Abstract
Background
Reducing cigarette nicotine content mayreduce smoking. Studies suggest that smokers believe that nicotine plays a role in smokingrelated morbidity. This may lead smokers to assume that reduced nicotine means reduced risk, and attenuate potential positive effects on smoking behaviour.
Methods
Data came from a multisite randomized trial in which smokers were assigned to use cigarettes varying in nicotine content for 6 weeks. We evaluated associations between perceived and actual nicotine content with perceived health risks using linear regression, and associations between perceived nicotine content and perceived health risks with smoking outcomes using linear and logistic regression.
Findings
Perceived—not actual—nicotine content was associated with perceived health risks; compared with those perceiving very low nicotine, individuals who perceived low (β=0.72, 95% CI 0.26 to 1.17), moderate (β=1.02, 95% CI 0.51 to 1.53) or high/very high nicotine (β=1.66, 95% CI 0.87 to 2.44) perceived greater health risks. Nevertheless, individuals perceiving low (OR=0.48, 95% CI 0.32 to 0.71) or moderate nicotine (OR=0.42, 95% CI 0.27 to 0.66) were less likely than those perceiving very low nicotine to report that they would quit within 1 year if only investigational cigarettes were available. Lower perceived risk of developing other cancers and heart disease was also associated with fewer cigarettes/day at week 6.
Conclusions
Although the perception of reduced nicotine is associated with a reduction in perceived harm, it may not attenuate the anticipated beneficial effects on smoking behaviour. These findings have implications for potential product standards targeting nicotine and highlight the need to clarify the persistent harms of reduced nicotine combusted tobacco products.
INTRODUCTION
The passage of the Family Smoking Preventionand Tobacco Control Act1authorised the Food and Drug Administration to mandate the reduction—though not elimination—of the nicotine content in cigarettes nationwide. It is hypothesised that reducing nicotine in cigarettes to a level below that which sustains dependence could help current smokers to reduce smoking or quit, as well as decrease the likelihood that new smokers will become dependent.2 ,3 Research lends support to a nicotine reduction policy, as recent work suggests that the use of reduced nicotine content (ie, cigarettes with a nicotine content lower than that of typical commercially available cigarette) cigarettes reduces smoking, nicotine dependence and exposure to nicotine and toxicants.3–6 Most recently, in a multisite randomised clinical trial involving 6 week exposure to cigarettes that vary in nicotine content,5 smokers assigned to smoke reduced nicotine content (RNC) cigarettes smoked fewer cigarettes per day (CPD) and had decreased biomarkers of exposure to nicotine compared with a normal nicotine content (NNC) control condition, with little evidence of compensatory smoking behaviours.
Research also suggests that smokers believe that nicotine in cigarettes is an important cause of smoking-related morbidity and mortality with a majority of smokers identifying nicotine as a potential cause of strokes, heart attack/heart disease, asthma7 and lung cancer.8–11 Given beliefs about the role of nicotine in the harms associated with cigarettes, smokers may perceive that RNC cigarettes are less harmful. Indeed, prior research has revealed that pregnant smokers12 and individuals exposed to advertising for lower nicotine cigarettes (ie, Quest cigarettes)13 believe that RNC cigarettes are safer than NNC cigarettes. In both of these studies, participants were naïve to and did not use RNC cigarettes as part of the study. Another study14 showed that, after brief exposure (ie, one study session) to investigational cigarettes that varied in nicotine content under double-blind conditions, participants sampling cigarettes with high and intermediate nicotine content estimated those cigarettes would engender greater risk for all health conditions assessed (eg, lung cancer, bronchitis) relative to low nicotine content cigarettes. An additional study15 briefly exposed all participants to RNC cigarettes but told them that their cigarette contained (1) ‘average’ or (2) ‘very low’ nicotine content. When participants were told that the cigarettes had ‘very low’ nicotine content, they rated them as less harmful to their health. Though acute effects have been examined, to our knowledge, the effects of prolonged use of RNC cigarettes on perceived risk for developing smoking-related health problems are unknown. Given that a nationwide nicotine reduction policy would result in long-term exposure to RNC products, it is important to investigate whether longer term experience with RNC cigarettes may influence users’ health risk perceptions. Thus, it is important to investigate the effects of the nicotine content of cigarettes—both perceived and actual—following prolonged use of RNC cigarettes on the perception of risk associated with smoking.
Health risk perceptions of nicotine could have important influences on smoking-related outcomes. Prior work3–5,16,17 has demonstrated that the actual nicotine content of investigational cigarettes is associated with various smoking-re-lated outcomes (eg, cigarettes smoked per day, self-reported quit attempts). Accordingly, perceived nicotine content may be similarly associated with smoking-related behavioural outcomes; however, the nature of this relationship remains unknown. Specifically, providing information about nicotine content may impart the perception of RNC cigarettes being less harmful and may deter current smokers from attempting to quit and encourage resumption of smoking among ex-smokers.18,19 These inaccurate perceptions run the risk of mitigating some of the potential beneficial public health effects of RNC cigarettes in the event that a nationwide nicotine reduction policy is implemented. Lending support to this possibility, one study indicated that among smokers who provided more favourable initial taste and strength ratings of RNC cigarettes, having more false beliefs about their benefits was associated with greater consumption of RNC cigarettes.20
Importantly, the association between nicotine content and perceived health risks may be moderated by other constituents in cigarettes that alter sensory perceptions of the cigarettes, such as menthol flavouring and/or tar. Menthol has a number of respiratory effects, including reduction of smoke harshness, facilitation of deeper and more prolonged inhalation, and cough suppression.21 Its cooling and anaesthetic properties likely contribute to smoothness, mildness, easing of uncomfortable physical symptoms like irritation, perceived lower nicotine and tar yield, and the perception that cigarettes with menthol as a characterising flavour (ie, ‘menthol cigarettes’) are ‘less strong’.9,22 Previous research9,23–26 shows that cigarettes with these attributes are perceived to impart reduced harm. Thus, there may be a difference in perceived health risk of smoking between menthol and non menthol cigarettes, and the impact of perceived and actual nicotine content on this effect remains unexplored.
