Abstract
Objectives:
Characterization of the epidemiology and cost of lawn-mower injuries is potentially useful to inform injury prevention and health policy efforts. We examined the incidence, distribution, types and severity, and emergency department (ED) and hospitalization charges of lawn-mower injuries among all age groups across the United States.
Methods:
This retrospective, cross-sectional study used nationally representative, population-based (all-payer) data from the US Nationwide Emergency Department Sample for lawn-mower–related ED visits and hospitalizations from January 1, 2006, through December 31, 2013. Lawn-mower injuries were identified by using International Classification of Diseases, Ninth Revision, Clinical Modification code E920 (accidents caused by a powered lawn mower). We analyzed data on demographic characteristics, age, geographic distribution, type of injury, injury severity, and hospital charges.
Results:
We calculated a weighted estimate of 51 151 lawn-mower injuries during the 8-year study period. The most common types of injuries were lacerations (n = 23 907, 46.7%), fractures (n = 11 433, 22.4%), and amputations (n = 11 013, 21.5%). The most common injury locations were wrist or hand (n = 33 477, 65.4%) and foot or toe (n = 10 122, 19.8%). Mean ED charges were $2482 per patient, and mean inpatient charges were $36 987 per patient. The most common procedures performed were wound irrigation or debridement (n = 1436, 29.9%) and amputation (n = 1230, 25.6%).
Conclusions:
Lawn-mower injuries occurred at a constant rate during the study period. Changes to nationwide industry safety standards are needed to reduce the frequency and severity of these preventable injuries.
Keywords: epidemiology, burden of disease, public health, emergency care, noncommunicable disease, morbidity and mortality trends, lawn-mower injuries
Lawn-mower accidents in the United States result in harm to children and adults, despite longstanding awareness and recognition of the problem and current industry injury-prevention standards.1,2 Several studies have estimated the rate of injuries in adults and children during various time intervals. For example, in a study of adults during 1996-2004, the lawn-mower injury incidence rate was estimated at 20-30 per 100 000 population.3 In a study of lawn-mower injuries among children during 1990-2013, the incidence rate was estimated at 10 per 100 000 population, and it remained steady during the study period.4,5 Another study of lawn-mower injuries among children during 1990-2104 showed a slightly decreasing annual rate.6 Other studies reported the types of injuries, including lacerations (25%-40%), soft-tissue injuries (20%-30%), fractures (8%-10%), burns (5%-15%), and amputations (3%-5%).3,4,7 The most frequently injured body parts were the hands and fingers (14.7%-34.6%), the lower extremity (14.7%-18.9%), and the foot or toe (11.5%-17.7%).4,5,7
Lawn-mower injuries are often severe and result in substantial preventable morbidity and cost to the health care system. A study of the Kids’ Inpatient Database estimated $21.6 million in hospital charges for pediatric amputation injuries in 2003.8 Another study of pediatric lower-extremity amputees from 1980-2000 estimated annual prosthetic costs ranging from $43.9 million to $75.4 million.9
Most estimates rely on data from the National Electronic Injury Surveillance System (NEISS), which is maintained by the US Consumer Product Safety Commission.10 This publicly available national database collects data from participating NEISS hospitals on injuries associated with consumer products. It is somewhat limited by a relatively small sample size (data came from 96 hospitals in 2015) and the type of data recorded. The small sample size results in less accurate national estimates than estimates obtained with a larger sample and an inability to present stratified results. Information about costs of injuries is also not included.
The Nationwide Emergency Department Sample (NEDS) is a national database of the Healthcare Utilization Project (HCUP) that provides data from 945 hospitals in 33 states, comprising a 20% stratified sample of US hospitals.11 Data on more than 100 clinical and nonclinical variables are collected, providing valuable information on disease processes and injuries. The objective of this study was to describe the incidence, distribution, types and severity, and emergency department (ED) and hospitalization charges of lawn-mower injuries among all age groups across the United States. We hypothesized that injury patterns would be similar to patterns described in previous studies and would provide new information about charges, procedures performed, and patient demographic characteristics for these types of injuries.
Methods
Data Source
HCUP is sponsored by the Agency for Healthcare Research and Quality and industry partners and consists of several databases that are the product of numerous health care data collection efforts.12 One such database, NEDS, is the largest all-payer ED database in the United States. NEDS captures data on 25-30 million ED visits annually, comprising about 20% of estimated ED visits in the United States. When weighted, these data allow for national estimates of clinical data on ED visits, and the database has been shown to provide similar estimates of injury frequency as other large national databases.11,13 All data are de-identified, and no patient identifiers are available. We searched the NEDS database for data on ED visits and hospitalizations containing the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code E920 (accidents caused by a powered lawn mower)14 from January 1, 2006, through December 31, 2013.
