Abstract
Introduction:
Proximal humerus fractures (PHFs) are a common fragility fracture and have been shown to increase mortality in elderly patients. In the last decade, reverse total shoulder arthroplasty (RTSA) was introduced as a reliable operative treatment option for this indication. In other fragility fractures, most notably hip fractures, urgent surgical treatment can reduce mortality. The purpose of this study is to evaluate whether treatment with RTSA can reduce 1-year mortality in elderly patients with complex displaced PHFs.
Materials and Methods:
A retrospective study was performed to compare 1-year mortality between 2 groups of elderly patients (>75 years old) who presented to a level 1 trauma center emergency department with complex displaced PHFs. The conservative treatment group (n = 83; mean age, 83.7 years) presented from 2008 to 2010 when RTSA was not yet available, and treatment was nonoperative. The surgical treatment group (n = 62; mean age, 82.2 years) presented from 2012 to 2015 and underwent RTSA.
Results:
One-year mortality was 8.1% (male 7.1%; female 8.3%) in the surgical treatment group and 10.8% (male 18.8%; female 9.0%) in the conservative treatment group. The reduction in mortality in the surgical treatment group was not significant (entire cohort P = .56; males P = .35; females P = .59).
Discussion:
Recent studies failed to show better functional results after surgical treatment with RTSA when compared to conservative treatment. This study suggests that a benefit of surgical treatment with RTSA that was not examined until now might exist—a reduction in the increased mortality risk associated with PHFs.
Conclusions:
There was no significant difference in 1-year mortality between the groups, although there was a trend showing lower mortality with RTSA, mostly in men. Further studies with larger populations and longer follow-up times are needed to determine whether this trend is of clinical significance.
Keywords: reverse total shoulder arthroplasty, proximal humerus fracture, elderly patients, 1-year mortality, conservative treatment, fragility fractures
Introduction
Proximal humerus fractures (PHFs) are a common fragility fracture in elderly patients. They account for 6% of all fractures in adult patients1 and are the third most common fractures in elderly patients after those of the hip and distal radius. Proximal humerus fractures are 3 to 4 times more common in elderly women than men.2,3 The incidence increases with age, with more than 70% occurring in patients over 60 years of age and the highest incidence occurring among patient ages 73 to 78.4 Proximal humerus fractures are associated with substantial burden of disability and impaired quality of life.
Proximal humerus fractures have been found to increase 1-year mortality in elderly patients.5-8 One-year mortality after PHFs, treated conservatively or surgically, was found to be between 5% and 22%.5,9-11 An increase in 1-year mortality was also observed in other fragility fractures, and in hip fractures, 1-year mortality is as high as 40%.5,12,13 In the case of hip fractures, the current paradigm is that urgent surgical treatment reduces mortality by allowing early mobilization, though this was not demonstrated in randomized clinical trials.14
Treatment of PHFs depends on fracture type, fracture stability, and the degree of fragment displacement. Approximately 80% of PHFs are nondisplaced or minimally displaced,3 and nonoperative treatment is successful.15 The optimum treatment becomes less clear in more complex displaced fracture patterns.16,17 Up until recently, the operative treatment of choice for complex displaced fractures had been primary hemiarthroplasty. However, in elderly patients, fractures are characterized by osteopenic bone, thereby causing hemiarthroplasty to be less successful and correlate with poor functional outcomes.18 In addition, when comparing the operative (hemiarthroplasty/open reduction & internal fixation [ORIF]) and nonoperative treatment of displaced PHFs, there was no difference in the pooled estimate of mortality rate.17,19
In recent years, reverse total shoulder arthroplasty (RTSA) has gained popularity as a viable treatment option for complex displaced fractures in elderly patients.20,21 This procedure, which was originally used for treating patients with cuff tear arthropathy, was found to achieve more reliable functional results.22 The objective of this study is to evaluate whether RTSA reduces 1-year mortality in elderly patients with complex displaced PHFs versus conservative treatment.
