Abstract
Background:
Patient navigation (PN) programs can improve cancer screening in underserved populations. PN may advance quality and equity of care by supporting individuals at increased risk of not receiving recommended care.
Objective:
To evaluate patient satisfaction with medical care and PN for cancer screening.
Methods:
We conducted a telephone survey of patients enrolled in a randomized control trial evaluating the impact of PN for cancer screening to assess their satisfaction with overall medical care and the PN program. We measured patient satisfaction with medical care using the Patient Satisfaction Questionnaire-18 and evaluated patient satisfaction with PN in the navigated group using the Patient Satisfaction with Interpersonal Relationships with Navigator questionnaire.
Key Results:
Satisfaction surveys were completed by 114 navigated and 108 non-navigated patients (33% response rate). Patients who received PN had higher satisfaction scores with overall medical care (71.0 vs 66.8; P < .001).
Conclusions:
Our findings show that patients at high risk of nonadherence with comprehensive cancer screening were satisfied with PN and suggest that PN could positively influence patient satisfaction with overall medical care.
Keywords: patient navigation, cancer screening, patient satisfaction
Introduction
Advances in medical care over the past several decades have resulted in significant survival gains and improvement in health outcomes; however, these innovations have been accompanied by fragmentation of the health-care system and subspecialization of health services. This complexity creates barriers for patients seeking care and exacerbates preexisting inequity, disadvantaging historically disenfranchised populations who may not have the opportunity, access, or financial means to navigate the health-care system. One strategy to address this challenge is to utilize specially trained community health workers, called patient navigators, to identify patient-reported barriers to care and to address larger disparities in health-care access and quality (1).
Patient navigation (PN) programs were initially developed to address disparities in cancer screening and treatment outcomes among vulnerable populations (1 –4). PN programs promote increased participation in cancer screening and adherence to diagnostic follow-up after detection of an abnormality (5). Similarly, PN programs for cancer screening have been shown to be effective when targeting disenfranchised populations (6 –8). The most successful patient outcomes have been seen in PN programs that focus on cancer screening and outreach among patient populations with navigators whose race and language reflect that of the patient community (3,5,6,9).
Although PN programs have been implemented in many patient populations and at different stages of cancer care, the correlation between patient satisfaction with PN programs and overall medical care has not been broadly studied (3,10). Navigators are viewed as an extension of the health-care system, which underscores the importance of investigating the relationship between PN and satisfaction with overall medical care. Patients’ experiences with PN may directly impact their views of the health-care system as a whole, particularly as PN becomes part of routine delivery of care. Understanding the relationship between satisfaction with PN and with the health-care system, in general, is important because a positive interaction with a navigator may encourage increased engagement with other dimensions of health care.
Studies utilizing validated surveys to examine satisfaction with cancer care between navigated and non-navigated patients have shown mixed results. Two studies evaluating large, multicenter PN programs found no difference in satisfaction with care between patients randomized to navigation and to usual care following an abnormal cancer screening result (10–11). Similarly, a study evaluating PN for women requiring core biopsy after an abnormal breast finding showed no difference in satisfaction between navigated and non-navigated patients (12). In contrast, an evaluation of a PN program focused on care of minority and low-income women with abnormal mammogram findings found that PN was associated with significantly higher satisfaction with overall medical care and a reduction in patient-reported anxiety (3). Another recent study among medically underserved patients with a definitive cancer diagnosis has found a significant, positive relationship between PN and satisfaction with overall cancer care (13). Two additional studies and a systemic review of PN during cancer treatment showed higher satisfaction with care in patients who were navigated (14 –16). In all, although data are mixed, the current literature supports a trend toward improvement in patient satisfaction among patients who have PN for cancer treatment or confirmatory testing.
Differences in the impact of PN on satisfaction with care may be due to variation between programs or to characteristics of the patients targeted by PN. However, to our knowledge, no study to date has employed validated survey instruments to evaluate patient satisfaction with overall medical care—including noncancer care—among patients receiving PN for cancer screening.
The objective of this study was to evaluate patient satisfaction with a novel patient-centered PN program for comprehensive cancer screening among patients at high risk of nonadherence within a large primary care network and to evaluate the relationship between patient satisfaction with navigation and their satisfaction with overall medical care (17).