This study used data from a trial conducted by Donny and colleagues,5 which offered a unique opportunity to evaluate the following research questions: (1) Is perceived versus actual nicotine content of investigational cigarettes associated with perceived health risks of using these products; (2) Is perceived nicotine content of investigational cigarettes associated with smoking-related outcomes; and (3) Are perceived health risks associated with smoking-related outcomes. Furthermore, we explored whether menthol smoking status moderated the afore-mentioned associations. Given the documented perceptions that nicotine is related to smoking-related illness,7–10 we hypothesised that smokers who perceive less nicotine in their assigned cigarettes would also perceive these cigarettes as less harmful, and that this effect would be greater in those who smoke menthol cigarettes compared with non-menthol cigarettes. Find-ings have the potential to inform regulatory efforts by addressing a common concern about low nicotine product standards and building an empirical basis for public messaging campaigns that could accompany regulatory action.
METHODS
Participants
From 2013 to 2014, daily smokers were recruited using flyers, direct mailings, television/radio, websites and other advertisements. Inclusion criteria were as follows: age>18; smoking>5 CPD; expired breath carbon monoxide (CO) >8 parts per million (ppm) or urinary cotinine >100 ng/mL. Exclusion criteria were as follows: intention to quit smoking in next 30 days, use of other tobacco products on >9 of past 30 days, frequent binge drinking, significant or unstable medical/psychiatric conditions, positive illicit drug toxicology screen (other than tetrahydrocannabinol (THC)), pregnancy/breastfeeding and exclusively using ‘roll your own’ cigarettes. A total of 839 eligible smokers were randomised and 780 completed the study.
Study design
The methods for the parent study have been described in detail elsewhere.5 The sevenarm, doubleblind, 10-site randomised trial included a 2-week baseline and 6-week investigational period. During the baseline period, participants purchased and smoked their usual brand of cigarettes. In the parent study, participants were randomly assigned to smoke investigational cigarettes that varied in nicotine content (described below); one condition was assigned to smoke their usual brand of cigarette. For the present analysis, participants assigned to smoke their usual brand cigarettes were excluded since they were not blinded to nicotine condition and, relatedly, perceived nicotine content was not assessed in this group. Participants received menthol or non-menthol cigarettes, according to their preference. All investigators, staff and participants were blind to condition assign-ment other than the usual brand condition. During the informed consent process, participants were told that the study cigarettes may or may not contain lower nicotine than their usual brand. Study cigarettes were supplied by the National Institute on Drug Abuse (NIDA; NOT-DA-14–004).
Participants completed weekly laboratory assessments during which they were provided with a free 14-day cigarette supply. The purpose of providing participants with a 2-week supply was to account for missed visits and potential compensatory smoking. Participants were asked not to use other cigarettes; however, there was no penalty for non-compliance. Brief weekly counselling aimed to increase compliance by providing participants with strategies to overcome barriers to only smoking study cigarettes. Subjective, behavioural and physiological measures, described below, were collected weekly throughout the baseline and intervention periods. Participants were contacted by telephone 30 days after their last session to ascertain whether they had made a quit attempt since the last study visit. Participants could earn up to $835 for completing all study procedures.
Measures
Sociodemographic characteristics
Sociodemographic characteristics in this analysis included sex, age (continuous), race (Caucasian, African American, other) and education (less than high school/general equivalency degree (GED), high school graduate/GED, greater than high school/ GED). Menthol cigarette smoking status was assessed by asking participants the following question: ‘Would you prefer to be assigned to smoke a menthol or non-menthol cigarette for the duration of the study?’.
Nicotine condition: assigned and perceived
Participants were randomly assigned to smoke investigational cigarettes of varying nicotine content: 15.8 mg of nicotine per g of tobacco (which served as a study cigarette control group), 5.2 mg/g, 2.4 mg/g, 1.3 mg/g, 0.4 mg/g (regular tar) and 0.4 mg/g (high tar) or their usual brand cigarettes. Tar yields (Interna-tional Organisation for Standardization) were 8–10 mg for all investigational cigarettes except for 0.4 mg/g (high tar) which had a tar yield of 13 mg. At postrandomisation week 6, participants assigned to smoke investigational cigarettes were asked the following question: ‘What level of nicotine do you think was in your study cigarette?’ Response options included very low in nicotine, low in nicotine, moderate amount of nicotine, high in nicotine, very high in nicotine.
Perceived health risks
The Perceived Health Risks scale27 was administered at the baseline 1 (eg, 1 week before randomisation) and week 6 study visits. At baseline 1, participants responded to the statement: ‘Based on smoking your usual brand cigarette, indicate what you believe your risk is for developing [health condition]’, while at week 6 participants were presented with: ‘Based on smoking your assigned study cigarettes, indicate what you believe your risk is for developing [health condition]’. Conditions evaluated included lung cancer, emphysema, bronchitis, other cancers, heart disease and stroke. Responses involved rating perceived disease risk on a 1–10 visual analogue scale, with 1 anchored at ‘very low risk’ and 10 anchored at ‘very high risk’. Health conditions were assessed individually, as well as using a measure of perceived risk that averaged across all health conditions.
