Abstract
Background
The Walch B3 glenoid is theorized to be a progression of the B2 biconcave pattern. The present study aimed to compare glenoid indices between B2 and B3 patterns. We hypothesized that the B3 pattern would have significantly worse retroversion, inclination and medialization.
Methods
Computed tomography scans of 50 patients with B2 erosions [mean (SD) age 68 (9) years; 25 male] and 50 patients with B3 erosions [mean (SD) age 72 (8) years; 22 males] were converted into three-dimensional reconstructions. Retroversion, inclination, medialization and humeral head subluxation were compared.
Results
The data demonstrated no statistically significant differences [mean (SD)] between groups when assessing retroversion: B2 = 21 (8)°, B3 = 24 (7)° (p = 0.602); glenoid inclination: B2 = 9 (6)°, B3 = 8 (6)° (p = 0.967); or medialization: B2 = 12 (4) mm, B3 = 14 (4) mm (p = 0.384). In the B2 group, the mean (SD) humeral head subluxation was 80% (10%) according to the scapular plane and 55% (9%) according to the glenoid plane, which was not statistically different from the B3 group with a mean (SD) humeral head subluxation of 81% (7%) according to the scapular plane (p = 0.680) and 54% (7%) according to the glenoid plane (p = 0.292).
Conclusions
These results demonstrated no significant differences between the B2 and B3 erosion patterns, with respect to the glenoid indicies measured. The aetiology of the B3 glenoid cannot be completely explained by progression of wear in a B2 glenoid.
Keywords: glenohumeral osteoarthritis, shoulder arthritis, total shoulder arthroplasty, Walch B2, Walch B3
Introduction
Primary glenohumeral joint osteoarthritis is a common cause of shoulder pain, loss of function, and disability.1 Currently, evidence supports the use of total shoulder arthroplasty (TSA) over hemiarthroplasty for the surgical treatment of end-stage, symptomatic glenohumeral osteoarthritis.2 Analyses of nationwide data in the USA reveal a five-fold increase in the use of TSA between 2000 and 2010.3 The growth in TSA utilization necessitates a thorough understanding of glenoid morphology because it can be an important prognostic factor in implant outcomes and survivorship.4–6
Walch et al.7 originally described three major patterns of glenoid erosion (A, B and C). Recently, Bercik et al.8 introduced the B3 glenoid, characterized by a uni-concave articular surface with greater than 15° retroversion and/or at least 70% posterior humeral head subluxation. One potential theory regarding the aetiology of the B3 is that the erosion results from progression of a B2 glenoid.8 As wear progresses, the newly eroded glenoid surface (neoglenoid) increases. Eventually, the neoglenoid occupies the entire articular surface, converting a bi-concave B2 into a uni-concave B3 glenoid (Figure 1).
Figure 1.
An axillary radiograph (a) of a Walch B2 glenoid wear pattern characterized by posterior humeral head subluxation, posterior glenoid bone loss and a bi-concave appearance. Also shown is a Walch B3 glenoid (b) wear pattern characterized by posterior humeral head subluxation, excessive retroversion and a uni-concave appearance.
The present study aimed to investigate the development of B3 glenoids by comparing them with the B2 glenoid. We hypothesized that glenoid measurements would be significantly worse in the B3 than the B2, including retroversion, inclination, medialization and posterior humeral head subluxation. This would support the notion that, as a B2 progresses, it converts into a B3 glenoid.
Materials and methods
Prospectively collected shoulder arthroplasty databases from two institutions were used to identify 50 B2 and 50 B3 glenoids. Two senior experienced shoulder surgeons (GW and GSA) confirmed the glenoid morphologies. The B2 glenoid was defined as having posterior humeral head subluxation and a bi-concave articular surface.7,8 The B3 glenoid was defined as having greater than 15° of retroversion, a uni-concave appearance and/or at least 70% posterior humeral head subluxation.8 Patients with rotator cuff tear arthropathy, inflammatory arthritis or post-traumatic arthritis were excluded. In the B2 glenoids, there were 25 males and 25 females with a mean (SD) age of 68 (9) years (range 42 years to 84 years). The B3 glenoid group had 22 male and 28 female patients with a mean (SD) age of 72 (8) years (range 57 years to 87 years).
The DICOM (Digital Imaging and Communications in Medicine) data from each patient’s pre-operative shoulder computed tomography (CT) scan were uploaded into validated three-dimensional (3D) imaging software (Glenosys; Imascap, Brest, France).9,10 All CT scans that did not include the entire scapula were excluded. A mathematical algorithm was used to calculate glenoid version and inclination in an automated fashion. Additionally, posterior humeral head subluxation was determined according to the scapular plane and the glenoid plane. Glenoid medialization was measured (mm) manually using the Glenosys software.