Materials and Methods
After institutional review board approval, a retrospective study examining a cohort of patients over 75 years of age who underwent RTSA of PHFs between 2012 and 2015 in one level 1 trauma center was reviewed. In our medical center, surgical treatment with RTSA is offered to active, cognitively intact elderly patients, who would be able to adhere to the postoperative rehabilitation process. Exclusion criteria from the study were: (1) concomitant lower limb fracture and (2) patient was medically unstable prior to surgery (American Society of Anaesthesiologists [ASA] score >3).
The control group consisted of patients over 75 years of age who presented to the medical center’s emergency department with displaced PHFs (Neer 4, Neer 3, and Neer 2 with complete displacement of the humeral head) between 2008 and 2010, a time when RTSA was not yet available as a treatment option in our medical center. Most patients were treated conservatively by immobilization for 6 weeks followed by physiotherapy, and some were treated surgically by hemiarthroplasty/ORIF. In order to include only the patient who would have been treated with RTSA by current practices, we excluded patients with (1) unstable medical condition at presentation; (2) inactive, dependent, and/or cognitively impaired patients; and (3) patients with insufficient data to determine their medical status retrospectively. Other exclusion criteria from the study were patient who had received surgical treatment or patient with concomitant lower limb fracture.
One-month and 1-year mortality following either surgery or fracture (in the control group) was determined using the Israeli Ministry of the Interior database.
Statistical Analysis
Statistical analysis was performed using IBM SPSS 21 Statistics Data Editor. Categorical variables were compared using the Fisher exact test or the χ2 test. Quantitative variables were summarized by mean and standard error of the mean. Parametric variable means were compared using the Student t test, and in the case of nonparametric variables, the groups were compared using the Mann-Whitney test.
Kaplan-Meier curves were constructed to estimate the distribution of 1-year survival, and comparison between the groups was assessed by log-rank test. For all tests, a P value of <.05 was considered statistically significant.
Results
A total of 66 patients met the inclusion criteria for the surgical treatment group, of which 4 were excluded (2 had concomitant tibial fracture, 1 was classified as ASA 4 at the time of surgery, and 1 was a tourist lost to follow-up), leaving 62 patients. A total of 182 patients met the inclusion criteria for the conservative treatment group, of which 99 were excluded (44 lacked medical data; 34 inactive, dependent, and/or cognitively impaired; 13 had surgical treatment using other techniques: external fixation, ORIF, or hemiarthroplasty; and 8 had concomitant lower limb fracture), leaving 83 patients.
The patients’ demographics and medical background are summarized in Table 1. Differences between the 2 groups were minor; therefore, we did not use propensity score matching for the statistical analysis.
Table 1.
Demographic Characteristics and Medical Background of Patients With PHFs.
| Conservative Treatment (n = 83) | Surgical Treatment (RTSA; n = 62) | P Value | |
|---|---|---|---|
| Female | 67 (80.7%) | 48 (77.4%) | .63 |
| Age | 83.7 (5.3) [M-84.2, F-83.6] | 82.2 (5.1) [M-82.8, F-82.0] | .07 |
| Any comorbidity | 78 (94%) | 59 (95.2%) | .53 |
| Hypertension | 61 (73.5%) | 46 (74.2%) | .54 |
| Diabetes | 24 (28.9%) | 19 (30.6%) | .48 |
| Hyperlipidemia | 26 (31.3%) | 22 (35.5%) | .36 |
| CHF | 7 (8.4%) | 2 (3.2%) | .18 |
| IHD | 18 (21.7%) | 14 (22.6%) | .53 |
| Valvular disease | 5 (6%) | 5 (8.1%) | .44 |
| Arrhythmia | 17 (20.5%) | 6 (9.7%) | .06 |
| History of CVA | 7 (8.4%) | 3 (4.8%) | .31 |
| History of malignancy | 16 (19.3%) | 12 (19.4%) | .58 |
| COPD/asthma | 16 (19.3%) | 5 (8.1%) | <.05 |
| CCI | |||
| 3-4 | 33 (39.8%) | 24 (38.7%) | |
| 5-6 | 31 (37.3%) | 28 (45.2%) | |
| 7-8 | 18 (21.7%) | 9 (14.5%) | |
| 9-10 | 1 (1.2%) | 1 (1.6%) | |
| Average | 5.25 | 5.05 | .4 |
Abbreviations: CCI, Charlson comorbidity index; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; CVA, cerebrovascular accident; F, female; IHD, ischemic heart disease; M, male; RTSA, reverse total shoulder replacement.