Smoking outcome measures
The number of CPD was derived via an Interactive Voice Response system that automatically called participants daily; participants reported the number of cigarettes smoked the previous day. After being assigned to investigational cigarettes, participants separately reported the study and non-study cigarettes that they smoked. Weekly averages of daily total CPD (study + non-study) were computed (ie, days between each weekly session). CPD (continuous) in the present analyses came from the postrandomisation week 6. At week 6, participants were also asked the following question: ‘Starting today, if the study cigarette was the only type of cigarette available for purchase, by a year from now I would (stop smoking/smoke less/smoke same/smoke more).’ Responses were dichotomised (stop smoking vs something else). Additionally, during the 30 day follow up phone call (when participants no longer had access to the investigational experimental cigarettes), participants reported whether they had made a quit attempt since completing the study.
Statistical analyses
Of the 780 participants who completed the parent study, the present sample includes n=663 who were randomised to inves-tigational cigarettes and completed the week 6 visit. The associations between perceived and actual nicotine content with perceived health risks were evaluated using multivariate linear regression. For all analyses of perceived nicotine content, the high and very high categories were combined due to low endorsement of both options (3.9% and 2.9%, respectively). Similarly, the associations between perceived nicotine content and perceived risk of developing smoking-related diseases at week 6 with smoking outcomes measures were evaluated using multivariate linear (CPD at week 6) or logistic regression (quit attempts, quitsmoking within 1 year). Throughout, all multivariate regression analyses were adjusted for the baseline value (when appropriate) and covariates significantly associated (ie, p<0.05) with the outcome in an unadjusted model. Menthol status was assessed as a moderator for all associations by testing menthol-by-covariate interaction terms in all multivariate regression models. To further explore associations between assigned and perceived nicotine content, assigned (15.8 mg vs 0.4–5.2 mg/g conditions) and perceived (low very low vs moderate very high) nicotine content were dichotomised. Post hoc analyses were also conducted to evaluate the potential mediating effects of (1) perceived nicotine content on the association between perceived health risks and CPD and (2) perceived health risks on the association between perceived nicotine content and self-predicted cessation within 1 year. All analyses were conducted using STATA SE statistical software V. 14.0.28
RESULTS
Participant characteristics
Approximately half of the sample (55.8%) was male, and 50.2% were Caucasian. The average age was 42.1 (SD=13.3) and most (57.3%) had more than a high school education. Fifty-seven per cent of participants smoked menthol cigarettes. African American race (p’s<0.001) and menthol status (p’s<0.001) were negatively associated, and having attended college (p’s=0.001–0.007) was positively associated with perceived risk for all health conditions at week 6.
Perceived and actual nicotine content
All interaction terms with menthol were found to be non-signif-icant, were removed and thus are not discussed further. At week 6, 33.8% perceived the nicotine content of their assigned ciga-rettes to be very low, 35.6% to be low, 23.8% to be moderate and 6.8% to be high or very high. Seventy-two per cent of participants assigned to the RNC group perceived that they were assigned to smoke low or very low nicotine content cigarettes, compared with 54.0% of participants assigned to the NNC group. Of participants assigned to the NNC group, 45.9% perceived that they were assigned to smoke moderate–high nico-tine cigarettes; 72.5% of individuals assigned to the RNC group perceived that they were assigned to smoke low or very low nicotine content cigarettes. The odds that a participant assigned to the RNC group perceived low/very low nicotine content cigarettes were more than twice that of participants randomised to the NNC group (OR=2.24, 95% CI 1.47 to 3.39).
Perceived nicotine content as a correlate of perceived health risks
Perceived nicotine content was significantly associated with an average measure of perceived health risks, even after adjusting for potential confounders (table 1; figure 1a). This significant association persisted for each of the diseases assessed: compared with perceived very low nicotine content, perceived low (β’s=0.71– 0.97, p’s<0.001–0.004), moderate (β’s=0.91–1.27, p’s<0.001–0.001) and high/very high (β’s=1.72–1.88, p’s<0.001–0.001) nicotine contents were associated with greater perceived risk of developing all health conditions that were assessed.
Table 1.
Linear regression analyses for association between perceived nicotine content and perceived disease risk of assigned SPECTRUM cigarettes (n=663)
| Adjusted* β (95% CI) | |
|---|---|
| Average of all perceived health risks | |
| Perceived nicotine content | |
| High/very high nicotine | 1.66 (0.87 to 2.44) |
| Moderate nicotine | 1.02 (0.51 to 1.53) |
| Low nicotine | 0.72 (0.26 to 1.17) |
| Very low nicotine | REF |
| Lung cancer | |
| Perceived nicotine content | |
| High/very high nicotine | 1.91 (1.10 to 2.72) |
| Moderate nicotine | 1.28 (0.75 to 1.81) |
| Low nicotine | 0.94 (0.47 to 1.41) |
| Very low nicotine | REF |
| Emphysema | |
| Perceived nicotine content | |
| High/very high nicotine | 1.77 (0.93 to 2.61) |
| Moderate nicotine | 1.14 (0.59 to 1.68) |
| Low nicotine | 0.68 (0.20 to 1.17) |
| Very low nicotine | REF |
| Bronchitis | |
| Perceived nicotine content | |
| High/very high nicotine | 1.77 (0.92 to 2.61) |
| Moderate nicotine | 1.01 (0.46 to 1.56) |
| Low nicotine | 0.72 (0.23 to 1.21) |
| Very low nicotine | REF |
| Other cancers | |
| Perceived nicotine content | |
| High/very high nicotine | 1.49 (0.65 to 2.32) |
| Moderate nicotine | 1.02 (0.48 to 1.56) |
| Low nicotine | 0.66 (0.17 to 1.14) |
| Very low nicotine | REF |
| Heart disease | |
| Perceived nicotine content | |
| High/very high nicotine | 1.74 (0.90 to 2.58) |
| Moderate nicotine | 0.99 (0.45 to 1.54) |
| Low nicotine | 0.77 (0.29 to 1.26) |
| Very low nicotine | REF |
| Stroke | |
| Perceived nicotine content | |
| High/very high nicotine | 1.76 (0.91 to 2.61) |
| Moderate nicotine | 0.90 (0.34 to 1.45) |
| Low nicotine | 0.74 (0.25 to 1.23) |
| Very low nicotine | REF |
Adjusted for race/ethnicity, educational attainment, actual nicotine content, menthol status, cigarettes smoked per day and baseline perceived risk.