Measures
We collected data on the demographic characteristics of patients who visited the ED because of a lawn-mower injury. We collected data on age (grouped into the following categories: 0-4, 5-9, 10-14, 15-19, 20-29, 30-39, 40-49, 50-69, and ≥70 years) and sex (male, female). To assess the distribution of lawn-mower injuries by geography, we collected data on the patient’s county of residence. Each county of residence was classified into 1 of 6 categories according to a classification scheme developed by the National Center for Health Statistics. The categories separate counties by level of urbanization and differentiate between central, urban counties of large metropolitan areas (ie, inner cities), and more peripheral rural counties (suburbs). The 6 categories were large central metropolitan, large fringe metropolitan, medium metropolitan, small metropolitan, micropolitan nonmetropolitan, and noncore nonmetropolitan.15
We also collected data on whether the ED visit occurred on a Saturday or Sunday, the month of the visit grouped into quarters (January-March, April-June, July-September, October-December), and the region of the country where the hospital was located (Northeast, Midwest, South, West). We analyzed data on the number of medical conditions listed in the patient record by using the Charlson Comorbidity Index. The Charlson Comorbidity Index is a method of characterizing patient comorbidity using ICD-9-CM codes. The system identifies 17 comorbidities and assigns each one a weight (from 1 to 6) based on the risk of mortality; these weights are then summed to create a score. A score of 0 indicates that the patient has no comorbidities; higher scores indicate more severe comorbid disease and a greater risk of mortality.16,17
We classified body region of injury by using the Barell Injury Diagnosis Matrix, a tool for standardizing the description of injury type and body region of injury using ICD-9-CM codes.18 We also computed Injury Severity Scores (ISSs). The ISS is the sum of the squares of the Abbreviated Injury Scale (AIS) scores of the 3 most severe injuries. The AIS ranges from 1 (minor) to 6 (maximally severe, currently untreatable) by classifying injuries according to the probability of mortality. Any patient with an injury of AIS 6 severity automatically generates an ISS of 75; otherwise, the scores are summed as indicated previously. Accordingly, the ISS is a discontinuous variable that can range from 1 to 75; an ISS ≥9 is considered severe.19
We collected data on the types of surgical procedures performed. We reviewed principal procedure codes and categorized them into one of the following types of surgical procedures: amputation, wound irrigation and/or debridement, reduction and/or fixation, skin and soft-tissue grafting, muscle and/or tendon repair, other orthopedic procedure (not otherwise specified), digit and or/limb reattachment, ophthalmologic, or “other.”
We collected data on the disposition of the patient if discharged alive from the ED (home, inpatient admission, admission to another facility, miscellaneous), the disposition if discharged alive from a hospital stay (home, transfer to another facility, home health care, miscellaneous), the number of inpatient procedures performed, the principal procedure performed as recorded in the inpatient record, and length of hospital stay (in days). Finally, we collected the following data on hospital charges (as described previously): total and mean charges for ED visits and total and mean inpatient charges. We adjusted charges for inflation by using the Consumer Price Index.20
Data Analysis
We applied weights provided by HCUP to obtain estimates of national incidence of lawn-mower injuries for all ages during the study period. To calculate the denominator, we used US Census data from July 1, 2010.21 To analyze the body region of injury, we recoded Barell Injury Diagnosis Matrix locations into the following categories: head/neck, eye/face, torso, upper extremity, wrist/hand, lower extremity, foot/toe, and other. We grouped injury types as amputations, burns, fractures, lacerations, soft tissue, and other. We stratified these categories by age group for adults and children. We conducted statistical analyses by using Stata/MP version 14.2 using standard descriptive statistical methods.22 The Johns Hopkins Institutional Review Board reviewed and approved the study methods.