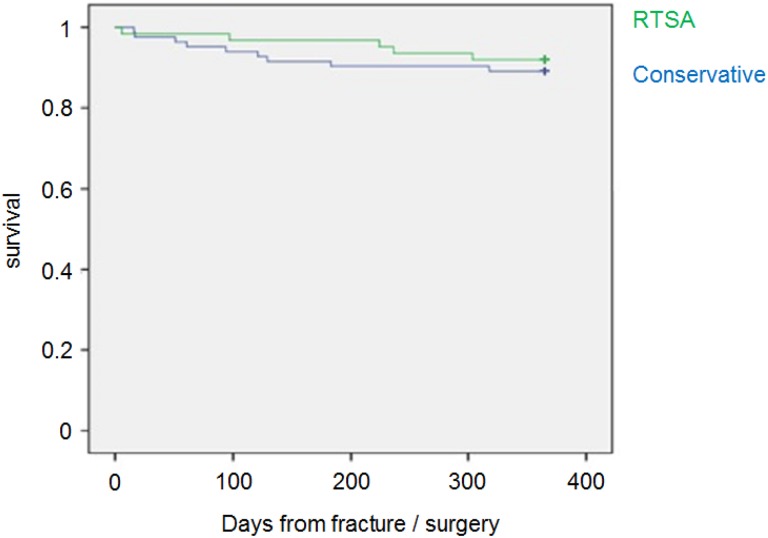
One-month mortality was 1 (1.6%) in the surgical treatment group versus 2 (2.4%) in the conservative treatment group (P = .61). One-year mortality for the entire cohort (N = 145) was 14 (9.7%). In the surgical treatment group, 5 (8.1%) patients died in 1 year, of whom 1 (7.1%) was male and 4 (8.3%) were female. In the conservative treatment group, 9 (10.8%) patients died in 1 year, of whom 3 (18.8%) were male and 6 (9.0%) were female. This favorable trend for surgical treatment was not significant: P = .56 for the entire cohort, P = .35 for males only, and P = .59 for females only (Figure 1).
Figure 1.
One-year survival rates for the 2 groups. The surgical treatment group had a higher survival rate, although these findings were not statistically significant.
Discussion
The aim of the current study was to assess whether surgical treatment of complex displaced PHFs in elderly patients with RTSA can reduce 1-year mortality, compared with conservative treatment. According to our results, 1-year mortality was 10.8% in the conservative treatment group versus 8.1% in the RTSA group, but the difference was not significant (P = .56).
The recommended treatment for complex displaced PHFs in elderly patients is in constant debate. Recent studies failed to show better functional results after surgical treatment (ORIF/hemiarthroplasty,19 RTSA23) when compared to conservative treatment and thus concluded that there is no benefit in surgical treatment for this indication. Our study suggests that a benefit of surgical treatment that was not examined until now might exist—a reduction in the increased mortality risk associated with PHFs.
The causes of increased mortality after PHFs are not well studied, but it seems that the fracture is more an indicator of frailty than the cause for increased mortality. This is suggested by comparing mortality after PHFs to that after hip fracture. Whereas mortality related to hip fracture is highest in the first year after the fracture and then levels off,24 relative mortality after upper extremity fracture increases linearly for several years after the fracture. Since this process continues well beyond the fracture healing and rehabilitation stages, this probably represents this populations’ vulnerability,6 and more support comes from examining the risk factors for mortality after PHFs, which are mostly associated with reduced social independence prior to the fracture.9
If, in fact, the morbidity associated with PHFs is not the main cause for the clear increase in mortality, one must wonder why surgical treatment would reduce mortality. One possible explanation is that the hospitalization and rehabilitation process that comes with surgical treatment can have a beneficial effect on many other aspects of the patient’s life not assessed by our study. A second explanation is that when the elderly patient with PHFs suffers from osteoporosis, conservative treatment with upper limb immobilization predisposes him to future fractures and reduced self-efficacy by exacerbating preexisting sarcopenia, muscle weakness, and osteoarthritis. Prompt, definitive surgical care aimed at early restoration of function might reduce these risks.