Glenoid measurements
Glenoid retroversion was determined in the Glenosys software by adjusting a best-fit sphere to the articular surface and measuring the angle between the centre line of this glenoid sphere and the scapula plane projected on the transverse axis (Figure 2). Glenoid inclination was the angle between the glenoid sphere centre line and the vertical plane of the scapula.
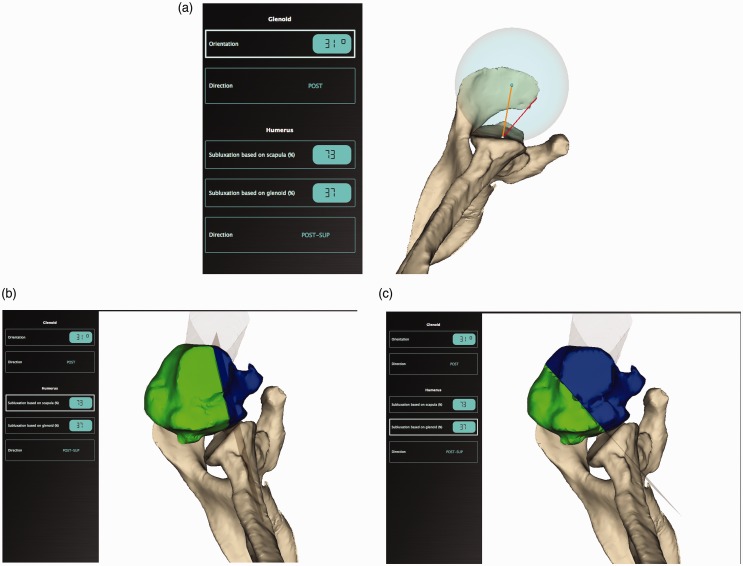
Figure 2.
The Glenosys software was used to calculated glenoid retroversion (a), humeral head subluxation according to the scapular plane (b) and humeral head subluxation according to the glenoid plane (c).
Posterior humeral head subluxation according to the scapular plane was calculated by dividing the 3D volumetric portion of the humeral head that lies posterior to the scapular plane by the whole volume of the humeral head. Humeral head subluxation according to the glenoid plane was calculated as described by Walch et al.7 The percentage of subluxation was interpreted using the same criteria as Walch et al.7 Values between 45% and 55% represented a centred humeral head, whereas values less than 45% were anteriorly subluxated and those greater than 55% were posteriorly subluxated (Figure 2). Finally, glenoid medialization was measured by determining the maximum depth (mm), orthogonal to the scapular plane, from the anterior rim of the glenoid to the most medial eroded part of the posterior rim.
Statistical analysis
Statistical analyses were performed using SPSS (IBM, Armonk, NY, USA). Descriptive parameters were reported as the mean (SD). Continuous variables were compared using Student’s t-tests between the B2 and B3 glenoids with the p-value adjusted using the Bonferroni correction. Linear regression analyses were performed to determine the correlation between degree of glenoid erosion and the various glenoid indices that were measured.
Results
Table 1 summarizes the comparisons between B2 and B3 glenoids. There was no statistically significant difference in age between the groups (Bonferroni adjusted p = 0.03). We also identified no statistically significant differences between the two types of glenoids in any of the parameters measured. When assessing mean glenoid retroversion, there were no differences between B2s [21 (8°)] and B3s [24 (7°)], (p = 0.602). There were no differences in glenoid inclination between B2s [9 (6°)] and B3s [8 (6°)], (p = 0.967). The degree of posterior glenoid bone loss, which was measured as medialization, was not different between B2s [12 (4) mm] and B3s [14 (4) mm] (p = 0.384).
Table 1.
Summary of parameters compared between B2 and B3 cohorts.
| B2 glenoid | B3 glenoid | p value | |
|---|---|---|---|
| Retroversion | 21 (8)° | 24 (7)° | 0.602 |
| Inclination | 9 (6)° | 8 (6)° | 0.967 |
| Medialization | 12 (4) mm | 14 (4) mm | 0.384 |
| Subluxation (glenoid plane) | 55% (9%) | 54% (7%) | 0.292 |
| Subluxation (scapular plane) | 80% (10%) | 81% (7%) | 0.680 |
Data are the mean (SD).
In the B2 group, the mean (SD) humeral head subluxation was 80% (10%) according to the scapular plane and 55% (9%) according to the glenoid plane. These B2 values were not statistically different from the B3 group, with a mean humeral head subluxation of 81% (7%) according to the scapular plane (p = 0.680), and 54% (7%) according to the glenoid plane (p = 0.292).
