Abstract
Objectives:
Death certificate data indicate that the age-adjusted death rate for pneumonia and influenza is higher in New York City than in the United States. Most pneumonia and influenza deaths are attributed to pneumonia rather than influenza. Because most pneumonia deaths occur in hospitals, we analyzed hospital discharge data to provide insight into the burden of pneumonia in New York City.
Methods:
We analyzed data for New York City residents discharged from New York State hospitals with a principal diagnosis of pneumonia, or a secondary diagnosis of pneumonia if the principal diagnosis was respiratory failure or sepsis, during 2001-2014. We calculated mean annual age-adjusted pneumonia-associated hospitalization rates per 100 000 population and 95% confidence intervals (CIs). We examined data on pneumonia-associated hospitalizations by sociodemographic characteristics and colisted conditions.
Results:
During 2001-2014, a total of 495 225 patients residing in New York City were hospitalized for pneumonia, corresponding to a mean annual age-adjusted pneumonia-associated hospitalization rate of 433.8 per 100 000 population (95% CI, 429.3-438.3). The proportion of pneumonia-associated hospitalizations with in-hospital death was 12.0%. The mean annual age-adjusted pneumonia-associated hospitalization rate per 100 000 population increased as area-based poverty level increased, whereas the percentage of pneumonia-associated hospitalizations with in-hospital deaths decreased with increasing area-based poverty level. The proportion of pneumonia-associated hospitalizations that colisted an immunocompromising condition increased from 18.7% in 2001 to 33.1% in 2014.
Conclusion:
Sociodemographic factors and immune status appear to play a role in the epidemiology of pneumonia-associated hospitalizations in New York City. Further study of pneumonia-associated hospitalizations in at-risk populations may lead to targeted interventions.
Keywords: epidemiology, hospitalization, pneumonia
Pneumonia is an acute respiratory illness with numerous infectious etiologies.1-3 Influenza virus is among the most important contributors to pneumonia, through primary pulmonary infection and secondary bacterial infection.4
During 2001-2014, pneumonia and influenza ranked as the seventh- to ninth-leading cause of death in the United States.5-8 In contrast, during this same period, pneumonia and influenza ranked as the third-leading cause of death in New York City.9,10 Furthermore, in 2014, the annual age-adjusted death rate for pneumonia and influenza was 15.1 per 100 000 population in the United States and 25.0 per 100 000 population in New York City.5,9 Most deaths for which pneumonia and influenza are listed on the death certificate in both the United States and New York City indicate pneumonia rather than influenza as the underlying cause of death, although the precipitating event of pneumonia deaths may have been influenza.11,12
The discrepancies between data in the United States and data in New York City in cause-of-death ranking and death rate for pneumonia are not well understood. One possibility for this discrepancy is the existence of artifacts, such as differences in cause-of-death reporting by physicians.13,14 However, we are not aware of data indicating that physicians in New York City are systematically more likely to code pneumonia as an underlying cause of death or are more prone to erroneous death certificate completion than physicians elsewhere in the United States.
Because most pneumonia deaths in New York City occur in hospitals, analyzing hospital discharge data can provide insights into the burden of pneumonia in New York City, including preventable factors associated with poor outcomes. The objective of our study was to examine the burden of pneumonia-associated hospitalizations in New York City to better understand the potential causes of the high death rate for pneumonia in New York City.
Methods
Data Source and Study Population
We analyzed hospital discharge data for New York City residents who were hospitalized during 2001-2014 at acute-care facilities in New York State by using the following data sets from the Statewide Planning and Research Cooperative System (SPARCS): SPARCS_MHYEPI 0714 for 2001-2009, SPARCS_MHYEPI 0615 for 2010, and SPARCS_MHYEPI_201703 for 2011-2014. SPARCS is a comprehensive all-payer data reporting system that collects discharge data from all hospitals in New York State.15 Each discharge record in SPARCS includes a principal diagnosis and up to 24 secondary diagnoses that are coded by using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes.16
Definitions
The definitions we used are consistent with a nationwide investigation of pneumonia-associated hospitalizations.17 We defined a pneumonia-associated hospitalization as a hospitalization with a principal diagnosis of pneumonia (ICD-9-CM codes 480-486, 487.0, 488.01, 488.11, or 488.81) or a secondary diagnosis of pneumonia when respiratory failure (ICD-9-CM codes 518.81, 518.82, 518.84, or 799.1) or sepsis (ICD-9-CM codes 038, 785.52, 995.91, or 995.92) was listed as the principal diagnosis.18
We considered a pneumonia-associated hospitalization to be of unspecified etiology if the principal diagnosis was either bronchopneumonia, organism unspecified (ICD-9-CM code 485) or pneumonia, organism unspecified (ICD-9-CM code 486). We considered all other pneumonia-associated hospitalizations that listed a pneumonia diagnostic code as the principal diagnosis other than ICD-9-CM codes 485 or 486 to be of specified etiology. We identified pneumonia-associated hospitalizations involving patients with an immunocompromising condition if ≥1 ICD-9-CM code for an immunocompromising condition was colisted on the discharge record.17 The study was determined to be human subjects research in which the Centers for Disease Control and Prevention (CDC) was not engaged, human subjects research that was exempt from federal regulations by the New York City Department of Health and Mental Hygiene, and human subjects research approved by the Columbia University Mailman School of Public Health.