Note, Bold text indicates statistically significant findings.
Figure 1.
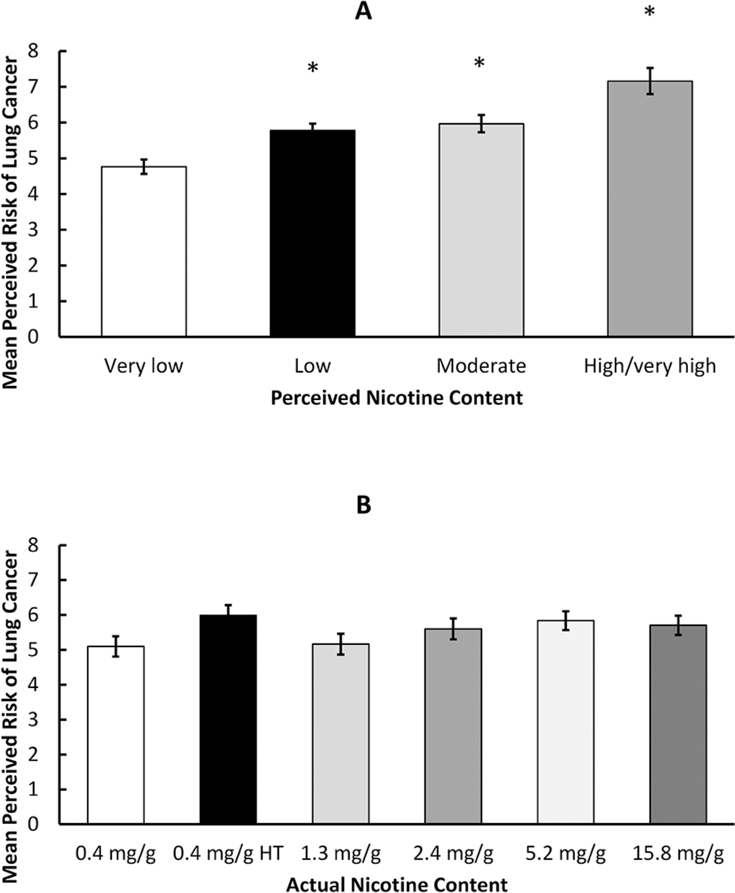
Mean (SE) perceived risk of developing smoking-related disease by perceived nicotine content (A) and actual nicotine content (B) of investigational cigarettes compared with perceived very low nicotine content, perceived low, moderate and high/very high nicotine content were significantly associated with greater perceived risk of developing smoking-related disease (A), while no associations were observed between actual nicotine content and perceived risk of developing smoking-related disease (B). * indicates p<0.05 comparing perceived low, moderate and high/very high nicotine content to perceived very low nicotine content.
Actual nicotine content as correlates of perceived health risks
After adjusting for race, education, baseline perceived risk and menthol status, there were no associations between actual nicotinecontent and an average measure of perceived health risks (table 2; figure 1b). However, when examining associationsAfter adjusting for race, education, baseline perceived risk andmenthol status, there were no associations between actual nicotine content and an average measure of perceived health risks (table 2; figure 1b). However, when examining associations between actual content and individual diseases, participants in the 0.4 mg/g high tar group perceived greater risk of developing lung cancer (β=0.68, 95% CI 0.01 to 1.34) and stroke (β=0.93, 95% CI 0.24 to 1.62) compared with the 0.4 mg/g group. No additional significant associations between actual nicotine content and perceived health risk were observed.
Table 2.
