Abstract
Background:
Femoroacetabular impingement (FAI) represents complex alterations in the bony morphology of the proximal femur and acetabulum. Imaging studies have become crucial in diagnosis and treatment planning for symptomatic FAI but also have limited patient understanding and satisfaction. Exploration of alternative patient counseling modalities holds promise for improved patient understanding, satisfaction, and ultimately for outcomes.
Purpose:
To compare perceived understanding of functional anatomy and FAI pathomorphology among patients counseled with routine computed tomography (CT), generic hip models, and a 3-dimensional (3D) model printed in accordance with a patient’s specific anatomy.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
A prospective randomized analysis of patients presenting with radiographically confirmed FAI was conducted between November 2015 and April 2017. Patients were randomized into groups that received preoperative counseling with CT imaging alone, a generic human hip model, or a haptic 3D model of their hip. All groups were subjected to a novel questionnaire examining patient satisfaction and understanding on a variety of topics related to FAI. Data were compared with bivariate and multivariate analyses. Statistical significance was determined as P < .05.
Results:
Thirty-one patients were included in this study (25 men, 6 women). Ten patients were randomized to the CT-only group, 11 to the generic hip model group, and 10 to receive custom 3D-printed models of their hips. Patients preoperatively counseled with isolated CT imaging or a generic hip model reported greater understanding of their pathophysiology and the role of surgical intervention when compared with those counseled with haptic 3D models (P = .03). At final follow-up, patients counseled with the use of isolated CT imaging or haptic 3D models reported greater increases and retention of understanding as compared with those counseled with generic hip models alone (P = .03).
Conclusion:
Preoperative counseling with haptic 3D hip models does not appear to favorably affect patient-reported understanding or satisfaction with regard to FAI when compared with the use of CT imaging alone. Continued research into alternative counseling means may serve to further improve patient understanding and satisfaction on this complex anatomic phenomenon.
Keywords: arthroscopic hip surgery, femoroacetabular impingement, haptic 3-dimensional models, patient counseling
Femoroacetabular impingement (FAI) represents an alteration in the bony morphology of the proximal femur and acetabulum, which may cause symptomatic anatomic conflict during dynamic motion.5,10,16 This phenomenon was shown to be more common among young and physically active adults, resulting in early chondral injury or degenerative disease of the joint if the underlying cause of the impingement is not addressed.7,9,10,13 Over the past 10 to 15 years, hip preservation surgery has gained considerable momentum and has emerged as a potential means to alter the natural history of untreated symptomatic FAI.6,16
A variety of impingement types have been described, and they have a significant impact on the surgical management of the deformity. Cam impingement refers to damage caused by a nonspherical head rotating within the acetabulum.5,10 The resultant shear forces against the acetabular articular cartilage result in partial-thickness damage or chondral delamination. Pincer impingement results from direct contact between a prominent acetabular rim and the femoral head-neck junction and can contribute to labral and articular injury.10 Additionally, many gradations and combinations of these FAI mechanisms have been described in the literature. Nonetheless, understanding the specific anatomic regions of conflict requires a thorough awareness of complex functional anatomy, joint kinematics, and the spatial and geometric constraints that dictate joint motion.
While patients with FAI can have a specific constellation of physical examination findings, imaging plays a particularly important role in diagnosis and treatment planning given the complexity of the hip joint.12 Plain radiography is typically the first step in the assessment of hip pathology, as it allows for assessment of joint morphology, bony changes, and joint space preservation while minimizing patient harm. For patients with FAI, plain films may reveal acetabular overcoverage, abnormal sphericity of the femoral head, herniation pits, and other subtle signs of impingement.8,15,17 Despite its utility, plain radiography represents a 2-dimensional image of a 3-dimensional (3D) anatomic lesion and thus has limitations for interpreting and understanding a patient’s FAI.