Results
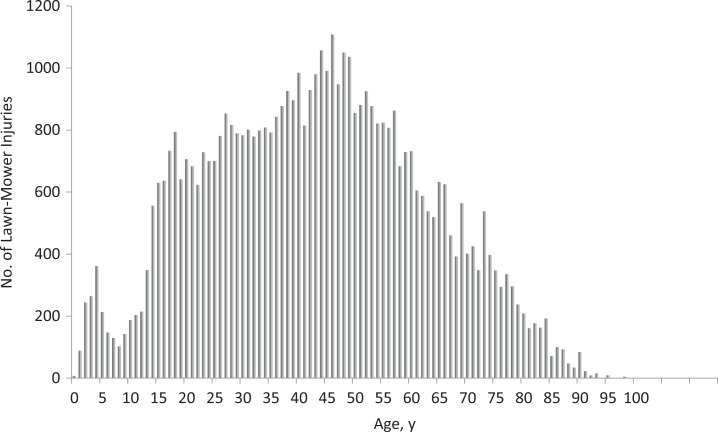
We identified 14 878 patients with lawn-mower injuries during 2006-2013. We determined a national estimate of 51 151 cases (95% confidence interval [CI], 49 422-52 879) and an average of 6394 cases annually (Table 1). The estimated annual incidence of lawn-mower injuries per 100 000 person-years decreased slightly from 2.3 (95% CI, 2.1-2.5) in 2006 to 1.8 (95% CI, 1.6-2.0) in 2013. In general, lawn-mower injuries in the pediatric population were clustered among children aged 0-4 (n = 965; 95% CI, 813-1116) and teenagers aged 15-19 (n = 3433; 95% CI, 3155-3711) (Figure).
Table 1.
National estimates of characteristics of lawn-mower injury cases in the United States, based on data from 14 878 patients in the Nationwide Emergency Department Sample, 2006-2013a
| Characteristic | Weighted Estimate of Lawn-Mower Injury Cases, No. (95% CI) [%]b | US Population, 2010 Census (%)c,d |
|---|---|---|
| Total | 51 151 (49 422-52 879) [100.0] | 308 745 538 (100.0) |
| Sex | ||
| Male | 43 567 (42 060-45 074) [85.2] | 151 781 326 (49.2) |
| Female | 7584 (7098-8070) [14.8] | 156 964 212 (50.8) |
| Patient county of residence, NCHS urban–rural codee | ||
| Large central metropolitan | 8110 (7461-8759) [15.8] | (30.5)f |
| Large fringe metropolitan | 11 836 (11 059-12 614) [23.1] | (24.7) |
| Medium metropolitan | 11 614 (10 752-12 477) [22.7] | (20.9) |
| Small metropolitan | 5832 (5149-6515) [11.4] | (9.2) |
| Micropolitan nonmetropolitan | 7094 (6571-7618) [13.9] | (8.7) |
| Noncore nonmetropolitan | 6421 (5923-6920) [12.6] | (6.1) |
| Missing | 244 [0.5] | — |
| Visit occurred on a Saturday or Sunday | ||
| No | 33 886 (32 619-35 153) [66.3] | — |
| Yes | 17 260 (16 514-18 006) [33.7] | — |
| Missing | —g | — |
| Visit quarter | ||
| January-March | 3048 (2714-3384) [6.8] | — |
| April-June | 19 951 (19 057-20 844) [44.4] | — |
| July-September | 16 735 (15 947-17 524) [37.3] | — |
| October-December | 5185 (4755-5616) [11.5] | — |
| Missing | 6230 (5510-6951) [12.2] | — |
| Hospital region | ||
| Northeast | 10 644 (9881-11 407) [20.8] | 55 317 240 (17.9) |
| Midwest | 15 305 (14 352-16 257) [29.9] | 66 927 001 (21.7) |
| South | 19 162 (18 055-20 270) [37.5] | 114 555 744 (37.1) |
| West | 6040 (5520-6560) [11.8] | 71 945 553 (23.3) |
| Charlson Comorbidity Indexh | ||
| 0 | 47 341 (45 724-48 958) [92.6] | — |
| 1 | 3217 (2930-3505) [6.3] | — |
| ≥2 | 592 (489-696) [1.1] | — |
| Injury Severity Score (ISS)i | — | |
| 1 | 28 643 (27 073-29 397) [55.4] | — |
| <4 | 35 994 (34 649-37 339) [70.6] | — |
| ≥4 and <9 | 14 128 (13 446-14 810) [27.7] | — |
| ≥9 and <15 | 761 (622-900) [1.5] | — |
| ≥15 | 65 (27-103) [0.1] | — |
| ED disposition if discharged alive | ||
| Home | 43 222 (41 648-44 795) [84.5] | — |
| Inpatient admission | 4809 (4423-5194) [9.4] | — |
| Transfer to another facility | 2335 (2071-2598) [4.5] | — |
| Miscellaneous | 774 (565-984) [1.5] | — |
| Charges, $j | ||
| Total ED charges | 113 million (107 million-119 million) | — |
| Charge per ED visit, mean | 2482 (2379-2585) | — |
| Total inpatient charges | 177 million (152 million-202 million) | — |
| Inpatient charge per stay, mean | 36 987 (33 065-40 909) | — |
| Hospital length of stay, median (mean) [95% CI] | 2 (3.9) (3.5-4.3) | — |
| Inpatient disposition if discharged alive | ||
| Home | 3939 (3602-4276) [82.0] | — |
| Transfer to another facility | 209 (145-273) [4.3] | — |
| Home health care | 599 (479-720) [12.5] | — |