Data Analysis
The unit of analysis was a hospitalization. We expressed mean annual and annual hospitalization rates as the number of hospitalizations per 100 000 population. We derived annual population estimates for the 5 boroughs of New York City (Bronx, Brooklyn, Manhattan, Queens, and Staten Island) from US Census Bureau data.19,20 We age-adjusted rates by using the direct method based on the 2000 US standard population. We calculated rate ratios (RRs) and 95% confidence intervals (CIs) by using Poisson regression analysis, with P < .05 considered significant.
We examined data on pneumonia-associated hospitalizations by patient sex (male, female), age group (<1, 1-4, 5-19, 20-44, 45-64, 65-74, 75-84, ≥85), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic American Indian/Alaska Native, non-Hispanic Asian/Pacific Islander, non-Hispanic other), borough (Bronx, Brooklyn, Manhattan, Queens, Staten Island), area-based poverty level (low [<10% of the federal poverty level (FPL)], medium [1%-19% FPL], high [20%-29% FPL], very high [≥30% FPL]), month of admission, in-hospital death, and colisting of immunocompromising conditions.21 We derived poverty estimates from the 2005-2012 American Community Survey.22 Some discharge records indicated unknown or missing data on sex (<0.001%) and race/ethnicity (9.2%); population estimates indicated missing data on area-based poverty level (0.19%); however, we did not adjust for unknown or missing data.
We performed multivariable Poisson regression analysis adjusted by sex, age group, race/ethnicity, borough, and area-based poverty level. Patients with missing data (8.3%) were not included. We investigated multicollinearity by using Cramer’s V, with >.30 considered significant. We conducted all analyses by using R version 3.3.3.23
Results
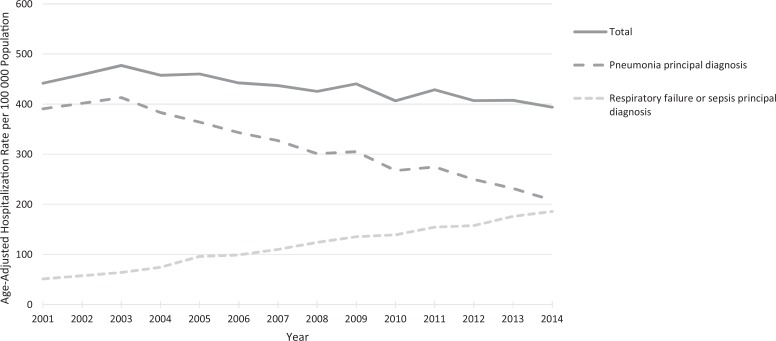
During 2001-2014, of 16 185 402 total hospitalizations for New York City residents, 495 225 (3.1%) were pneumonia-associated, corresponding to a mean annual age-adjusted pneumonia-associated hospitalization rate per 100 000 population of 433.8 (95% CI, 429.3-438.3) (Table 1). The mean annual age-adjusted rate of pneumonia-associated hospitalizations per 100 000 population declined from 459.3 (95% CI, 456.6-462.1) during 2001-2003 to 402.7 (95% CI, 400.3-405.2) during 2012-2014. The annual age-adjusted pneumonia-associated hospitalization rate in New York City declined during the study period (Figure 1). Of the 495 225 pneumonia-associated hospitalizations of New York City residents, 96.3% were at acute-care facilities in New York City and 3.7% were at acute-care facilities in New York State but not New York City.
Table 1.
Pneumonia-associated hospitalizations by demographic characteristics, New York City, 2001-2014a
| Demographic Characteristics | Pneumonia-Associated Hospitalizations, No.b | Mean Annual Age-Adjusted Pneumonia-Associated Hospitalization Rate per 100 000 Population (95% CI)c | Rate Ratio (95% CI) | Pneumonia-Associated Hospitalizations With In-Hospital Death, % | Total Hospitalizations for Any Cause, No. | Total Hospitalizations for Any Causes That Were Pneumonia-Associated, % |
|---|---|---|---|---|---|---|
| Total | 495 225 | 433.8 (429.3-438.3) | NA | 12.0 | 16 185 402 | 3.1 |
| Sex | ||||||
| Male | 239 917 | 504.8 (497.2-512.6) | 1.3 (1.3-1.3) | 11.7 | 7 065 048 | 3.4 |
| Female | 255 304 | 383.6 (378.0-389.3) | 1 [Reference] | 12.3 | 9 120 176 | 2.8 |
| Age group, y | ||||||
| <1 | 12 172 | 758.1 (744.7-771.6) | 8.8 (8.1-9.6) | 0.5 | 1 883 808 | 0.6 |
| 1-4 | 30 717 | 523.23 (517.5-529.1) | 6.1 (5.7-6.5) | 0.2 | 302 874 | 10.1 |
| 5-19 | 18 035 | 85.8 (84.5-87.1) | 1 [Reference] | 0.6 | 742 907 | 2.4 |
| 20-44 | 48 629 | 107.9 (106.9-108.8) | 1.3 (1.2-1.3) | 3.6 | 4 517 386 | 1.1 |
| 45-64 | 110 519 | 408.0 (405.6-410.4) | 4.8 (4.5-5.0) | 8.3 | 3 942 871 | 2.8 |
| 65-74 | 76 560 | 1033.4 (1026.2-1040.7) | 12.0 (11.3-12.8) | 12.9 | 1 857 532 | 4.1 |
| 75-84 | 102 265 | 2216.2 (2202.8-2229.6) | 25.8 (24.4-27.4) | 16.6 | 1 811 273 | 5.6 |