Computed tomography (CT) has been shown to be far superior at showing bony architecture and structure and has been beneficial in analyzing and quantifying lesions implicated in FAI. CT with 3D reconstructions can provide the clearest image of cam lesions and their morphology, playing important roles in surgical planning.1,5,12 Data generated from these advanced scans can also be utilized in combination with technological advances in the realm of 3D printing, enabling the creation of patient-specific models. These models were shown in other areas of medicine to be well liked by patients and considered to be more meaningful.3,4
It remains unclear whether current imaging strategies employed by orthopaedic surgeons in analyzing FAI are sufficient to impart a substantial degree of understanding to patients undergoing future surgery. As surgeons and physicians strive to improve quality-of-care metrics, optimize clinical outcomes, and enhance patient satisfaction, it is essential to determine the most efficacious vehicle for delivering complex information to patients to allow them to make informed decisions regarding their care. In the past few years, 3D printing has been shown to have a variety of medical applications in medical decision making, patient education, and operative planning. Recent studies have also indicated that 3D prints can have positive influences on patient understanding, satisfaction, and compliance.14
The purpose of this study was to compare patients’ perceived understanding of the functional anatomy and pathomorphology of their FAI. Patients were counseled with either routine CT imaging, a generic hip model, or a patient-specific 3D model printed in accordance with their anatomy, and perceived understanding was measured by a novel patient-reported questionnaire. We hypothesized that patients counseled with the assistance of a personalized 3D hip model would report higher satisfaction and greater understanding of the functional anatomy and pathomorphology of their FAI.
Methods
After approval by our institution’s research subjects review board, patients presenting for evaluation of radiographically confirmed FAI were prospectively enrolled into this single institution–based study conducted between November 20, 2015, and April 14, 2017. The primary outcome for this study was improvement in patient-rated understanding of one’s hip pathology as rated by a specialized questionnaire.
Inclusion criteria for this study were patients between the ages of 18 and 65 years with radiographically confirmed FAI who were potential surgical candidates presenting for preoperative evaluation at our institution. Patients were required to be English speaking and competent to understand their pathomorphology. Patients presenting for evaluation with incomplete radiographic imaging, those outside the established age ranges, and non-English-speaking patients were excluded. Additionally, patients being treated for hip pathology other than FAI (hip dysplasia, Perthes disease, avascular necrosis, etc) were excluded from this study.
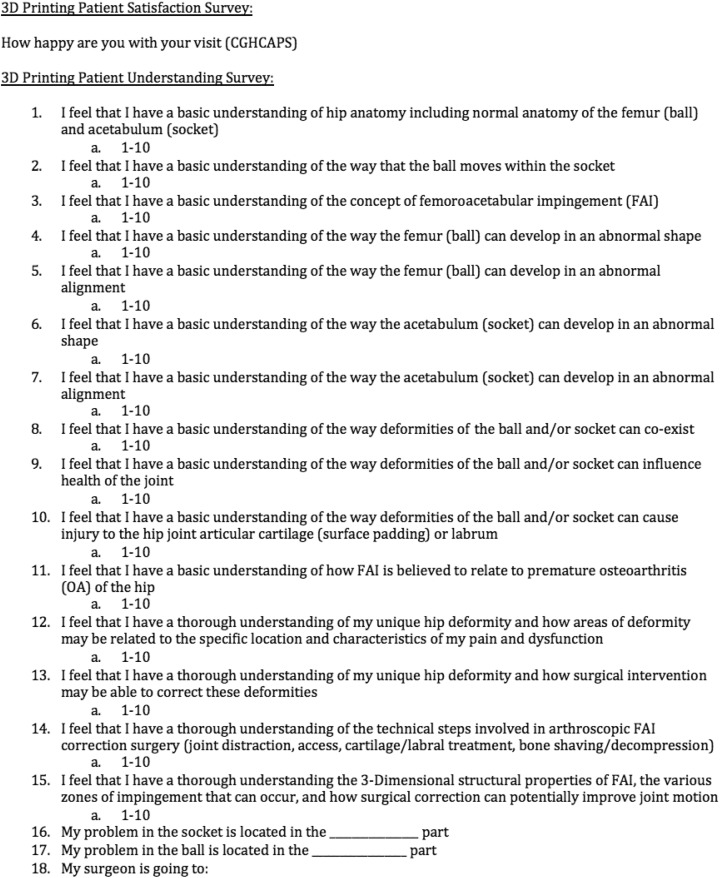
At the time of their first appointment, all patients underwent an extensive clinical evaluation by the primary surgeon of this study (B.G.), and their pathologic hip condition was described with the assistance of plain radiographs. At the completion of this first clinical encounter, a novel questionnaire was administered to all patients (Figure 1). This survey asked patients to rate their clinical understanding on a variety of topics, including but not limited to normal hip anatomy, the concept of FAI, the femoral and acetabular contributions to FAI, the patients’ own anatomic abnormalities, and the goals of surgical intervention. All responses were recorded and maintained in a secure manner compliant with the Health Insurance Portability and Accountability Act. Patients were also asked to report their level of preoperative pain during their initial clinical visitation in an effort to anchor the subsequent levels of satisfaction determined by the later surveys. This was based on the belief that if patients within one of the study groups had significantly different pain levels, their responses and satisfaction regarding the clinical encounters may be inherently different. Final pain scores were obtained at the 1-year postoperative time point for all patients. It is important to distinguish that this survey reports patients’ perceived understanding and is not a true measure of understanding.