Linear regression analyses for association between actual nicotine content and perceived disease risk of assigned SPECTRUM cigarettes (n=663)
| Adjusted* β (95% CI) | |
|---|---|
| Average of all perceived health risks | |
| 15.8 mg/g† | 0.30 (−0.35 to 0.95) |
| 5.2 mg/g | 0.44 (−0.20 to 1.09) |
| 2.4 mg/g | 0.40 (−0.25 to 1.05) |
| 1.3 mg/g | 0.11 (−0.53 to 0.75) |
| 0.4 mg/g HT‡ | 0.61 (−0.03 to 1.25) |
| 0.4 mg/g | REF |
| Lung cancer | |
| 15.8 mg/g† | 0.41 (−0.27 to 1.09) |
| 5.2 mg/g | 0.62 (−0.04 to 1.30) |
| 2.4 mg/g | 0.60 (−0.07 to 1.28) |
| 1.3 mg/g | 0.11 (−0.56 to 0.77) |
| 0.4 mg/g HT‡ | 0.65 (−0.01 to 1.32) |
| 0.4 mg/g | REF |
| Emphysema | |
| 15.8 mg/g | 0.33 (−0.36 to 1.03) |
| 5.2 mg/g | 0.37 (−0.32 to 1.06) |
| 2.4 mg/g | 0.42 (−0.27 to 1.11) |
| 1.3 mg/g | 0.10 (−0.59 to 0.78) |
| 0.4 mg/g HT | 0.49 (−0.19 to 1.18) |
| 0.4 mg/g | REF |
| Bronchitis | |
| 15.8 mg/g | 0.32 (−0.39 to 1.02) |
| 5.2 mg/g | 0.66 (−0.04 to 1.35) |
| 2.4 mg/g | 0.49 (−0.21 to 1.19) |
| 1.3 mg/g | 0.24 (−0.45 to 0.94) |
| 0.4 mg/g HT | 0.60 (−0.09 to 1.29) |
| 0.4 mg/g | REF |
| Other cancers | |
| 15.8 mg/g | 0.38 (−0.31 to 1.07) |
| 5.2 mg/g | 0.36 (−0.32 to 1.04) |
| 2.4 mg/g | 0.43 (−0.26 to 1.12) |
| 1.3 mg/g | −0.03 (−0.71 to 0.65) |
| 0.4 mg/g HT | 0.52 (−0.16 to 1.20) |
| 0.4 mg/g | REF |
| Heart disease | |
| 15.8 mg/g | 0.13 (−0.57 to 0.83) |
| 5.2 mg/g | 0.39 (−0.30 to 1.08) |
| 2.4 mg/g | 0.27 (−0.42 to 0.97) |
| 1.3 mg/g | 0.13 (−0.56 to 0.82) |
| 0.4 mg/g HT | 0.56 (−0.12 to 1.25) |
| 0.4 mg/g | REF |
| Stroke | |
| 15.8 mg/g | 0.33 (−0.38 to 1.04) |
| 5.2 mg/g | 0.45 (−0.25 to 1.14) |
| 2.4 mg/g | 0.38 (−0.33 to 1.08) |
| 1.3 mg/g | 0.15 (−0.54 to 0.84) |
| 0.4 mg/g HT | 0.91 (0.21 to 1.60) |
| 0.4 mg/g | REF |
Adjusted for race/ethnicity, education, baseline perceived risk and menthol status.
mg/g = milligrams of nicotine per gram of tobacco.
HT = high tar.
Note, Bold text indicates statistically significant findings.
Perceived nicotine content as correlates of smoking outcomes
Compared with participants who perceived very low nicotine in their investigational cigarettes and controlling for actual nicotine condition, individuals who perceived low (OR=0.48, 95% CI 0.32 to 0.71) or moderate nicotine (OR=0.42, 95% CI 0.27 to 0.66) were less likely to report that they would stop smoking if the investigational cigarettes were the only ones available on the market (table 3). No additional significant associations were observed between perceived nicotine content and smoking outcomes. Furthermore, we did not find evidence that perceived health risks mediated the association between perceived nicotine content and self-predicted cessation in 1 year (not shown).
Table 3.
Linear and logistic regression analyses for associations between perceived nicotine content with smoking related outcomes
| Outcome | Adjusted* β or OR (95% CI) |
|---|---|
| Cigarettes per day at week 6 | |
| High/very high nicotine | −1.18 (−3.63 to 1.28) |
| Moderate nicotine | 0.24 (−1.37 to 1.85) |
| Low nicotine | 1.12 (−0.31 to 2.54) |
| Very low nicotine | REF |
| Quitting smoking in 1 year | |
| High/very high nicotine | 0.80 (0.41 to 1.54) |
| Moderate nicotine | 0.42 (0.27 to 0.66) |
| Low nicotine | 0.48 (0.32 to 0.71) |
| Very low nicotine | REF |
| Any quit attempt(s) | |
| High/very high nicotine | 0.52 (0.21 to 1.25) |
| Moderate nicotine | 1.29 (0.79 to 2.12) |
| Low nicotine | 0.98 (0.63 to 1.53) |
| Very low nicotine | REF |
Adjusted for actual nicotine condition and corresponding baseline characteristic (when available).
Note, Bold text indicates statistically significant findings.
Perceived health risks as correlates of smoking outcomes
A greater average perceived risk was associated with an 8% decreased likelihood (adjusted odds ratio (aOR)=0.92, 95% CI 0.85 to 0.99) of reporting having made a quit attempt since the end of the study; no significant associations were observed between an average measure of perceived health risks and CPD or self-predicted cessation in 1 year (table 4). When examining individual perceived health risks, higher perceived risk of developing lung cancer, emphysema, bronchitis and other cancers were associated with a slightly decreased likelihood of making a quit attempt since the end of the study (aORs=0.91–0.92). No additional significant associations were observed between perceived health risks and smoking outcomes. We did not find evidence that perceived nicotine content mediated the association between perceived health risks and CPD (not shown).
Table 4.