| ≥85 | 96 328 | 5037.3 (5006.4-5068.4) | 58.7 (55.3-62.3) | 22.4 | 1 126 751 | 8.5 |
| Race/ethnicity | ||||||
| Non-Hispanic white | 178 810 | 332.1 (326.2-338.2) | 1.7 (1.6-1.8) | 15.9 | 4 876 321 | 3.7 |
| Non-Hispanic black | 129 766 | 507.9 (497.5-518.4) | 2.6 (2.4-2.7) | 10.4 | 4 403 647 | 2.9 |
| Hispanic | 90 298 | 361.4 (352.2-370.9) | 1.8 (1.7-1.9) | 7.9 | 3 232 722 | 2.8 |
| Non-Hispanic American Indian/Alaska Native | 2322 | 1077.0 (915.0-1261.7) | 5.1 (4.3-6.0) | 11.9 | 87 798 | 2.6 |
| Non-Hispanic Asian/ Pacific Islander | 23 798 | 226.7 (215.7-238.2) | 1 [Reference] | 13.4 | 880 319 | 2.7 |
| Non-Hispanic other | 29 528 | 2924.5 (2791.8-3062.3) | 12.6 (11.9-13.5) | 10.7 | 1 152 845 | 2.6 |
| Borough | ||||||
| Bronx | 100 506 | 564.7 (551.6-578.0) | 1.5 (1.5-1.6) | 10.1 | 3 323 945 | 3.0 |
| Brooklyn | 145 957 | 423.6 (415.5-431.8) | 1.1 (1.1-1.2) | 12.8 | 5 011 094 | 2.9 |
| Manhattan | 86 736 | 377.4 (367.9-387.1) | 1 [Reference] | 10.2 | 2 973 536 | 2.9 |
| Queens | 129 457 | 397.5 (389.4-405.7) | 1.0 (1.0-1.1) | 13.2 | 3 957 893 | 3.3 |
| Staten Island | 32 569 | 496.3 (476.2-517.0) | 1.3 (1.2-1.4) | 14.8 | 918 934 | 3.5 |
| Area-based poverty leveld | ||||||
| Low (<10% FPL) | 80 397 | 310.2 (302.1-318.5) | 1 [Reference] | 13.9 | 2 596 652 | 3.1 |
| Medium (10%-19% FPL) | 170 055 | 418.6 (411.1-426.1) | 1.3 (1.3-1.4) | 13.3 | 5 233 152 | 3.2 |
| High (20%-29% FPL) | 128 678 | 446.7 (437.6-456.0) | 1.4 (1.4-1.5) | 11.7 | 4 129 148 | 3.1 |
| Very high (≥30% FPL) | 115 156 | 583.5 (570.6-596.7) | 1.9 (1.9-2.0) | 9.3 | 4 160 891 | 2.8 |
Abbreviations: FPL, federal poverty level; NA, not applicable.
a Data source: New York State Statewide Planning and Research Cooperative System.15
b Some numbers do not add up to total because of missing data.
c Age group rates are not age-adjusted.
d Area-based poverty level is defined as the percentage of the population in a given area whose household income is below the FPL; area is based on modified ZIP code tabulation areas.
Figure 1.
Annual age-adjusted rates of pneumonia-associated hospitalizations, New York City, 2001-2014. Data source: New York State Statewide Planning and Research Cooperative System.15
Of 495 225 pneumonia-associated hospitalizations, 360 415 (72.8%) listed a principal diagnosis of pneumonia and 134 810 (27.2%) listed a principal diagnosis of respiratory failure or sepsis (Table 2), corresponding to a mean annual age-adjusted hospitalization rate per 100 000 population of 316.1 (95% CI, 312.2-320.0) for a principal diagnosis of pneumonia and 117.7 (95% CI, 115.3-120.1) for a principal diagnosis of respiratory failure or sepsis. The rate of pneumonia-associated hospitalizations listing a principal diagnosis of pneumonia declined during the study period, whereas the rate of pneumonia-associated hospitalizations listing a principal diagnosis of respiratory failure or sepsis increased (Figure 1).
Table 2.
Pneumonia-associated hospitalizations, by disease category and ICD-9-CM code, New York City, 2001-2014a
| Disease Category (ICD-9-CM Codeb) | No. (%) |
|---|---|
| Total | 495 225 (100.0) |
| Pneumonia principal code | 360 415 (72.8) |
| Noninfluenza viral pneumonia (480) | 6154 (1.2) |
| Pneumococcal pneumonia (481) | 4794 (1.0) |
| Nonpneumococcal bacterial pneumonia (482) | 23 251 (4.7) |
| Pneumonia due to other specified organism (483) | 1729 (0.3) |
| Pneumonia in infectious diseases classified elsewhere (484) | 0 |
| Bronchopneumonia, organism unspecified (485) | 2714 (0.5) |
| Pneumonia, organism unspecified (486) | 318 959 (64.4) |
| Influenza virus (487.0, 488.01, 488.11, or 488.81) | 2814 (0.6) |
| Respiratory failure or sepsis principal code with secondary pneumonia code | 134 810 (27.2) |
| Respiratory failure (518.81, 518.82, 518.84, or 799.1) | 31 109 (6.3) |
| Sepsis (038, 785.52, 995.91, or 995.92) | 103 701 (20.9) |
Most pneumonia-associated hospitalizations listing a principal diagnosis of pneumonia were of unspecified etiology; ICD-9-CM codes 485 and 486 accounted for 321 673 (89.3%) of all such pneumonia-associated hospitalizations (Table 2).