Figure 1.
Novel questionnaire administered to patients within the study.
Upon completion of the first clinical encounter, all patients underwent CT imaging of their pathologic hip. Patients were then randomized to 1 of 3 groups. In group 1, patients returned to the clinic 2 weeks after their CT imaging, where the imaging was reviewed in detail with the primary surgeon. At the completion of this second clinical encounter, patients were once again asked to complete the same understanding/satisfaction surveys. In group 2, a generic 3D model of a human hip was used in conjunction with personalized CT imaging to review the patient’s pathoanatomy during his or her second preoperative visitation (Figure 2). In group 3, patients received a custom-printed 3D model of their hips (Figure 3) in additional to CT imaging to further review their pathoanatomy. These models were not gifted to the patients upon completion of the study and cost approximately $75 to produce. Two weeks after the second encounter, patients were asked to complete the same questionnaire to gauge their retention of information prior to proceeding with further treatment; this also coincided with the last preoperative clinical visit.
Figure 2.
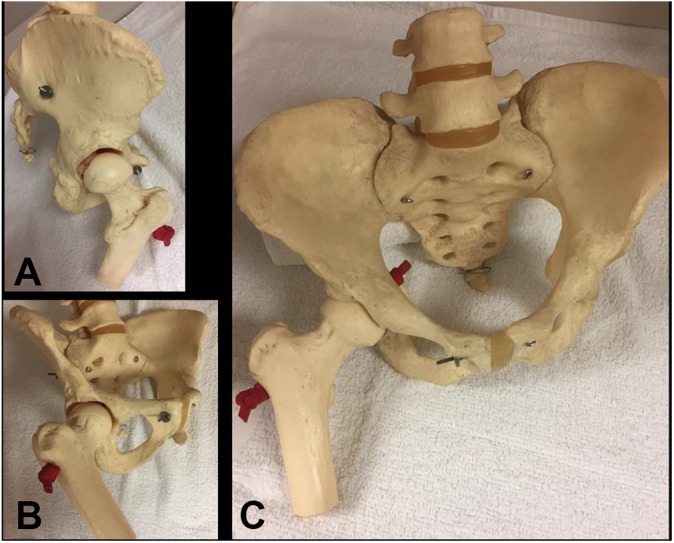
(A-C) Photographs of generic hip model used within the study.
Figure 3.
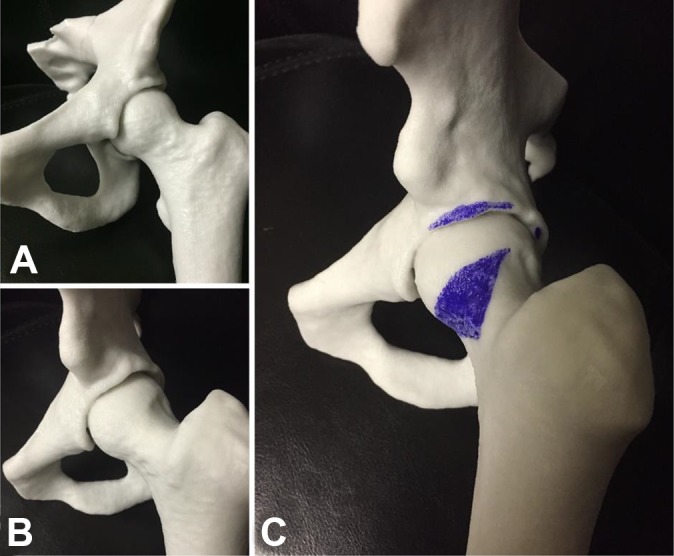
(A-C) Photographs of custom-printed 3-dimensional models used within the study. (C) How markings were used in conjunction with the models to identify areas of pathology.