Linear regression analyses demonstrated that increasing glenoid erosion (neoglenoid) correlated with decreasing subluxation of the humeral head based on the glenoid plane (Figure 3). Specifically, for every 1% increase in neoglenoid, there was a 0.1% decrease in posterior humeral head subluxation, although this was not statistically significant (p = 0.103). Linear regression also demonstrated that glenoid retroversion (Figure 4a) and medialization (Figure 4b) increased with progressive glenoid erosion. These correlations were statistically significant. For every 1% increase in neoglenoid, there was a 0.1° increase in glenoid retroversion (p = 0.003) and 0.1 mm increase in medialization (p = 0.002).
Figure 3.
A scatter plot with a best-fit line comparing the amount of neoglenoid and posterior humeral head subluxation according to the glenoid plane.
Figure 4.
Scatter plots demonstrating a positive correlation between glenoid erosion and glenoid retroversion (a) and medialization (b).
Discussion
It is assumed that posterior humeral head subluxation leads to asymmetric loading of the posterior glenoid rim and eventual posteroinferior glenoid wear.11 This produces the bi-concave erosion pattern now commonly referred to as B2, according to the Walch classification.7 The newly eroded posterior facet of the glenoid has been termed the neoglenoid, whereas the remaining anterior native articular surface is referred to as the paleoglenoid. As glenoid wear progresses, it has been theorized that the neoglenoid becomes larger and would eventually occupy the entire glenoid articular surface, creating a uni-concave surface recently referred to as B3.8 If this were the natural progression to a B3 wear pattern, it would imply that B3 glenoids would be more worn, with greater medialization and retroversion. The results of the present study identified no significant differences between the B2 and B3 glenoids when measuring retroversion, inclination, medialization and humeral head subluxation. However, linear regression analyses demonstrated small trends that would support the theory of progression from B2 to B3. Specifically, as glenoid erosion increases, there are corresponding increases in glenoid retroversion and medialization, whereas posterior humeral head subluxation decreases. These results suggest that the pathoanatomy of glenoid erosion in osteoarthritis is more complex than simply progressive degenerative changes from B2 to B3. Overall, the results of the present study demonstrate that the only substantial difference between a B2 and a B3 glenoid is the glenoid appearance, bi-concave versus uni-concave, respectively.
There are several theories that may explain the observed findings. Bercik et al.8 proposed the possibility that the posteriorly subluxated humeral head may erode the entire glenoid with greater wear posteriorly, leading to pathological glenoid retroversion without an interval B2 phase. Alternatively, the B3 glenoids may represent a variant of the type C glenoids, which are dysplastic, severely retroverted glenoids not caused by erosion.7 A third explanation may relate to the limited sample size. It is conceivable that the 3° increase in glenoid retroversion and the greater 2 mm medialization from B2s to B3s is a truly significant finding that represents progression of a B2 to a B3. Overall, the results of the present study improve our understanding of glenohumeral joint osteoarthritis; however, they still leave several important aetiological questions unanswered. Further comparative and natural history studies are required to understand the erosion patterns in glenohumeral osteoarthritis.
Recognizing differences in glenoid morphology has important clinical implications during shoulder arthroplasty. Failure to appreciate excessive glenoid retroversion or posterior humeral head subluxation can lead to suboptimal outcomes.5 Uncorrected pathological retroversion during shoulder arthroplasty may also lead to early glenoid component loosening.12,13 With the recent classification of B3 glenoids, longitudinal studies on clinical outcomes are required to assess whether this new morphological pattern matches the outcomes seen with B2 glenoids. If clinical outcomes are worse than the suboptimal outcomes observed with excessive B2 retroversion, alternative treatment options may be necessary to address the B3 glenoid.
A strength of the present study is the use of a validated software system that automatically calculates glenoid version, inclination and humeral head subluxation.9,10 Additionally, 3D reconstructed images were used to measure glenoid parameters, which have been shown to be more accurate than 2D measurements.14–16 The limitations of the present study include the smaller sample size and the use of static CT images to determine subluxation. Glenohumeral subluxation is likely a dynamic process, which varies according to rotator cuff muscle activation, arm position and patient position in the CT scanner. Although all patients were scanned with a similar protocol in the supine position, it is possible that the subluxation index would be different if patients could be scanned standing or in functional arm positions.