In-Hospital Death
In-hospital death occurred in 59 596 of 495 225 (12.0%) pneumonia-associated hospitalizations during 2001-2014, ranging from 10.9% to 12.7% during the study period. The percentage of pneumonia-associated hospitalizations with in-hospital death was 11.9% (12 801 of 107 868) during 2001-2003 and 12.1% (12 637 of 104 558) during 2012-2014. The percentage of pneumonia-associated hospitalizations with in-hospital death was 5.7% (20 592 of 360 415) among hospitalizations with a principal diagnosis of pneumonia and 28.9% (39 004 of 134 810) among hospitalizations with a principal diagnosis of respiratory failure or sepsis.
Hospitalizations by Demographic Characteristics
Males had a higher mean annual age-adjusted rate of pneumonia-associated hospitalizations per 100 000 population than females (RR = 1.3; 95% CI, 1.3-1.3) (Table 1). The mean annual age-adjusted rate of pneumonia-associated hospitalizations decreased for both males and females from 2001-2003 to 2012-2014 (Table 3).
Table 3.
Pneumonia-associated hospitalizations, by demographic characteristics of patients and years of hospitalization, New York City, 2001-2014a
| Characteristic | 2001-2003 Mean Annual Age-Adjusted Hospitalization Rate per 100 000 Population (95% CI)b | 2012-2014 Mean Annual Age-Adjusted Hospitalization Rate per 100 000 Population (95% CI)b | Rate Ratio (95% CI)c |
|---|---|---|---|
| Total | 459.3 (456.6-462.1) | 402.7 (400.3-405.2) | 0.9 (0.9-0.9) |
| Sex | |||
| Male | 531.8 (527.1-536.6) | 472.8 (468.6-476.9) | 0.9 (0.9-0.9) |
| Female | 409.0 (405.6-412.4) | 353.4 (350.4-356.5) | 0.9 (0.8-0.9) |
| Age group, y | |||
| <1 | 932.4 (900.8-964.7) | 508.6 (485.4-532.6) | 0.5 (0.5-0.6) |
| 1-4 | 546.9 (534.0-560.0) | 431.5 (420.3-442.8) | 0.8 (0.7-0.8) |
| 5-19 | 85.0 (82.4-87.7) | 79.7 (77.0-82.4) | 0.9 (0.9-1.0) |
| 20-44 | 127.3 (125.0-129.5) | 90.7 (88.8-92.6) | 0.7 (0.7-0.7) |
| 45-64 | 392.0 (386.7-397.4) | 415.3 (410.2-420.4) | 1.1 (1.0-1.1) |
| 65-74 | 1077.2 (1060.7-1093.9) | 982.1 (967.6-996.7) | 0.9 (0.9-0.9) |
| 75-84 | 2298.8 (2269.5-2328.4) | 2118.8 (2090.4-2147.5) | 0.9 (0.9-1.0) |
| ≥85 | 5802.1 (5726.9-5877.9) | 4471.0 (4411.5-4531.0) | 0.8 (0.7-0.8) |
| Race/ethnicity | |||
| Non-Hispanic white | 350.5 (347.0-354.0) | 295.1 (291.9-298.5) | 0.8 (0.8-0.9) |
| Non-Hispanic black | 512.1 (506.0-518.3) | 464.7 (459.1-470.3) | 0.9 (0.9-1.0) |
| Hispanic | 335.9 (330.2-341.7) | 342.8 (338.1-347.6) | 1.1 (1.0-1.1) |
| Non-Hispanic American Indian/Alaska Native | 702.4 (619.6-797.2) | 498.4 (436.0-567.9) | 0.7 (0.5-0.9) |
| Non-Hispanic Asian/Pacific Islander | 221.2 (213.7-229.0) | 206.2 (200.9-211.7) | 1.0 (0.9-1.1) |
| Non-Hispanic other | 2071.7 (2001.8-2143.7) | 4728.8 (4637.2-4821.9) | 2.2 (2.1-2.4) |
| Borough | |||
| Bronx | 561.2 (553.4-569.0) | 538.7 (531.6-545.9) | 1.0 (1.0-1.0) |
| Brooklyn | 461.7 (456.8-466.7) | 383.0 (378.6-387.4) | 0.8 (0.8-0.9) |
| Manhattan | 413.2 (407.3-419.1) | 333.9 (328.9-339.0) | 0.8 (0.8-0.8) |
| Queens | 409.4 (404.6-414.3) | 386.7 (382.2-391.2) | 0.9 (0.9-1.0) |
| Staten Island | 581.2 (568.1-594.4) | 427.6 (417.2-438.2) | 0.7 (0.7-0.8) |
| Area-based poverty leveld | |||
| Low (<10% FPL) | 332.5 (327.5-337.5) | 269.8 (265.5-274.2) | 0.8 (0.8-0.9) |
| Medium (10%-19% FPL) | 433.9 (429.4-438.4) | 411.2 (406.9-415.6) | 1.0 (0.9-1.0) |
| High (20%-29% FPL) | 480.0 (474.2-486.0) | 374.3 (370.0-378.8) | 0.8 (0.8-0.8) |
| Very high (≥30% FPL) | 595.5 (588.4-602.6) | 582.1 (574.8-589.5) | 1.0 (1.0-1.0) |
| Pneumonia principal diagnosis | 401.8 (399.2-404.3) | 229.5 (227.6-231.4) | 0.6 (0.6-0.6) |
| Respiratory failure or sepsis principal diagnosis with secondary pneumonia diagnosis | 57.6 (56.6-58.5) | 173.2 (171.6-174.8) | 3.0 (2.9-3.1) |
Abbreviation: FPL, federal poverty level.