Methods
Study Site
The Massachusetts General Primary Care Practice-Based Research Network consists of 18 primary care practices, including 6 community health centers, affiliated with Massachusetts General Hospital. The network has used a population health IT management system in all primary care practices since 2011 to identify patients with an established primary care physician (PCP) who are overdue for breast, cervical, and colorectal cancer screening and automatically sends reminder letters to encourage patients to schedule overdue screening tests. Additionally, the automated system utilizes an algorithm that incorporates patient information including number of overdue tests, primary language spoken, and no-show visit history to identify patients at high risk of nonadherence with cancer screening and refers them to the PN program (17).
Patient Navigators
Navigators in the PN program are community health workers experienced in cancer care navigation. Navigators are trained in motivational interviewing, problem-solving, goal setting, and use of the electronic health record system. Each navigator is assigned a panel of high-risk patients to guide in obtaining age-appropriate screening. They contact these high-risk patients via telephone and address overdue cancer screening (colorectal, breast, cervical), focusing on assisting patients with individual barriers to screening. Interaction with a navigator may range from an initial phone call to several discussions, depending on patient need. In addition, navigators take detailed notes about their conversations with patients and communicate with the patients’ PCP through the electronic health record. Patient navigation is provided in 5 languages and can offer services using an interpreter for patients who speak other languages.
Participants
Eligible patients from 18 Massachusetts General Hospital primary care practices were part of a randomized control trial designed to evaluate the effectiveness of a PN program for cancer screening. As a part of this larger study conducted between April and December 2014, patients overdue for breast, cervical, and/or colorectal screening and who were identified as being at high risk of nonadherence with screening were randomized to either PN (n = 792) or usual care (n = 820). All patients benefited from the standard of care, such as automated reminder letters, but only those randomized to PN received individualized navigation to help schedule and complete screening during the trial period (17). Patients were only asked to participate in our satisfaction study if they had the first contact with a navigator after July 2014. Because our study was nested within a larger, ongoing randomized control trial, only 340 PN patients met this inclusion criterion. For comparison, we randomly selected 340 patients in the usual care group for the satisfaction survey.
Study Design and Data Collection
Telephone surveys were conducted from September 2014 through January 2015. We sent introductory letters about the survey in batches of 80 per week to equal numbers of randomly selected patients in the PN and control arms. No remuneration was offered for participation. Patients were contacted by phone 1 week after the introductory letter was mailed and asked to complete the Patient Satisfaction Questionnaire-18 (PSQ-18). Patients in the PN group were then asked to complete the Patient Satisfaction with Navigation-Interpersonal (PSN-I) questionnaire, in that order. Our research team attempted to contact patients on a minimum of 3 separate occasions at both personal and work telephone numbers. Surveys were administered 1 to 5 months after contact with PN in the patient’s preferred language where possible.
Instruments and Measures
Several tools have been developed to evaluate patient satisfaction with PN (9,18). One of the most pertinent tools for evaluating a patient’s experience with PN is the PSN-I scale (19). The PSN-I employs a Likert scale to evaluate patient perception of their interaction with PN, including communication, empathy, and reliability. Patient Satisfaction with Navigation-Interpersonal scores range from 9 to 45, with higher scores indicating better satisfaction. The tool has been validated in both English and Spanish (20).
For this study, we utilized the PSQ-18 survey to evaluate patient satisfaction with general medical care. Published by the RAND Corporation in 1994, the PSQ-18 “Short-form Patient Satisfaction Questionnaire” is an 18-question survey that employs a 1 to 5 Likert scale to evaluate satisfaction with 7 dimensions of patient care: general satisfaction, technical quality, interpersonal manner, communication, financial aspects, time spent with doctor, and accessibility and convenience. Patient Satisfaction Questionnaire-18 scores range from 18 to 90 with higher scores indicating better satisfaction. The PSQ-18 is publicly available, has been translated into multiple languages, and is validated for the assessment of primary care services (21).
The institutional review board approved all study activities.
Statistical Analysis
We summarized continuous variables using mean (standard deviation) and categorical variables using frequency with percentage. We compared characteristics of respondents in the intervention and control arm using 2-sample t tests or χ2 tests, as appropriate. We employed 2-sample t tests to compare patient satisfaction with overall medical care, as measured by the PSQ-18, between the 2 study arms for all patients and relevant subgroups. In the navigated patients, we also summarized the relationship between patient satisfaction with PN (as measured by PSN-I) and their satisfaction with overall medical care (as measured by PSQ-18) using a Pearson correlation coefficient. We used a 2-way analysis of variance adjustment to address the racial differences between the 2 groups.