Associations between perceived risks of developing smoking-related conditions and week 6 and 30-day follow-up outcomes
| Cigarettes per day | Quitting smoking in 1 year | Any quit attempt(s) | |
|---|---|---|---|
|
Adjusted*
β (95% CI) |
Adjusted*
OR (95% CI) |
Adjusted*
OR (95% CI) |
|
| Average of all perceived health risks | 0.16 (−0.09 to 0.40) | 0.98 (0.92 to 1.04) | 0.92 (0.85 to 0.99) |
| Lung cancer | 0.16 (−0.07 to 0.39) | 0.98 (0.92 to 1.04) | 0.91 (0.85 to 0.97) |
| Emphysema | 0.16 (−0.07 to 0.38) | 0.98 (0.92 to 1.04) | 0.92 (0.86 to 0.99) |
| Bronchitis | 0.13 (−0.10 to 0.35) | 1.00 (0.94 to 1.05) | 0.92 (0.86 to 0.99) |
| Other cancers | 0.16 (−0.07 to 0.39) | 0.98 (0.93 to 1.04) | 0.92 (0.86 to 0.99) |
| Heart disease | 0.16 (−0.07 to 0.38) | 0.98 (0.93 to 1.04) | 0.94 (0.87 to 1.00) |
| Stroke | 0.08 (−0.15 to 0.30) | 0.99 (0.93 to 1.05) | 0.96 (0.89 to 1.02) |
Adjusted for baseline perceived risk and corresponding baseline characteristic (when available).
Note, Bold text indicates statistically significant findings.
DISCUSSION
Perceived nicotine content of investigational cigarettes, but not the actual nicotine content, was significantly associated with perceived health risks for lung cancer, emphysema, bronchitis, other cancers, heart disease and stroke. The observed associations were dose dependent in nature. Compared with individuals who perceived that their investigational cigarettes contained very low nicotine, the greater the perceived nicotine content, the greater the corresponding perceived health risks. These findings are consistent with, and build on, prior work indicating that smokers believe that nicotine is an important cause of smoking-related health conditions.7–10 Given the belief that nicotine is responsible for the health risks of smoking, it logically follows that cigarettes with known or perceived lower nicotine may be perceived as less harmful.
The belief that RNC cigarettes are less harmful than their NNC counterparts has the potential to be detrimental if a nico-tine product standard is enacted, or if RNC cigarettes become available on an open market. According to the Health Belief Model29—in which perceived risk influences decisions to engage in health-related behaviours—lower perceived risk regarding RNC cigarettes could result in decreased motivation to reduce or quit smoking and resumption of smoking among former smokers. In fact, research shows that smokers who have developed inaccurate beliefs about the benefits of reduced nicotine yield products (ie, ‘light’ and ‘ultralight’ cigarettes) take these beliefs into account when selecting cigarettes and this likely contributes to continued smoking and reduced intentions to quit.30–35 Moreover, inaccurate beliefs about the harms associated with nicotine have the potential to decrease interest in, and uptake of, e-cigarettes for the purpose of harm reduction, as well as nicotine replacement therapy (NRT) products for smoking cessation.10
However, we failed to observe evidence that the perception of reduced nicotine negatively impacted smoking outcomes. In fact, perceived very low nicotine content, compared with low and moderate nicotine content, was related to greater estimated odds of smoking cessation within a year if the very low nico-tine content cigarettes were the only cigarettes on the market, suggesting that the perception of health risks may be a less important determinant of long-term smoking than other factors related to perceived nicotine content (eg, reinforcement, depen-dence). The lack of a significant association between perceived high/very high nicotine content and smoking cessation within 1 year could possibly be due to small cell sizes: only 6.8% of the sample perceived that their investigational cigarette contained high/very high nicotine. Likewise, perceived health risk and CPD were largely unrelated during the last week of the trial. In fact, only other cancers and heart disease were associated with CPD and the association was in the opposite direction; lower perceived risk was related to fewer CPD at week 6. Though the observational nature of the data precludes the ability to make statements regarding causality, it is possible that this association is due to smokers having knowledge that heavier smoking is worse for one’s health, resulting in greater perceived risk of developing smoking-related health conditions. Regardless, these findings are incongruent with concerns regarding the potential for reduced perceived harm of RNC cigarettes to result in greater smoking behaviour.
In the present sample, menthol status did not moderate the associations between perceived/actual nicotine content and perceived health risks. In adjusted models, however, menthol remained a statistically significant correlate of perceived health risks, such that menthol smokers perceived lower risks for developing smoking-related disease. This is consistent with prior research indicating that menthol status is associated with perceived health risks.36–40 These findings add to the mounting data suggesting that the use of menthol as a characterising flavour in cigarettes may—via reduced perceived risk smoking-related harms—contribute to the public health harms surrounding smoking.9,23–26
This study has limitations that should be acknowledged. First, smoking outcomes were assessed via selfreport following 6 weeks of exposure to RNC cigarettes and estimated cessation under a hypothetical scenario of long-term use. If possible, future work should biochemically verify actual cessation outcomes following longer exposure to RNC products. The Perceived Health Risks scale did not include health problems that are clearly unrelated to cigarette smoking (ie, chicken pox, measles) to serve as a manipulation check. Additionally, it is possible that the wording of the Perceived Health Risks scale is somewhat ambiguous. We are unable to know whether participants interpreted their risk for developing various health conditions ‘based on smoking (their) assigned study cigarette’ based on the impact of 6 weeks of smoking these products, or whether they imagined their risk if they continued to smoke the assigned study cigarettes. Moreover, participants’ rationale used when formulating health risk perceptions of experimental cigarettes is not clear: though nicotine itself does not have strong carcinogenic properties, insofar as higher nicotine yields promote greater nicotine dependence and smoking behaviour, higher nicotine content may indirectly increase the risk of smoking-related health conditions. Related to this, the degree to which nicotine contributes directly to morbidity may vary across diseases, although non-nicotine factors likely contribute to all diseases considered in this work. Future work should attempt to clarify these points. The study also used only absolute and specific measures of risk perceptions; future work should consider incorporating relative (eg, risks relative to participants’ usual brand) and general measures of risk perception. Full psychometric properties for the Perceived Health Risks scale and question regarding selfpredicted cessation are not available.
