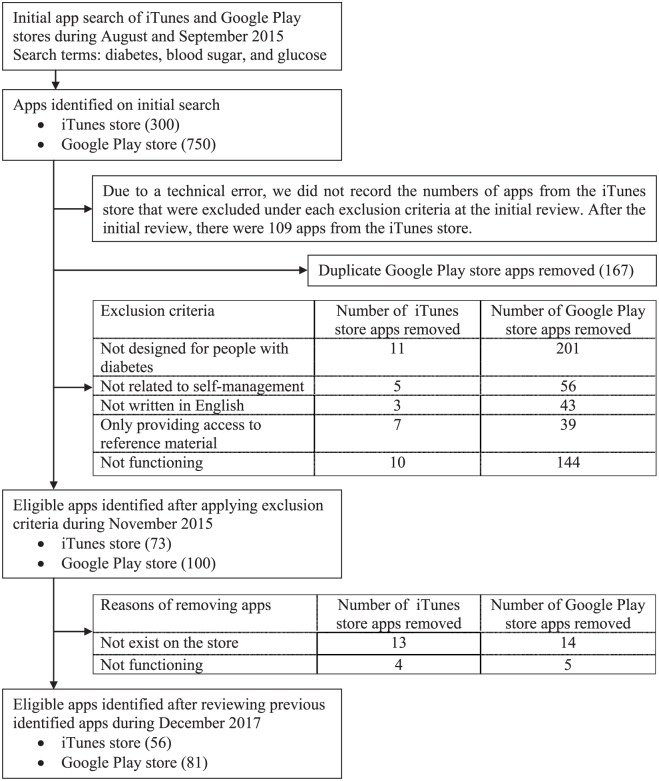
From the Statistics Portal in March 2017, there were 2 800 000 apps on Google Play, 2 200 000 apps on iTunes Store, and 669 000 apps on Windows Store.40 iTunes and Google Play are the two largest app stores and were therefore selected to search DSM apps. We chose iPad apps from the iTunes store because the iPad screen size may be easier to read for older people with diabetes with limited visual acuity and motor control.41 A multidisciplinary team of a usability expert (MSK), a diabetes education researcher (SAB), an endocrinologist (UK), an epidemiologist (EJS), and a mobile health intervention developer (QY) conducted a multistep review process (Figure 1). First, based on the use of search terms in other studies, the three terms “diabetes,”4,26,27,42-45 “blood sugar,”44 and “glucose”26,44 were used respectively in both the app stores. Second, titles and descriptions of the retrieved apps were reviewed for select eligible DSM apps. Based on previous literature,44,46 we developed the exclusion criteria. The apps were excluded if they (1) were not designed for people with diabetes, (2) were not related to self-management, (3) were not written in English, (4) only provided access to reference material, or (5) were not functioning at the time of the study. Third, the eligible apps from the iTunes store were downloaded on an iPad (4th generation). The eligible apps from the Google Play store were downloaded on a Nexus 7 and a Galaxy Tab SM-T230. The author who conducted the initial review (QY) applied the exclusion criteria and identified 173 apps that were eligible for the study. All authors then systematically analyzed and discussed features of each app during eight group meetings conducted over a period of three months. We tested the functionality and features of all the apps by creating a user account if required, and entering typical DSM information such as glucose level, weight, and medications. We collected iTunes apps between August 31 and September 1, 2015, and Google Play apps between October 13 and October 15, 2015. We recorded each app’s name, description, whether it is designed for type 1 or type 2 diabetes, price, vendor, URL, number of ratings of current version and all versions, average rating of current version and all versions, and mobile operating systems (eg, iOS, Android). Because we used three search terms individually for both the iTunes and Google Play stores, some apps appeared multiple times. We identified and removed these duplicate apps to avoid double counting when we computed the total eligible apps for this study. Considering that there were mobile apps removed from iTunes and Google Play stores, we checked the availability and applied the exclusion criteria on the 173 apps. Then we updated the feature analysis data on the eligible apps during December 2017.
Figure 1.
DSM apps study flow chart.