Male gender was found to be a risk factor for mortality after fragility fractures, possibly because osteoporotic bone is a more likely marker of poor underlying health in men than in women in whom fragility fractures are more common.25 A recent study found the risk of death related to PHFs in elderly men was even higher than previously reported for hip fracture.6 This phenomena was observed in our study in the conservative treatment group (1-year mortality 9% for female vs 18.8% for male), but not in the surgical treatment group (8.3% for female vs 7.1% for male). It is possible that this subgroup of older men has a much more significant reduction in mortality with surgical treatment, but this would have to be examined in future studies with larger populations.
Overall, 1-year mortality for the entire cohort (both RTSA and conservative treatment groups) was 9.7%. This seems to be in line with the current literature. In a large population-based study in Canada, 1-year mortality after PHFs in elderly patients was found to range from 10.2% to 22.6% in men and from 5.3% to 10.2% in women.5 In a nationwide Korean study, 1-year mortality after PHFs was lower at 7% (8.5% for men and 6.4% for women), but this study included a younger population (age over 50 years).10
No significant differences were found in 1-month mortality rates, with low rates for both groups (1.6% for RTSA and 2.4% for conservative treatment). This demonstrates that with proper patient selection, RTSA is a safe procedure even in the super-elderly population.
Strengths and Weaknesses
The main strength of this study is the control group (conservative treatment). Although the treatment was not randomized, we feel that the control group accurately represents the patients who would have been treated with RTSA by current practices.
Study weaknesses include the retrospective nature, small study population, short follow-up period, potential selection bias in the control group, and the temporal differences between the groups: (1) power analysis found that a 4% reduction in mortality, from 10% to 6%, would require a cohort of 125 patients (62 in each group) to be significant. We found a lower reduction (2.7%), thus not reaching significance. This limit is especially evident in the men group, where a large reduction in mortality was noted but with a very small study population, limiting the reliability of this observation. (2) One year might be too short of a follow-up period, as mortality rates after PHFs are elevated for over 5 years.10 (3) The large number of patients who were excluded from the control group due to lack of data could cause selection bias.4 (4) The patients in the control group had higher rates of congestive heart failure, cerebrovascular accident, and arrhythmia, which did not reach statistical significance, and significantly more chronic obstructive pulmonary disease/asthma. It is worth noting that arrhythmia (mostly atrial fibrillation) is not a major risk factor for 1-year mortality, but the higher comorbidity rates in the control group could lead to a bias.5 (5) The temporal difference between the groups (the fractures in the RTSA group occurring 5 years on average after those of the conservative treatment group) could lead to a bias as medical care is changing and constantly improving.
Conclusion
To our knowledge, no previous study compared mortality rates associated with RTSA for the treatment of complex displaced PHFs in elderly patients to that of conservative treatment. Although no significant reduction in 1-year mortality was found, there was a trend showing decreased 1-year mortality with RTSA, mostly in men. Further studies with larger populations and longer follow-up times are needed to determine whether this trend is of clinical significance.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Dani Rotman, MD  http://orcid.org/0000-0003-4013-0152
http://orcid.org/0000-0003-4013-0152
References
- 1. Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. [DOI] [PubMed] [Google Scholar]
- 2. Chu SP, Kelsey JL, Keegan TH, et al. Risk factors for proximal humerus fracture. Am J Epidemiol. 2004;160(4):360–367. [DOI] [PubMed] [Google Scholar]
- 3. Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72(4):365–371. [DOI] [PubMed] [Google Scholar]