Data Acquisition and Computer-Aided Design of Hip Models
CT scans of randomized patients were carried out with parameters indicated by our institution’s protocols. Digitization of the CT scans into 3D models was accomplished with the software AMIRA (v 5.5.0). First, DICOM files (voxel size: 0.424 × 0.424 × 0.625 mm) were generated after patient CT scans and imported into AMIRA. Segmentation of the region of interest was performed and translated from DICOM into STL format; this process was required because STL file formats are required for 3D printing. The virtual model of the hip was then transferred to the 3D printer–compatible software, ZPrint, in preparation for printing.
Rapid Prototyping of the Hip Models With a Binder Jetting 3D Printer
The 3D-printing process was carried out with a commercial 3D binder jetting system: a ZPrinter 450 (3DSystems). The specified layer thickness for each print was 0.0875 mm. The proximal femoral head and acetabulum were printed as 2 separate parts. Upon completion of the print, the model was dried for 90 minutes in the powder bed and then excavated. Residual powder was removed with an air gun. The cleaned model was then submerged in an infiltrating agent, Z-Color 101 (3DSystems), to postharden the finished product and was dried for an additional 30 minutes.
Statistical Analysis
A power analysis was performed in an effort to determine the appropriate sample size for this study. It was determined that a total sample size of 30 patients (10 per group) would provide 80% power to detect a 2-point difference in patient understanding on our questionnaire, with a 2-sided 0.05-level test. Data were analyzed among the groups with linear and logistic regression modeling. For categorical variables, such as sex, groups were compared via chi-square analysis. Analysis of variance and independent-sample Student t tests were used to compare the means for all continuous variables for the 3 groups. At the conclusion of the study, we performed an unblinded analysis of the constituent questions in our outcomes questionnaire. This was performed because our questionnaire was novel and its use has not yet been validated for study. The results of each question were individually compared with the overall study findings in an effort to determine which question types were most predictive of patient understanding and satisfaction.
Results
A total of 31 consecutive patients who met the inclusion criteria were prospectively enrolled into this study. Of these, 10 patients were randomized to the radiograph-only group (group 1), 11 to the generic plastic model group (group 2), and 10 to the personalized 3D model group (group 3). All patients enrolled into the study underwent surgery for their hip pathology.
Demographics
The radiograph-only group (group 1) consisted of 9 men and 1 woman, with a mean ± SD age of 26 ± 6.2 years. At the time of surgery, patients rated their pain as a mean 3.2 out of 10. Postoperatively, patients graded their pain as a 1.5 out of 10.
The generic plastic model group (group 2) consisted of 10 men and 1 woman, with a mean age of 27.2 ± 6.7 years. At the time of surgery, patients rated their pain as a mean 2.6 out of 10. Postoperatively, patients graded their pain as a 1.6 out of 10.
The personalized 3D model group (group 3) consisted of 6 men and 4 women, with a mean age of 27.9 ± 7.0 years. At the time of surgery, patients rated their pain as a mean 2.7 out of 10. Postoperatively, patients graded their pain as a 2 out of 10.
No significant demographic differences existed among groups (Table 1).
TABLE 1.
Demographic Data and Analyses of Patients Enrolled in the 3 Study Groupsa
| CT Alone | Generic Model | Haptic 3D Model | P | |
|---|---|---|---|---|
| Sex, n | ||||
| Male | 9 | 10 | 6 | |
| Female | 1 | 1 | 4 | .13307 |
| Age, mean ± SD, y | 26 ± 6.2 | 27.2 ± 6.7 | 27.9 ± 7.0 | .81 |
| Mean pain score (0-10) | ||||
| Preoperative | 3.2 | 2.6 | 2.7 | .79 |
| Postoperative | 1.5 | 1.6 | 2 | .81 |
a3D, 3-dimensional; CT, computed tomography.