Additionally, the parent study did not assess participants’ perceived nicotine content of their usual brand cigarettes, which would allow for comparisons with the perceived nicotine content of their assigned investigational cigarettes. The present work also did not assess baseline beliefs about nicotine; doing so would allow us to assess whether these beliefs moderate the associations between perceived nicotine content with perceived health risks and smoking outcomes. Additionally, perceived nicotine content was not experimentally manipulated, which would, in a more direct way, inform how public health messaging campaigns might impact the use and effects of nicotine reduction. Future research should also assess how smoking-related harm percetions change over time (eg, whether harm perceptions stabilise over time and if they become more or less accurate following greater experience with RNC cigarettes). The aforementioned limitations notwithstanding, this study has significant strengths. For instance, we assessed perceived risks of RNC cigarettes following extended exposure to these products. Moreover, to our knowledge, this is the first study to assess whether, under double-blind conditions, the perceived nicotine content of RNC cigarettes is associated with perceived health risks and smoking related outcomes.
Addressing misperceptions regarding the role of nicotine in smoking is a complex issue, but is an important one in the context of tobacco policy and regulation. Inaccurate beliefs are also relevant for promotion and uptake of products like NRT and e-cigarettes, as well as the possibility of a nationwide nicotine reduction policy being enacted in the USA or elsewhere. Findings from our study support the hypothesis that perceived reduction in nicotine content could reduce concerns about health risks of smoking, although this may not offset the benefit on smoking behaviour. However, it remains an open question whether informing smokers about the relative harms of nicotineand smoking modifies the effects of nicotine reduction on smoking behaviour. Empirically validated public messaging clarifying the relative harm of reduced nicotine content products would likely be an important component of any low nicotine product standard.
What this paper adds.
► Many smokers believe nicotine to be the disease-causing agent responsible for smoking-related morbidity, which may lead smokers to underestimate the risks of cigarettes and reduce cessation should a nationwide nicotine reduction policy be implemented.
► This paper provides the first analysis of whether nicotine content, both perceived and actual, is associated with perceived health risks and behavioural outcomes among smokers who have undergone extended exposure to investigational cigarettes that vary in nicotine content.
► Low perceived nicotine content—but not actual nicotine content—was associated with reduced perceived health risks, but also increased predicted cessation.
► Findings inform the need for carefully crafted warning labels on nicotine and tobacco products and/or educational or mass media campaigns that clarify the relative harm of reduced nicotine content products.
Acknowledgments
Funding Research reported in this publication was supported by the National Institute on Drug Abuse and FDA Center for Tobacco Products (U54 DA031659). Salary support for LRP during the preparation of this paper was provided by T32 AI007329. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Footnotes
Competing interests None declared
Patient consent N/A.
Ethics approval The study was approved by the institutional review board at each study site and was reviewed by the FDA Center for Tobacco Products. It was monitored by an independent data and safety monitoring board.
Provenance and peer review Not commissioned; externally peer reviewed.
References
- 1.Congress, U.S. Family smoking prevention and tobacco control federal reform act, in Pub. L No. 111$31, 2009.
- 2.Benowitz NL, Henningfield JE. Establishing a nicotine threshold for addiction. The implications for tobacco regulation. N Engl J Med 1994;331:123–5. [DOI] [PubMed] [Google Scholar]
- 3.Hatsukami DK, Kotlyar M, Hertsgaard LA, et al. Reduced nicotine content cigarettes: effects on toxicant exposure, dependence and cessation. Addiction 2010;105:343–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benowitz NL, Hall SM, Stewart S, et al. Nicotine and carcinogen exposure with smoking of progressively reduced nicotine content cigarette. Cancer Epidemiol Biomarkers Prev 2007;16:2479–85. [DOI] [PubMed] [Google Scholar]
- 5.Donny EC, Denlinger RL, Tidey JW, et al. Randomized Trial of Reduced-Nicotine Standards for Cigarettes. N Engl J Med 2015;373:1340–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mercincavage M, Souprountchouk V, Tang KZ, et al. A Randomized Controlled Trial of Progressively Reduced Nicotine Content Cigarettes on Smoking Behaviors, Biomarkers of Exposure, and Subjective Ratings. Cancer Epidemiol Biomarkers Prev 2016;25:1125–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bobak A, Shiffman S, Gitchell JG, et al. Perceived Safety of Nicotine and the Use of Nicotine Replacement Products Among Current Smokers in Great Britain: Results From Two National Surveys. The Journal of Smoking Cessation? 2010;5:115–22. [Google Scholar]
- 8.Bansal-Travers M, Cummings KM, Hyland A, et al. Educating smokers about their cigarettes and nicotine medications. Health Educ Res 2010;25:678–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giovino G, Sidney S, Gfroerer J, et al. Epidemiology of menthol cigarette use. Nicotine & Tobacco Research 2004;6:67–81. [DOI] [PubMed] [Google Scholar]
- 10.Mooney ME, Leventhal AM, Hatsukami DK. Attitudes and knowledge about nicotine and nicotine replacement therapy. Nicotine Tob Res 2006;8:435–46. [DOI] [PubMed] [Google Scholar]