a Data source: New York State Statewide Planning and Research Cooperative System.15
b Age group rates are not age-adjusted.
c Reference group: 2001-2003.
d Area-based poverty level is defined as the percentage of the population in a given area whose household income is below the FPL; area is based on modified ZIP code tabulation areas.
Mean annual rates of pneumonia-associated hospitalization were highest among patients aged <1 year and among patients aged ≥65 (Table 1). Mean annual rates of pneumonia-associated hospitalizations declined significantly for all age groups from 2001-2003 to 2012-2014 except for patients aged 5-19, 45-64, and 75-84 (Table 3). The percentage of pneumonia-associated hospitalizations with in-hospital deaths was highest for patients aged ≥65.
Non-Hispanic other, non-Hispanic American Indian/Alaska Native, and non-Hispanic black patients had a higher mean annual age-adjusted pneumonia-associated hospitalization rate than did Hispanic, non-Hispanic Asian/Pacific Islander, and non-Hispanic white patients (Table 1). The percentage of pneumonia-associated hospitalizations with in-hospital deaths was highest among non-Hispanic white patients (15.0%) and lowest among Hispanic patients (7.9%).
By borough, the Bronx had the highest mean annual age-adjusted pneumonia-associated hospitalization rate per 100 000 population (564.7; 95% CI, 551.6-578.0), and Manhattan had the lowest (377.4; 95% CI, 367.9-387.1) (Table 1). However, the Bronx had the lowest percentage of pneumonia-associated hospitalizations with in-hospital deaths (10.1%) and Staten Island had the highest (14.8%). The mean annual age-adjusted pneumonia-associated hospitalization rate decreased significantly from 2001-2003 to 2012-2014 for Brooklyn (RR = 0.8; 95% CI, 0.8-0.9), Manhattan (RR = 0.8; 95% CI, 0.8-0.8), and Staten Island (RR = 0.7; 95% CI, 0.7-0.8) (Table 3).
The mean annual age-adjusted pneumonia-associated hospitalization rate per 100 000 population increased as area-based poverty level increased, whereas the percentage of pneumonia-associated hospitalizations with in-hospital deaths decreased with increasing area-based poverty level (Table 1). Furthermore, the mean age at death during a pneumonia-associated hospitalization decreased significantly as area-based poverty level increased, from 79.4 years in areas with low poverty levels to 72.1 years in areas with very high poverty levels (P < .001).
Multivariable Poisson Regression
After adjusting for other variables, the mean annual rates of pneumonia-associated hospitalizations were highest among patients aged <1 year (RR = 8.6; 95% CI, 7.8-9.4), 1-4 (RR = 5.8; 95% CI, 5.4-6.3), 45-64 (RR = 4.9; 95% CI, 4.6-5.2), 65-74 (RR = 13.7; 95% CI, 12.9-14.6), 75-84 (RR = 30.7; 95% CI, 28.8-32.7), and ≥85 (RR = 74.7; 95% CI, 70.1-79.6) compared with patients aged 5-19. Mean annual age-adjusted rates of pneumonia-associated hospitalization were highest among non-Hispanic American Indian/Alaska Native patients (RR = 7.6; 95% CI, 6.5-9.0) and non-Hispanic other patients (RR = 12.1; 95% CI, 11.3-12.9) compared with non-Hispanic Asian/Pacific Islander patients. Of all 5 boroughs, Staten Island (RR = 1.5; 95% CI, 1.5-1.6) had the highest mean annual age-adjusted rate of pneumonia-associated hospitalizations compared with Manhattan. The mean annual age-adjusted rates of penumonia-associated hospitalizations were highest among those who resided in high poverty areas (RR = 1.3; 95% CI, 1.2-1.3) and very high poverty areas (RR = 1.3; 95% CI, 1.3-1.4) compared with low poverty areas. We found no significant multicollinearity between race/ethnicity and area-based poverty level (Cramer’s V = 0.24) or between race/ethnicity and borough (Cramer’s V = 0.18).