Questionnaire Results
With regard to the novel satisfaction- and knowledge-based questionnaire, there were no statistically significant differences among groups with respect to the overall score at the initial clinical visit (groups 1-3, respectively: 5.9 ± 2.7 vs 6.2 ± 2.4 vs 6.2 ± 2.4; P = .40). With regard to patient satisfaction scores during the initial clinical encounter, prior to randomization into study groups, there were no statistically significant differences between groups 1 to 3 (8.5 ± 1.8 vs 9.0 ± 1.5 vs 8.7 ± 1.1; P = .74).
On initial follow-up, there were no statistically significant between-group differences in patient satisfaction (groups 1-3, respectively: 9.5 ± 1.1 vs 9.4 ± 0.7 vs 9.7 ± 0.5; P = .62), nor were there any significant changes in satisfaction from the initial encounter to follow-up (1.0 ± 1.8 vs 0.4 ± 1.4 vs 1.0 ± 0.8; P = .47). Patients who received counseling with isolated CT of their pathology or demonstration with a generic hip model reported greater increases in understanding of their pathophysiology and the role of surgical intervention when compared with patients counseled with personalized 3D printouts (groups 1-3, respectively: 2.9 ± 2.7 vs 2.4 ± 2.3 vs 2.2 ± 1.9; P = .03). There were no statistically significant differences in the reported understanding of pathology between patients counseled with CT imaging alone and those with generic hip models (2.9 ± 2.7 vs 2.4 ± 2.3; P = .06).
During the final preoperative clinical encounter, which was used as a means of measuring retention of information, patients undergoing counseling with the use of CT imaging alone or the use of a 3D-printed hip model reported greater increases from their baseline understanding scores than did patients counseled with the use of a generic hip model (groups 1-3, respectively: 2.6 ± 5.4 vs 1.9 ± 7.0 vs 2.4 ± 5.6; P = .03). There were no statistically significant differences in understanding on final follow-up between patients counseled with CT imaging alone and with a 3D-printed hip model (Table 2).
TABLE 2.
Analysis of Patient-Reported Novel Questionnaire Results on Femoroacetabular Impingement Comprehensiona
| CT Alone | Generic Model | Haptic 3D Model | P | |
|---|---|---|---|---|
| Initial clinical visit: satisfaction (0-10) | 8.5 ± 1.8 | 9.0 ± 1.5 | 8.7 ± 1.1 | .74 |
| Initial follow-up | ||||
| Satisfaction | 9.5 ± 1.1 | 9.4 ± 0.7 | 9.7 ± 0.5 | .62 |
| ▵ satisfaction | 1.0 ± 1.8 | 0.4 ± 1.4 | 1.0 ± 0.8 | .47 |
| ▵ understanding | 2.9 ± 2.7 | 2.4 ± 2.3 | 2.2 ± 1.9 | .03b |
| Final follow-up (retention measure): ▵ understanding | 2.6 ± 5.4 | 1.9 ± 7.0 | 2.4 ± 5.6 | .03b |
aValues are presented as mean ± SD. 3D, 3-dimensional; CT, computed tomography.
bP < .05.
Analysis of Constituent Questions
An unblinded analysis of the constituent questions of our novel outcomes questionnaire revealed that certain questions were more predictive of the final results of our study than others. The following 3 questions most closely modeled the overall findings of our study with regard to trends in understanding among the 3 experimental groups: question 10, “I feel that I have a basic understanding of the way deformities of the ball and/or socket can cause injury to the hip joint articular cartilage (surface padding) or labrum”; question 11, “I feel that I have a basic understanding of how femoroacetabular impingement is believed to relate to premature osteoarthritis of the hip”; and question 13, “I feel that I have a thorough understanding of my unique hip deformity and how surgical intervention may be able to correct these deformities.”
Discussion
Use of a custom 3D hip model does not appear to lead to superior patient-reported understanding and satisfaction during the treatment of FAI when compared with the use of 3D CT imaging alone.
Osteoarthritis is an orthopaedic disorder commonly affecting the hip joint and can involve a variety of diverse etiologies.10,11,18 Over the past few decades, research has revealed the association between abnormal joint morphology and development of early-age osteoarthritis. This process, termed femoroacetabular impingement, has been heavily described in recent literature and has become a staple of modern sports orthopaedic practices.