- 11.Pacek LR, Rass O, Johnson MW. Knowledge about nicotine among HIV-positive smokers: Implications for tobacco regulatory science policy. Addict Behav 2017;65:81–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andersen A, Chisolm MS, Kleykamp BA, et al. Reduced Nicotine Content Cigarette Knowledge, Attitudes, and Practices of Patients at a Perinatal Substance Abuse Treatment Center. Addict Disord Their Treat 2013;12:111–7. [Google Scholar]
- 13.Shadel WG, Lerman C, Cappella J, et al. Evaluating smokers’ reactions to advertising for new lower nicotine quest cigarettes. Psychol Addict Behav 2006;20:80–4. [DOI] [PubMed] [Google Scholar]
- 14.Hatsukami DK, Heishman SJ, Vogel RI, et al. Dose-response effects of spectrum research cigarettes. Nicotine Tob Res 2013;15:1113–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Denlinger-Apte RL, et al. Low nicotine content descriptors reduce perceived health risks and positive cigarette ratings in participants using very low nicotine content cigarettes. Nicotine & Tobacco Research 2017. [DOI] [PMC free article] [PubMed]
- 16.Benowitz NL, Dains KM, Hall SM, et al. Smoking behavior and exposure to tobacco toxicants during 6 months of smoking progressively reduced nicotine content cigarettes. Cancer Epidemiol Biomarkers Prev 2012;21:761–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donny EC, Houtsmuller E, Stitzer ML. Smoking in the absence of nicotine: behavioral, subjective and physiological effects over 11 days. Addiction 2007;102:324–34. [DOI] [PubMed] [Google Scholar]
- 18.Donny EC, Hatsukami DK, Benowitz NL, et al. Reduced nicotine product standards for combustible tobacco: building an empirical basis for effective regulation. Prev Med 2014;68:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shiffman S, Pillitteri JL, Burton SL, et al. Smoker and ex-smoker reactions to cigarettes claiming reduced risk. Tob Control 2004;13:78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mercincavage M, Saddleson ML, Gup E, et al. Reduced nicotine content cigarette advertising: How false beliefs and subjective ratings affect smoking behavior. Drug Alcohol Depend In Press 2017;173:99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Committee TPSA. Menthol cigarettes and public health: review of the scientific evidence and recommendations, FDA, Editor, 2011. [Google Scholar]
- 22.Kreslake JM, Wayne GF, Connolly GN. The menthol smoker: tobacco industry research on consumer sensory perception of menthol cigarettes and its role in smoking behavior. Nicotine Tob Res 2008;10:705–15. [DOI] [PubMed] [Google Scholar]
- 23.Hammond D, Parkinson C. The impact of cigarette package design on perceptions of risk. J Public Health 2009;31:345–53. [DOI] [PubMed] [Google Scholar]
- 24.Paek HJ, Reid LN, Choi H, et al. Promoting health (implicitly)? A longitudinal content analysis of implicit health information in cigarette advertising, 1954–2003. J Health Commun 2010;15:769–87. [DOI] [PubMed] [Google Scholar]
- 25.Pollay RW, Dewhirst T. A Premiere example of the illusion of harm reduction cigarettes in the 1990s. Tob Control 2003;12:322–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wakefield M, Morley C, Horan JK, et al. The cigarette pack as image: new evidence from tobacco industry documents. Tob Control 2002;11(Suppl 1):i73–i80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hatsukami DK, Vogel RI, Severson HH, et al. Perceived Health Risks of Snus and Medicinal Nicotine Products. Nicotine Tob Res 2016;18:794–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.StataCorp. Stata Statistical Software: College Station, TX, 2015. [Google Scholar]
- 29.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q 1984;11:1–47. [DOI] [PubMed] [Google Scholar]
- 30.Cohen JB. Smokers’ knowledge and understanding of advertised tar numbers: health policy implications. Am J Public Health 1996;86:18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Etter JF, Kozlowski LT, Perneger TV. What smokers believe about light and ultralight cigarettes. Prev Med 2003;36:92–8. [DOI] [PubMed] [Google Scholar]
- 32.Kozlowski LT, Goldberg ME, Yost BA, et al. Smokers’ misperceptions of light and ultra-light cigarettes may keep them smoking. Am J Prev Med 1998;15:9–16. [DOI] [PubMed] [Google Scholar]
- 33.Kozlowski LT, Pillitteri JL. Beliefs about “Light” and “Ultra Light” cigarettes and efforts to change those beliefs: an overview of early efforts and published research. Tob Control 2001;10 (Suppl 1):i12–i16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shiffman S, et al. Effect of health messages about ‘light’ and ‘ultra light’ cigaretteson beliefs and quitting intent. Tob Control 2001;10(Suppl 1):i24–i32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shiffman S, et al. Smokers’ beliefs about ‘light’ and ‘ultra light’ cigarettes. Tob Control 2001;10(Suppl 1):i17–i23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Richter P, et al. Small-group discussions on menthol cigarettes: listening to adult african american smokers in Atlanta, georgia. Ethn Health 2008;13:171–82. [DOI] [PubMed] [Google Scholar]
- 37.Richter PA, Pederson LL, O’Hegarty MM. Young adult smoker risk perceptions of traditional cigarettes and nontraditional tobacco products. Am J Health Behav 2006;30:302–12. [DOI] [PubMed] [Google Scholar]
- 38.Wilson N, Weerasekera D, Peace J, et al. Smokers have varying misperceptions about the harmfulness of menthol cigarettes: national survey data. Aust N Z J Public Health 2011;35:364–7. [DOI] [PubMed] [Google Scholar]
- 39.Hymnowitz N, Mouton C, Edkholdt H. Menthol cigarette smoking in african Americans and Whites Tob Control, 1995:4, 194–5. p.. [Google Scholar]
- 40.Unger JB, Allen B, Leonard E, et al. Menthol and non-menthol cigarette use among Black smokers in Southern California. Nicotine Tob Res 2010;12:398–407. [DOI] [PubMed] [Google Scholar]