Results
Of the 680 patients contacted, 221 (32.5%) agreed to participate and completed the survey (114 [33.5%] intervention and 108 [31.8%] control). Among patients not agreeing to participate, 104 (15.3%) could not be contacted due to outdated or inaccurate contact information (41 intervention and 63 control), and 81 (11.9%) were reached but declined to participate (31 control, 50 intervention). Two patients selected for navigation by the algorithm died. The remaining patients did not respond to a standard voicemail explaining the project.
Respondents had a mean age of 59.4 years, most were female (57.5%), spoke English (90.0%), and 48.0% had commercial health insurance. Although there were significantly more non–white-navigated respondents, there was no difference in age, gender, primary language, type of insurance, patient–physician connectedness status, or number of clinic visits over the prior 3 years among intervention and control group respondents (Table 1).
Table 1.
Demographic Characteristics of Navigated And Non-Navigated Patients.
| Characteristics | Navigated (n = 114) | Non-Navigated (n = 107) | P Value |
|---|---|---|---|
| Age, mean (SD) | 59.5 (7.9) | 59.3 (8.0) | .86 |
| Gender, female | 66 (57.9%) | 61 (57.0%) | .89 |
| Race, white | 76 (66.7%) | 88 (82.2%) | .01 |
| Primary language, English | 99 (86.8%) | 100 (93.5%) | .10 |
| Insurance | .74 | ||
| Commercial | 58 (50.9%) | 48 (44.9%) | |
| Medicaid | 29 (25.4%) | 28 (26.2%) | |
| Medicare | 23 (20.2%) | 28 (26.2%) | |
| Self-pay | 4 (3.5%) | 3 (2.8%) | |
| Patient–physician connectedness status | .51 | ||
| PCP connected | 99 (86.8%) | 96 (89.7%) | |
| Practice connected | 15 (13.2%) | 11 (10.3%) | |
| Clinic visits over 3 years, mean (SD) | 8.2 (7.1) | 9.7 (8.9) | .19 |
Abbreviations: PCP, primary care physician; SD, standard deviation.
Patients in the PN (intervention) group had higher satisfaction with their overall medical care compared to control patients (mean PSQ-18: 71.0, standard deviation [SD]: 6.33 vs 66.8, SD: 8.39; P < .001). This difference persisted after adjusting for the racial differences between intervention and control groups (adjusted mean PSQ-18: 71.0 vs 66.7; P < .001). Patient satisfaction was also higher among intervention patients in relevant subgroups of age (<60 and ≥60 years), gender, race (white and non-white), insurance (commercial/Medicare and Medicaid/no insurance), and among English speakers, but not among a very small sample of non–English-speaking patients (Table 2).
Table 2.
Mean PSQ-18 Scores Among Navigated And Non-Navigated Patients.
| Navigated | Non-Navigated | ||||
|---|---|---|---|---|---|
| Mean (SD) | N | Mean (SD) | N | Mean (SD) | P Value |
| Overall | 114 | 71.0 (6.3) | 107 | 66.8 (8.4) | <.001 |
| Age | |||||
| <60 years | 62 | 70.7 (7.1) | 52 | 67.0 (6.8) | .01 |
| ≥60 years | 52 | 71.4 (5.3) | 55 | 66.5 (9.7) | .002 |
| Gender | |||||
| Female | 66 | 71.5 (5.8) | 61 | 68.7 (7.0) | .02 |
| Male | 48 | 70.4 (7.0) | 46 | 64.2 (9.4) | <.001 |
| Race | |||||
| White | 76 | 71.4 (6.7) | 88 | 66.5 (8.7) | <.001 |
| Non-white | 38 | 70.2 (5.6) | 19 | 68.1 (6.7) | .24 |
| Language | |||||
| English | 99 | 71.2 (6.1) | 100 | 66.4 (8.3) | <.001 |
| Non-English | 15 | 69.7 (7.6) | 7 | 72.7 (7.4) | .40 |
| Insurance | |||||
| Commercial or Medicare | 23 | 71.7 (5.9) | 28 | 69.9 (6.6) | .31 |
| Medicaid or none | 91 | 70.8 (6.4) | 79 | 65.7 (8.7) | <.001 |
Abbreviations: PSQ, Patient Satisfaction Questionnaire; SD, standard deviation.