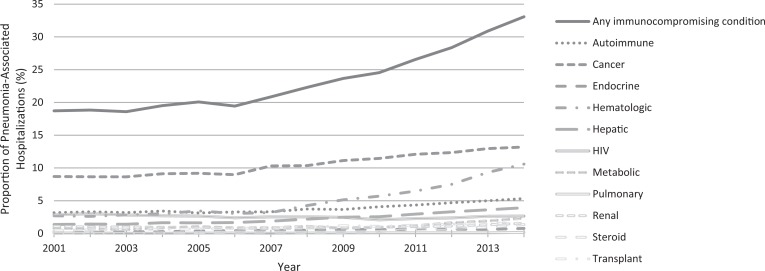
Hospitalizations by Immune Status and Secondary Diagnoses
During 2001-2014, the percentage of pneumonia-associated hospitalizations that colisted an immunocompromising condition increased significantly from 18.7% in 2001 to 33.1% in 2014 (P < .001) (Figure 2). The percentage difference between pneumonia-associated hospitalizations with in-hospital death among patients whose discharge data colisted an immunocompromising condition (21.4%) and patients whose discharge data did not colist an immunocompromising condition (11.5%) was significant (P < .001). During 2001-2003, a median of 3.0 secondary diagnoses were listed on the discharge record for any hospitalization (not just pneumonia-associated hospitalizations) in New York City, and this median increased to 6.0 during 2012-2014 (P < .001).
Figure 2.
Proportion of pneumonia-associated hospitalizations colisting an immunocompromising condition, New York City, 2001-2014. Data source: New York State Statewide Planning and Research Cooperative System.15
Seasonality
Age-adjusted rates of pneumonia-associated hospitalizations were highest during January, followed by December. The proportion of pneumonia-associated hospitalizations with in-hospital death was highest for the admission month of August (13.5%) and lowest for the admission month of December (11.5%).
Discussion
Our study replicates a 2018 study of the burden of pneumonia-associated hospitalizations in the United States, and comparisons can be made given similarities in the methodology.17 We found that the mean annual age-adjusted rate of pneumonia-associated hospitalizations, both overall and for subgroups, was often similar between New York City and the United States. For example, the mean annual age-adjusted rate of pneumonia-associated hospitalizations per 100 000 population in New York City during 2001-2014 (433.8) was similar to the rate in the United States (464.8). However, the percentage of in-hospital deaths among patients with pneumonia-associated hospitalizations was higher in New York City (12.0%) than in the United States (7.4%). The higher percentage of in-hospital deaths in New York City was seen for both sexes, all racial/ethnic groups, and most age groups.
Our analysis adds to evidence from death certificates suggesting that pneumonia mortality in New York City is higher than pneumonia mortality in the United States.12 To our knowledge, hospital discharge data are generated independently of death certificate data. If so, two separate data sources (hospital discharge data and death certificate data) suggest a disproportionate burden of pneumonia mortality in New York City. Although the data in our study do not definitively prove that there is a disproportionate burden of pneumonia mortality in New York City, they can help guide future investigations.
Pneumonia mortality is a function of the risk of acquiring pneumonia multiplied by the risk of a poor outcome (ie, death) from pneumonia. If we use “pneumonia-associated hospitalization” as a proxy for “pneumonia,” then the data in our study along with the nationwide data suggest that the risk of having pneumonia is similar in New York City and the United States.17 It is unlikely that New York City’s higher reported rates of pneumonia mortality reflect a greater risk of acquiring pneumonia in New York City than in the United States.
If we shift our focus to the risk of a poor outcome (ie, death) from pneumonia, data in our study suggest a higher risk of a poor outcome during a pneumonia-associated hospitalization in New York City than in the United States.17 It is important to acknowledge that we do not know that pneumonia mortality is worse in New York City than in the United States. Our observations might be due to differences in coding practices or an unrecognized artifact in the data. An important next step will be to verify the quality of hospital discharge data (and death certificate data) for pneumonia in New York City. If these data prove to be reliable, then true epidemiologic differences in pneumonia may exist between New York City and the United States, such as higher rates of antimicrobial resistance, less access to health care, or lower quality of health care in New York City. Additional investigation into differences between patients discharged after a pneumonia-associated hospitalization in New York City and patients discharged after a pneumonia-associated hospitalization in the United States is also needed, because these differences might affect reported mortality.
In New York City, the percentage of pneumonia-associated hospitalizations with in-hospital deaths was lower among patients who had a principal diagnosis of pneumonia (5.7%) than among patients with a principal diagnosis of respiratory failure or sepsis (28.9%), whereas in the United States, these percentages were 3.9% and 19.0%, respectively. Presumably, pneumonia-associated hospitalizations with a principal diagnosis of respiratory failure or sepsis represent more severe forms of pneumonia, and these appear to be driving pneumonia mortality in New York City. Thus, the sepsis regulations in New York State, issued in 2013, may have an effect on pneumonia mortality in New York City, especially because pneumonia is one of the most common causes of sepsis in New York State.24,25
Although the quality of data on race/ethnicity in SPARCS has been questioned before, we did find differences in rates of pneumonia-associated hospitalization by race/ethnicity that deserve further investigation. The higher rate may reflect underlying health inequities in New York City, such as conditions that increase the risk of pneumonia (eg, diabetes, obesity, asthma).26 Efforts to address chronic diseases across the general New York City population might therefore affect rates of pneumonia-associated hospitalizations.