| Miscellaneousk | 57 (19-95) [1.2] | — |
| Had an inpatient procedure | 4613 (4235-4990) [95.9] | — |
| Principal procedure from inpatient record | ||
| Amputation | 1230 (1058-1402) [25.6] | — |
| Wound irrigation/debridement | 1436 (1254-1619) [29.9] | — |
| Reduction/fixation | 831 (697-964) [17.3] | — |
| Skin and soft-tissue grafting/plastics | 527 (424-630) [11.0] | — |
| Muscle/tendon repair | 243 (173-312) [5.0] | — |
| Other orthopedic | 62 (28-96) [1.3] | — |
| Digit/limb reattachment | 65 (31-100) [1.3] | — |
| Ophthalmologic | 17 (0-35) [0.4] | — |
| Other | 397 (314-480) [8.2] | — |
Abbreviations: —, not applicable; ED, emergency department; NCHS, National Center for Health Statistics.
a Data source: Nationwide Emergency Department Sample.11
b Weights provided by the Healthcare Utilization Project in the data files were applied to obtain national estimates.11
c Data source: Howden and Meyer.21
d Data are provided in this column for characteristics that may be compared with US Census data; for characteristics where a comparison is not applicable, an em dash is used.
e NCHS urban–rural code is based on the Office of Management and Budget’s February 2013 delineation of metropolitan and micropolitan statistical areas.15
f Percentages for the distribution of the US population are provided by NCHS from the July 1, 2012, estimate of the resident population for vintage 2012 series of postcensus estimates and do not include numerators.21
g Cells with counts <11 are not shown.
h The Charlson Comorbidity Index is a method of characterizing patient comorbidity using International Classification of Diseases, Ninth Revision, Clinical Modification codes.14 The system identifies 17 comorbidities and assigns each one a weight (from 1 to 6) based on the risk of mortality; these weights are then summed to create a score. A score of 0 indicates that the patient has no comorbidities; higher scores indicate more severe comorbid disease and a greater risk of mortality.16,17
i The ISS is the sum of the squares of the Abbreviated Injury Scale (AIS) scores of the 3 most severe injuries. The AIS is a number that classifies injuries according to the probability of mortality, from 1 (low probability) to 5 (high probability). Accordingly, the ISS can range from 1 to 75 (corresponding to a range from 1 injury of AIS 1 to 3 injuries of AIS 5). An AIS >9 is generally considered severe.19
j Charges adjusted for inflation according to the Consumer Price Index.20
k Includes “against medical advice” (1.1%) and “died in hospital” (0.1%).
Figure.
Age distribution of national estimates of lawn-mower injuries in the United States, 2006-2013. Data source: Nationwide Emergency Department Sample.11
Of 51 151 cases of lawn-mower injuries, 43 567 (95% CI, 42 060-45 074; 85.2%) occurred among men, 17 260 (95% CI, 16 514-18 006; 33.7%) occurred on a Saturday or Sunday, 19 951 (95% CI, 19 057-20 844; 44.4%) occurred from April to June, and 16 735 (95% CI, 15 947-17 524; 37.3%) occurred from July to September (Table 1). Large central metropolitan counties, which encompass 30.5% of the US population, accounted for 15.8% of the observed lawn-mower injuries (n = 8110; 95% CI, 7461-8759). Conversely, micropolitan and noncore nonmetropolitan counties, which collectively encompass 14.8% of the US population, accounted for 13.9% (n = 7094; 95% CI, 6571-7618) and 12.6% (n = 6421; 95% CI, 5923-6920) of all injuries, respectively.