Feature Analysis Using AADE7™
Mobile apps are designed using specific elements or “features” to support user needs. Based on the description of each of the seven self-care behaviors in AADE7™ web page, we created a feature list which was categorized by seven self-care behaviors of AADE7™. After eligible apps were downloaded and tested, we recorded and classified the features of every app on the basis of the feature list. Features related to DSM but not listed in AADE7™, were recorded and classified into an “Others” category. We grouped the features in the “Others” category. We employed two types of descriptive statistics to analyze features against the AADE7™. First, we computed the unique number of apps that provide any number of features related to AADE7™. For example, an app was counted once for Healthy Eating category regardless of whether the app had one or five features that belonged to Healthy Eating. Second, we also counted the total number of features under an AADE7™ category across the apps. For example, we counted 45 features under Problem Solving. There were 38 features for “alert and reminder for abnormal data,” five features for “self-monitoring,” and two features for “discuss possible solutions with others.”
Interview With Diabetes Physicians and Educators
We conducted interviews with diabetes physicians and educators individually for addressing the reasons why few apps supported the features related to Problem Solving, Reducing Risks, and Healthy Coping. The interview questions included how long they had worked in diabetes care or education, if they had ever recommended DSM apps to people with diabetes, and their opinions on the research results. The interviews were recorded for retrospective analysis.
Results
Identification of Apps
We retrieved 300 apps from the iTunes store and 750 apps from the Google Play store. After a multilevel review process, 173 apps were found eligible during November 2015 and 137 apps during December 2017 for this study. There were 56 apps from the iTunes store and 81 apps from the Google Play store (Figure 1). There were two apps designed for type 1 diabetes, nine apps designed for type 2 diabetes, 19 apps designed for both type 1 and type 2 diabetes, and 107 apps did not report in their description information about the type of diabetes for which they were designed. Out of 137 apps, most apps were free (71%, 97/137). The median price of paid apps was $2.99. The price ranged from $0.99 to $14.99 for paid apps.
Feature Analysis Using AADE7™
We analyzed features of the eligible apps based on the AADE7™ during November 2015 and December 2017. As shown in Table 1, we found that many apps were designed to support behaviors of Healthy Eating (72% in 2015, 77% in 2017), Monitoring (73% in 2015, 76% in 2017), Taking Medication (53% in 2015, 58% in 2017), and Being Active (39% in 2015, 45% in 2017). On the other hand, few apps were designed to provide features that support the behaviors of Problem Solving (20% in 2015, 31% in 2017), Healthy Coping (9% in 2015, 10% in 2017), and Reducing Risk (6% in 2015, 5% in 2017).
Table 1.
Number of Apps Providing Features Related to Each Behavior of AADE7™.
| AADE7™ behaviors |
Number from November 2015 (%) | Number from December 2017 (%) |
|---|---|---|
| Healthy Eating | 125 (72) | 105 (77) |
| Being Active | 67 (39) | 62 (45) |
| Monitoring | 126 (73) | 104 (76) |
| Taking Medication | 92 (53) | 79 (58) |
| Problem Solving | 35 (20) | 42 (31) |
| Reducing Risks | 10 (6) | 7 (5) |
| Healthy Coping | 15 (9) | 14 (10) |
Table 2 presents the feature list in each self-care behavior and the number of features related to the AADE7™ across the 137 apps. There were several features that were covered well by current DSM apps, including “count carbohydrates” and “monitor eating” under Healthy Eating, “keep track of activities” under Being Active, “record blood sugar levels” and “record height or weight or BMI” under Monitoring, and “keep track of medications” under Taking Medication. There were several features that are suggested by AADE7™ with zero count, indicating that no apps provided any of those features. For example, “report smoking behavior” under Reducing Risks were not provided in any apps.
Table 2.
Number of Features Related to AADE7™ Across the 137 Apps.