Increases in area-based poverty level were also associated with increases in the rate of pneumonia-associated hospitalizations, consistent with previous data on economic status and rate of pneumonia-associated hospitalizations and pneumonia death rate.12,17 It was therefore surprising that Staten Island had the highest rate of pneumonia-associated hospitalizations among all 5 boroughs, because Staten Island also has the second-highest median household income among all 5 boroughs.27 We suspect that the findings in Staten Island reflect unknown artifacts, as hypothesized in an examination of the surprisingly high pneumonia death rate in Staten Island published in 2018, such as systematic differences in cause-of-death reporting among the boroughs.12
The percentage of pneumonia-associated hospitalizations that colisted an immunocompromising condition increased in New York City during the study period, and these data suggest a target population for prevention efforts. This trend is not limited to New York City. The percentage of pneumonia-associated hospitalizations that colisted an immunocompromising condition in the United States increased from 18.7% in 2001 to 29.9% in 2014.17 We suspect that the increase in colisting of immunocompromising conditions partially reflects changes in discharge coding practices. Specifically, in both New York City and the United States, the median number of secondary diagnoses listed on the discharge record of any hospitalization (not just pneumonia-associated hospitalizations) has increased over time. In New York City, during 2001-2003, a median of 3.0 secondary diagnoses were listed on the discharge record for any hospitalization, which increased to 6.0 during 2012-2014. In the United States, the median number of secondary diagnoses listed on the discharge record for any hospitalization increased from 3.8 to 7.5 during these same 2 periods.17 These data also indicate that in any given year, the median number of secondary diagnoses listed on the discharge record does not differ greatly between New York City and the United States. If we use the median number of secondary diagnoses on the discharge record as an indicator of a patient’s general level of health, it suggests that patients in New York City have a similar general level of health as patients in the United States. Thus, the higher percentage of in-hospital deaths during a pneumonia-associated hospitalization in New York City compared with the United States is unlikely to be explained by differences in the general level of health of patients in New York City compared with the United States.
Limitations
This study had several limitations. First, the unit of analysis in this study was a hospitalization rather than a patient. Thus, patients who were readmitted for the same episode of pneumonia were treated as having unique pneumonia-associated hospitalizations. Second, we likely underestimated the burden of pneumonia in New York City because we only used inpatient data rather than a combination of inpatient and outpatient data.28,29 Third, we were unable to determine whether the threshold for admitting patients with pneumonia was different in New York City than elsewhere. Differing thresholds of admission could have biased the percentage of in-hospital deaths, because a higher threshold of admission would admit patients who had a higher chance of death. Fourth, our study did not account for the various settings of pneumonia acquisition; therefore, the data likely represented a mix of community-acquired pneumonia, health care-associated pneumonia, hospital-acquired pneumonia, and ventilator-associated pneumonia.30 We also did not include pneumonia due to aspiration, an important cause of pneumonia with high mortality rates, which should be investigated.
Fifth, discharge coding, the basis for analyses using SPARCS, can be subject to bias. Our inclusion of respiratory failure and sepsis in our definition of a pneumonia-associated hospitalization addressed a previously reported bias, but other biases may not have been accounted for (eg, the change to the inpatient prospective payment system by the Centers for Medicare & Medicaid Services in 2008).18,31,32 Sixth, using ICD-9-CM codes to identify pneumonia was imperfect, and we did not verify the accuracy of discharge records in SPARCS.31 Finally, because our analysis did not adjust for missing data, the results from our multivariable analysis may have been biased.
Conclusions
This study offers insight into the burden of pneumonia in New York City. Sociodemographic factors and immune status appear to play a strong role in the epidemiology of pneumonia-associated hospitalizations in New York City. Further investigation is needed into the underlying reasons for why pneumonia mortality might be higher in New York City than elsewhere.
Acknowledgments
The authors thank Dana Haberling, MSPH, and Alicia Fry, MD, MPH, of the Centers for Disease Control and Prevention (CDC) for their assistance in developing this study. The findings and conclusion in this article are those of the authors and do not necessarily represent the official position of CDC or the New York City Department of Health and Mental Hygiene.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Epi Scholars program.
References
- 1. World Health Organization. Pneumonia. 2016. http://www.who.int/mediacentre/factsheets/fs331/en . Accessed July 20, 2018.
- 2. Centers for Disease Control and Prevention. Pneumonia. Page updated August 2017 https://www.cdc.gov/pneumonia. Accessed July 20, 2018.
- 3. Ruiz M, Ewig S, Marcos MA, et al. Etiology of community-acquired pneumonia: impact of age, comorbidity, and severity. Am J Respir Crit Care Med. 1999;160(2):397–405. [DOI] [PubMed] [Google Scholar]
- 4. Jain S, Self WH, Wunderink RG, et al. Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med. 2015;373(5):415–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. National Center for Health Statistics. Health, United States, 2015: with special feature on racial and ethnic health disparities. Updated June 2017 https://www.cdc.gov/nchs/data/hus/hus15.pdf#019. Accessed July 20, 2018. [PubMed]
- 6. Anderson RN, Smith BL. Deaths: leading causes for 2001. Natl Vital Stat Rep. 2003;52(9):1–86. [PubMed] [Google Scholar]
- 7. Heron M. Deaths: leading causes for 2014. Natl Vital Stat Rep. 2016;65(5):1–96. [PubMed] [Google Scholar]
- 8. Heron M. Deaths: leading causes for 2010. Natl Vital Stat Rep. 2013;62(6):1–97. [PubMed] [Google Scholar]
- 9. New York State Department of Health. Leading causes of deaths, New York State, 2008-2015. January 2018. https://apps.health.ny.gov/public/tabvis/PHIG_Public/lcd/reports/#state. Accessed July 20, 2018.