A total of 47 341 (95% CI, 45 724-48 958; 92.6%) cases were Charlson Comorbidity Index 0. Fifty-five percent of patients had an ISS of 1, 29.4% had an ISS ≥4 and <9, 1.5% had an ISS ≥9 and <15, and 0.1% had an ISS ≥15 (indicating severe injury) (Table 1). Based on the Barell Injury Diagnosis Matrix, of 51 151 cases, 33 477 (65.4%) were characterized as injuries to the wrist or hand, 10 122 (19.8%) to the foot or toe, and 3339 (6.5%) to the lower extremity. The most common injury types were lacerations (n = 23 907, 46.7%), fractures (n = 11 433, 22.4%), amputations (n = 11 013, 21.5%), and soft tissue (n = 3022, 5.9%) (Table 2).
Table 2.
National estimates of cases of lawn-mower injuries in the United States, by type of injury and location of injury on the body, by age, based on data from 14 878 patients in the Nationwide Emergency Department Sample, 2006-2013a
| Characteristic | Total | Weighted Estimate of Cases of Lawn-Mower Injuries by Age Group, No.b (%) | |||
|---|---|---|---|---|---|
| 0-4 y | 5-9 y | 10-14 y | 15-19 y | ||
| Total | 51 151 (100) | 965 (1.9) | 735 (1.4) | 1509 (2.9) | 3433 (6.7) |
| Barell Injury Diagnosis Matrix categoriesc | |||||
| Head/neck | 693 (1.4) | 31 (3.2) | 41 (5.6) | 46 (3.0) | 63 (1.8) |
| Eye/face | 521 (1.0) | 13 (1.3) | 24 (3.2) | 18 (1.2) | 19 (0.6) |
| Torso | 792 (1.5) | 11 (1.1) | 13 (1.8) | 12 (0.8) | —d |
| Upper extremity | 1402 (2.7) | 30 (3.1) | 22 (3.1) | 60 (4.0) | 56 (1.6) |
| Wrist/hand | 33 477 (65.4) | 185 (19.2) | 185 (25.2) | 592 (39.2) | 1890 (55.1) |
| Lower extremity | 3339 (6.5) | 117 (12.1) | 136 (18.5) | 154 (10.2) | 213 (6.2) |
| Foot/toe | 10 122 (19.8) | 517 (53.6) | 314 (42.6) | 595 (39.5) | 1153 (33.6) |
| Other | 804 (1.6) | 61 (6.3) | 0 | 32 (2.1) | 28 (0.8) |
| Total | 51 150 (99.9)e | 965 (99.9) | 735 (100.0) | 1509 (100.0) | 3433 (100.0) |
| Injury category | |||||
| Amputation | 11 013 (21.5) | 306 (32.6) | 179 (24.3) | 294 (19.5) | 799 (23.3) |
| Burns | 203 (0.4) | 23 (2.4) | —d | 13 (0.9) | 13 (0.4) |
| Fracture | 11 433 (22.4) | 220 (23.5) | 115 (15.6) | 296 (19.6) | 687 (20.0) |
| Laceration | 23 907 (46.7) | 320 (34.2) | 367 (50.0) | 723 (47.9) | 1635 (47.6) |
| Soft tissue | 3022 (5.9) | 40 (4.2) | 62 (8.4) | 122 (8.1) | 200 (5.8) |
| Other | 1165 (2.3) | 30 (3.2) | —d | 35 (2.3) | 71 (2.1) |
| Missing | 408 (0.8) | 26 (0.0) | 0 | 26 (1.7) | 28 (0.8) |
| Weighted Estimate of Cases of Lawn-Mower Injuries by Age Group, No.b (%) | |||||
| Characteristic | 20-29 y | 30-39 y | 40-49 y | 50-69 y | ≥70 y |
| Total | 7377 (14.4) | 8304 (16.2) | 9897 (19.3) | 13 921 (27.2) | 5013 (9.8) |
| Barell Injury Diagnosis Matrix | |||||
| Head/neck | 102 (1.4) | 61 (0.7) | 91 (0.9) | 151 (1.1) | 109 (2.2) |
| Eye/face | 68 (0.9) | 111 (1.3) | 88 (0.9) | 134 (1.0) | 46 (0.9) |
| Torso | 100 (1.4) | 115 (1.4) | 126 (1.3) | 271 (1.9) | 133 (2.7) |
| Upper extremity | 226 (3.1) | 210 (2.5) | 266 (2.7) | 333 (2.4) | 199 (4.0) |
| Wrist/hand | 4590 (62.2) | 5644 (68.0) | 6953 (70.3) | 10 007 (71.9) | 3432 (68.5) |
| Lower extremity | 406 (5.5) | 417 (5.0) | 517 (5.2) | 860 (6.2) | 520 (10.4) |
| Foot/toe | 1766 (23.9) | 1587 (19.1) | 1728 (17.5) | 1993 (14.3) | 469 (9.4) |
| Other | 119 (1.6) | 159 (1.9) | 128 (1.3) | 172 (1.2) | 105 (2.1) |
| Injury category | |||||
| Amputation | 1507 (20.4) | 1630 (19.6) | 2105 (21.3) | 3138 (22.5) | 1056 (21.1) |
| Burns | 50 (0.7) | 13 (0.2) | 30 (0.3) | 45 (0.3) | —d |
| Fracture | 1442 (19.5) | 1874 (22.6) | 2377 (24.0) | 3245 (23.3) | 1176 (23.5) |
| Laceration | 3656 (49.6) | 4041 (48.7) | 4515 (45.6) | 6350 (45.6) | 2300 (45.9) |
| Soft tissue | 426 (5.8) | 511 (6.2) | 561 (5.7) | 800 (5.7) | 301 (6.0) |
| Other | 226 (3.1) | 144 (1.7) | 247 (2.5) | 275 (2.0) | 134 (2.7) |
| Missing | 70 (0.9) | 91 (1.1) | 62 (0.6) | 68 (0.5) | 39 (0.8) |
a Data source: Nationwide Emergency Department Sample.11
b Weights provided by the Healthcare Utilization Project in the data files were applied to obtain national estimates. Values shown are rounded to the nearest patient, which explains slight differences in totals.