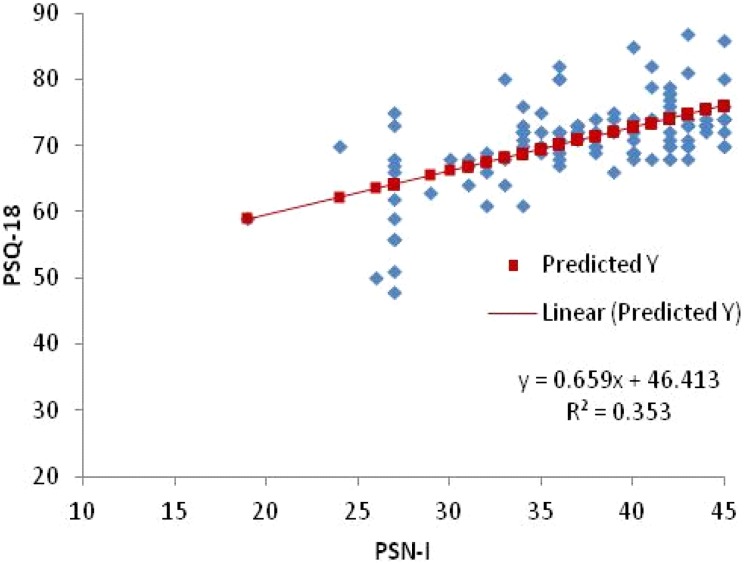
The average PSN-I score among the 114 intervention respondents was 36.7 (SD: 7.6), which is equivalent to 78.6 on a 0 to 100 scale (4). Among intervention patients, the Pearson correlation coefficient between PSN-I score and PSQ-18 score was 0.5 (Figure 1).
Figure 1.
Patient Satisfaction with Interpersonal Relationships with Navigator versus PSQ-18 (navigated patients). PSQ-18 indicates Patient Satisfaction Questionnaire-18.
Discussion
Our study examined patient satisfaction with general medical care among individuals overdue and at high risk of screening nonadherence who were randomly assigned to PN or usual care. We found that patients who were randomized to PN had significantly higher overall satisfaction with medical care. In addition, we found a positive relationship between satisfaction with PN and satisfaction with general medical care. These findings have several implications as patient navigators become part of the care team responsible for engaging patients in their health.
First, this study indicates that PN can positively impact a patient’s overall satisfaction with medical care, especially the positive interpersonal experience with navigators. This finding suggests that personalized attention via PN may improve satisfaction with overall health care as well as lead to potential improvement of targeted outcomes. Although this study did not evaluate subsequent engagement in general medical care, a likely positive effect of satisfaction with medical care is participation in said care. This is a particular area of interest for future research.
Second, our findings suggest that a PN program guided by an automated algorithm that bypasses PCP referral is generally well received by patients. This has implications for further development of PN as part of population health management because it suggests that PN programs do not necessarily have to rely on PCPs to identify patients who might benefit from navigation (22).
Although there is mixed published data on the impact of PN on patient satisfaction, recent studies have demonstrated increased satisfaction with medical care among patients receiving PN support for cancer treatment and/or follow-up of an abnormal test result (3, 13). Other studies that do not demonstrate a significant difference in satisfaction with care between navigated and non-navigated patients nevertheless demonstrate that navigated patients are more likely than non-navigated patients to understand what to expect at visits following up abnormal cancer screenings (10,23,24). Our findings contribute to a growing literature showing a positive relationship between PN and patient satisfaction and mirror the findings of a recent study that demonstrated increased satisfaction with cancer-related care among patients who ranked the interpersonal relationship with their navigators highly (25).
Our study has few limitations. First, our program took place in a single academic primary care network with a sophisticated, centralized IT system, and established PN program, which may not be generalizable to other primary care networks. In addition, our data are entirely patient-reported and therefore subject to recall bias. We have endeavored to mitigate this bias by only surveying patients with recent PN experience; however, recall bias is an inherent methodological weakness in all survey-based research (9). To reduce response fatigue, we employed shorter surveys; however, the respondents were asked up to 27 questions and conversations lasted up to 20 minutes, which may have limited willingness to participate. Further, our low-response rate may mean that the results presented here do not reflect the broader population. In addition, because our study design asked patients to opt-in to participate in the satisfaction surveys, our data may be subject to response bias, where patients may have elected to respond only if they had strong positive or negative feelings about PN or health care. Due to the inherent design of this study, the interviewer administering the survey was not blinded to the patient’s PN status. Finally, although our study demonstrates significantly higher satisfaction scores among the navigated group, it is unclear whether a difference of 4.3 points on the PSQ-18 is a clinically meaningful difference because, although the questionnaire has been shown to have internal validity, it has not been validated across institutions (21).