While the etiology behind FAI has yet to be completely understood, its prevalence has significantly risen over the past few years. Diagnosis of FAI involves comprehensive physical and radiographic examinations by well-trained practitioners. Plain radiography is routinely utilized to closely examine bony morphology of the hip joint. While version, orientation, and geometry of the acetabulum and proximal femur can be readily assessed, plain radiographs are unable to fully capture the unique 3D anatomy and dynamic interaction of the hip joint. Given this limitation, some surgeons have moved to utilizing CT or magnetic resonance imaging (MRI) for their associated multidimensional processing techniques, which can be helpful in both assessment and surgical planning. While these imaging modalities may help to guide practitioners on treatment, they may be of little assistance when preoperatively counseling patients on the etiology of their symptoms.
Haptic 3D-printed models have proven to be useful in educating patients on their anatomy and pathophysiology in various areas of modern medicine.2–4 Given the increasing emphasis on and importance of patient understanding and satisfaction, the use of these models will likely make their way into other areas of medicine, particularly those involving complex anatomic relationships.
In the current study, patients who underwent preoperative counseling with haptic 3D-printed hip models paradoxically demonstrated reduced perceived comprehension of their FAI pathophysiology but had similar clinical satisfaction to those counseled with isolated CT imaging and generic hip models at initial follow-up. This rejects the hypothesis of our study. In contrast, at the time of final follow-up (retention measure), patients preoperatively counseled with isolated CT imaging as well as those counseled with haptic 3D models had greater increases in their reported perceived comprehension of FAI as compared with those counseled with generic hip models. Therefore, one could conclude that the use of an individualized haptic 3D hip model may be useful for patient retention of clinical information. Various factors can likely explain the former findings. FAI is a complex orthopaedic phenomenon involving a variety of anatomic variations as well as the physical forces that coincide with them. Patients without medical training, knowledge of human anatomy, or a thorough understanding of joint physiology may initially struggle to comprehend and digest the volume of information presented to them at their initial clinical encounter. Additionally, there may exist a limit in the amount of information that patients can reasonably digest at each clinical encounter; any information beyond this amount may confuse them and decrease their understanding and satisfaction. Finally, a wide spectrum of intellect likely exists among patients, allowing some to better process and understand clinical information than others.
The findings of this study are of immediate relevance to arthroscopic hip surgery, as it reveals the most effective modality that can be used to preoperatively counsel patients on their FAI. Enhancing patient understanding and satisfaction in a cost-effective manner continues to be of utmost importance in modern medicine, especially during the perioperative time frame. This study reveals that the use of 3D CT imaging alone provides patients with ample data to understand the cause of their hip pathology as well as the planned surgical intervention. Thus, these data signify that utilizing 3D patient-specific hip models may not be a cost-effective means of enhancing patient understanding within these areas.
Limitations
Study limitations include the lack of blinding within the study design as well as the use of a novel questionnaire that has not yet been validated. As previously stated, this study was designed to examine patients’ perception of their understanding regarding FAI, an area that has gained considerable momentum in recent years. Unfortunately, there are no current validated questionnaires gauging patients’ understanding with respect to the topic of FAI; thus, one was created to implement in this study. The questionnaire was designed to examine understanding and satisfaction of each component of FAI. Blinding was not performed during this study, as the primary surgeon utilized the imaging/modeling data during clinical encounters with patients in an effort to outline their individual pathology as well as discuss the role of surgical intervention. This lack of blinding may have introduced some degree of bias.
The inability to control for patient-level education as well as possible physician counseling prior to referral also leads to some degree of bias and error. Before referral to orthopaedic care, patients often may have undergone initial workup or discussion with primary care providers or nonoperative orthopaedic specialists. This is not a readily predictable pattern and may cause some patients to experience increased physician counseling times, thus influencing their reported understanding and clinical satisfaction. Future studies may benefit from controlling for this factor.
As a study focusing on patients’ understanding and satisfaction, inclusion of other validated outcome questionnaires would have been helpful to better characterize each patient’s baseline function, pain, and mood, as these may be tied to their satisfaction within the study. Additionally, time spent with each patient was not recorded during this study and could have played a role in our findings. Patients who received more face time with a provider may have reported increased satisfaction with the clinical visit, which could have altered our results. This should be adequately addressed in future studies.