c The Barell Injury Diagnosis Matrix18 is a tool for standardizing the description of injury type and body region of injury using International Classification of Diseases, Ninth Revision, Clinical Modification codes.14
d Cells with counts <11 are not shown.
e Total is not 51 151 because of rounding errors; each category is rounded to the nearest whole patient (injury).
Injuries to the wrist or hand occurred among 70.4% of adults aged 30-69, 25.2% of children aged 5-9, and 19.2% of children aged 0-4. Conversely, injuries to the foot or toe composed 53.6% of injuries among children aged 0-4 and 42.6% of injuries among children aged 5-9, yet only 16.5% of injuries among adults aged 30-69. Injuries to the lower extremities followed a similar pattern. Furthermore, amputation injuries occurred among 32.6% of children aged 0-4 and 21.4% of adults aged 30-69. Other injury types were similarly proportioned in the various age categories (Table 2). The morbidity of these injuries was further characterized by the reporting of types of procedures performed. Ninety-six percent of admitted patients underwent ≥1 procedure. Wound irrigation and debridement was the most common type of procedure (29.9%), followed by amputation (25.6%). Given that 9.4% of patients were admitted, 2.4% of all patients in our study received an amputation procedure (Table 1).
Among discharges from the ED, 43 222 (84.5%) patients were discharged home, 4809 (9.4%) were inpatient admissions, and 2335 (4.5%) were transferred to another facility (ie, short-term hospital, skilled nursing facility, intermediate care facility, or other facility); only 11 (0.02%) patients died in the ED (Table 1). The median hospital length of stay for an admission was 2 days (mean, 3.9 days). Home health care was required for 599 (12.5%) patients at discharge, and 209 (4.3%) of those admitted were discharged to another facility.
The mean inflation-adjusted charge per ED visit was $2482 (Table 1), and total ED charges were $113 million (95% CI, $107 million-$119 million) for the study period, or roughly $14.1 million annually. Total inpatient charges were $177 million (95% CI, $152 million-$202 million) for the study period, for an average of $22.1 million annually. The mean inpatient charge per case was $36 987 (95% CI, $33 065-$40 909).
Discussion
This study presents new data on the incidence and distribution (by age and geography) of lawn-mower injuries in the United States and the hospital charges resulting from such injuries. Using the NEDS database to study data on these injuries allowed for a greater understanding of the epidemiology of these injuries by studying injury type by age category, as well as the morbidity and cost associated with them by providing national estimates of procedures performed, ED charges, and hospital charges.
For patients aged 0-20, the observed age distribution of lawn-mower injuries was consistent with the distribution described in previous studies.3,5,6 National estimates of the incidence of lawn-mower injuries in this study were lower than national estimates obtained in previous studies.3,5-7 Several factors could explain this difference. One factor is whether the ED visit or hospitalization contained ICD-9-CM code E920. Conceivably, the participating hospitals in the NEISS database (on which previous studies have relied) may capture and record data on lawn-mower injuries at a higher rate than data captured by using a single ICD-9-CM code. A second factor is a difference between NEDS and NEISS in the number of hospitals in the sample sizes. The NEISS data are derived from 96 hospitals, whereas NEDS data are derived from 945 hospitals. The larger sample size of NEDS decreases the risk of sampling error.