| AADE7™ behaviors | Number of features across the apps |
|---|---|
| Healthy Eating (316) | Count carbohydrates*
(79) Monitor eating (58) Measure each serving* (46) Read food labels* (45) Provide Recipes (20) Prevent high or low blood sugar* (19) Provide knowledge of healthy eating (13) Set goals for healthy eating* (12) Remind to eat (9) Develop an eating plan* (7) Share record of eating, send it through Email, forum (5) Provide restaurants information (3) |
| Being Active (99) | Keep track of activities*
(54) Check blood sugar levels before and after exercise* (18) Provide knowledge of exercise (8) Set exercise goal (7) Remind to do exercise (7) Send record of exercise through forum and email (3) Start exercising* (1) Do exercise at personal pace* (1) Mix it up* (0) Choose activities* (0) Find a friend to exercise with* (0) Take a class* (0) Join an adult league* (0) |
| Monitoring (322) | Record blood sugar levels*
(97) Record height or weight or BMI (54) Set goals (44) Record blood pressure, pulse (41) Record lab test results (25) Remind to check blood sugar* (24) Send record of blood sugar through forum and email (15) Prepare solutions when the numbers are out of the target range* (7) Provide knowledge of blood sugar (7) Record other vital signs (4) Record the spot of blood sugar testing or insulin injection (3) Learn how to use a blood sugar (glucose) meter* (1) |
| Taking Medication (164) | Keep track of medications (68) Manage medication list* (45) Calculate recommended insulin dosage (20) Remind to take medication (13) Send record of medication through forum and email (10) Provide knowledge of medication (5) Record medicine adherence (2) Clinical goal of medication* (1) |
| Problem Solving (45) | Alert and reminder for abnormal data
(38) Self-monitoring* (5) Discuss possible solutions with others* (2) Take action* (0) Learn from experience* (0) Try new solutions* (0) |
| Reducing Risks (16) | Visit the eye doctor at least once a year* (4) Take care of the feet* (4) Provide knowledge of reducing risks (3) See the doctor regularly* (2) See the dentist every six months* (1) Listen to the body* (1) Provide forum topics include diabetes complication (1) Report smoking behavior* (0) |
| Healthy Coping (14) | Record mood (8) Attend support groups* (5) Do exercise* (1) Participate in faith-based activities or meditation* (0) Pursue hobbies* (0) |
| Others (93) | Share general reports, forum topics include diabetes
management (61) General reminder (14) Provide knowledge related to diabetes (13) Export data (4) Record emergency contact information (1) |
The number in the parentheses after each of the seven behaviors indicates the sum of features related to each of the seven self-care behaviors. The number in the parentheses after each feature indicates the sum of each feature category across the entirety mobile apps.
Features from AADE7™.
Interview with Diabetes Physicians and Educators
The author (QY) conducted six interviews with two diabetes physicians and four diabetes educators during November 2016. The interviews lasted between 15 and 30 minutes. The median experience working with people with diabetes was 15 years for this group, and ranged from 14 months to 29 years.
Based on these interviews, we summarized the main reasons for lack of features addressed in DSM apps.
Regarding Problem Solving, the interviewees summarized four main reasons why features related to Problem Solving have been less developed in DSM apps.
First, features related to Problem Solving are more likely to be based on qualitative information rather than quantitative data, and as such may be hard to incorporate in a mobile app for DSM. An example of comments from interviewees:
“Healthy Eating, Being Active, Monitoring, and Taking Medication, are all the things that you can write down. For Problem Solving, that’s not easy to pinpoint.”
Second, there may be too many variables in the decision making process to address Problem Solving in DSM. An example of comments from interviewees:
“(Why did you not have breakfast?) Because I got up later. (Why did you get up late?) Because I have three kids. You need to consider many variables in the problem tree.”
Third, the interviewees also identified that Problem Solving, especially in chronic diseases, is best done with direct interaction between the learner and the educator. An example of comments from interviewees:
“There is no human interaction to support your need.”
Fourth, online search engines are easily accessible for information regarding diabetes. Many people with diabetes may be using these search engines to address Problem Solving related to DSM. The interviewees thought that when compared to the online search engines, the DSM apps failed to provide effective support for solving problems. This may be related to ease of query, and to simultaneous suggestions of possible answers within a few seconds. An example of comments from interviewees:
“When they had problems, Google was even faster than the app.”
Regarding Reducing Risks, the interviewees summarized four main reasons why the features related to Reducing Risks have been less developed in DSM apps.
First, again, as in Problem Solving, features related to Reducing Risks are not based on quantitative data. An example of comments from interviewees:
“It’s not like black and white concrete information. It’s not based on numbers.”
Second, regular follow up, and evaluation of comorbidities is part of Reducing Risks. Many people with diabetes use other tools like calendars and notebooks to set up reminders. An example of comments from interviewees:
“I see many people with diabetes set reminders in [their] calendar.”
Third, Reducing Risk needs appropriate suggestions from providers. Many people with diabetes may be unaware of their role in this process. An example of comments from interviewees:
“For example, [the person who is] quitting smoking needs to find other alternatives to replace cigarettes. [The person who involved in] Nicotine replacement therapy need suggestions from physicians.”