Conclusion
Our data suggest that systematically addressing patient-identified barriers to care using targeted PN for cancer screening may improve patient satisfaction with health-care overall. Specifically, we show that patients at high risk of nonadherence with cancer screening who were automatically referred to a PN program reported a more positive overall experience with medical care than patients not referred to the program within a multisite, academic primary care network.
PN is an important tool that may improve care delivery, equity, and quality of care in large, complex, health-care networks. The goals of PN are aligned with the overarching goals of patient-centered medical home efforts that seek to improve quality of care by promoting health-care coordination and patient satisfaction through patient-centered care. Although this study does not evaluate outcomes or cost effectiveness, it has implications for development of PN programs in that it highlights the positive effects that PN can have on satisfaction with general medical care. As PN programs are established in multiple care delivery environments and become standard of care, common expectations and training for patient navigators as well as standardized metrics for evaluation will be necessary for further evaluations of PN effectiveness and the impact of PN on patient satisfaction (26).
Author Biographies
Emilia A Hermann, MD, MPH, is a third-year resident in Internal Medicine at New York Presbyterian, Columbia University Medical Center.
Jeffrey M Ashburner, PHD, MPH, is an epidemiologist in the Division of General Internal Medicine, Massachusetts General Hospital, and an Instructor of Medicine at Harvard Medical School. His research has focused on population health management, preventive cancer screening, and cardiovascular disease prevention.
Steven J Atlas, MD, MPH, is an associate professor of Medicine at Harvard Medical School, and Director of the Practice-Based Research and Quality Improvement in the Division of General Internal Medicine Division at Massachusetts General Hospital, where he is also a practicing primary care physician.
Yuchiao Chang, PhD, is a statistician based at Division of General Internal Medicine, Massachusetts General Hospital. She is also an assistant professor at Harvard Medical School.
Sanja Percac-Lima, MD, PHD, MPH, is an associate professor of Medicine at Harvard Medical School and Physician Leader for Cancer Outreach programs at Massachusetts General Hospital Cancer Center. She is a practicing primary care physician and researcher in the Division of General Internal Medicine at Massachusetts General Hospital.
Footnotes
Authors’ Note: Massachusetts General Hospital entered into a royalty arrangement on June 27, 2013, to commercialize the population management system with SRG Technology, a for-profit company. Dr Atlas is a beneficiary of this royalty arrangement but has not received any payments to date. Dr Atlas has received payments as a consultant for the company. Emilia E. Hermann presented this study at the 38th SGIM Annual Meeting in Toronto, Canada, in May, 2015.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Sanja Percac-Lima is in part supported by American Cancer Society: Cancer Control Career Development Award for Primary Care Physicians, CCCDAA-14-012-01-CCCDA and the Lazarex Cancer Foundation.
References
- 1. Freeman HP, Muth BJ, Kerner JF. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Pract. 1995;3:19–30. [PubMed] [Google Scholar]
- 2. Dohan D, Schrag D. Using navigators to improve care of underserved patients. Cancer. 2005;104:848–55. [DOI] [PubMed] [Google Scholar]
- 3. Ferrante JM, Chen PH, Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. J Urban Health. 2008;85:114–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Paskett ED, Harrop J, Wells KJ. Patient navigation: an update on the state of the science. CA Cancer J Clin. 2011;61:237–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Charlot M, Santana MC, Chen CA, Bak S, Heeren TC, Battaglia TA, et al. Impact of patient and navigator race and language concordance on care after cancer screening abnormalities. Cancer. 2015;121:1477–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Genoff MC, Zaballa A, Gany F, Gonzalez J, Ramirez J, Jewell ST, et al. Navigating language barriers: a systematic review of patient navigators’ impact on cancer screening for limited English proficient patients. J Gen Intern Med. 2016;31:426–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jandorf L, Braschi C, Ernstoff E, Wong CR, Thelemaque L, Winkel G, et al. Culturally targeted patient navigation for increasing African Americans’ adherence to screening colonoscopy: a randomized clinical trial. Cancer Epidemiol Biomarkers Prev. 2013;22:1577–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lasser KE, Murillo J, Lisboa S, Casimir AN, Valley-Shah L, Emmons KM, et al. Colorectal cancer screening among ethnically diverse, low-income patients: a randomized controlled trial. Arch Intern Med. 2011;171:906–12. [DOI] [PubMed] [Google Scholar]