This study provides nationwide data on the severity of lawn-mower injuries and the types of in-hospital surgical procedures performed after the injury. Only 9.4% of patients were admitted to the hospital, which was similar to the rate observed in other studies.3,5-7 Of these patients, 94.9% underwent at least 1 surgical procedure; the most common was wound irrigation and debridement (30.6%), followed by amputation (27.5%), reduction/fixation (17.5%), and skin and soft-tissue grafting (11.2%). The 2.4% rate of amputation procedure observed in this study was also similar to the 3%-5% found in previous studies3,5-7
The most common type of injury observed was laceration (46.7%), which was similar to the percentage of laceration injuries found in other studies (25%-40%).3,6,7 Our study found a 21.5% incidence of amputation injury, however, and it is unclear why. These amputation injuries were possibly minor (eg, digital) injuries treated in the ED and discharged without an operation.
Analysis of body region injured as stratified by age revealed important differences between adults and children in the epidemiology of lawn-mower injuries. Studies of pediatric lawn-mower injuries did not separate the location of injury based on age.3,4 We found that children aged 0-4 were more likely than teenagers aged 15-19 or adults to be injured on the foot or toe and to sustain an amputation injury. Anecdotally, and based on our experiences treating these patients, this finding equates with young children running into the yard while a family member is operating a lawn mower or sitting on the lap of a riding mower operator, falling, and their foot becoming trapped in the machine. Conversely, older teens and adults were more likely than young children to have an injury to the hand or upper extremity, likely because they stuck their hands into the mower to clear debris from the mower and were injured by the blade. These injury mechanisms have important implications for engineers designing safer machines. For example, a safety mechanism that might prevent injuries to young children could focus on increased visibility for operators, whereas automatic stopping features that are engaged when human flesh is detected near the blades may more uniformly protect against several types of injuries.
Prevention strategies for lawn-mower injuries vary. The American National Standards Institute and the Outdoor Power Equipment Institute maintain voluntary industry standards governing push mowers and riding mowers to ensure uniform operating conditions.2 In 2003, the standards were updated to include a “no mow in reverse” feature, but the standard allows for temporarily disabling this safety mechanism. Safe operating guidelines are published by the Consumer Product Safety Commission,23,24 and professional societies have drafted position statements on safe practices for lawn-mower operation to promote safety awareness.1,25 Despite these efforts, however, available estimates of injury incidence appear relatively unchanged.4,6 Technological safety improvements that are not optional are more likely to be successful than any form of intervention that does not circumvent human behavior. Human factor studies reveal that educational interventions are more likely to fail than new technologies, which bypass human choice.26
Limitations
This study had several limitations. First, we relied on administrative data, particularly ICD-9-CM coding, which is used mostly for billing purposes. In addition, we used a particular E-code to identify lawn-mower injuries. A few states do not require the reporting of E-codes, or their reporting of E-codes to HCUP is incomplete.27 The potential for E-codes to capture data on all lawn-mower injuries may help explain why the incidence of injury observed in this study differed from NEISS data. Second, HCUP provides information only on hospital charges, which do not represent the true costs to the patient, hospital, or third-party payers. Finally, the NEDS database, although it contains 30 million ED records and more than 100 clinical and nonclinical data elements, is missing data on certain items; according to NEDS, about 11% to 15% of data are missing for some information types.11 If cases with and without values are assumed to be similar, however, then the missing data may not be a major concern.