Fourth, many people with diabetes may lack information or resources to address risks associated with diabetes, and as such, cannot participate actively in an app feature for Reducing Risks. An example of comments from interviewees:
“I have not seen patients respond well. For example, see the dentist. The patients need to pay.”
Regarding Healthy Coping, the interviewees summarized three main reasons why the features related to Healthy Coping have been less developed in DSM apps.
First, every person with diabetes deals with not just chronic medical condition, but may be facing distinctly different social, financial, and psychological stresses in life. The interviewees thought this would make it difficult to develop a DSM app with the features related to Healthy Coping. An example of comments from interviewees:
“It is not easy to develop such an app.”
Second, Healthy Coping requires self-care and establishment of a support network. The lack of an emotional connection when using mobile apps may be a drawback. This feature would be hard to incorporate in a mobile app also. An example of comments from interviewees:
“We should consider the emotional needs. To develop an app on Healthy Coping, [a] video conference with [a] group [of] people may help.”
Third, the interviewees pointed to health disparities in diabetes, and suggested developers need to consider cultural variations in coping with life stress, including chronic diseases like diabetes. An example of comments from interviewees:
“Different cultures have different attitudes towards healthy coping. For example, Asian and African are different from American.”
Discussion
This study revealed that, compared to the AADE7™, there was an unbalanced feature development of current DSM apps. We found that many DSM apps provided features related to Healthy Eating, Monitoring, Taking Medication, and Being Active behaviors, which were positive aspects. However, few apps offered features related to Problem Solving, Reducing Risks, and Healthy Coping behaviors, which need to be developed in future DSM apps. This result was similar to Breland et al’s study, which reported that many apps supported features for Healthy Eating (44.9%), Being Active (24.7%), Self-Monitoring (48%), Medication (46.7%), and Problem Solving (29.5%).27 On the other hand, few apps supported features related to Reducing Risks (11.9%) and Healthy Coping (5.7%).27 Our result was consistent with studies by Eng and Lee4 and Arnhold et al.47 Eng and Lee’s study reviewed 516 diabetes apps for iPhone. They found the largest percentage of diabetes apps (33%) provided features for health tracking, based on quantitative data entry, such as tracking insulin doses, activity, and blood sugar levels.4 Arnhold et al’s study analyzed 656 diabetes apps from iTunes and Google Play stores. Their results showed that 348 (53%) apps provided the feature of documentation focused on recording and monitoring eating habits, physical activity, and medical therapy.47 Our study also found that features related to Healthy Eating, Monitoring, Taking Medication, and Being Active were frequently developed in mobile apps. Compared to the features analysis data from November 2015 and December 2017 (Table 1), the unbalanced feature development trend did not change much.
Reasons why few apps supported the features related to Problem Solving, Reducing Risks, and Healthy Coping need to be defined. Breland et al suggested that the two behaviors of Reducing Risks and Healthy Coping are usually addressed by direct interaction with diabetes educators.32 This was also identified by interviewees in our study. Another possible reason may be that it is hard to incorporate qualitative information into mobile apps which are easily designed for quantitative data. We found features with high appearance, such as “count carbohydrates” (79/316, 25%) under Healthy Eating, “keep track of activities” (54/99, 55%) under Being Active, “record blood sugar levels” (97/322, 30%) under Monitoring, and “keep track of medications” (68/164, 41%) are all quantitative and therefore easy to enter into an app. Emotional needs and human interactions in management of diabetes may be hard to replace by apps. For example, quitting smoking needs interaction between patients and physicians so that physicians can provide professional guidance.48 For people with diabetes, emotional interactions, such as face-to-face communication in support groups, may be a more effective method to cope with stress compared to a mobile app.49 However, features such as interactive video for supporting emotional interaction may be incorporated into DSM apps as recommended in our study by interviewees. Another reason why people with diabetes may not use mobile apps for Problem Solving, Reducing Risks, and Healthy Coping could be there are alternate efficient methods to fulfill same features other than using apps. For Problem Solving, people with diabetes could use a search engine to find answers for their questions, such as searching on Google when they have low blood glucose after exercise.