- 10. New York City Department of Health and Mental Hygiene. EpiQuery mortality module. 2017. https://a816-healthpsi.nyc.gov/epiquery/VS/index.html . Accessed July 20, 2018.
- 11. American Lung Association, Epidemiology and Statistics Unit, Research and Health Education Division. Trends in pneumonia and influenza morbidity and mortality. 2015. http://www.lung.org/assets/documents/research/pi-trend-report.pdf. Accessed July 20, 2018.
- 12. Cordoba E, Maduro G, Huynh M, Varma JK, Vora NM. Deaths from pneumonia—New York City, 1999-2015. Open Forum Infect Dis. 2018;5(2):ofy020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wexelman BA, Eden E, Rose KM. Survey of New York City resident physicians on cause-of-death reporting, 2010. Prev Chronic Dis. 2013;10:E76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. German RR, Fink AK, Heron M, et al. The accuracy of cancer mortality statistics based on death certificates in the United States. Cancer Epidemiol. 2011;35(2):126–131. [DOI] [PubMed] [Google Scholar]
- 15. New York State Department of Health. Statewide Planning and Research Cooperative System (SPARCS). Revised 2018 https://www.health.ny.gov/statistics/sparcs. Accessed July 20, 2018.
- 16. Center for Disease Control and Prevention. International classification of diseases, ninth revision, clinical modification (ICD-9-CM). Updated 2013 https://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed July 20, 2018.
- 17. Hayes BH, Haberling DL, Kennedy J, Varma JK, Fry AM, Vora NM. Burden of pneumonia-associated hospitalizations—United States, 2001-2014. Chest. 2018;153(2):427–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lindenauer PK, Lagu T, Shieh MS, Pekow PS, Rothberg MB. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003-2009. JAMA. 2012;307(13):1405–1413. [DOI] [PubMed] [Google Scholar]
- 19. Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People 2010 Stat Notes. 2001;20:1–10. [PubMed] [Google Scholar]
- 20. New York City Department of Health and Mental Hygiene. NYC DOHMH Population Estimates, Modified From the US Census Bureau Interpolated Intercensal Population Estimates, 2000-2016. New York: New York City Department of Health and Mental Hygiene; 2017. [Google Scholar]
- 21. Toprani A, Hadler JL. Selecting and Applying a Standard Area-Based Socioeconomic Status Measure for Public Health Data: Analysis for New York City. New York: New York City Department of Health and Mental Hygiene; 2013. http://www1.nyc.gov/assets/doh/downloads/pdf/epi/epiresearch-SES-measure.pdf. Accessed July 20, 2018. [Google Scholar]
- 22. US Census Bureau. American Community Survey. 2018. https://www.census.gov/acs/www/data/data-tables-and-tools/index.php. Accessed July 20, 2018.
- 23. R Development Core Team. R software. Vienna, Austria: R Foundation for Statistical Computing; 2008. [Google Scholar]
- 24. Novosad SA, Sapiano MRP, Grigg C, et al. Vital signs: epidemiology of sepsis: prevalence of health care factors and opportunities for prevention. MMWR Morb Mortal Wkly Rep. 2016;65(33):864–869. [DOI] [PubMed] [Google Scholar]
- 25. Seymour CW, Gesten F, Prescott HC, et al. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017;376(23):2235–2244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Santibanez TA, Lu PJ, O’Halloran A, Meghani A, Grabowsky M, Singleton JA. Trends in childhood influenza vaccination coverage—U.S., 2004-2012. Public Health Rep. 2014;129(5):417–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. US Census Bureau. QuickFacts: New York County (Manhattan Borough), New York: 2018. https://www.census.gov/quickfacts/fact/map/newyorkcountymanhattanboroughnewyork/INC110216. Accessed July 20, 2018. [Google Scholar]
- 28. Jackson ML, Neuzil KM, Thompson WW, et al. The burden of community-acquired pneumonia in seniors: results of a population-based study. Clin Infect Dis. 2004;39(11):1642–1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Weiss K, Tillotson GS. The controversy of combination vs monotherapy in the treatment of hospitalized community-acquired pneumonia. Chest. 2005;128(2):940–946. [DOI] [PubMed] [Google Scholar]
- 30. Corrado RE, Lee D, Lucero DE, Varma JK, Vora NM. Burden of adult community-acquired, healthcare-associated, hospital-acquired, and ventilator-associated pneumonia: New York City, 2010 to 2014. Chest. 2017;152(5):930–942. [DOI] [PubMed] [Google Scholar]
- 31. National Center for Health Statistics, Centers for Medicare & Medicaid Services. Conversion table of new ICD-9-CM codes, 2013. https://www.cdc.gov/nchs/data/icd/icd-9-cm_fy14_cnvtbl_final.pdf. 2013. Accessed July 20, 2018.
- 32. Centers for Medicare & Medicaid Services, US Department of Health and Human Services. Medicare program: changes to the hospital inpatient prospective payment systems and fiscal year 2009 rates; payments for graduate medical education in certain emergency situations; changes to disclosure of physician ownership in hospitals and physician self-referral rules; updates to the long-term care prospective payment system; updates to certain IPPS-excluded hospitals; and collection of information regarding financial relationships between hospitals; final rule. Fed Regist. 2008;73(161):48433–49084. [PubMed] [Google Scholar]