Conclusion
Lawn mowers are a source of preventable injury among children and adults. Hospital charges resulting from these injuries are high. Further prevention policies and engineering solutions are needed on a national scale.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Smith GA; Committee on Injury and Poison Prevention. Technical report: lawn mower-related injuries to children. Pediatrics. 2001;107(6):e106. [DOI] [PubMed] [Google Scholar]
- 2. American National Standards Institute. Consumer Turf Care Equipment—Pedestrian-Controlled Mowers and Ride-On Mowers—Safety Specifications. ANSI/OPEI(B71.1-2017) Washington, DC: American National Standards Institute; 2017. [Google Scholar]
- 3. Vollman D, Smith GA. Epidemiology of lawn-mower-related injuries to children in the United States, 1990-2004. Pediatrics. 2006;118(2):e273–e278. [DOI] [PubMed] [Google Scholar]
- 4. Bachier M, Feliz A. Epidemiology of lawnmower-related injuries in children: a 10-year review. Am J Surg. 2016;211(4):727–732. [DOI] [PubMed] [Google Scholar]
- 5. Ren KS, Chounthirath T, Yang J, Friedenberg L, Smith GA. Children treated for lawn mower-related injuries in US emergency departments, 1990-2014. Am J Emerg Med. 2017;35(6):893–898. [DOI] [PubMed] [Google Scholar]
- 6. Costilla V, Bishai DM. Lawnmower injuries in the United States: 1996 to 2004. Ann Emerg Med. 2006;47(6):567–573. [DOI] [PubMed] [Google Scholar]
- 7. Hammig B, Childers E, Jones C. Injuries associated with the use of riding mowers in the United States, 2002-2007. J Safety Res. 2009;40(5):371–375. [DOI] [PubMed] [Google Scholar]
- 8. Conner KA, McKenzie LB, Xiang H, Smith GA. Pediatric traumatic amputations and hospital resource utilization in the United States, 2003. J Trauma. 2010;68(1):131–137. [DOI] [PubMed] [Google Scholar]
- 9. Loder RT, Dikos GD, Taylor DA. Long-term lower extremity prosthetic costs in children with traumatic lawnmower amputations. Arch Pediatr Adolesc Med. 2004;158(12):1177–1181. [DOI] [PubMed] [Google Scholar]
- 10. Schroeder T, Ault K. The NEISS Sample (Design and Implementation) From 1979 to 1996. Washington, DC: US Consumer Product Safety Commission; 2001. [Google Scholar]
- 11. Healthcare Cost and Utilization Project. 2014 introduction to the HCUP Nationwide Emergency Department Sample (NEDS). 2015. https://www.hcup-us.ahrq.gov/db/nation/neds/NEDS_Introduction_2015.jsp. Accessed June 18, 2018.
- 12. US Department of Health and Human Services. About Agency for Healthcare Research and Quality (AHRQ). Reviewed November 2017 https://www.ahrq.gov/cpi/about/index.html. Accessed June 18, 2018.
- 13. Taylor CA, Greenspan AI, Xu L, Kresnow MJ. Comparability of national estimates for traumatic brain injury-related medical encounters. J Head Trauma Rehabil. 2015;30(3):150–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Centers for Disease Control and Prevention, National Center for Health Statistics. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Reviewed November 2015 https://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed June 18, 2018.
- 15. Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat. 2012;2(154):1–73. [PubMed] [Google Scholar]
- 16. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 17. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. [DOI] [PubMed] [Google Scholar]
- 18. Barell V, Aharonson-Daniel L, Fingerhut LA, et al. An introduction to the Barell body region by nature of injury diagnosis matrix. Inj Prev. 2002;8(2):91–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Baker SP, O’Neill B, Haddon W, Jr, Long WB. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–196. [PubMed] [Google Scholar]
- 20. US Department of Labor, Bureau of Labor Statistics. CPI inflation calculator. https://www.bls.gov/data/inflation_calculator.htm. Accessed June 18, 2018.
- 21. Howden LM, Meyer JA. Age and sex composition: 2010. 2010 Census Briefs. 2011. http://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf. Accessed June 18, 2018.
- 22. StataCorp. Stata: Release 14.2. College Station, TX: StataCorp; 2015. [Google Scholar]
- 23. US Consumer Product Safety Commission. CPSC fact sheet: power lawn mowers. https://www.cpsc.gov/s3fs-public/5126%20Walk%20Behind%20Power%20Mower%20Fact%20Sheet.pdf. Accessed June 18, 2018.
- 24. US Consumer Product Safety Commission. CPSC fact sheet: riding lawnmowers. https://www.cpsc.gov/s3fs-public/588%20Riding%20Lawnmower%20Fact%20Sheet.pdf. Accessed June 18, 2018.
- 25. American Academy of Orthopedic Surgeons. Position statement: power lawnmower safety. Revised June 2014 https://www.aaos.org/uploadedFiles/PreProduction/About/Opinion_Statements/position/1142%20Power%20Lawnmower%20Safety(1).pdf. Accessed June 18, 2018.
- 26. Shouhed D, Gewertz B, Wiegmann D, Catchpole K. Integrating human factors research and surgery: a review. Arch Surg. 2012;147(12):1141–1146. [DOI] [PubMed] [Google Scholar]
- 27. Agency for Healthcare Research and Quality. NIS description of data elements: ECODEn—ICD-9-CM external cause of injury code. 2008. https://www.hcup-us.ahrq.gov/db/vars/ecoden/nisnote.jsp. Accessed June 18, 2018.