Limitations of the Study
Due to the explorative nature of the study, there were several limitations. First, the initial 1050 apps were collected during 2015. Given the rapid rate of app development, there are new DSM apps available on iTunes and Google Play stores. The results of our research may not perfectly match the current app stores. Second, we used AADE7™ to analyze features of DSM apps considering that both the ADA36 and the AGS37 recommend the AADE7™ for DSM; there may be other valid guidelines used by app developers. Third, we excluded apps that provided access to reference material only. These apps may be likely to address certain aspects of the guidelines. For example, there is an app with an e-book providing coping strategies for people with diabetes.
Conclusion
This study found that features of current DSM apps from two main app stores did not have balanced development compared to the DSM guidelines from AADE7™. Healthy Eating, Being Active, Monitoring, and Taking Medication are covered well by current DSM apps. Few apps provided features supporting Problem Solving, Reducing Risks, and Healthy Coping. These three behaviors are essential components of AADE7™ for successful DSM. Future diabetes apps should incorporate balanced features from the AADE7™ to better support changing self-management behaviors of people with diabetes. More research is needed on how we can target future app development to include features that support qualitative data entry rather than limiting apps to quantitative data.
Acknowledgments
The authors thank the diabetes physicians and educators who attended their interview.
Footnotes
Abbreviations: AADE, American Association of Diabetes Educators; ADA, American Diabetes Association; AGS, American Geriatrics Society; apps, applications; DSM, diabetes self-management; DSME, diabetes self-management education; HbA1c, hemoglobin A1c.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was funded by a grant from Center for Diabetes Translation Research (CDTR) Pilot & Feasibility (P&F) program grant awarded through National Institute of Diabetes and Digestive and Kidney Disorders (NIDDK) P30DK092950.
ORCID iD: Qing Ye  https://orcid.org/0000-0001-5442-1714
https://orcid.org/0000-0001-5442-1714
References
- 1. Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159-1171. [DOI] [PubMed] [Google Scholar]
- 2. Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561-587. [DOI] [PubMed] [Google Scholar]
- 3. Nicolucci A, Cavaliere D, Scorpiglione N, et al. A comprehensive assessment of the avoidability of long-term complications of diabetes. A case-control study. SID-AMD Italian Study Group for the Implementation of the St. Vincent Declaration. Diabetes Care. 1996;19:927-933. [DOI] [PubMed] [Google Scholar]
- 4. Eng DS, Lee JM. The promise and peril of mobile health applications for diabetes and endocrinology. Pediatr Diabetes. 2013;14:231-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Research 2 Guidance. mHealth app developer economics 2016. Available at: www.research2guidance.com. Accessed September 8, 2017.
- 6. Whitlock L, McLaughlin A, Harris M, Bradshaw J. The design of mobile technology to support diabetes self-management in older adults. In: Zhou J, Salvendy G. eds. Human Aspects of IT for the Aged Population Design for Everyday Life. Lecture Notes in Computer Science, vol. 9194 Cham, Switzerland: Springer; 2015:211-221. [Google Scholar]
- 7. Hou C, Carter B, Hewitt J, Francisa T, Mayor S. Do mobile phone applications improve glycemic control (HbA1c) in the self-management of diabetes? A systematic review, meta-analysis, and GRADE of 14 randomized trials. Diabetes Care. 2016;39:2089-2095. [DOI] [PubMed] [Google Scholar]
- 8. Quinn CC, Clough SS, Minor JM, Lender D, Okafor MC, Gruber-Baldini A. WellDoc mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol Ther. 2008;10:160-168. [DOI] [PubMed] [Google Scholar]
- 9. Orsama AL, Lahteenmaki J, Harno K, et al. Active assistance technology reduces glycosylated hemoglobin and weight in individuals with type 2 diabetes: results of a theory-based randomized trial. Diabetes Technol Ther. 2013;15:662-669. [DOI] [PubMed] [Google Scholar]
- 10. Yoo HJ, Park MS, Kim TN, et al. A Ubiquitous Chronic Disease Care system using cellular phones and the internet. Diabetic Med. 2009;26:628-635. [DOI] [PubMed] [Google Scholar]
- 11. Istepanian RS, Zitouni K, Harry D, et al. Evaluation of a mobile phone telemonitoring system for glycaemic control in patients with diabetes. J Telemed Telecare. 2009;15:125-128. [DOI] [PubMed] [Google Scholar]