MRI and MRI arthrogram also exist as available diagnostic methods to evaluate patients with FAI. As these methods help to closely examine cartilaginous damage and defects, they serve an important role in understanding the disease mechanism of symptomatic patients. In this study, we did not utilize a separate arm examining the influence of MRI on patient comprehension or satisfaction. Thus, future studies may benefit from a separate cohort in which MRI is utilized to inform patients on the pathomorphology.
Last, a more ideal control group of patients for this study would have been patients who received plain radiographs alone without the use of CT imaging or modeling. In our current practice, all patients with radiographically diagnosed FAI undergo routine CT imaging of the hip to better quantify and describe the morphology and size of their implicated lesions. This CT imaging is also used to determine if an arthroscopic surgical intervention is warranted or possible. In future studies, patients could be administered the initial questionnaire after plain radiographs to create a more ideal baseline score. Additionally, a fourth group of patients who undergo only plain radiographs could be added to better serve as a control; however, these patients may eventually require CT imaging if their lesions warrant surgical intervention.
Conclusion
Preoperative counseling with haptic 3D hip models does not appear to favorably affect patient-reported understanding or satisfaction with regard to one’s FAI when compared with the use of CT imaging alone. Continued research into alternative counseling means may serve to improve patient understanding and satisfaction on this complex anatomic phenomenon.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: J.E. has received research support from Synthes. B.G. has received research support from Carticept, Exactech, Smith & Nephew, Prodigy, and Arthrex; is a consultant for Arthrex; receives royalties from Arthrex; and is a paid speaker/presenter for Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Research Subjects Review Board at the University of Rochester.
References
- 1. Audenaert EA, Baelde N, Huysse W, et al. Development of a three-dimensional detection method of cam deformities in femoroacetabular impingement. Skeletal Radiol. 2011;40(7):921–927. [DOI] [PubMed] [Google Scholar]
- 2. Bernhard JC, Isotani S, Matsugasumi T, et al. Personalized 3D printed model of kidney and tumor anatomy: a useful tool for patient education. World J Urol. 2016;34(3):337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Biglino G, Capelli C, Wray J, et al. 3D-manufactured patient-specific models of congenital heart defects for communication in clinical practice: feasibility and acceptability. BMJ Open. 2015;5(4):e00716 5-2014-007165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Biglino G, Koniordou D, Gasparini M, et al. Piloting the use of patient-specific cardiac models as a novel tool to facilitate communication during cinical consultations. Pediatr Cardiol. 2017;38(4):813–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Byrd JW. Femoroacetabular impingement in athletes, part I: cause and assessment. Sports Health. 2010;2(4):321–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Byrd JW. Femoroacetabular impingement in athletes, part II: treatment and outcomes. Sports Health. 2010;2(5):403–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Byrd JW, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467(3):739–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Clohisy JC, Nunley RM, Otto RJ, et al. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115–121. [DOI] [PubMed] [Google Scholar]
- 9. Ganz R, Gill TJ, Gautier E, et al. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83(8):1119–1124. [DOI] [PubMed] [Google Scholar]
- 10. Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed] [Google Scholar]
- 11. Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed] [Google Scholar]
- 12. Jacobson JA, Bedi A, Sekiya JK, et al. Evaluation of the painful athletic hip: imaging options and imaging-guided injections. AJR Am J Roentgenol. 2012;199(3):516–524. [DOI] [PubMed] [Google Scholar]
- 13. Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73(3):423–429. [DOI] [PubMed] [Google Scholar]
- 14. Kleyer A, Beyer L, Simon C, et al. Development of three-dimensional prints of arthritic joints for supporting patients’ awareness to structural damage. Arthritis Res Ther. 2017;19(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Leunig M, Beck M, Kalhor M, et al. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement. Radiology. 2005;236(1):237–246. [DOI] [PubMed] [Google Scholar]
- 16. Leunig M, Ganz R. The evolution and concepts of joint-preserving surgery of the hip. Bone Joint J. 2014;96B(1):5–18. [DOI] [PubMed] [Google Scholar]
- 17. Meyer DC, Beck M, Ellis T, et al. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181–185. [DOI] [PubMed] [Google Scholar]
- 18. Reginster JY. The prevalence and burden of arthritis. Rheumatology (Oxford). 2002;41(suppl 1):3–6. [PubMed] [Google Scholar]