Conclusions
The present study demonstrated no significant differences between B2 and B3 glenoid wear patterns in terms of retroversion, inclination, medialization and humeral head subluxation. The results suggest that the development of the type B3 glenoid is more complex than progressive erosion from a B2 glenoid. Further studies are needed to clarify the pathoanatomy of B2 and B3 glenoids in glenohumeral osteoarthritis.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Disclaimer: The authors (KC, NKK, & LMF), their immediate families and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article. JC is an employee of Imascap. GW is a consultant for Wright Medical-Tornier Inc. and has ownership of Imascap. GSA is a consultant for Wright Medical-Tornier Inc., Imascap and Depuy Synthes. No company had any input in to the study design, protocol, testing, data analysis or manuscript preparation.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
Institutional Review Board Approval (IRB) was obtained at the Lawson Research Institute/St. Josephs Health Care (Approval #R-15-057).
References
- 1.Singh JA, Sperling J, Buchbinder R, et al. Surgery for shoulder osteoarthritis. Cochrane Database Syst Rev 2010, pp. Cd008089–Cd008089. [DOI] [PubMed] [Google Scholar]
- 2.Radnay CS, Setter KJ, Chambers L, et al. Total shoulder replacement compared with humeral head replacement for the treatment of primary glenohumeral osteoarthritis: a systematic review. J Shoulder Elbow Surg 2007; 16: 396–402. [DOI] [PubMed] [Google Scholar]
- 3.Trofa D, Rajaee SS, Smith EL. Nationwide trends in total shoulder arthroplasty and hemiarthroplasty for osteoarthritis. Am J Orthop 2014; 43: 166–172. [PubMed] [Google Scholar]
- 4.Walch G, Moraga C, Young A, et al. Results of anatomic nonconstrained prosthesis in primary osteoarthritis with biconcave glenoid. J Shoulder Elbow Surg 2012; 21: 1526–1533. [DOI] [PubMed] [Google Scholar]
- 5.Iannotti JP, Norris TR. Influence of preoperative factors on outcome of shoulder arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg 2003; 85A: 251–258. [DOI] [PubMed] [Google Scholar]
- 6.Denard PJ, Walch G. Current concepts in the surgical management of primary glenohumeral arthritis with a biconcave glenoid. J Shoulder Elbow Surg 2013; 22: 1589–1598. [DOI] [PubMed] [Google Scholar]
- 7.Walch G, Badet R, Boulahia A, et al. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplast 1999; 14: 756–760. [DOI] [PubMed] [Google Scholar]
- 8.Bercik MJ, Kruse K, II, Yalizis M, et al. A modification to the Walch classification of the glenoid in primary glenohumeral osteoarthritis using three-dimensional imaging. J Shoulder Elbow Surg 2016; 25: 1601–1606. [DOI] [PubMed] [Google Scholar]
- 9.Moineau G, Levigne C, Boileau P, et al. Three-dimensional measurement method of arthritic glenoid cavity morphology: feasibility and reproducibility. Orthop Traumatol Surg Res 2012; 98: S139–S145. [DOI] [PubMed] [Google Scholar]
- 10.Walch G, Vezeridis PS, Boileau P, et al. Three-dimensional planning and use of patient-specific guides improve glenoid component position: an in vitro study. J Shoulder Elbow Surg 2015; 24: 302–309. [DOI] [PubMed] [Google Scholar]
- 11.Knowles NK, Keener JD, Ferreira LM, et al. Quantification of the position, orientation, and surface area of bone loss in type B2 glenoids. J Shoulder Elbow Surg 2015; 24: 503–510. [DOI] [PubMed] [Google Scholar]
- 12.Farron A, Terrier A, Buchler P. Risks of loosening of a prosthetic glenoid implanted in retroversion. J Shoulder Elbow Surg 2006; 15: 521–526. [DOI] [PubMed] [Google Scholar]
- 13.Shapiro TA, McGarry MH, Gupta R, et al. Biomechanical effects of glenoid retroversion in total shoulder arthroplasty. J Shoulder Elbow Surg 2007; 16: S90–S95. [DOI] [PubMed] [Google Scholar]
- 14.Budge MD, Lewis GS, Schaefer E, et al. Comparison of standard two-dimensional and three-dimensional corrected glenoid version measurements. J Shoulder Elbow Surg 2011; 20: 577–583. [DOI] [PubMed] [Google Scholar]
- 15.Hoenecke HR, Jr., Hermida JC, Flores-Hernandez C, et al. Accuracy of CT-based measurements of glenoid version for total shoulder arthroplasty. J Shoulder Elbow Surg 2010; 19: 166–171. [DOI] [PubMed] [Google Scholar]
- 16.Kwon YW, Powell KA, Yum JK, et al. Use of three-dimensional computed tomography for the analysis of the glenoid anatomy. J Shoulder Elbow Surg 2005; 14: 85–90. [DOI] [PubMed] [Google Scholar]