- 12. Holmen H, Torbjornsen A, Wahl AK, et al. A mobile health intervention for self-management and lifestyle change for persons with type 2 diabetes. Part 2: one-year results from the Norwegian randomized controlled trial renewing health. JMIR Mhealth Uhealth. 2014;2:e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nagrebetsky A, Larsen M, Craven A, et al. Stepwise self-titration of oral glucose-lowering medication using a mobile telephone-based telehealth platform in type 2 diabetes: a feasibility trial in primary care. J Diabetes Sci Technol. 2013;7:123-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Quinn CC, Shardell MD, Terrin ML, Barr EA, Ballew SH, Gruber-Baldini AL. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011;34:1934-1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Faridi Z, Liberti L, Shuval K, Northrup V, Ali A, Katz DL. Evaluating the impact of mobile telephone technology on type 2 diabetic patients’ self-management: the NICHE pilot study. J Eval Clin Pract. 2008;14:465-469. [DOI] [PubMed] [Google Scholar]
- 16. Waki K, Fujita H, Uchimura Y, et al. DialBetics: a novel smartphone-based self-management support system for type 2 diabetes patients. J Diabetes Sci Technol. 2014;8:209-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Takenga C, Berndt RD, Musongya O, et al. An ICT-based diabetes management system tested for health care delivery in the African context. Int J Telemed Appl. 2014;2014:437307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wu Y, Yao X, Vespasiani G, et al. Mobile app-based interventions to support diabetes self-management: a systematic review of randomized controlled trials to identify functions associated with glycemic efficacy. JMIR Mhealth Uhealth. 2017;5:e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kirwan M, Vandelanotte C, Fenning A, Duncan MJ. Diabetes self-management smartphone application for adults with type 1 diabetes: randomized controlled trial. J Med Internet Res. 2013;15:e235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hsu WC, Lau KH, Huang R, et al. Utilization of a cloud-based diabetes management program for insulin initiation and titration enables collaborative decision making between healthcare providers and patients. Diabetes Technol Ther. 2016;18:59-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Baron JS, Hirani S, Newman SP. A randomised, controlled trial of the effects of a mobile telehealth intervention on clinical and patient-reported outcomes in people with poorly controlled diabetes. J Telemed Telecare. 2017;23:207-216. [DOI] [PubMed] [Google Scholar]
- 22. Drion I, Pameijer LR, van Dijk PR, Groenier KH, Kleefstra N, Bilo HJ. The effects of a mobile phone application on quality of life in patients with type 1 diabetes mellitus: a randomized controlled trial. J Diabetes Sci Technol. 2015;9:1086-1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rossi MC, Nicolucci A, Lucisano G, et al. Impact of the “Diabetes Interactive Diary” telemedicine system on metabolic control, risk of hypoglycemia, and quality of life: a randomized clinical trial in type 1 diabetes. Diabetes Technol Ther. 2013;15:670-679. [DOI] [PubMed] [Google Scholar]
- 24. Charpentier G, Benhamou PY, Dardari D, et al. The Diabeo software enabling individualized insulin dose adjustments combined with telemedicine support improves HbA1c in poorly controlled type 1 diabetic patients: a 6-month, randomized, open-label, parallel-group, multicenter trial (TeleDiab 1 Study). Diabetes Care. 2011;34:533-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rossi MC, Nicolucci A, Di Bartolo P, et al. Diabetes Interactive Diary: a new telemedicine system enabling flexible diet and insulin therapy while improving quality of life: an open-label, international, multicenter, randomized study. Diabetes Care. 2010;33:109-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chomutare T, Fernandez-Luque L, Arsand E, Hartvigsen G. Features of mobile diabetes applications: review of the literature and analysis of current applications compared against evidence-based guidelines. J Med Internet Res. 2011;13:e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Breland JY, Yeh VM, Yu J. Adherence to evidence-based guidelines among diabetes self-management apps. Transl Behav Med. 2013;3:277-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Povey RC, Clark-Carter D. Diabetes and healthy eating: a systematic review of the literature. Diabetes Educ. 2007;33:931-959; discussion 960-931. [DOI] [PubMed] [Google Scholar]
- 29. Kavookjian J, Elswick BM, Whetsel T. Interventions for being active among individuals with diabetes: a systematic review of the literature. Diabetes Educ. 2007;33:962-988; discussion 989-990. [DOI] [PubMed] [Google Scholar]