- 4. Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87–92. [DOI] [PubMed] [Google Scholar]
- 5. Morin S, Lix LM, Azimaee M, Metge C, Caetano P, Leslie WD. Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos Int. 2011;22(9):2439–2448. [DOI] [PubMed] [Google Scholar]
- 6. Olsson C, Petersson C, Nordquist A. Increased mortality after fracture of the surgical neck of the humerus: a case-control study of 253 patients with a 12-year follow-up. Acta Orthop Scand. 2003;74(6):714–717. [DOI] [PubMed] [Google Scholar]
- 7. Piirtola M, Vahlberg T, Lopponen M, Räihä I, Isoaho R, Kivelä SL. Fractures as predictors of excess mortality in the aged-a population-based study with a 12-year follow-up. Eur J Epidemiol. 2008;23(11):747–755. [DOI] [PubMed] [Google Scholar]
- 8. Somersalo A, Paloneva J, Kautiainen H, Lönnroos E, Heinänen M, Kiviranta I. Increased mortality after upper extremity fracture requiring inpatient care. Acta Orthop. 2015;86(5):533–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Clement ND, Duckworth AD, McQueen MM, Court-Brown CM. The outcome of proximal humeral fractures in the elderly: predictors of mortality and function. Bone Joint J. 2014;96-B(7):970–977. [DOI] [PubMed] [Google Scholar]
- 10. Park C, Jang S, Lee A, et al. Incidence and mortality after proximal humerus fractures over 50 years of age in South Korea: national claim data from 2008 to 2012. J Bone Metab. 2015;22(1):17–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yian E, Zhou H, Schreiber A, et al. Early hospital readmission and mortality risk after surgical treatment of proximal humerus fractures in a community-based health care organization. Perm J. 2016;20(1):47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Johnell O, Kanis JA, Oden A, et al. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15(1):38–42. [DOI] [PubMed] [Google Scholar]
- 14. Parker MJ, Handoll HH, Bhargara A. Conservative versus operative treatment for hip fractures. Cochrane Database Syst Rev. 2000;(4):CD000337. [DOI] [PubMed] [Google Scholar]
- 15. Gaebler C, McQueen MM, Court-Brown CM. Minimally displaced proximal humeral fractures: epidemiology and outcome in 507 cases. Acta Orthop Scand. 2003;74(5):580–585. [DOI] [PubMed] [Google Scholar]
- 16. Gomberawalla MM, Miller BS, Coale RM, Bedi A, Gagnier JJ. Meta-analysis of joint preservation versus arthroplasty for the treatment of displaced 3- and 4-part fractures of the proximal humerus. Injury. 2013;44(11):1532–1539. [DOI] [PubMed] [Google Scholar]
- 17. Rabi S, Evaniew N, Sprague SA, Bhandari M, Slobogean GP. Operative vs non-operative management of displaced proximal humeral fractures in the elderly: a systematic review and meta-analysis of randomized controlled trials. World J Orthop. 2015;6(10):838–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ferrel JR, Trinh TQ, Fischer RA. Reverse total shoulder arthroplasty versus hemiarthroplasty for proximal humeral fractures: a systematic review. J Orthop Trauma. 2015;29(1):60–68. [DOI] [PubMed] [Google Scholar]
- 19. Rangan A, Handoll H, Brealey S, et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. JAMA. 2015;313(10):1037–1047. [DOI] [PubMed] [Google Scholar]
- 20. Schairer WW, Nwachukwu BU, Lyman S, Craig EV, Gulotta LV. Reverse shoulder arthroplasty versus hemiarthroplasty for treatment of proximal humerus fractures. J Shoulder Elbow Surg. 2015;24(10):1560–1566. [DOI] [PubMed] [Google Scholar]
- 21. Schairer WW, Nwachukwu BU, Lyman S, Gulotta LV. Arthroplasty treatment of proximal humerus fractures: 14-year trends in the United States. Phys Sportsmed. 2017;45(2):92–96. [DOI] [PubMed] [Google Scholar]
- 22. Sirveaux F, Roche O, Mole D. Shoulder arthroplasty for acute proximal humerus fracture. Orthop Traumatol Surg Res. 2010;96(6):683–694. [DOI] [PubMed] [Google Scholar]
- 23. Roberson TA, Granade CM, Hunt Q, et al. Nonoperative management versus reverse shoulder arthroplasty for treatment of 3- and 4-part proximal humeral fractures in older adults. J Shoulder Elbow Surg. 2017;26(6):1017–1022. [DOI] [PubMed] [Google Scholar]
- 24. O’Neill TW, Roy DK. How many people develop fractures with what outcome? Best Pract Res Clin Rheumatol. 2005;19(6):879–895. [DOI] [PubMed] [Google Scholar]
- 25. Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353(9156):878–882. [DOI] [PubMed] [Google Scholar]