- 9. Fiscella K, Ransom S, Jean-Pierre P, Cella D, Stein K, Bauer JE, et al. Patient-reported outcome measures suitable to assessment of patient navigation. Cancer. 2011;117:3601–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Post DM, McAlearney AS, Young GS, Krok-Schoen JL, Plascak JJ, Paskett ED. Effects of patient navigation on patient satisfaction outcomes. J Cancer Educ. 2015;30:728–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wells KJ, Winters PC, Jean-Pierre P, Warren-Mears V, Post D, Van Duyn MA, et al. Patient navigation research program investigators. Effect of patient navigation on satisfaction with cancer-related care. Support Care Cancer. 2016;24:1729–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Harding M. Effect of nurse navigation on patient care satisfaction and distress associated with breast biopsy. Clin J Oncol Nurs. 2015;19:E15–20. [DOI] [PubMed] [Google Scholar]
- 13. Jean-Pierre P, Cheng Y, Wells KJ, Freund KM, Snyder FR, Fiscella K, et al. Satisfaction with cancer care among underserved racial-ethnic minorities and lower-income patients receiving patient navigation. Cancer. 2016;122:1060–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fillion L, de Serres M, Cook S, Goupil RL, Bairati I, Doll R. Professional patient navigation in head and neck cancer. Semin Oncol Nurs. 2009;25:212–21. [DOI] [PubMed] [Google Scholar]
- 15. Lee T, Ko I, Lee I, Kim E, Shin M, Roh S, et al. Effects of nurse navigators on health outcomes of cancer patients. Cancer Nurs. 2011;34:376–84. [DOI] [PubMed] [Google Scholar]
- 16. Tho PC, Ang E. The effectiveness of patient navigation programs for adult cancer patients undergoing treatment: a systematic review. JBI Database System Rev Implement Rep. 2016;14:295–321. [DOI] [PubMed] [Google Scholar]
- 17. Percac-Lima S, Ashburner JM, Zai AH, Chang Y, Oo SA, Guimaraes E, et al. Patient navigation for comprehensive cancer screening in high-risk patients using a population-based health information technology system: a randomized clinical trial. JAMA Intern Med. 2016;176:930–7. [DOI] [PubMed] [Google Scholar]
- 18. Freund KM, Battaglia TA, Calhoun E, Dudley DJ, Fiscella K, Paskett E, et al. National cancer institute patient navigation research program. Cancer. 2008;113:3391–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jean-Pierre P, Fiscella K, Winters PC, Post D, Wells KJ, McKoy JM, et al. Psychometric development and reliability analysis of a patient satisfaction with interpersonal relationship with navigator measure: a multi-site patient navigation research program study. Psychooncology. 2012;21:986–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Grogan S, Conner M, Norman P, Willits D, Porter I. Validation of a questionnaire measuring patient satisfaction with general practitioner services. Qual Health Care. 2000;9:210–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Marshall GN, Hays RD. The Patient Satisfaction Questionnaire Short Form (PSQ-18). Santa Monica, CA: RAND Corporation; 1994:p7865. [Google Scholar]
- 22. Atlas SJ, Zai AH, Ashburner JM, Chang Y, Percac-Lima S, Levy DE, et al. Non-visit-based cancer screening using a novel population management system. J Am Board Fam Med. 2014;27:474–85. [DOI] [PubMed] [Google Scholar]
- 23. Donelan K, Mailhot JR, Dutwin D, Barnicle K, Oo SA, Hobrecker K, et al. Patient perspectives of clinical care and patient navigation in follow-up of abnormal mammography. J Gen Intern Med. 2011;26:116–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rohan EA, Slotman B, DeGroff A, Morrissey KG, Murillo J, Schroy P. Refining the patient navigation role in a colorectal cancer screening program: results from an intervention study. J Natl Compr Canc Netw. 2016;14:1371–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jean-Pierre P, Winters PC, Clark JA, Warren-Mears V, Wells KJ, Post DM, et al. Patient navigation research program group. Do better-rated navigators improve patient satisfaction with cancer-related care? J Cancer Educ. 2013;28:527–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wender R. Cancer screening navigation: from promising practice to standard of care. JAMA Intern Med. 2016;176:937–8. [DOI] [PubMed] [Google Scholar]