- 30. McAndrew L, Schneider SH, Burns E, Leventhal H. Does patient blood glucose monitoring improve diabetes control? A systematic review of the literature. Diabetes Educ. 2007;33:991-1011; discussion 1012-1013. [DOI] [PubMed] [Google Scholar]
- 31. Odegard PS, Capoccia K. Medication taking and diabetes: a systematic review of the literature. Diabetes Educ. 2007;33:1014-1029. [DOI] [PubMed] [Google Scholar]
- 32. Hill-Briggs F, Gemmell L. Problem solving in diabetes self-management and control: a systematic review of the literature. Diabetes Educ. 2007;33:1032-1050. [DOI] [PubMed] [Google Scholar]
- 33. Boren SA, Gunlock TL, Schaefer J, Albright A. reducing risks in diabetes self-management: a systematic review of the literature. Diabetes Educ. 2007;33:1053-1077. [DOI] [PubMed] [Google Scholar]
- 34. Fisher EB, Thorpe CT, Devellis BM, Devellis RF. Healthy coping, negative emotions, and diabetes management: a systematic review and appraisal. Diabetes Educ. 2007;33:1080-1103; discussion 1104-1086. [DOI] [PubMed] [Google Scholar]
- 35. Boren SA. AADE7™ self-care behaviors: systematic reviews. Diabetes Educ. 2007;33:866, 871. [DOI] [PubMed] [Google Scholar]
- 36. Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of diabetes educators, and the Academy of nutrition and dietetics. Clin Diabetes. 2016;34:70-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. American Geriatrics Society Expert Panel on the Care of Older Adults with Diabetes Mellitus, Moreno G, Mangione CM, Kimbro L, Vaisberg E. Guidelines abstracted from the American Geriatrics Society guidelines for improving the care of older adults with diabetes mellitus: 2013 update. J Am Geriatr Soc. 2013;61:2020-2026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. American Association of Diabetes Educators. AADE7™ self care behaviors. American Diabetes Educators Association. 2014. Available at: https://www.diabeteseducator.org/docs/default-source/legacy-docs/_resources/pdf/publications/aade7_position_statement_final.pdf?sfvrsn=4. Accessed August 18, 2017.
- 39. Austin MM. Diabetes educators: partners in diabetes care and management. Endocr Pract. 2006;12(suppl 1):138-141. [DOI] [PubMed] [Google Scholar]
- 40. Number of apps available in leading app stores as of March 2017. Available at: https://www.statista.com/statistics/276623/number-of-apps-available-in-leading-app-stores/. Accessed September 15, 2017.
- 41. Lee YS. Older Adults’ User Experiences with Mobile Phones: Identification of User Clusters and User Requirements. Blacksburg: Virginia Polytechnic Institute and State University; 2007. [Google Scholar]
- 42. Martinez-Perez B, de la Torre-Diez I, Lopez-Coronado M. Mobile health applications for the most prevalent conditions by the World Health Organization: review and analysis. J Med Internet Res. 2013;15:e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Caburnay CA, Graff K, Harris JK, et al. Evaluating diabetes mobile applications for health literate designs and functionality, 2014. Prev Chronic Dis. 2015;12:1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Demidowich AP, Lu K, Tamler R, Bloomgarden Z. An evaluation of diabetes self-management applications for Android smartphones. J Telemed Telecare. 2012;18:235-238. [DOI] [PubMed] [Google Scholar]
- 45. El-Gayar O, Timsina P, Nawar N, Eid W. Mobile applications for diabetes self-management: status and potential. J Diabetes Sci Technol. 2013;7:247-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Anderson K, Burford O, Emmerton L. App chronic disease checklist: protocol to evaluate mobile apps for chronic disease self-management. JMIR Res Protoc. 2016;5:e204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Arnhold M, Quade M, Kirch W. Mobile applications for diabetics: a systematic review and expert-based usability evaluation considering the special requirements of diabetes patients age 50 years or older. J Med Internet Res. 2014;16:e104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Edwards SA, Callaghan RC, Mann RE, Bondy SJ. Association between socioeconomic status and access to care and quitting smoking with and without assistance. Nicotine Tob Res. 2017;20:40-49. [DOI] [PubMed] [Google Scholar]
- 49. Chew BH, Vos RC, Shariff Ghazali S, et al. The effectiveness of a value-based emotion-cognition-focused educational programme to reduce diabetes-related distress in Malay adults with Type 2 diabetes (VEMOFIT): study protocol for a cluster randomised controlled trial. BMC Endocr Disord. 2017;17:22. [DOI] [PMC free article] [PubMed] [Google Scholar]